Published online May 27, 2014. doi: 10.4240/wjgs.v6.i5.80
Revised: January 10, 2014
Accepted: April 17, 2014
Published online: May 27, 2014
Processing time: 188 Days and 9.5 Hours
The occurrence of a hepatoduodenal ligament teratoma is extremely rare, with only a few cases reported in the literature. This case report describes the discovery of a hepatoduodenal ligament lesion revealed during abdominal ultrasonography for cholelithiasis-related abdominal pain in a 27-year-old female. Cross-sectional imaging identified a 5 cm × 4 cm heterogeneous mass of fat tissue with irregular calcification located in the posterior-superior aspect of the head of the pancreas. An encapsulated lesion showing no invasion to the common bile duct or adjacent organs and vessels was exposed during laparotomy and resected. Intraoperative cholangiography during the cholecystectomy showed no abnormalities. The postoperative course was uneventful. Pathological analysis of the resected mass indicated hepatoduodenal ligament teratoma. This case report demonstrates that cross-sectional imaging, such as computed tomography, can reveal suspected incidences of this rare type of teratoma, which can then be confirmed after pathologic analysis of the specimen. The prognosis after complete surgical resection of lesions presenting with benign pathological features is excellent.
Core tip: The 10th reported case of hepatoduodenal ligament teratoma is presented in a patient who underwent cross-sectional imaging for the evaluation of an abdominal mass. As incidences of hepatoduodenal ligament teratoma are extremely rare, this report may help physicians to suspect this disorder in an emergent group of patients with abdominal incidentaloma.
- Citation: Jeismann VB, Dumarco RB, Loreto CD, Barbuti RC, Jukemura J. Rare cause of abdominal incidentaloma: Hepatoduodenal ligament teratoma. World J Gastrointest Surg 2014; 6(5): 80-83
- URL: https://www.wjgnet.com/1948-9366/full/v6/i5/80.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v6.i5.80
Teratomas are neoplasms comprised of mixed dermal elements derived from the three germ cell layers. Although the majority of teratomas are congenitally present in the gonads of men and women, they have been identified in extra-gonadal sites, such as the anterior mediastinum, retroperitoneum and sacrococcygeal regions[1]. Teratomas in the hepatoduodenal ligament are extremely rare, with only nine cases described in the literature[2-10] (Table 1). We report a case of hepatoduodenal ligament teratoma in an adult female patient examined for cholelithiasis-related abdominal pain.
| Patient | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Year reported | 1986 | 1989 | 1993 | 2004 | 2004 | 2005 | 2008 | 2008 | 2012 | 2013 |
| Ref. | Frexes et al[2] | Akimov et al[3] | Kim et al[4] | Demircan et al[5] | Wang et al[6] | Sasaki et al[7] | Ukiyama et al[8] | Souftas et al[9] | Bagga et al[10] | Our case |
| Age | Neonate | 6 yr | 5 yr | 4 mo | 29 yr | 38 yr | 20 mo | 26 yr | 11 yr | 27 yr |
| Sex | NA | NA | Male | Female | Female | Male | Male | Female | Female | Female |
| Origin | Extrahepatic bile duct | HL | CBD | Anomalous CBD | HL | HL | HL | HL | HL and fistulization with the CBD | HL |
| Signs and symptoms | Jaundice | Portal hypertension | Jaundice | Jaundice, abdominal distension | Portal hypertension | Abdominal mass | Abdominal mass | Abdominal pain | Jaundice, abdominal mass | Asymptomatic |
| Size | Small mass | NA | NA | Cystic mass 15 cm | Solid mass 7 cm × 6 cm × 6 cm | Cystic mass 8 cm | Solid mass 9 cm × 6 cm × 6 cm | Cystic mass 11 cm | Cystic mass 9 cm × 9 cm | 5 cm × 4 cm |
| Pathology | Teratoma | NA | Endodermal sinus tumor associated with teratoma | Benign cystic teratoma | Benign teratoma | Benign cystic teratoma | Benign teratoma | Dermoid cyst | Benign cystic teratoma | Benign teratoma |
| Treatment | Local excision, recurrence, re-excision with chemotherapy | NA | Whipple’s operation with chemotherapy | Extirpation with CBD | Extirpation | Extirpation with CBD, Roux-en-Y, Choledocho-jejunostomy | Extirpation | Excision of the tumor | Extirpation leaving the outer cyst wall in situ (Lilly technique), hepatico-duodenostomy | Extirpation |
| Prognosis | Asymptomatic after 5 yr | Death | Death | Asymptomatic after 4 yr | Asymptomatic after 2 yr | NA | Asymptomatic after 5 yr | Asymptomatic after 33 mo | Asymptomatic after 2 yr | Asymptomatic after 6 mo |
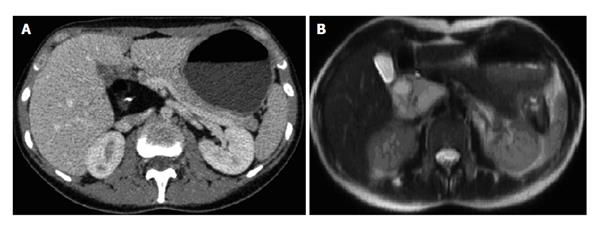
A 27-year-old female presented with cholelithiasis-related pain. There was no history of jaundice, and the past medical history was unremarkable. Physical examination failed to detect the presence of an abdominal mass, and routine laboratory tests were normal. Abdominal ultrasonography revealed cholelithiasis and a mass adjacent to the hepatic hilum. Computed tomography (CT) and magnetic resonance imaging revealed a heterogeneous mass of 5 cm × 4 cm comprised of fat tissue and irregular calcifications located in the hepatoduodenal ligament at the posterior-superior aspect of the head of the pancreas (Figure 1).
