INTRODUCTION
Intraductal papillary mucinous neoplasms (IPMN) are mucin producing cystic neoplasms of the pancreas first recognized by the World Health Organization in 1996[1]. Dysplasia within these lesions is categorized as low grade, moderate grade and high grade[2]. Associated invasive carcinoma may be identified in 40%-60% of resected IPMN lesions with estimated five-year survival rates following complete resection approaching 40% in most reported series[3-5]. Estimated five-year survival rates are over 90% in non-invasive resected IPMN lesions[2,3].
Long-term survival following complete surgical resection for conventional pancreatic ductal adenocarcinoma is historically poor with five-year survival rates ranging from 10%-20%[6,7]. Traditionally, patients with resected invasive IPMN are presumed to have a more favorable prognosis than patients resected for conventional pancreatic ductal adenocarcinoma[3,4]. Until recently, a paucity of patients and a lack of detailed histological subtype analysis have prevented a valid comparison of prognosis between patients with pancreatic adenocarcinoma arising in the setting of IPMN and conventional pancreatic ductal adenocarcinoma (unpublished data).
This article describes the current understating of outcomes following resection of pancreatic adenocarcinoma arising in the setting of IPMN and compares this to the reported survival outcomes of resected conventional adenocarcinoma. Survival following resection of invasive IPMN has been shown to be strongly influenced by histological subtype (colloid carcinoma and tubular carcinoma) and the differences between these two entities are highlighted.
PROGNOSIS BY CLINICOPATHOLOGICAL SUBTYPE
Two distinct histopathological subtypes of invasive IPMN have been described, colloid carcinoma and tubular carcinoma[8]. Tubular carcinoma arising in association with IPMN is similar in histological appearance to conventional pancreatic ductal adenocarcinoma with neoplastic cells arranged in small, tubular glands with associated desmoplastic invasion[8]. Colloid carcinoma arising in association with IPMN is characterized by an abundance of acellular matrix. By definition, colloid carcinoma has greater than 80% of the invasive component composed of extensive stromal pools of acellular matrix lined by or containing floating neoplastic epithelial cells[8].
Invasive colloid and tubular carcinoma present as two distinct histological entities and are presumed to arise from histologically distinct IPMN precursor lesions. Colloid carcinoma is generally identified in association with intestinal-type IPMN and tubular carcinoma is generally found in association with pancreatobiliary IPMN[9].
Immunohistochemical studies have identified differences in the expression of the glycoproteins, MUC1, MUC2 and CDX2, between invasive colloid and tubular carcinoma IPMN, further suggesting that these entities are distinct from a molecular standpoint[10-12]. Colloid carcinoma associated with IPMN generally expresses both MUC2 and CDX2, markers of intestinal differentiation, a characteristic of more indolent carcinomas[13]. Tubular carcinoma associated with IPMN generally expresses MUC1, which is also generally expressed in conventional pancreatic ductal adenocarcinoma, but not MUC2 or CDX2[12-14]. Together these data suggest that colloid carcinoma arising in association with IPMN should be considered as a separate biological entity from tubular carcinoma associated with IPMN.
