Published online Sep 27, 2012. doi: 10.4240/wjgs.v4.i9.220
Revised: August 22, 2012
Accepted: September 17, 2012
Published online: September 27, 2012
A 64-year-old female patient presented with upper abdominal pain and vomiting. Ultrasonography showed a hyperechoic mass in the right lower abdomen and computed tomography showed a low-density mass with intestinal invagination. An emergency laparoscopic right-hemicolectomy was performed, and the resected specimen was found to contain three tumors, which were identified histopathologically as intestinal lipomas. Adult intussusception is relatively rare and difficult to be diagnosed, since most symptoms of adult intussusception are nonspecific. We report our clinical experience of the diagnosis and emergent laparoscopic surgery for an adult patient with intussusception.
- Citation: Hou YC, Lee PC, Chang JJ, Lai PS. Laparoscopic management of small-bowel intussusception in a 64-year-old female with ileoal lipomas. World J Gastrointest Surg 2012; 4(9): 220-222
- URL: https://www.wjgnet.com/1948-9366/full/v4/i9/220.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v4.i9.220
Ileal lipomas are relative uncommon benign tumors of the gastrointestinal tract. Most ileal lipomas are asymptomatic and need no treatment. Lipomas larger than 2 cm might cause symptoms, such as bleeding, diarrhea or constipation, intestinal obstruction, and intussusceptions, and might be a cause of surgical emergencies[1-3]. Intussusception of the bowel in adults is uncommon. Adults generally present with nonspecific findings of variable duration. Diagnosis is based on radiologic or surgical findings. Abdominal echo and computerized tomography (CT) results can diagnose intussusception in most case. Laparoscopic surgery has its benefits in reducing incision size, postoperative pain, risk of hernia, and recovery time. In this report, we present a case with giant ileal lipomas causing ileal -colonic intussusception leading to an emergent laparoscopic right hemicolectomy.
A 64-year-old female with a history of hypertension presented with sudden-onset upper abdominal pain that shifted to the right lower quadrant area with time. As the pain was progressive, the patient was sent to our emergency room 12 h later. She denied hunger pains, nausea, vomiting or diarrhea in recent days, and no radiation pain was noted. Physical examination showed no significant findings. The abdomen was soft and no palpated mass except diffused tenderness, more severe over right periumbilical area. The bowel sound was normoactive and blood tests showed leukocytosis with a white blood cell of 15 600 and a high C-reactive protein level. An abdominal plain X-ray showed no definite free gas and an air-fluid level was present over the left upper quadrant area, and under impression of ileus without a definite focus, we arranged further imaging study.
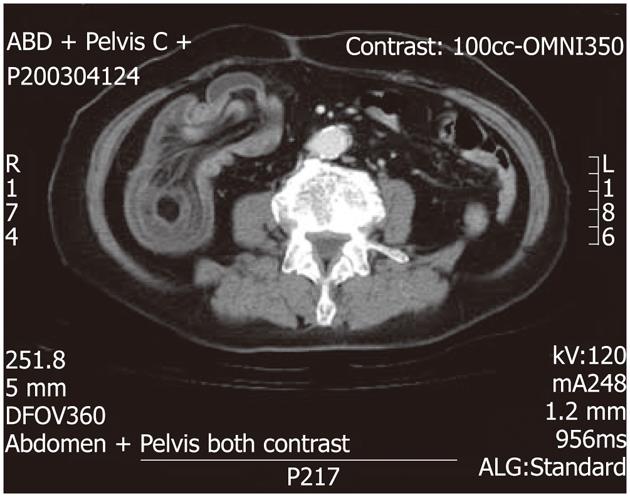
Ultrasound showed a prominent swelling of the intestinal wall with target signs and a hyperechoic mass of 67 mm × 60 mm in size over the right lower quadrant area (Figure 1), and abdominal CT showed right ileocolic intussusception of the terminal ileum into the ascending colon with thickening of the bowel wall (Figure 2). Under the impression of intestinal lipoma-induced intussusception with terminal ileum ischemic change, the patient underwent emergency surgery.
After the induction of general anesthesia, the patient was placed in a supine position. First, a skin incision was made above the umbilicus and a 12-mm trocar was inserted. Pneumoperitoneum was established by insufflation with carbon dioxide to an abdominal pressure of 15 mmHg. Under laparoscopic guidance, we then inserted three 5-mm trocars (left lower quadrant, right lower quadrant and right upper quadrant). Owing to necrotic change of the intussuscepted ileum, we decided to dissect it as a colon tumor rather than perform a reduction. Under laparoscopic viewing, the intestine was found to be dilated, and ileocolic vessel torsion was observed, rendering it difficult to start to divide the mesentery. Hence, we began with lateral to medial dissection. The peritoneal reflection of the right colon was divided using electrocautery and the duodenum was identified and reflected posteriorly. The gastrocolic ligament was divided with endo-ligasure and the hepatic flexure and ascending colon was taken down by lateral to medial approach with electrocautery, clipping the right colic vessels. After fully mobilizing the mesocolon, the ileocolic artery could be identified by turning the mesocolon upwards. We then ligated the vessels using a note pusher. At this point, the colon was readily movable. An extension incision was performed round the umbilicus port site of about 7 cm, through which the bowel was delivered.
