Published online Jul 27, 2025. doi: 10.4240/wjgs.v17.i7.106712
Revised: April 17, 2025
Accepted: May 20, 2025
Published online: July 27, 2025
Processing time: 140 Days and 19.2 Hours
Choledocholithiasis is a common benign disease of the biliary tract. We identified a particular type of choledocholithiasis characterized by sudden narrowing of the common bile duct at the site of impaction, which caused a marked increase in surgical difficulty and risk compared to treatment for typical choledocholithiasis. This phenomenon has not been described in previous studies.
To propose the ice-breaking sign and evaluate its influence on treatment strategies for choledocholithiasis.
Using a retrospective case-control study design, patients who were diagnosed with common bile duct stones and admitted to the Emergency Department of Peking University Third Hospital between January 2018 and December 2023 were included. Propensity score matching was used to match cases and controls. Univariate analysis was conducted to assess the differences in clinical data between the two groups of patients.
There were no significant differences in the baseline data between the two groups, except for higher incidence of jaundice, alkaline phosphatase and total bilirubin in the ice-breaking sign group. Compared to the control group, the ice-breaking sign group had lower success rates for endoscopic retrograde cholangiopancreatography (25.0% vs 81.8%, P = 0.006) and laparoscopic common bile duct exploration (69.4% vs 93.8%, P = 0.007), longer operation time (148.04 ± 60.55 minutes vs 106.15 ± 35.21 minutes, P = 0.001), higher likelihood of T-tube placement (62.2% vs 31.3%, P = 0.016) and using lithotripsy techniques during surgery (29.7% vs 0%, P = 0.001), more intraoperative bleeding [25.0 (20.0-50.0) mL vs 10.0 (10.0-20.0) mL, P < 0.001] and longer postoperative hospital stay [6.50 (5.0-9.0) days vs 5.50 (3.0-6.50) days, P = 0.002]. The ice-breaking sign group showed significantly more dilatation in the proximal than distal bile duct.
The ice-breaking sign, a newly identified radiological phenomenon, may influence therapeutic decisions in choledocholithiasis, suggesting laparoscopic common bile duct exploration as the preferred approach over endoscopic retrograde cholangiopancreatography in patients exhibiting this sign.
Core Tip: This study identified the ice-breaking sign, a novel radiological marker on magnetic resonance cholangiopancreatography, characterized by abrupt distal common bile duct narrowing with proximal dilation in choledocholithiasis. Patients with this sign exhibited markedly lower success rates for endoscopic retrograde cholangiopancreatography (25.0% vs 81.8%) and laparoscopic common bile duct exploration (69.4% vs 93.8%), necessitating advanced techniques like lithotripsy. The sign indicates higher surgical complexity and underscores laparoscopic common bile duct exploration as the preferred approach over endoscopic retrograde cholangiopancreatography. Preoperative recognition aids in risk stratification, optimizing treatment strategies for challenging bile duct stones.
