Published online Jul 27, 2025. doi: 10.4240/wjgs.v17.i7.106700
Revised: April 6, 2025
Accepted: May 19, 2025
Published online: July 27, 2025
Processing time: 140 Days and 23.2 Hours
Congenital malrotation of the intestine is characterized by an abnormality in intestinal anatomy and mesenteric fixation resulting from disordered rotation of the intestine around the mesenteric artery during embryonic life. This disease can cause intestinal torsion, intestinal obstruction and other acute abdominal sym
A 23-year-old female patient was admitted to our hospital on January 11, 2024, with a history of recurrent periumbilical pain for over 10 years and worsening for 6 months. In this report, the patient was diagnosed with a congenital midgut malrotation with herniation of the jejunum into a malformed omentum in surgery. The patient developed a hernia sac of the omentum adjacent to the duodenum, with the upper jejunum herniating to form an intra-abdominal hernia. During surgery, the jejunum-ileum and ileocecal junction were positioned according to their normal anatomy, and the mesentery root was linearly fixed to the posterior abdominal wall. Ascending colon and right transverse colon were repositioned in their normal anatomical locations. The patient was monitored for more than 1 year post-surgery and recovered well with no signs of abdominal pain or dis
Congenital midgut reverse transposition is a specific malrotation of the intestine that is often found in adulthood. It is prone to forming intra-abdominal epiploic hernias. Personalized surgical treatment can achieve better results.
Core Tip: This paper describes the mechanism of congenital midgut reverse transposition, which is characterized by easy adult-onset and intraomental hernia. In this case, we performed personalized surgery according to the patient's intraoperative conditions. The operation achieved good results. The purpose of this case sharing is to provide a reference for clinicians to improve the diagnosis and treatment of similar cases. At the same time, we hope to actively explore laparoscopic surgery for intestinal volvulus and internal hernias in the future, because laparoscopic surgery can minimize surgical trauma and promote faster recovery of patients.
- Citation: Wang Q, Sun K, Gong XS. Congenital midgut reverse transposition with herniation of the jejunum into a malformed omentum: A case report. World J Gastrointest Surg 2025; 17(7): 106700
- URL: https://www.wjgnet.com/1948-9366/full/v17/i7/106700.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i7.106700
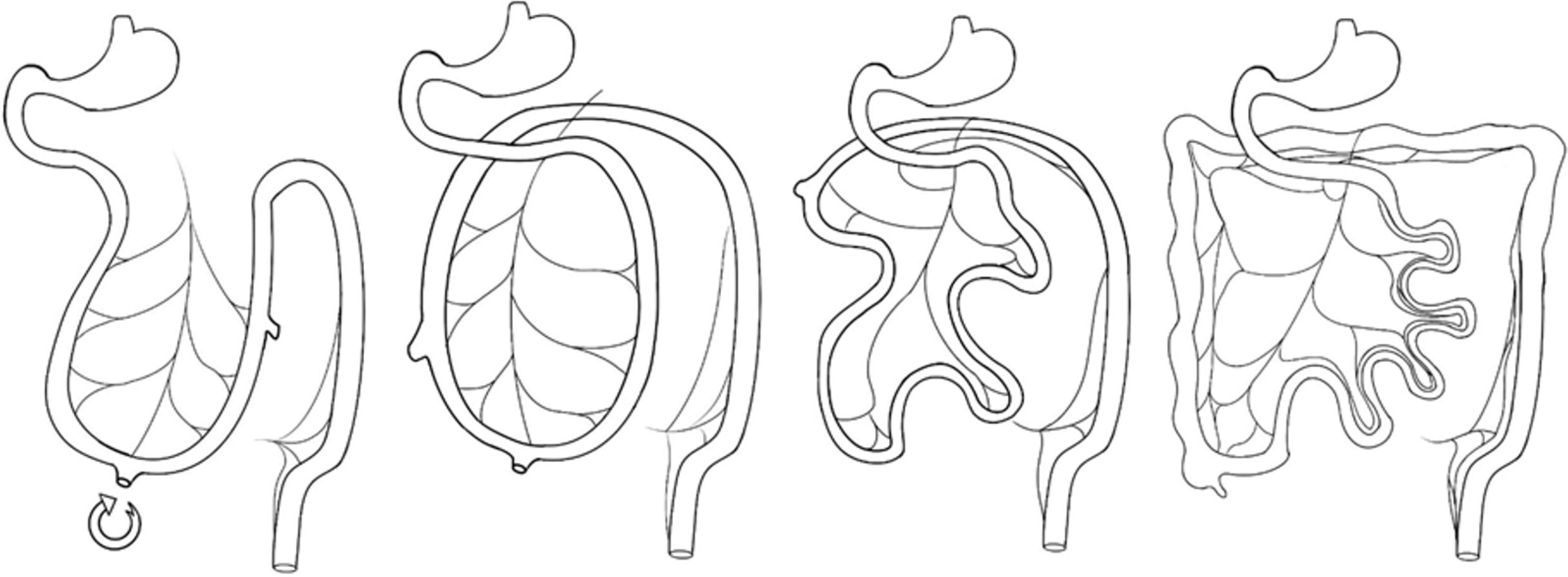
As is well known, in the 4th week of embryonic development, the primitive intestinal canal forms a sagittal relationship with the abdominal trunk, superior mesenteric artery and inferior mesenteric artery, giving rise to the foregut (upper duodenum, gastrointestinal tract and digestive organs), midgut (middle duodenum to right two-thirds of the transverse colon) and hindgut (left one-third of transverse colon and descending colon). By the 6th-8th weeks, the primitive intestinal canal grows in length and size, with some portions being squeezed into the umbilical coelom and rotating 90° an
A 23-year-old female patient was admitted to the Gastroenterology Department of our hospital on January 11, 2024, with a history of recurrent periumbilical pain for over 10 years and worsening for 6 months.