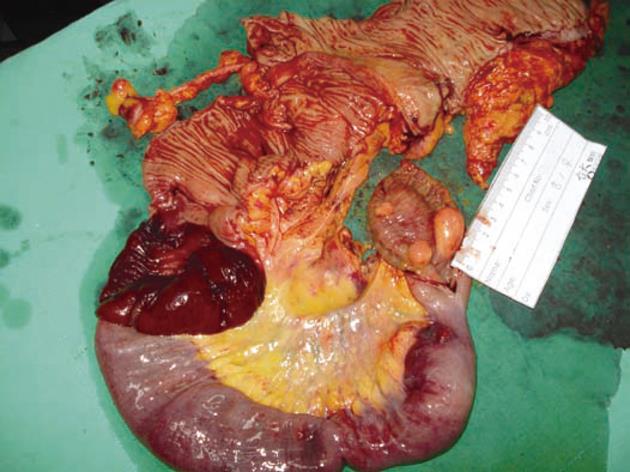
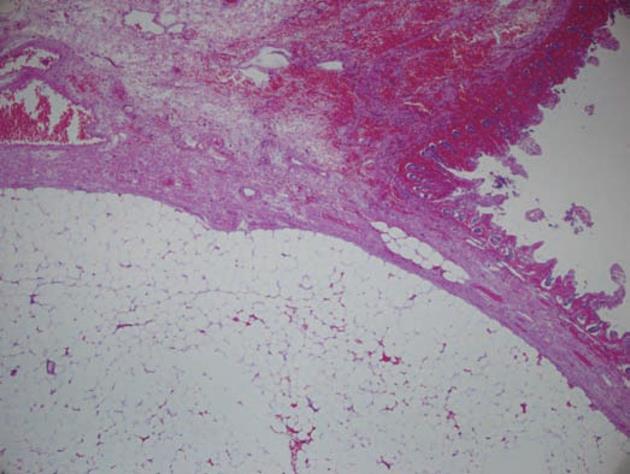
Approximately 10 cm of small intestine and another 30 cm ascending to include the intussusception tumor and intestine was resected, and an end-to-side ileocolostomy was created. The duration of the operation was 123 min. The macroscopic finding was intussusceptions with segmental ischemic change, secondary to multiple lipomas of ileum (Figure 3). The microscopic feature showed submucosal lipomas with focal mucosal necrosis (Figure 4). The patient had an uneventful recovery; she passed flatus on postoperative day (POD) 3, commenced oral fluids on POD 4, and was discharged on POD7.
In contrast to intussusception in pediatric patients, adult intussusception is relatively rare, accounting for only 5%-16% of all cases of intussusception[4]. Most symptoms of adult intussusception are nonspecific, unless bowel perforation or compromise occurs. The most common presenting symptoms of adult patients with intussusception are abdominal pain, vomiting, and bleeding[5]. The majority of adult intussusception in adult is due to an underlying lesion in the bowel lumen. Most intussusceptions arising in the small bowel are due to benign tumors, usually lipoma. Other causes of small bowel intussusception include malignant tumors, sarcoma, meckel’s diverticulum, chronic ulcer, adhesion, a hetrotopic pancreas, and foreign body[6].
A number of different techniques have been reported to be useful in the diagnosis of intussusception. Contrast barium enema study, which is used in the pediatric population, is rarely used in adults and is not utilized to reduce the intussusception. Abdominal sonography may reveal target signs and pseudo-kidney signs[7]. Several reports have suggested that abdominal CT is an useful radiologic method for diagnosing intestinal intussusception[5,8-10]. On computed tomography scan, lipomas appear ovoid with absorption densities of -40 to -120 Hounsfield units, typical of fatty composition[11]. In our case, abdominal sonography showed swelling of intestinal wall with target signs, and intussusception with gangrenous change was noted. Contrast barium enema study was not arranged owing to the risk of bowel perforation. CT showed ileocecal intussuception of the terminal ileum into the ascending colon with thickening of the bowel wall. There are some fat-density lesions in the lumen of terminal ileum, highly suspected terminal ileum lipoma induce intussusception.