- Citation: Zhao XY, Chen M, Wang G, Cui L, Xu Z, Hou CS, Wang LX, Zhang LF, Ling XF. Ice-breaking sign: A radiological sign influencing the treatment strategies for choledocholithiasis. World J Gastrointest Surg 2025; 17(7): 106712
- URL: https://www.wjgnet.com/1948-9366/full/v17/i7/106712.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i7.106712
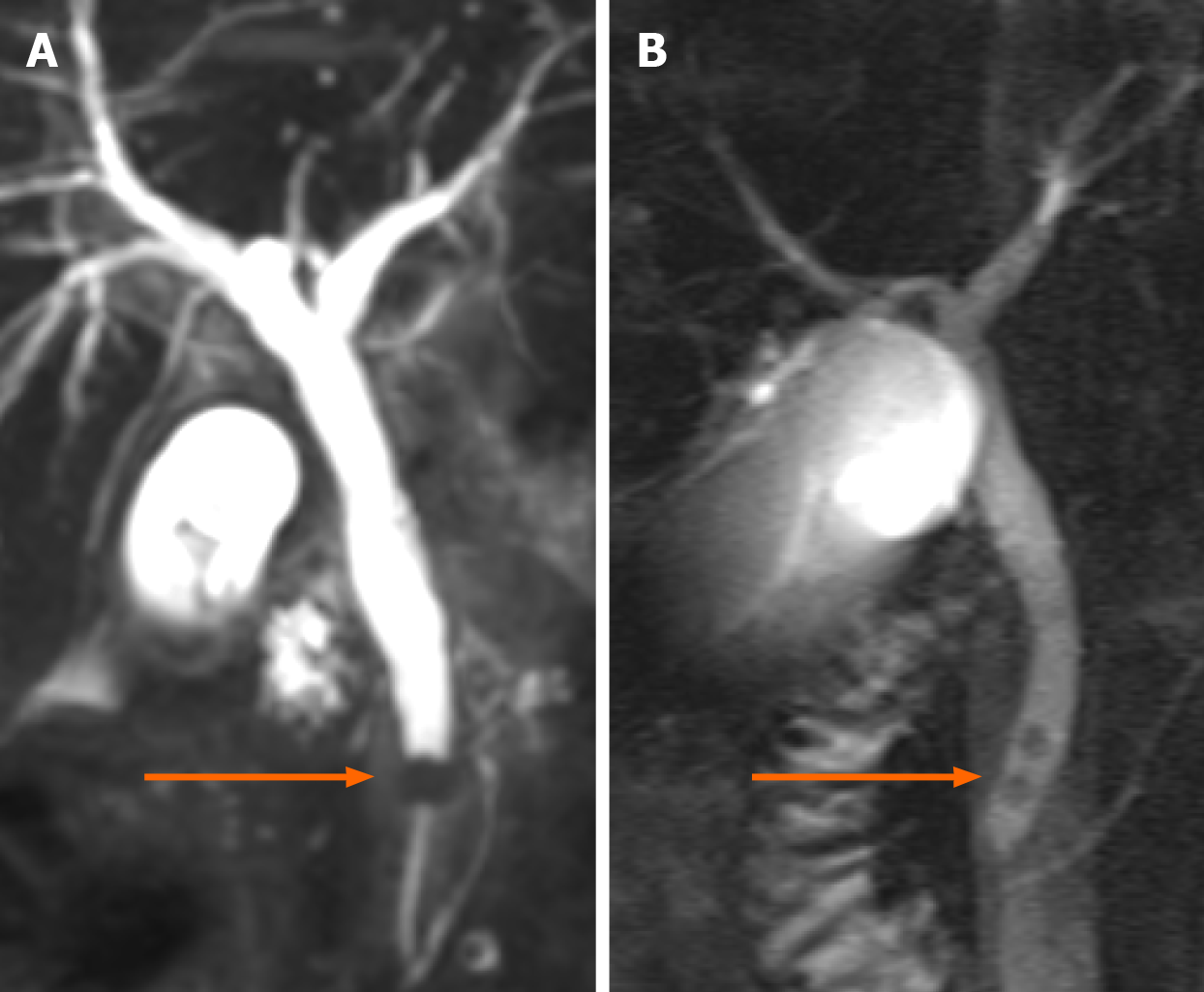
Choledocholithiasis is one of the most common benign diseases of the biliary system. Although it is a benign disease, choledocholithiasis often coexists with cholangitis and is prone to complications such as biliary pancreatitis, obstructive jaundice and liver dysfunction. Once diagnosed, regardless of symptoms, prompt treatment with choledocholithotomy should be performed[1]. Currently, the main treatment modalities for choledocholithiasis are endoscopic retrograde cholangiopancreatography (ERCP) and laparoscopic common bile duct exploration (LCBDE), and a consensus on the priority of these two treatment methods has not yet been reached[1,2]. However, for some choledocholithiasis patients, the failure rate of ERCP is significantly higher than that of LCBDE. Some studies have proposed the concept of difficult bile duct stones[3], which are defined as large stones (> 15 mm), multiple stones (> 3), intrahepatic bile duct stones, or obstructive common bile duct stones. For these difficult common bile duct stones, LCBDE may be a more suitable treatment method[4], and auxiliary lithotripsy may be required[5]. In clinical practice at our center, we identified a specific type of common bile duct stone characterized by impaction obstruction, upstream dilatation of the obstructed bile duct, downstream narrowing or complete closure, and abrupt narrowing of the bile duct. Because this phenomenon resembles a ship breaking ice, we have named it the ice-breaking sign (Figure 1). This sign is particularly evident on three-dimensional (3D) reconstructions of magnetic resonance cholangiopancreatography (MRCP) images. Based on our subjective experience in treating such patients at this center, the treatment outcomes differ from those of patients with general bile duct stones. The success rate of ERCP is lower, and the retrieval of stones using a stone extraction basket during LCBDE is also challenging. Often, lithotripsy by stone extraction basket, biopsy forceps, or biliary electrohydraulic techniques are required to remove the stones, which increases the risk of downstream bile duct injury. Due to the strong guiding significance of this phenomenon in the treatment of common bile duct stones, this study summarizes some typical cases from this center to specifically describe this sign and explore its clinical implications.