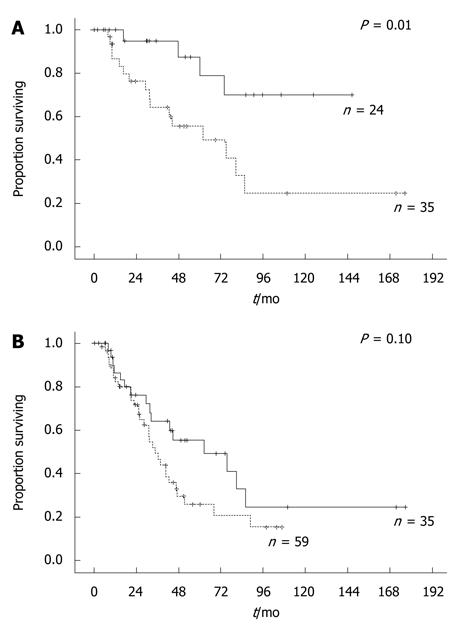
The characterization of invasive IPMN by histological subtype is also clinically relevant as patients with resected colloid and tubular carcinoma have significantly different disease-specific outcome. Multiple series have reported a more favorable outcome for colloid carcinoma compared to the tubular carcinoma subtype. Estimated five-year survival rates following resection of colloid carcinoma range from 57%-83% and estimated five-year survival following resection of tubular carcinoma range from 24%-55%[15-17]. In a previous report from the Memorial Sloan Kettering Cancer Center (MSKCC) the tubular carcinoma subtype had a worse prognosis and was associated with malignant regional lymph nodes and a disseminated recurrence pattern[4]. This initial series has been recently updated (data not published) and in this larger series of patients multivariate analysis identified the tubular carcinoma subtype and the presence of malignant regional lymph nodes to be the only factors predictive of decreased survival following resection of invasive IPMN (unpublished data). Figure 1A illustrates the association between histopathological subtype and survival. The five-year estimated survival rates for tubular carcinoma and colloid carcinoma were 55% and 87% (P = 0.01), respectively.
Figure 1 Kaplan-Meier estimated overall survival curves.
A: Kaplan-Meier estimated overall survival curves of invasive colloid IPMN (soild line) and invasive tubular IPMN (dotted line); B: Kaplan-Meier estimated overall survival curves of invasive tubular IPMN (soild line) and conventional pancreatic ductal adenocarcinoma (dotted line).
The difference in disease-specific survival outcome between invasive colloid and tubular IPMN appears to be a function of disease biology, as patients with the tubular subtype tend to have larger tumors with a propensity for metastasis to regional lymph nodes. These prognostic factors should be considered in the decision-making process regarding adjuvant therapy following resection of invasive IPMN, although because of the relative rarity of these lesions no prospective data exist to assist in the decision regarding adjuvant therapy. In the updated MSKCC series noted above we favored the use of chemotherapy for patients with poor prognostic factors including malignant regional lymph nodes or tumor recurrence.
It is unclear if all patients with the tubular subtype should be considered for adjuvant chemotherapy, as there is clearly a subset of these patients that have a favorable disease biology and experience long-term survival. Patients with a tubular subtype, tumor size less than 1 cm and an absence of spread to regional lymph nodes experienced a three-year survival rate approaching 85%, nearly identical to the colloid carcinoma subtype. The role of adjuvant therapy in these patients is even more controversial than in the large node positive tubular lesions. Future studies with cohorts of patients characterized by histological subtype and prognostic factors will provide important recurrence and survival information to clarify the role of adjuvant radiotherapy and chemotherapy in resected invasive IPMN.
PREDICTORS OF INVASIVE INTRADUCTAL PAPILLARY MUCINOUS NEOPLASMS AND HISTOLOGICAL SUBTYPE
Several studies have described preoperative predictors of invasive carcinoma associated with IPMN, including the presence of mural nodules, tumor size > 3.5 cm, solid component and a significantly dilated pancreatic duct (> 10 mm) [18,19]. However, current imaging techniques lack sufficient sensitivity and radiological features to adequately distinguish between histological subtypes and future studies are needed to better define preoperative predictors of subtype. Routine laboratory values including serum CEA and CA19-9 also currently lack the sensitivity necessary to serve as a predictive biomarker of histological subtype. Recently we have shown that serum and pancreatic cyst fluid mucin levels are predictive of dysplasia in resected IPMN specimens[20]. Currently there is no role for tumor biopsy for histological subtyping of suspected IPMNs which could act as an aid to guide pre-operative management decisions.
