Published online Oct 27, 2014. doi: 10.4240/wjgs.v6.i10.204
Revised: August 1, 2014
Accepted: September 6, 2014
Published online: October 27, 2014
Processing time: 142 Days and 1.8 Hours
Axial torsion and necrosis of Meckel’s diverticulum causing simultaneous mechanical small bowel obstruction are the rarest complications of this congenital anomaly. This kind of pathology has been reported only eleven times. Our case report presents this very unusual case of Meckel’s diverticulum. A 41-year-old man presented at the emergency department with complaints of crampy abdominal pain, nausea and retention of stool and gases. Clinical diagnosis was small bowel obstruction. Because the origin of obstruction was unknown, computer tomography was indicated. Computed tomography (CT)-scan revealed dilated small bowel loops with multiple air-fluid levels; the oral contrast medium had reached the jejunum and proximal parts of the ileum but not the distal small bowel loops or the large bowel; in the right mid-abdomen there was a 11 cm × 6.4 cm × 7.8 cm fluid containing cavity with thickened wall, which was considered a dilated bowel-loop or cyst or diverticulum. Initially the patient was treated conservatively. Because of persistent abdominal pain emergency laparotomy was indicated. Abdominal exploration revealed distended small bowel loops proximal to the obstruction, and a large (12 cm × 14 cm) Meckel’s diverticulum at the site of obstruction. Meckel’s diverticulum was axially rotated by 720°, which caused small bowel obstruction and diverticular necrosis. About 20 cm of the small bowel with Meckel’s diverticulum was resected. The postoperative course was uneventful and the patient was discharged on the fifth postoperative day. We recommend CT-scan as the most useful diagnostic tool in bowel obstruction of unknown origin. In cases of Meckel’s diverticulum causing small bowel obstruction, prompt surgical treatment is indicated; delay in diagnosis and in adequate treatment may lead to bowel necrosis and peritonitis.
Core tip: Axial torsion and necrosis of Meckel’s diverticulum causing simultaneous mechanical small bowel obstruction are the rarest complications of this congenital anomaly. This kind of pathology has been reported only eleven times.
- Citation: Murruste M, Rajaste G, Kase K. Torsion of Meckel's diverticulum as a cause of small bowel obstruction: A case report. World J Gastrointest Surg 2014; 6(10): 204-207
- URL: https://www.wjgnet.com/1948-9366/full/v6/i10/204.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v6.i10.204
Although Meckel’s diverticulum was first described by Fabricus Heldanus in 1650[1], and reported thereafter by Levator in 1671[2] and by Ruysch in 1730[3], it was named after Johann Friedrich Meckel who established its embryonic origin in 1809[4].
The characteristics of Meckel’s diverticulum can be best remembered by the “rule of two”: occurs in 2% of population; usually discovered before 2 years of age; 2 inches long and 2 cm in diameter; located 2 feet proximal to the ileocecal valve; 2 times more common in males; only 2% of the individuals with Meckel’s diverticulum are symptomatic[5-7].
Blood supply is derived from a remnant of the primitive vitelline artery arising from the superior mesenteric artery, or less commonly from the ileocolic artery[8,9].
We present a very unusual case of Meckel’s diverticulum-small bowel obstruction caused by axial torsion and gangrene of Meckel’s diverticulum.
Axial torsion of Meckel’s diverticulum is the rarest of complications[10]; gangrene of Meckel’s diverticulum secondary to axial torsion has been reported only eleven times in adults[10-17].
Only two cases of coexistence of gangrenous Meckel’s diverticulum and small bowel obstruction have been reported in the English-language literature[14,15].
A 41-year-old man presented at the emergency department with complaints of crampy and intermittent abdominal pain, nausea and retention of stool and gases. Previously the patient had been hospitalized four times with small bowel obstruction and conservative treatment had always been successful. The etiology of small bowel obstruction had remained unclear. The patient had never undergone any operations; nor had he hernias of abdominal wall. He did not have any other accompanying diseases and did not take any medications.
Physical examination revealed normal body temperature, and stable haemodynamics. The right mesogastrium was tender on palpation, peristalsis was high-sounding. On rectal examination the rectum contained no stool.
Initial laboratory tests showed haemoconcentration, the biochemical values were all normal. Initial abdominal X-ray showed air-fluid levels in projection of the small bowel (Figure 1).
Ultrasonography of the abdomen showed dilated small-bowel loops with peristalsis partially present.
