Published online Mar 27, 2015. doi: 10.4240/wjgs.v7.i3.47
Peer-review started: July 14, 2014
First decision: August 14, 2014
Revised: January 20, 2015
Accepted: January 30, 2015
Article in press: February 2, 2015
Published online: March 27, 2015
Processing time: 260 Days and 14 Hours
Amyand’s hernia is a rare condition defined by the inclusion of the appendix vermiformis within the hernia sac. Its incidence among cases of groin hernia is less than 1%. The clinical manifestation of incarcerated inguinal hernia generally masks the symptoms and signs of acute appendicitis, which renders preoperative diagnosis difficult. In this study, we present two cases of Amyand’s hernia that were diagnosed preoperatively. The patients were taken for operation with the prediagnosis of ıncarcerated inguinal hernia. We evaluated these cases along with data from prior studies.
Core tip: Amyand’s hernia is a seldom surgical pathology whereby there is inclusion of the appendix vermiformis within the groin hernia sac. Its incidence among cases of groin hernia is less than 1%. The clinical presentation of incarcerated inguinal hernia generally masks the symptoms and signs of acute appendicitis, which renders preoperative identification difficult. Owing to the rarity of the condition there is yet no general consensus pertaining the diagnosis and management approach. Arguments continue as to whether to do or not appendectomy and where to employ a mesh during operation. In this paper we share our experience in the diagnosis and treatment of this rare condition by presenting two cases of Amyand’s hernia one having acute appendicitis and the other gangraneous appendicitis.
- Citation: Ciftci F, Abdulrahman I. Incarcerated amyand hernia. World J Gastrointest Surg 2015; 7(3): 47-51
- URL: https://www.wjgnet.com/1948-9366/full/v7/i3/47.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v7.i3.47
Amyand’s hernia may present with the inflammation of the appendix vermiformis enclosed in its sac, albeit rarely. The disorder comprises less than 1% of all inguinal hernia cases and 0.2% of appendicitis cases. Consensus has yet to be reached regarding the risk involved in herniorrhaphy with prosthetic material subsequent to the resection of the inflammed appendix and regarding the necessity of resecting an uninflammed appendix. Due to the rarity of this condition, management of Amyand’s hernia varies amongst different clinicians and can even vary for the same clinician over time. The presence of an inflammed appendix vermiformis in the sac of an inguinal hernia is referred to as Amyand’s hernia. The condition was first described by an English surgeon named Claudius Amyand in an 11-year-old male patient after finding a perforated appendix in the sac of the inguinal hernia. The disorder has since carried Amyand’s name. The incidence of the presence of an uninflammed appendix vermiformis in the sac of an inguinal hernia is estimated to be 0.13%, but it is even rarer to find an inflammed appendix in an inguinal hernia sac[1,2]. Routinely found within the sac of an inguinal are the omentum, small intestine or urinary bladder. Aside from these conditions, Meckel’s diverticulum (Littre’s hernia), part of the wall of the intestine (Richter’s hernia), or inflammed or uninflammed appendix vermiformis (Amyand’s hernia) may be included in the sac of an inguinal hernia[3,4]. In this paper, we aim to discuss our cases along with data from current studies.
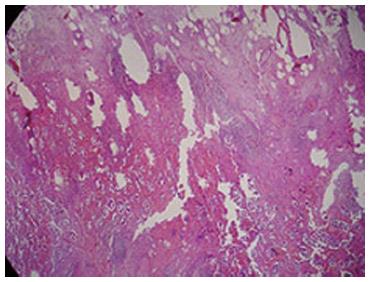
A 27-year-old male patient reported to our emergency clinic with complaints of pain, swelling and loss of appetite for the past 10 h of an inguinal hernia that had been present for 3 years. There was tenderness at the right lower quadrant. Neither defence nor rebound tenderness was present. Air-fluid levels attributable to the small bowel could be appreciated on a direct X-ray of the abdomen. The patient had not experienced any loss in appetite and could break wind. He had no fever, and his white blood count was 12000⁄mm3. He was operated on for irreducible hernia and perioperatively, the cecum was found to be within the hernia sac (Figure 1). As expected in Amyand’s hernias, a sliding hernia formed part of the sac wall, and the appendix was slightly edematous and gangrenous, presumably due to impaired blood circulation. An appendectomy was accomplished, the stump was embedded, and the cecum was retrieved from the sac. Part of the hernia sac was resected, and the peritoneum was covered, after which non-tensile plication with prolen was accomplished. A prolen mesh (15 cm × 10 cm) was spread to reinforce the herniorrhaphy region. The patient was discharged from the hospital without complications on the second postoperative day. In a follow-up one week later, the right inguinal region looked to be healing well. The pathology examination reported an acute gangrenous appendicitis. There was active intense inflammation with neutrophilic leucocytes predominance that infiltrates tissues surrounding the appendix and distruct all layers of the appendix wall (Figure 2).