The Ethics Committee of Peking University Third Hospital approved this study (IRB00006761-M2022592) and waived the requirement for informed consent. In the Department of Emergency, for patients who present with symptoms such as abdominal pain, jaundice, and fever and who are highly suspected of having common bile duct stones, routine MRCP is performed. Once the diagnosis of common bile duct stones is confirmed, patients should be advised to undergo common bile duct stone extraction as soon as possible unless there are severe surgical contraindications. This study included patients who were admitted to the Emergency Department of Peking University Third Hospital between January 2018 and December 2023 and who were diagnosed with common bile duct stones. The inclusion criteria were as follows: (1) LCBDE or ERCP; and (2) Common bile duct stones confirmed during the procedure. Patients with missing preoperative MRCP information, intrahepatic bile duct stones, or who underwent conversion to other surgical methods were excluded.
The ice-breaking sign was identified as a sudden narrowing of the distal common bile duct on 3D reconstructed MRCP images. A biliary surgeon (Zhao XY) and a radiologist (Chen M) independently assessed the MRCP images of all patients to determine the presence of the ice-breaking sign. In cases of disagreement between the two evaluators, a senior biliary surgeon (Ling XF) conducted a discussion with both doctors to reach a consensus. Prior to the evaluation, all three doctors underwent brief training and were blinded to patient information during the assessment process. For patients who underwent ERCP, a duodenoscope was inserted under general anesthesia into the descending part of the duodenum through the mouth, esophagus, gastric cardia and pylorus. The duodenal papilla was found and selectively intubated until reaching the common bile duct under the guidance of a guide wire. The contrast agent was injected through the incision knife for ERCP. For patients whose stones could be removed through the duodenal papilla, endoscopic sphincterotomy was performed using the knife-retraction method along the 11 o’clock direction of the duodenal papilla, and papillary balloon dilation was conducted as needed. According to the location, size, number and hardness of the stones, the appropriate methods for lithotomy and lithotripsy were selected. After lithotomy, the presence or absence of residual stones was confirmed using cholangiography, and if there were residual stones, duodenoscopic lithotomy was performed again. After endoscopic lithotomy, a nasobiliary drainage tube was inserted for bile duct irrigation and bile drainage. After the operation, the patients’ blood, urine amylase and clinical signs were closely monitored. One to two days after ERCP, the nasobiliary drainage tube was withdrawn if no abnormalities were detected via naso-cholangiography. ERCP success was defined as the complete removal of common bile duct stones during a single procedure, with no residual stones seen on postoperative cholangiography[6,7].
Patients who underwent LCBDE underwent laparoscopic cholecystectomy under general anesthesia. The common bile duct was confirmed through puncture and bile removal. A longitudinal incision (approximately 1 cm long) was made on the anterior wall of the common bile duct near its mid-upper end, the internal and external bile ducts were explored using a choledochoscope, and the stones in the common bile duct were removed using a stone basket. After it was confirmed by choledochoscopy that there were no residual stones in the intrahepatic bile duct or common bile duct and that the stone basket could smoothly pass through the duodenal papilla, the anterior wall of the common bile duct was subjected to phase I continuous full-thickness suturing using absorbable surgical sutures. After the operation, the patients’ blood, urine amylase, clinical signs and peritoneal drainage were closely monitored. On the next day, the patients could eat food. LCBDE success was defined as the complete clearance of common bile duct stones under full laparoscopic visualization without conversion to open surgery intraoperatively, and postoperative cholangiography showing no residual stones in the common bile duct[8,9].
The data required for the research were collected by a resident physician specializing in hepatobiliary surgery. All collected and entered information was sourced from the electronic medical records system of Peking University Third Hospital. If available, the following information was collected from the patient’s medical records: Age, sex, height, weight, clinical manifestations, laboratory tests, imaging examinations and surgery-related data. Clinical manifestations included abdominal pain, fever, jaundice, history of biliary disease and history of biliary surgery. Laboratory tests included blood cell count, percentage of neutrophils, prothrombin activity, transaminases, bilirubin, amylase, g-glutamyl transferase, blood urea nitrogen and creatinine. Imaging studies included percentage of distal and proximal bile duct narrowing, intrahepatic bile duct dilatation, diameter of the distal and proximal bile ducts, stone diameter, and presence of the gallbladder. The proximal end of the bile duct was located close to the porta hepatis, and the distal end close to the duodenal papilla, with measurements of the proximal and distal bile duct diameters taken 2 mm from the impacted stone. Surgery-related data included success rates of ERCP and LCBDE, operation time, surgical bleeding, status of T-tube placement, number of auxiliary stones, total length of hospital stay, and length of postoperative hospital stay. Postoperative complications included bile leakage, bleeding, residual stones and pancreatitis, and were graded according to the Clavien-Dindo classification system. All the data are stored in a dedicated database.