Laparoscopy is valuable and is widely used in the diagnosis and management of abdominal emergencies[12-15]. There are various advantages of laparoscopic surgery, such as a shorter hospital stay, shorter duration of postoperative narcotics use, and a decreased interval until return of bowel function and oral intake, with consequent psychological, cosmetic, and economic benefits. However, emergency operations have been associated with a significantly high likelihood of morbidity and mortality[16]. Abdominal distension with ileus limits the use of laparoscopic colon resection surgery. In this patient, we performed a right hemicolectomy in preference to a segmental resection owing to an inability to preoperatively exclude the possibility of colonic malignancy. Because of the increased incidence of malignancy in colonic intussusception, several reports have suggested that this type of intussusception should be left unreduced and should be resected as a single mass[4,5,17]. In our case, with intussusceptions-induced small-bowel dilation and torsion of the ileocolic vessels, it was difficult to identify and dissect the ileocolic vessels. We attempted therefore to dissect the ascending colon by lateral to medial dissection rather than the traditional medial to lateral dissection. After mobilizing the ascending colon and pulling up the mesocolon of the ascending colon, the roots of the ileocolic vessels were easily identified and ligated.
In conclusion, laparoscopic surgery is beneficial for benign colon lesions such as lipomas even in some surgical emergency.
| 1. | Rogy MA, Mirza D, Berlakovich G, Winkelbauer F, Rauhs R. Submucous large-bowel lipomas--presentation and management. An 18-year study. Eur J Surg. 1991;157:51-55. [PubMed] |
| 2. | Pfeil SA, Weaver MG, Abdul-Karim FW, Yang P. Colonic lipomas: outcome of endoscopic removal. Gastrointest Endosc. 1990;36:435-438. [PubMed] |
| 3. | Vecchio R, Ferrara M, Mosca F, Ignoto A, Latteri F. Lipomas of the large bowel. Eur J Surg. 1996;162:915-919. [PubMed] |
| 4. | Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997;173:88-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 386] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 6. | Gordon RS, O'Dell KB, Namon AJ, Becker LB. Intussusception in the adult--a rare disease. J Emerg Med. 1991;9:337-342. [PubMed] |
| 7. | Sofia S, Casali A, Bolondi L. Sonographic diagnosis of adult intussusception. Abdom Imaging. 2001;26:483-486. [PubMed] |
| 8. | Wang LT, Wu CC, Yu JC, Hsiao CW, Hsu CC, Jao SW. Clinical entity and treatment strategies for adult intussusceptions: 20 years' experience. Dis Colon Rectum. 2007;50:1941-1949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 115] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 9. | Huang WS, Changchien CS, Lu SN. Adult intussusception: a 12-year experience, with emphasis on etiology and analysis of risk factors. Chang Gung Med J. 2000;23:284-290. [PubMed] |
| 10. | Takeuchi K, Tsuzuki Y, Ando T, Sekihara M, Hara T, Kori T, Kuwano H. The diagnosis and treatment of adult intussusception. J Clin Gastroenterol. 2003;36:18-21. [PubMed] |
| 11. | Heiken JP, Forde KA, Gold RP. Computed tomography as a definitive method for diagnosing gastrointestinal lipomas. Radiology. 1982;142:409-414. [PubMed] |
| 12. | Golash V, Willson PD. Early laparoscopy as a routine procedure in the management of acute abdominal pain: a review of 1,320 patients. Surg Endosc. 2005;19:882-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 77] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Agresta F, Ciardo LF, Mazzarolo G, Michelet I, Orsi G, Trentin G, Bedin N. Peritonitis: laparoscopic approach. World J Emerg Surg. 2006;1:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Ates M, Coban S, Sevil S, Terzi A. The efficacy of laparoscopic surgery in patients with peritonitis. Surg Laparosc Endosc Percutan Tech. 2008;18:453-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Favuzza J, Friel JC, Kelly JJ, Perugini R, Counihan TC. Benefits of laparoscopic peritoneal lavage for complicated sigmoid diverticulitis. Int J Colorectal Dis. 2009;24:797-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 50] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Paton BL, Mostafa G, Lincourt AE, Kercher KW, Heniford BT. Profile and significance of emergency colonic resections. Am Surg. 2008;74:305-309. [PubMed] |
| 17. | Barussaud M, Regenet N, Briennon X, de Kerviler B, Pessaux P, Kohneh-Sharhi N, Lehur PA, Hamy A, Leborgne J, le Neel JC. Clinical spectrum and surgical approach of adult intussusceptions: a multicentric study. Int J Colorectal Dis. 2006;21:834-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 171] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
Peer reviewers: Akira Tsunoda, MD, PhD, Professor, Department of Surgery, Kameda Medical Center 929 Higashi-cho, Kamogawa City, Chiba 296-8602, Japan; Yong-Song Guan, MD, PhD, Professor, Department of Oncology and Radiology, State Key Laboratory of Biotherapy, West China Hospital of Sichuan University, Chengdu 610041, Sichuan Province, China
S- Editor Wen LL L- Editor A E- Editor Xiong L