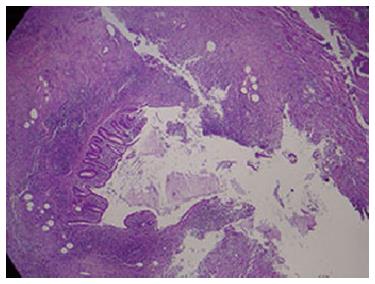
A 24-year-old male patient reported with increased swelling and pain for the last 3 h in his inguinal hernia that had been present for 2 years. An attempt to reduce the hernia was unsuccessful. The patient’s white blood count was within normal range (9800/mm3), and direct abdominal X-rays revealed nothing noteworthy. In the operation, the appendix was found to adhere to the inner surface of the hernia sac (Figure 3). The pathology looked to be an acute appendicitis with a mixture of inflaming cells on the appendiceal wall, presenting a great deal of eosinophils and few focus of granulomatous lesion (Figure 4). Through the same incision, an appendectomy, herniorrhaphy and prolen mesh reinforcement were accomplished. The patient was discharged from the hospital without complications on the first postoperative day. In a follow-up one week later, the right inguinal region looked to be healing well.
The current practical approach includes appendectomy and hernia repair with prolen mesh in cases in which the appendix is intact or inflammed without perforation. However, in the presence of perforation, the proposal includes appendectomy and herniorrhaphy without the use of prolen mesh so as to avoid subsequent infection, recurrent hernia and enterocutaneous fistula. The lack of consensus is due, in large part, to a lack of large-scale studies and meta analyses. The absence of typical clinical presentation and manifestation of acute appendicitis in the cases presented above indicates that the appendicitis was the result of extraluminal tension. The disorder is generally right-located due to the malpositioning of the cecum as a predisposing factor. The inflammation of the appendix in an Amyand’s hernia of an incarcerated or sliding type may be due to the process of incarceration itself[5]. In cases with chronic hernia adhesions and increased intraabdominal pressure due to contraction of the abdominal wall, the appendiceal mesothelium is squeezed, thereby hindering the perfusion of the appendix. This in turn leads to inflammation and increased bacterial colonization of the appendix[6]. A chronic process is always involved in the disorder’s mechanism of development.
Differential diagnoses of Amyand’s hernia include incarcerated or strangulated inguinal hernia, inguinal lympadenitis, testicular torsion, acute epididymitis, acute hydrocele and focal panniculitis[6-8]. It is difficult to diagnose Amyand’s hernia preoperatively. Patient clinical complaints and laboratory findings are usually inadequate for the diagnosis. Generally, although it is easy to diagnose a hernia, an ultrasonic or tomographic evaluation is needed to ascertain the presence of an inflamed or intact appendix within the hernia sac. These two techniques are not routinely employed in hernia surgery. Nevertheless, there are reports of cases being diagnosed with the aid of tomography prior to an operation[9]. In most instances, however, the diagnosis is made during the operation, as was the case with our diagnoses.
Amyand hernia is an unusual condition involving the presence of different entities, and a preoperative identification enigma, and requiring expertise in two surgical difficulties: symptomatic hernia and appendicitis. Management is surgical, and in a hernioplasty with or without an appendectomy related to intraoperative detection, a routine prophylactic appendectomy is not indicated[10-12].