MRCP was performed using a 1.5 T clinical magnetic resonance imaging system (Signa, GE Medical Systems, Milwaukee, WI, United States) and phased-array surface coil. Conventional sequences, such as 2D axial T1-weighted images [repetition time (TR)/echo time (TE) 180-220/4.7 milliseconds], 2D axial T2-weighted images (TR/TE 6000-10000/85 milliseconds) and coronal fast imaging using steady-state acquisition sequences (TR/TE 4.7/1.5 milliseconds), were obtained with a slice thickness of 6 mm, intersection overlap of 1 mm, and field of view (FOV) of 34-38 mm. 3D-MRCP was performed using fast recovery fast spin echo in the coronal plane. The parameters were as follows: TR/TE 4000-7500/730-1000 milliseconds, slice thickness 1.6 mm, no gap between sections, matrix 288 × 256, and field of view 20-40 mm. Fat saturation was used to suppress interference from the surrounding fat tissues. The T2-weighted images were obtained with the patients in a free breathing state, and the other images were obtained with the patients holding their breath to reduce the artifacts created by respiratory motion.
Statistical analysis was conducted using SPSS 26.0 software. Propensity score matching was used to match the patients in the case group with those in the control group based on age and sex. Continuous variables are presented as the mean ± SD if they were normally distributed; otherwise, they are presented as the median and interquartile range. Categorical variables are presented as patient counts and percentages. All clinical and imaging data were compared between patients with and without ice-breaking signs. Student’s t test was used to compare normally distributed continuous variables, while the Mann-Whitney U test was used for nonnormally distributed variables. Pearson’s χ2 test or Fisher’s exact test was used to compare categorical variables. A two-tailed P < 0.05 was considered to indicate statistical significance.
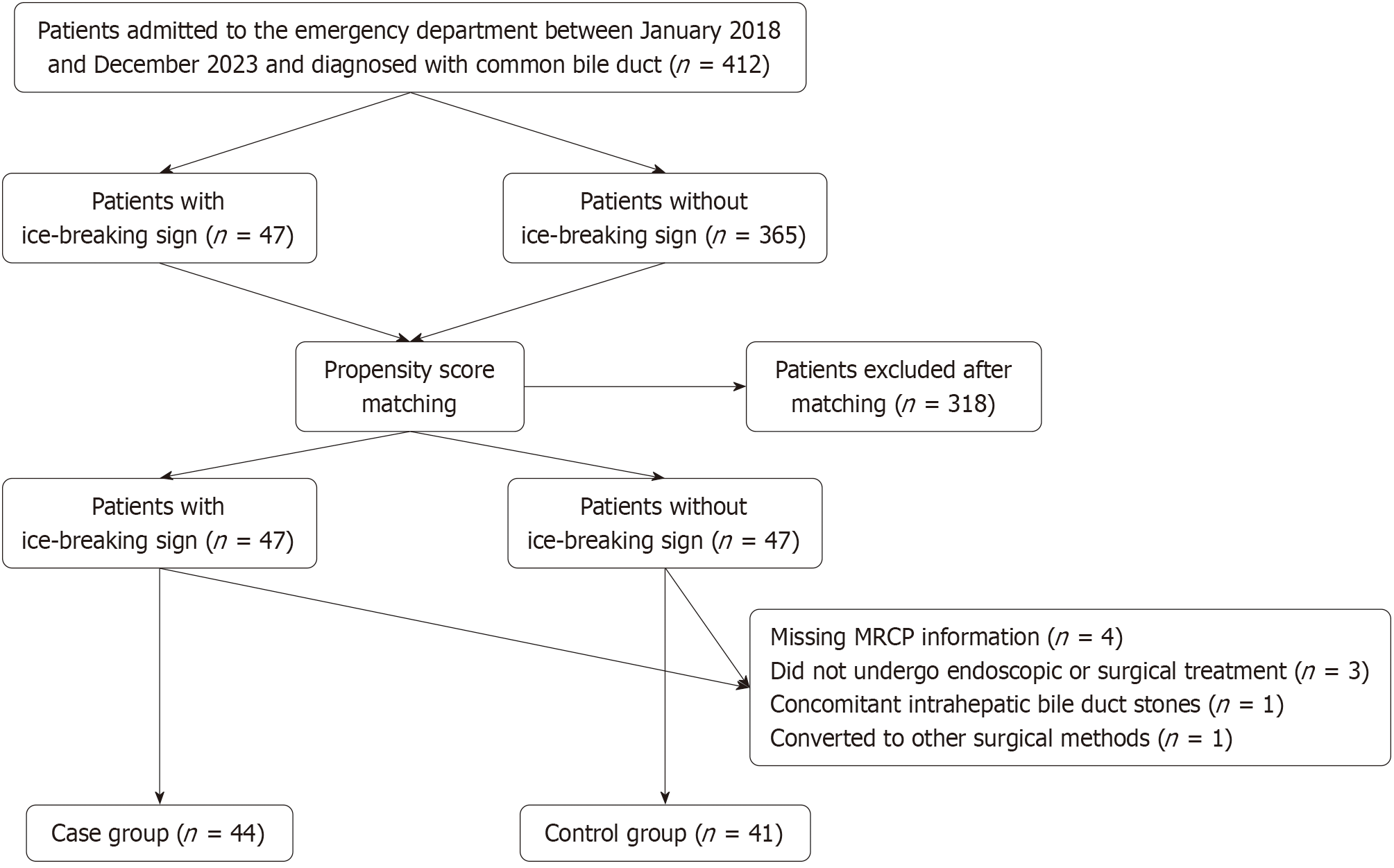
This study initially included 411 patients with common bile duct stones, among whom, 47 presented with ice-breaking signs on imaging and formed the case group; the remaining 365 patients were included in the control group. Due to the significant difference in the number of patients between the two groups and considering that age[8] and sex[9] may have a significant impact on the success rate of surgery, a propensity score matching method was used to match the patients in the two groups at a 1:1 ratio based on sex and age. After matching, there were 47 patients in both the case and control groups, resulting in a total of 94 patients whose case data were collected and entered. During the data entry process, one patient was found to no longer exhibit the ice-breaking sign upon re-evaluation. In addition, one patient with missing MRCP information and one who was diagnosed with a common bile duct cyst during exploration were excluded from the case group, while three patients with missing MRCP information, three patients who did not undergo endoscopic or surgical treatment, and one patient with concomitant intrahepatic bile duct stones were excluded from the control group (Figure 2). A total of 85 patients were included in the final statistical analysis, with 44 in the case group and 41 in the control group.