COMPARISON TO CONVENTIONAL PANCREATIC DUCTAL ADENOCARCINOMA
Historically, reports have suggested improved outcomes for patients with resected invasive IPMN compared to patients who have undergone resection for conventional pancreatic ductal adenocarcinoma. Sohn et al[15] demonstrated that patients resected for invasive carcinoma in association with IPMN had a more favorable prognosis than patients resected for conventional pancreatic ductal adenocarcinoma. Estimated five-year survival following resection of invasive IPMN was 62% while the estimated five-year survival following resection of conventional pancreatic ductal adenocarcinoma was 19%[15]. This initial report however failed to stratify the invasive IPMN group by histological subtype. An updated series by Sohn et al[3] demonstrated that colloid carcinoma had a more favorable prognosis than tubular carcinoma although no comparison to conventional pancreatic ductal adenocarcinoma was carried out. This series, as well as an additional large series from MSKCC were limited with respect to duration of patient follow-up, overall patient numbers and a lack of a matched analysis[21-24]. The lack of stratification into the tubular and colloid histological subtypes may explain the general belief that invasive IPMN carries a more favorable prognosis than conventional pancreatic ductal adenocarcinoma. When stratification by histopathological subtype has been performed, the outcome of the tubular subtype has been generally similar to what is expected for conventional pancreatic ductal adenocarcinoma while the colloid subtype appears to have a significantly better prognosis[4].
The most recent update of the MSKCC experience with invasive IPMN sought to perform a carefully matched comparison of post-resection outcome in patients resected for conventional pancreatic ductal adenocarcinoma and invasive IPMN. Patients with invasive IPMN were matched to patients with conventional pancreatic adenocarcinoma through the use of a post-resection pancreatic adenocarcinoma nomogram developed by Brennan et al[25]. This validated nomogram predicts outcome more accurately than tumor stage and allows matching of relevant clinicopathological variables such as tumor size and nodal status through the use of an overall nomogram score. We prefer this approach because of the difficulty in matching T-stage within the IPMN group. AJCC guidelines currently define a pT1 tumor as being between 0.1 to 2.0 cm diameter[21-24]. Therefore a patient with a 0.1 cm invasive IPMN could be compared to a 2.0 cm conventional pancreatic ductal adenocarcinoma despite evidence suggesting that tumor size is a strong predictor of regional lymph node status and overall survival. Given the proportion of patients who present with a < 1 cm focus of invasive IPMN, matching to this variable alone may favor the IPMN group.
The results of this matched analysis demonstrated that the colloid carcinoma subtype had a favorable prognosis compared to conventional pancreatic ductal adenocarcinoma. The estimated five-year survival outcomes for colloid carcinoma and ductal adenocarcinoma were 87% and 23% (P = 0.01) respectively. There was no difference in overall survival between the tubular subtype and ductal adenocarcinoma groups (Figure 1B). However, when these groups were stratified by regional lymph node status patients with negative regional lymph nodes and the tubular subtype experienced significantly better survival than patients with a similar nodal status and ductal adenocarcinoma, with estimated five-year survival rates of 73% and 27% (P = 0.01) respectively. Patients with positive regional lymph nodes had a similar outcome whether they had a tubular subtype or ductal adenocarcinoma. Regional lymph node status appears to be a surrogate marker of disease biology of invasive tubular IPMN.
CONCLUSION
The prognosis of invasive IPMN is strongly correlated to the histological subtype with favorable survival in patients with colloid carcinoma. Patients with resected invasive tubular IPMN should, on the whole, be expected to have a similar outcome as conventional pancreatic ductal adenocarcinoma, although patients with small, node negative lesions are likely to experience greater long-term survival. Although the role of adjuvant chemotherapy remains undefined these prognostic factors should be considered in the decision-making process.
Peer reviewer: Yong-Song Guan, MD, PhD, Professor, Department of Oncology and Radiology, State Key Laboratory of Biotherapy, West China Hospital of Sichuan University, Chengdu 610041, Sichuan Province, China
S- Editor Wang JL L- Editor Hughes D E- Editor Ma WH