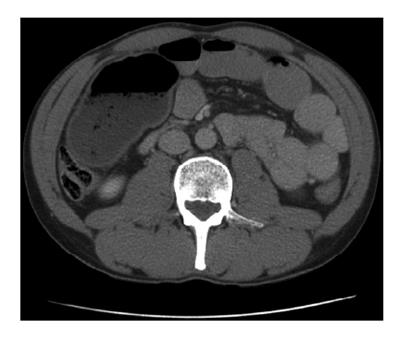
Initial management of the patient included intravenous fluid resuscitation and nasogastric tube insertion. An abdominal computed tomography (CT)-scan was performed to specify the cause of small bowel obstruction. The CT-scan showed markedly dilated small-bowel loops with multiple air-fluid levels. The oral contrast medium was seen in the jejunum and proximal parts of the ileum but not in the distal small bowel loops or in the large bowel. In the right mid-abdomen there was a 11 cm × 6.4 cm × 7.8 cm fluid and gas containing cavity with thickened wall, which the radiologist considered dilated bowel-loop or cyst or diverticulum. A small amount of free fluid was present in the peritoneal cavity. The origin of small bowel obstruction remained still unclear (Figure 2).
Despite conservative treatment abdominal pain intensified. Therefore, an emergency laparotomy was opted for. Abdominal exploration revealed a small amount of haemorrhagical fluid in the peritoneal cavity and dilated small bowel loops. At approximately 50 cm from the ileo-caecal junction there was a necrotic Meckel’s diverticle, which was axially torsioned, with a size of 12 cm × 14 cm. The consequence of the torsion of Meckel’s diverticle was small bowel obstruction.
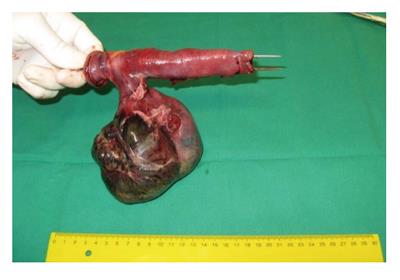
Approximately 20 cm of the small bowel with Meckel’s diverticle was resected. On a later examination, the mucosa of the diverticle was entirely necrotic, the diverticle was filled with hemorrhagic fluid (Figures 3 and 4). Postoperative recovery was uncomplicated and the patient was discharged on the fifth postoperative day.
Treatment of small bowel obstructions depends strongly on the etiology of obstruction and presence of intestinal strangulation. Therefore, quick correct diagnosis is highly important. Although Meckel’s diverticulum is a rare cause of small bowel obstruction, it should never be forgotten and once it is diagnosed surgical treatment is indicated.
Suspicion of Meckel’s diverticulum arises first of all in patients without common causes of small bowel obstruction, e.g., those without incarcerated hernias and previous abdominal surgery (low probability for adhesive obstruction). The preoperative diagnosis of almost all remaining causes of small bowel obstruction is difficult, especially with regard to complications of Meckel’s diverticulum, with only about 6% of cases being diagnosed correctly[18-20]. The most useful diagnostic tool is CT-scan[21,22], as can also be seen in the present report. Once the diagnosis of Meckel’s diverticulum as the cause of small bowel obstruction is made, surgical treatment is indicated. Delay in surgery carries a risk of intestinal necrosis and peritonitis.
A 41-year-old man with small-bowel obstruction.
Abdominal pain in the right mesogastrium, retention of gases, high-sounding peristalsis.
Tumor, adhesions.
Laboratory tests showed haemoconcentration, the biochemical values were all normal.
Abdominal computed tomography (CT)-scan showed markedly dilated small-bowel loops with multiple air-fluid levels. Oral contrast medium had reached the jejunum and the proximal ileum, but no contrast was noted distally. In the right mid-abdomen, subhepatically there was 11 cm × 6.4 cm × 7.8 cm dilated bowel-loop with a thickened wall containing fluid. A small amount of free fluid was present in the peritoneal cavity.
Mucosa of the diverticulum was entirely necrotic and the cavity was filled with hemorragic fluid.
Approximately 20 cm of the small bowel with Meckel’s diverticulum was resected.
This pathology has only been reported eleven times in English-language literature and they are named in the authors references.
In cases of small-bowel obstruction with unknown etiology, CT-scan is the most useful diagnostic tool detecting possible cause. Once the diagnosis of Meckel’s diverticulum as the cause of small bowel obstruction is made, surgical treatment is indicated. Delay in surgery carries a risk of intestinal necrosis and peritonitis.