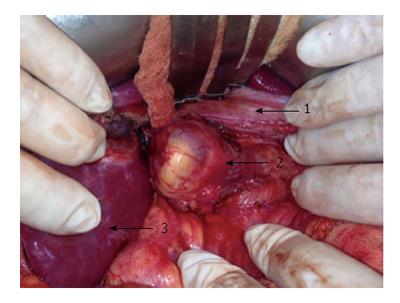
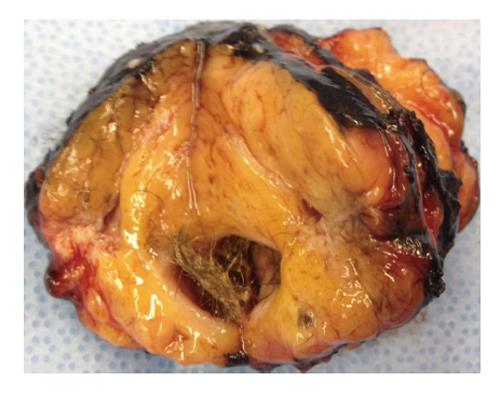
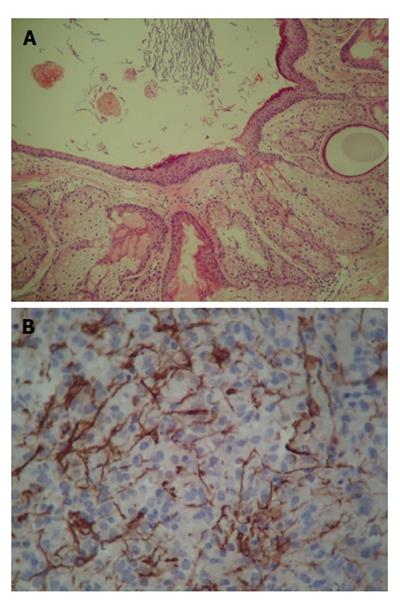
Following patient consent, a laparotomy was performed. A Kocher maneuver with extensive mobilization of the duodenum exposed an encapsulated lesion. It was dissected and resected, and the multiple small vessels from the hepatic pedicle to the lesion were divided. There was no invasion of adjacent organs, vessels or the common bile duct (Figures 2 and 3). A cholecystectomy was performed and the intraoperative cholangiogram did not show abnormalities. The postoperative course was uneventful, and the patient was discharged after four days. The patient remains asymptomatic after six months. Histopathology confirmed that the mass was a mature teratoma. Microscopic examination revealed the presence of a cystic wall with cutaneous annexes and a mature neural area with glial fibrillary acidic protein immunoreactivity (Figure 4).
Teratomas are composed of structures derived from the three germ layers, namely the ectoderm, mesoderm and endoderm. Most mature teratomas are benign, but can undergo a malignant change in one of their elements[6]. Although plain abdominal radiographs show calcification in most (60%) extra-gonadal teratomas, either in the wall of the cyst or in structures such as teeth or bones, CT is generally the most helpful imaging modality for diagnosis[7].