Sharma et al[13] briefly discussed treatment for Amyand’s hernia amid 18 patients within a 15-year time period, including appendectomy followed by the Bassini repair, mesh hernioplasty, later reduction of a normal appendix, and Bassini’s hernia repair plus a lower midline laparotomy for a pelvic washout. His strategy is dependent on the status of the appendix in the sac.
The management for hernial appendicitis is appendectomy through the herniotomy with primary hernia repair using the identical incision. Lyass et al[14] reported delayed wound closure due to retroperitoneal abscess secondary to the appendicular inflammation. Mesh is not recommended in a contaminated abdominal wall defects due to a greater risk of being wounded or of developing an infection or appendiceal stump fistula. Laparoscopic reduction of Amyand’s hernia has been studied previously[15].
In our cases, each patient suffered from a right inguinal hernia. Presumably, repetitive reduction led to inflammation of the region, or in the absence of inflammation pressure on the organs causes pain, thus leading patients to feel the need to report to the hospital.
When the appendix enclosed in the hernia sac is inflamed or perforated, complication rates increase. In such cases, repair methods for Amyand’s hernia differ from the standard approach. Grafting may be employed in cases in which neither inflammation nor perforation occurs. In other situations, grafting provokes an inflammatory reaction that may lead to complications, such as incision site infection and stump fistula[8,10]. As reported in the literature, a prosthetic mesh should be avoided due to a high risk of infection. Findings regarding the use of prosthetic mesh to repair Amyand’s hernia with Losanoff 2-4 have been reported (Table 1) by Priego et al[16]. In all cases, an appendectomy was performed via the hernia sac, and acute appendicitis was found to be present in four them. A prosthetic mesh was used in 3 cases, and 1 case of wound infection was also found. In the other cases, the hernia ring was sutured using propilene. In each of our cases, at the same time that we carried out the appendectomy, we successfully treated the hernia through an inguinal incision anatomically with a propilene mesh. There was minimal abscess formation found in the sac. Both patients were discharged from the hospital with no complications. The patients seemed healthy in a follow-up two years later.
| Definition | Surgical management | |
| Type 1 | Normal appendix | Reduction, mesh hernioplasty |
| Type 2 | Acute appendicitis No abdominal sepsis | Appendectomy through the hernia, hernioplasty with native tissues, no mesh |
| Type 3 | Acute appendicitis Abdominal sepsis present | Appendectomy through laparatomy, hernioplasty with native tissues, no mesh |
| Type 4 | Acute appendicitis within inguinal hernia Other abdominal pathology Related or unrelated | Manage as with types 1 to 3 hernia investigate or treat second pathology as appropriate |
As for the repair of the hernia, several authors recommend delayed repair or suturing repair rather than prosthetic mesh so as to avoid complications arising from potential infection. Further study is required to define the optimal surgical strategy, prognostic factors and risk of hernia recurrence[4,17-20]. In each of our cases, the operation was performed immediately, and minimally abscess formation was found in the sac. We chose simultaneous appendectomy and primary hernioplasty using prosthetic mesh as treatment for these cases. Although mesh is generally not suggested for use with Amyand’s hernia, mesh can be used with acute appendicitis in selected cases.
The authors express their gratitude and thanks to all participating patients and do clinical staff.
Clinical symptoms include abdominal pain, and new onset swelling in hours around the hernia and loss of appetite.
Incarcerated amyand hernia, acute gangrenous appendicitis at the same time.
Incarcerated hernia.
Laboratory tests showed a leucocytosis for case 1 (12000/mm3; 4100-11200) and case 2 (9800/mm3; 4100-11200).
An abdominal X-ray radiography indicated air-fluid levels.
Pathology findings indicated acute gangrenous appendicitis.
Appendectomy and prolen mesh in use hernia sac repair.
Amyand’s hernia is a rare condition defined by the inclusion of the appendix vermiformis within the hernia sac. Its incidence among cases of groin hernia is less than 1%. The clinical manifestation of incarcerated inguinal hernia generally masks the symptoms and signs of acute appendicitis, which renders preoperative diagnosis difficult.