There were no significant differences in the baseline data between the case and control groups (Table 1). Regarding clinical manifestations, among the six indicators included in this study, there was only a significant difference in the incidence of jaundice (P = 0.017) - the incidence was higher in the biliary sepsis group than in the control group. The incidence of the remaining five indicators was not significantly different (Table 2). In terms of laboratory indicators, the levels of alkaline phosphatase and total bilirubin in the biliary sepsis group were significantly higher than in the control group (P = 0.007 and P = 0.025), and there were also significant differences in the amylase levels between the two groups
| Baseline date | Control group | Case group | P value | |
| Age (years) | 45.0 (29.50-64.0) | 47.0 (35.0-58.0) | 0.689 | |
| Sex, n (%) | Male | 30 (73.2) | 33 (75.0) | 1.000 |
| Female | 11 (26.8) | 11(25.0) | ||
| Height (cm) | 170.0 (159.50-176.0) | 171.0 (165.0-176.0) | 0.178 | |
| Weight (kg), mean ± SD | 68.60 ± 12.76 | 71.35 ± 18.89 | 0.533 | |
| BMI (kg/m2) | 24.77 (23.04-25.81) | 24.68 (22.22-26.81) | 0.874 | |
| Clinical manifestations | Classifications | Control group | Case group | P value |
| Abdominal pain | Yes | 38 (92.7) | 41 (93.2) | 1.000 |
| No | 3 (7.3) | 3 (6.8) | ||
| Fever | Yes | 11 (26.8) | 12 (27.3) | 1.000 |
| No | 30 (73.2) | 32 (72.7) | ||
| Jaundice | Yes | 17 (41.5) | 30 (68.2) | 0.017 |
| No | 24 (58.5) | 14 (31.8) | ||
| History of biliary tract disease | Yes | 18 (43.9) | 20 (45.5) | 1.000 |
| No | 23 (56.1) | 24 (54.5) | ||
| History of biliary surgery | Yes | 7 (17.1) | 9 (20.5) | 0.785 |
| No | 34 (82.9) | 35 (79.5) |
| Laboratory indicators | Control group | Case group | P value |
| RBC (× 1012/L) | 4.66 ± 0.48 | 4.70 ± 0.72 | 0.859 |
| Hb (g/L) | 139.75 ± 17.97 | 137.58 ± 24.0 | 0.127 |
| WBC (× 109/L) | 7.99 (7.17-11.55) | 7.19 (5.89-10.71) | 0.075 |
| PLT (× 109/L) | 228.0 (203.50-269.0) | 223.0 (175.0-249.0) | 0.926 |
| N% | 79.08 ± 12.05 | 79.90 ± 11.08 | 0.716 |
| N (× 109/L) | 6.66 (4.86-10.06) | 5.95 (4.35-5.95) | 0.115 |
| INR | 1.13 (1.05-1.18) | 1.18 (1.09-1.22) | 0.062 |
| ALT (U/L) | 242.0 (134.0-434.0) | 260.50 (162.0-525.0) | 0.316 |
| AST (U/L) | 185.50 (74.0-387.0) | 114.50 (61.0-515.0) | 0.656 |
| ALP (U/L) | 181.0 (123.0-220.0) | 182.0 (138.0-316.0) | 0.007 |
| TBIL (μmol/L) | 60.95 (44.15-124.85) | 112.35 (52.70-154.30) | 0.025 |
| TP (g/L) | 78.43 ± 7.48 | 75.64 ± 9.83 | 0.957 |
| ALB (g/L) | 43.57 ± 4.96 | 40.99 ± 6.71 | 0.174 |
| GGT (U/L) | 440.50 (263.0-557.0) | 357.0 (263.0-442.0) | 0.180 |
| CR (μmol/L) | 66.50 (53.50-87.50) | 62.0 (55.00 -80.0) | 0.526 |
| BUN (mmol/L) | 4.00 (2.65-5.25) | 3.06 (2.52-4.41) | 0.181 |
| UA (μmol/L) | 300.50 (236.5-381.5) | 254.0 (170.0-349.0) | 0.071 |
| AMY (U/L) | 126.0 (87.50-772.50) | 68.50 (55.0-82.0) | < 0.001 |
| Surgery-related information | Classifications | Control group | Case group | P value |
| ERCP success rate | Success | 9 (81.8) | 4 (25.0) | 0.006 |
| Fail | 2 (18.2) | 12 (75.0) | ||
| LCBDE success rate | Success | 30 (93.8) | 24 (69.4) | 0.007 |