The case report includes the description of symptoms and applied diagnostic and therapeutic procedures. The title of this paper appropriately reflects the purpose of the study.
| 1. | Chaudhuri TK, Christie JH. False positive Meckel’s diverticulum scan. Surgery. 1972;71:313. [PubMed] |
| 2. | Dalinka MK, Wunder JF. Meckel’s diverticulum and its complications, with emphasis on roentgenologic demonstration. Radiology. 1973;106:295-298. [PubMed] |
| 3. | Duszynski DO. Radionuclide imaging studies of gastrointestinal disorders. Semin Nucl Med. 1972;2:383-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Opitz JM, Schultka R, Göbbel L. Meckel on developmental pathology. Am J Med Genet A. 2006;140:115-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Skandalakis PN, Zoras O, Skandalakis JE, Mirilas P. Littre hernia: surgical anatomy, embryology, and technique of repair. Am Surg. 2006;72:238-243. [PubMed] |
| 6. | Sharma RK, Jain VK. Emergency surgery for Meckel’s diverticulum. World J Emerg Surg. 2008;3:27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 89] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 7. | Chan KW. Perforation of Meckel’s diverticulum caused by a chicken bone: a case report. J Med Case Rep. 2009;3:48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Smithy HG, Chamberlin JA. Persistence of the vitelline (omphalomesenteric) artery as a clinical problem. Surg Gynecol Obstet. 1946;82:579-585. [PubMed] |
| 9. | Rutherford RB, Akers DR. Meckel’s diverticulum: a review of 148 pediatric patients, with special reference to the pattern of bleeding and to mesodiverticular vascular bands. Surgery. 1966;59:618-626. [PubMed] |
| 10. | Malhotra S, Roth DA, Gouge TH, Hofstetter SR, Sidhu G, Newman E. Gangrene of Meckel’s diverticulum secondary to axial torsion: a rare complication. Am J Gastroenterol. 1998;93:1373-1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 32] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Eser M, Oncel M, Kurt N. Gangrene secondary to axial torsion in a patient with Meckel’s diverticulum. Int Surg. 2002;87:104-106. [PubMed] |
| 12. | Limas C, Seretis K, Soultanidis C, Anagnostoulis S. Axial torsion and gangrene of a giant Meckel’s diverticulum. J Gastrointestin Liver Dis. 2006;15:67-68. [PubMed] |
| 13. | Kiyak G, Ergul E, Sarikaya SM, Kusdemir A. Axial torsion and gangrene of a giant Meckel’s diverticulum mimicking acute appendicitis. J Pak Med Assoc. 2009;59:408-409. [PubMed] |
| 14. | Sharma RK, Jain VK, Kamboj S, Murari K. Gangrenous Meckel’s diverticulum causing acute intestinal obstruction in an adult. ANZ J Surg. 2008;78:1046-1047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Cartanese C, Petitti T, Marinelli E, Pignatelli A, Martignetti D, Zuccarino M, Ferrozzi L. Intestinal obstruction caused by torsed gangrenous Meckel’s diverticulum encircling terminal ileum. World J Gastrointest Surg. 2011;3:106-109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Ruiz LVA, Camacho OLA, Diaz TDA. Giant Meckel’s diverticula with necrosis due to axial torsion. Rev Col Gastroenterol. 2010;25:398-400. |
| 17. | Alvite Canosa M, Couselo Villanueva JM, Iglesias Porto E, González López R, Montoto Santomé P, Arija Val F. [Intestinal obstruction due to axial torsion and gangrene of a giant Meckel diverticulum]. Gastroenterol Hepatol. 2012;35:452-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Bani-Hani KE, Shatnawi NJ. Meckel’s diverticulum: comparison of incidental and symptomatic cases. World J Surg. 2004;28:917-920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 92] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 19. | Lüdtke FE, Mende V, Köhler H, Lepsien G. Incidence and frequency or complications and management of Meckel’s diverticulum. Surg Gynecol Obstet. 1989;169:537-542. [PubMed] |
| 20. | Rossi P, Gourtsoyiannis N, Bezzi M, Raptopoulos V, Massa R, Capanna G, Pedicini V, Coe M. Meckel’s diverticulum: imaging diagnosis. AJR Am J Roentgenol. 1996;166:567-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 79] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 21. | Prall RT, Bannon MP, Bharucha AE. Meckel’s diverticulum causing intestinal obstruction. Am J Gastroenterol. 2001;96:3426-3427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 35] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | Bennett GL, Birnbaum BA, Balthazar EJ. CT of Meckel’s diverticulitis in 11 patients. AJR Am J Roentgenol. 2004;182:625-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 60] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
P- Reviewer: Gurkan A, Katsoulis IE, Lorenzo-Zuniga V, Maric I S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