The authors described two cases of Amyand’s hernia in two adult male patients. It is an extremely interesting cases series.
| 1. | Ozturk E, Garip G, Yilmazlar T. Amyand hernia. Uludag Universitesi Tip Fakultesi Dergisi. 2004;30:225-226. |
| 2. | Suliman E, Popa D, Palade R, Simion G. Amyand’s hernia--case presentation and a discussion about diagnosis problems and surgical treatment. Chirurgia (Bucur). 2012;107:393-396. [PubMed] |
| 3. | Amyand C. Of an inguinal rupture, with a pin in the appendix caeci encrusted with stone: some observations on wounds in the guts. Phil Trans R Soc Lond. 1936;39:329-336. [RCA] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 90] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Kwok CM, Su CH, Kwang WK, Chiu YC. Amyand’s Hernia - Case Report and Review of the Literature. Case Rep Gastroenterol. 2007;1:65-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Solecki R, Matyja A, Milanowski W. Amyand’s hernia: a report of two cases. Hernia. 2003;7:50-51. [PubMed] |
| 6. | Carey LC. Acute appendicitis occurring in hernias: a report of 10 cases. Surgery. 1967;61:236-238. [PubMed] |
| 7. | Davies MG, O’Byrne P, Stephens RB. Perforated appendicitis presenting as an irreducible inguinal hernia. Br J Clin Pract. 1990;44:494-495. [PubMed] |
| 9. | Luchs JS, Halpern D, Katz DS. Amyand’s hernia: prospective CT diagnosis. J Comput Assist Tomogr. 2000;24:884-886. [PubMed] |
| 10. | Psarras K, Lalountas M, Baltatzis M, Pavlidis E, Tsitlakidis A, Symeonidis N, Ballas K, Pavlidis T, Sakantamis A. Amyand’s hernia-a vermiform appendix presenting in an inguinal hernia: a case series. J Med Case Rep. 2011;5:463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Quartey B, Ugochukwu O, Kuehn R, Ospina K. Incarcerated recurrent Amyand’s hernia. J Emerg Trauma Shock. 2012;5:344-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Torino G, Campisi C, Testa A, Baldassarre E, Valenti G. Prosthetic repair of a perforated Amyand’s hernia: hazardous or feasible? Hernia. 2007;11:551-552; author reply 553-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Sharma H, Gupta A, Shekhawat NS, Memon B, Memon MA. Amyand’s hernia: a report of 18 consecutive patients over a 15-year period. Hernia. 2007;11:31-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 160] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 14. | Lyass S, Kim A, Bauer J. Perforated appendicitis within an inguinal hernia: case report and review of the literature. Am J Gastroenterol. 1997;92:700-702. [PubMed] |
| 15. | Bamberger PK. Revisiting Amyand’s hernia in the laparoscopic era. Surg Endosc. 2001;15:1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Priego P, Lobo E, Moreno I, Sánchez-Picot S, Gil Olarte MA, Alonso N, Fresneda V. Acute appendicitis in an incarcerated crural hernia: analysis of our experience. Rev Esp Enferm Dig. 2005;97:707-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Chatzimavroudis G, Papaziogas B, Koutelidakis I, Tsiaousis P, Kalogirou T, Atmatzidis S, Atmatzidis K. The role of prosthetic repair in the treatment of an incarcerated recurrent inguinal hernia with acute appendicitis (inflamed Amyand’s hernia). Hernia. 2009;13:335-336; author reply 337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Kueper MA, Kirschniak A, Ladurner R, Granderath FA, Konigsrainer A. Incarcerated recurrent inguinal hernia with covered and perforated appendicitis and periappendicular abscess: case report and review of the literature. Hernia. 2007;11:189-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Losanoff JE, Basson MD. Amyand hernia: a classification to improve management. Hernia. 2008;12:325-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 129] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 20. | Ebisawa K, Yamazaki S, Kimura Y, Kashio M, Kurito K, Yasumuro S, Nishida S, Takayama T. Acute Appendicitis in an Incarcerated Femoral Hernia: A Case of De Garengeot Hernia. Case Rep Gastroenterol. 2009;3:313-317. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Piccolo G, Park KU, Rangarajan M, Sanabria A S- Editor: Gong XM L- Editor: A E- Editor: Wu HL