| Fail | 2 (6.3) | 13 (35.1) | ||
| Duration of surgery (minutes), mean ± SD | - | 106.15 ± 35.21 | 148.04 ± 60.55 | 0.001 |
| Surgical bleeding (mL) | - | 10.0 (10.0-20.0) | 25.0 (20.0-50.0) | < 0.001 |
| T tube | Yes | 10 (31.3) | 23 (62.2) | 0.016 |
| No | 22 (68.8) | 14 (37.8) | ||
| Lithotripsy techniques | Yes | 0 | 11(29.7) | 0.001 |
| No | 32 (100) | 26 (70.3) | ||
| Length of hospital stay (days) | - | 8.0 (6.0-11.50) | 8.50 (7.0-12.0) | 0.302 |
| Length of postoperative hospital stay (days) | - | 5.50 (3.0-6.50) | 6.50 (5.0-9.0) | 0.002 |
The MRCP imaging features of the two groups of patients were summarized. The percentage of narrowing the proximal and distal bile ducts in the ice-breaking sign group was significantly more than that in the control group (P < 0.001). According to the other imaging indicators, the breaking-ice sign group had a wider proximal bile duct (P < 0.001), narrower distal bile duct (P < 0.001), and larger stones (P = 0.002). There was no significant difference between the two groups in terms of intrahepatic bile duct dilation or the presence of a gallbladder (Table 5).
| Radiological indices | Classifications | Control group | Case group | P value |
| Percentage of narrowing of the proximal and distal bile duct | - | 0% (0.0-20.54) | 72.08% (62.50-77.78) | < 0.001 |
| Intrahepatic bile duct dilation | Yes | 37 (90.2) | 43 (97.7) | 0.192 |
| No | 4 (9.8) | 1 (2.3) | ||
| Proximal bile duct diameter (mm) | - | 7.95 ± 2.76 | 11.65 ± 2.83 | < 0.001 |
| Distal bile duct diameter (mm) | - | 9.0 (6.50-10.50) | 3.0 (2.0-4.0) | < 0.001 |
| Presence of a gallbladder | Yes | 36 (87.8) | 41 (93.2) | 0.474 |
| No | 5 (12.2) | 3 (6.8) | ||
| Stone diameter (mm) | - | 7.50 (6.0-8.0) | 8.0 (6.0-10.0) | 0.002 |
Patients with the ice-breaking sign have a significantly higher incidence of jaundice than those without the sign, suggesting that the sign indicates more severe biliary obstruction. In terms of laboratory indicators, the higher levels of alkaline phosphatase and total bilirubin in the ice-breaking sign group support this speculation, while the significantly lower levels of amylase in the ice-breaking sign group suggest a lower likelihood of biliary pancreatitis, which may be related to the difficulty of passing impacted stones through the ampulla of Vater. In addition, the ice-breaking sign is a strong indicator for surgery, as its presence may indicate that ERCP and LCBDE may be unsuccessful, prompting biliary surgeons to expect a higher likelihood of placing T-tubes and using intraoperative lithotripsy techniques when encountering this sign and to operate more carefully and cautiously to reduce the risk of intraoperative bleeding. There was no significant difference in the total length of hospital stay between the two groups, but the length of the postoperative hospital stay in the ice-breaking sign group was significantly longer than that of patients in the control group. This was possibly due to more severe biliary obstruction and faster disease progression in patients with the ice-breaking sign, requiring more prompt endoscopic treatment or surgical intervention to relieve the obstruction.