An extensive review of the literature identified nine reported cases of hepatoduodenal teratoma[2-10]. Six of the described cases were in children[2-5,8,10], and the oldest patient identified was 38 years old at the time of diagnosis[7]. A small gender difference is evident, as the lesions were more often described in women[5,6,9,10]. Clinical manifestations were variable, including jaundice[2,4,10], portal hypertension[3,6] and a palpable abdominal mass[7,8,10]. Some patients demonstrated elevated levels of serum alpha-fetoprotein, carcinoembryonic antigen and carbohydrate antigen 19-9, but these do not appear to be clinically useful[7]. The majority of cases reported tumors with benign pathology features, except for one case with an endodermal sinus tumor[4], and two cases that did not provide described pathology report details[2,3]. All patients underwent surgical resection, and two patients received chemotherapy[2,4], with only one incidence of recurrence[2]. Since a definitive diagnosis is only achieved following histologic examination of the cyst, surgical resection remains the primary treatment with an excellent prognosis[7]. In conclusion, this is the first reported asymptomatic case, to our knowledge, of hepatoduodenal ligament teratoma, indicating that teratomas should not be ruled out in cases of abdominal incidentaloma.
The patient was asymptomatic.
The patient was diagnosed with abdominal incidentaloma uncovered during investigation of cholelithiasis-related abdominal pain.
Benign and malignant abdominal tumors were alternative diagnoses.
A heterogeneous mass of 5 cm × 4 cm with fat tissue and irregular calcifications was located in the posterior-superior aspect of the head of the pancreas, into the hepatoduodenal ligament.
Analysis by microscopy revealed a mature teratoma cystic wall with cutaneous annexes and glial fibrillary acidic protein staining of a mature neural area, findings that are consistent with a teratoma.
The patient was treated by surgical resection of the tumor.
A hepatoduodenal teratoma is a rare occurrence and, to the best of the authors’ knowledge, this is the 10th reported case and the 1st asymptomatic reported case.
Hepatoduodenal ligament teratoma refers to a neoplasm that is comprised of mixed dermal elements derived from the three germ cell layers and located at the portion of the lesser omentum extending between the porta hepatis of the liver and superior part of the duodenum. Computer tomography is a technology that uses computer-processed X-rays to produce cross-sectional imaging of the human body. Abdominal incidentaloma has been defined as an intraabdominal tumor found in a patient without symptoms, usually during evaluation of unrelated diseases or screening programs. Cholelithiasis is defined by the presence/formation of stones within the biliary tract, most commonly the gallbladder.
Teratomas must be included on differential diagnosis of all abdominal incidentalomas.
This case report provides a description of a rare disease that may be under-diagnosed due to a low index of suspicion. The pathological, radiological and surgical findings are well documented.
| 1. | Engel RM, Elkins RC, Fletcher BD. Retroperitoneal teratoma. Review of the literature and presentation of an unusual case. Cancer. 1968;22:1068-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 2. | Frexes M, Neblett WW, Holcomb GW. Spectrum of biliary disease in childhood. South Med J. 1986;79:1342-1349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Akimov OV. [Hepatoduodenal ligament teratoma followed by hypertensive syndrome of the portal vein]. Arkh Patol. 1989;51:60-62. [PubMed] |
| 4. | Kim WS, Choi BI, Lee YS, Chi JG, Park HR, Kim I, Yeon KM, Han MC. Endodermal sinus tumour associated with benign teratoma of the common bile duct. Pediatr Radiol. 1993;23:59-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Demircan M, Uguralp S, Mutus M, Kutlu R, Mizrak B. Teratoma arising from anomalous common bile ducts: a case report. J Pediatr Surg. 2004;39:e1-e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Wang H, Dong J. Teratoma in the hepatoduodenal ligament followed by portal hypertension syndrome. J Gastroenterol Hepatol. 2004;19:477-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Sasaki H, Ajiki T, Takase S, Fujino Y, Suzuki Y, Tominaga M, Ku Y, Kuroda Y. Images of interest. Hepatobiliary and pancreatic: mature cystic teratoma in the hepatoduodenal ligament. J Gastroenterol Hepatol. 2005;20:317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Ukiyama E, Endo M, Yoshida F. Hepatoduodenal ligament teratoma with hepatic artery running inside. Pediatr Surg Int. 2008;24:1239-1242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Souftas V, Polychronidis A, Giatromanolaki A, Perente S, Simopoulos C. Dermoid cyst in the hepatoduodenal ligament: report of a case. Surg Today. 2008;38:959-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Bagga D, Jindal B, Naredi BK, Yadav DK, Acharya SK, Mahato R, Gupta K. Portal teratoma causing obstructive jaundice in children: a rarity. J Pediatr Surg. 2012;47:1449-1452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
P- Reviewers: Scheidbach H, Sugawara Y, Seow-Choen F S- Editor: Qi Y L- Editor: A E- Editor: Liu SQ