In terms of imaging features, there was a clear difference in the percentage of narrowing of the proximal and distal bile ducts between the two groups of patients. In the icebreaking sign group, only 13.6% (6/44) of patients had > 50% of narrowing of the proximal and distal ducts, and only 17.1% (7/41) of patients in the control group had < 50% of narrowing. This finding is consistent with the initial subjective impression of sudden narrowing of the common bile duct in this study, indicating that patients with this type of common bile duct stones are distinct from those with general common bile duct stones, and may have their own independent pathophysiological mechanisms and predisposing factors.
Choledocholithiasis has long been considered one of the most challenging biliary diseases to treat. Its associated complications such as cholangitis, obstructive jaundice and biliary pancreatitis may be life-threatening. According to both domestic and international guidelines, early and proactive surgical intervention is recommended[1]. In recent years, with the advancement of endoscopic and minimally invasive surgical techniques, ERCP and LCBDE have been widely used in the treatment of choledocholithiasis. Their safety and efficacy as evidence-based practices have been supported by research reporting various levels of evidence[1]. However, despite these advances, some cases of choledocholithiasis pose significant treatment challenges, with both endoscopic and surgical interventions having high failure rates, leading to it being characterized by the presence of difficult bile duct stones. There have been numerous studies on difficult bile duct stones. Some research indicates that factors contributing to failed ERCP include larger stone size, multiple stones, hard stone consistency, angulated bile ducts, and distal bile duct narrowing[7]. Additionally, other studies suggest that a smaller ratio of bile duct diameter to stone diameter is an independent predictor of ERCP difficulty[10]. However, none of the above studies has addressed the influence of the ratio of stone distribution between the proximal and distal ends on the success of ERCP. It is generally believed that large stones (> 15 mm), multiple stones (> 3), intrahepatic bile duct stones and obstructive bile duct stones are considered difficult bile duct stones. Based on this definition, the preferred treatment for difficult bile duct stones is endoscopic sphincterotomy plus balloon dilation, with stone fragmentation under cholangioscopic guidance considered an alternative option[11]. According to our study, the success rate of LCBDE is higher than that of ERCP for patients with the ice-breaking sign (69.4% vs 25.0%); therefore, for these patients, the above conclusion does not apply, and LCBDE should be the preferred option for stone removal.
Research related to the failure of LCBDE suggests that no clinical factors have been found to predict success. Compared with the surgical removal of multiple stones, the surgical removal of single large stones is likely to fail, but the difference is not significant[8]. In this study, however, there was a significant difference in the success rate of LCBDE between the case and control groups. This difference can be used to better define difficult common bile duct stones, distinguish ordinary and common bile duct stones, and help hepatobiliary surgeons assess the degree of surgical difficulty and risk preoperatively, thereby providing more targeted treatment plans. Previous studies have proposed grading the difficulty of LCBDE surgery to assist hepatobiliary surgeons in assessing surgical difficulty and risk[12]. The ice-breaking sign can also serve as a supplement to this. In our experience, dilating the distal bile duct during cholangioscopy is difficult in patients with the ice-breaking sign, making it difficult for the stone retrieval basket to pass through and significantly increasing the difficulty of stone retrieval and the risk of injury during dilation of the distal bile duct. This has important implications for assessing the difficulty and risk of surgery. Furthermore, with the widespread application of MRCP, the ice-breaking sign is easily observed on images, which helps hepatobiliary surgeons quickly interpret patient condition, evaluate surgical risks, and prepare for preoperative work.
Although the ice-breaking sign may resemble benign distal common bile duct strictures on imaging, our study suggests that it is likely unrelated to such benign strictures. Benign common bile duct strictures are typically caused by biliary diseases or prior biliary surgery and are generally persistent in nature[13]. In contrast, there was no significant difference between the ice-breaking sign and control groups in terms of history of biliary disease or biliary surgery. All patients underwent postoperative cholangiography, which revealed no evidence of biliary stricture. These findings suggest that the ice-breaking sign has a distinct underlying mechanism, which warrants further investigation and exploration.
This study had some limitations. As the characterization of the ice-breaking sign was inspired by clinical practice, research is still ongoing into the exploration stage in terms of specifically and objectively defining this phenomenon. Experienced biliary surgeons assigned patients to the case group by only reviewing images. The sample size of this study was small, and the underlying causes of the ice-breaking sign have not yet been fully elucidated. Future research should involve prospective multicenter studies with larger sample sizes to more precisely define this imaging feature, explore its pathogenesis, and further validate its clinical significance and utility.
The ice-breaking sign has guiding significance for the treatment of common bile duct stones, suggesting that ERCP is not suitable and that LCBDE should be the preferred treatment option. Furthermore, the ice-breaking sign may indicate increased surgical difficulty and higher surgical risks, requiring the surgeon to be more vigilant and adequately prepared preoperatively and to exercise caution during anatomical dissection and operation. For centers in which lithotripsy techniques or laparoscopic T-tube placement is impossible, prompt transfer or referral to a center equipped for these services should be considered.
| 1. | Manes G, Paspatis G, Aabakken L, Anderloni A, Arvanitakis M, Ah-Soune P, Barthet M, Domagk D, Dumonceau JM, Gigot JF, Hritz I, Karamanolis G, Laghi A, Mariani A, Paraskeva K, Pohl J, Ponchon T, Swahn F, Ter Steege RWF, Tringali A, Vezakis A, Williams EJ, van Hooft JE. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019;51:472-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 463] [Cited by in RCA: 431] [Article Influence: 61.6] [Reference Citation Analysis (0)] |
| 2. | Lan WF, Li JH, Wang QB, Zhan XP, Yang WL, Wang LT, Tang KZ. Comparison of laparoscopic common bile duct exploration and endoscopic retrograde cholangiopancreatography combined with laparoscopic cholecystectomy for patients with gallbladder and common bile duct stones a meta-analysis of randomized controlled trials. Eur Rev Med Pharmacol Sci. 2023;27:4656-4669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 3. | Anderloni A. Difficult common bile duct stones: still "difficult" or just... "different"? Endoscopy. 2020;52:429-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Ma Z, Zhou J, Yao L, Dai Y, Xie W, Song G, Meng H, Xu B, Zhang T, Zhou B, Yang T, Song Z. Safety and efficacy of laparoscopic common bile duct exploration for the patients with difficult biliary stones: 8 years of experiences at a single institution and literature review. Surg Endosc. 2022;36:718-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Navaratne L, Martínez Cecilia D, Martínez Isla A. The ABCdE score for PREdicting Lithotripsy Assistance during transcystic Bile duct Exploration by Laparoendoscopy (PRE-LABEL). Surg Endosc. 2021;35:5971-5979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Marcelino LP, Thofehrn S, Eyff TF, Bersch VP, Osvaldt AB. Factors predictive of the successful treatment of choledocholithiasis. Surg Endosc. 2022;36:1838-1846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Almadi MA, Eltayeb M, Thaniah S, Alrashed F, Aljebreen MA, Alharbi OR, Azzam N, Aljebreen AM. Predictors of failure of endoscopic retrograde cholangiography in clearing bile duct stone on the initial procedure. Saudi J Gastroenterol. 2019;25:132-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Kao CT, Seagar R, Heathcock D, Tacey M, Lai JM, Yong T, Houli N, Bird D, Hodgson R. Factors That Predict the Success of Laparoscopic Common Bile Duct Exploration for Choledocholithiasis: A 10-Year Study. Surg Laparosc Endosc Percutan Tech. 2021;31:565-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Sirimanna P, Suh H, Falk GL. Laparoscopic common bile duct exploration: what factors determine success? ANZ J Surg. 2024;94:375-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 10. | Üsküdar O, Parlak E, Dışıbeyaz S, Köksal AS, Cıçek B, Kılıç ZM, Ödemiş B, Şaşmaz N. Major predictors for difficult common bile duct stone. Turk J Gastroenterol. 2013;24:423-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Dollhopf M, Schmetkamp H. Endoscopic management of difficult common bile duct stones. Minerva Gastroenterol (Torino). 2022;68:144-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 12. | Nassar AHM, Sallam M, Khan KS, Kilpatrick R, Zino S, Katbeh TZ. A proposed difficulty grading system for laparoscopic bile duct exploration: benefits to clinical practice, training and research. Surg Endosc. 2023;37:7012-7023. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Reference Citation Analysis (0)] |
| 13. | Dadhwal US, Kumar V. Benign bile duct strictures. Med J Armed Forces India. 2012;68:299-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/