The patient had recurrent abdominal pain and had previously sought medical advice at another hospital, where she was diagnosed with an intra-abdominal hernia based on computed tomography (CT) imaging. She received conservative treatment that provided temporary relief but did not undergo surgical intervention.
There was no relevant medical history such as diabetes, hypertension, or surgery.
There was no relevant personal and family history.
On physical examination, the patient presented with upper abdominal distension, soft abdominal muscles, tenderness in the upper right abdomen, no rebound pain, and normal bowel sounds.
The patient’s laboratory tests were generally normal and unremarkable.
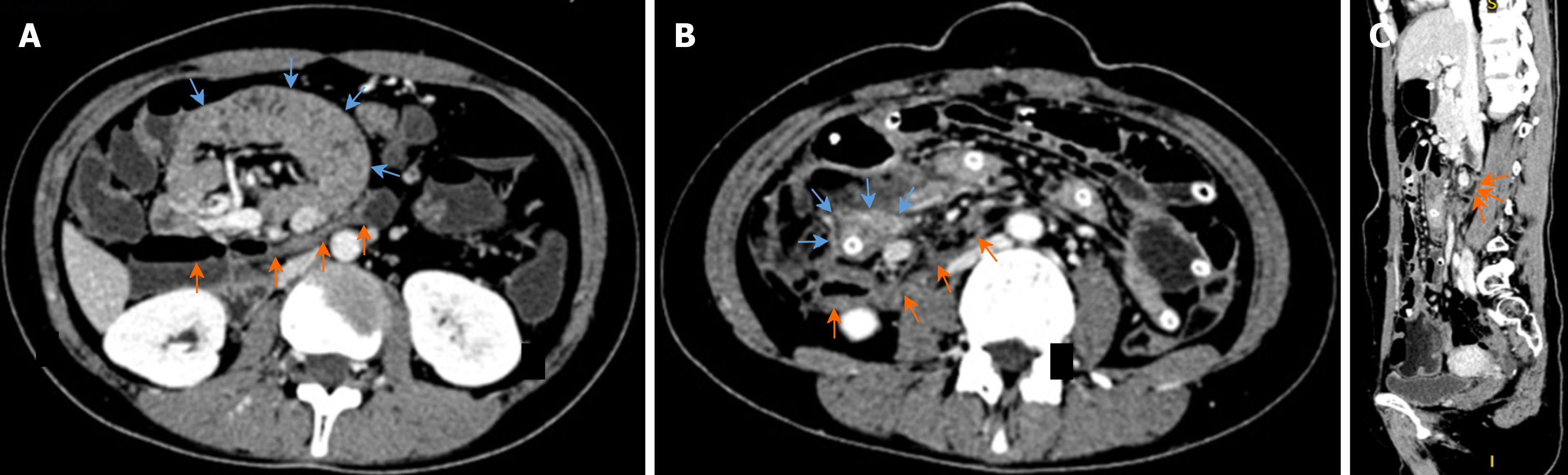
After admission, gastrointestinal endoscopy did not reveal any obvious abnormalities, but a subsequent CT enterography of the small intestine revealed abnormal aggregation of the small intestines in the upper right abdomen, suggesting an intra-abdominal hernia. The duodenum was found to be located anteriorly to the transverse colon, with associated mesenteric blood vessels gathering, expanding and twisting, leading to local compression of the transverse colon (Figure 3A). A follow-up CT scan on the 7th day post-surgery showed the horizontal segment of duodenum with an intestinal obstruction catheter as shown by the orange arrows and the transverse colon passing behind the duodenum as shown by the orange arrows (Figure 3B and C)
Based on the clinical presentation and auxiliary examination results, a final diagnosis of congenital midgut reverse transposition was confirmed.
The patient had recurrent abdominal pain and had previously sought medical advice at another hospital, where she had been diagnosed with an intra-abdominal hernia based on CT imaging. She had received conservative treatment that provided temporary relief but had not undergone surgical intervention. On physical examination, the patient presented with upper abdominal distension, soft abdominal muscles, tenderness in the upper right abdomen, no rebound pain, and normal bowel sounds. After admission, gastrointestinal endoscopy did not reveal any obvious abnormalities, but a subsequent CT enterography of the small intestine revealed abnormal aggregation of the small intestines in the upper right abdomen, suggesting an intra-abdominal hernia. The duodenum was found to be located anteriorly to the trans
After surgery, the patient was given symptomatic treatments, including gastrointestinal decompression, fasting, anal exhaust and defecation recovery. The patient started consuming small amounts of fluid food on the 5th day after surgery. A follow-up CT scan on the 7th day post-surgery showed no signs of intestinal obstruction (Figure 3B). The ileus tube was removed, and the patient was discharged from the hospital with recovery. The patient was monitored for more than 1 year post-surgery and recovered well with no signs of diarrhea or constipation.
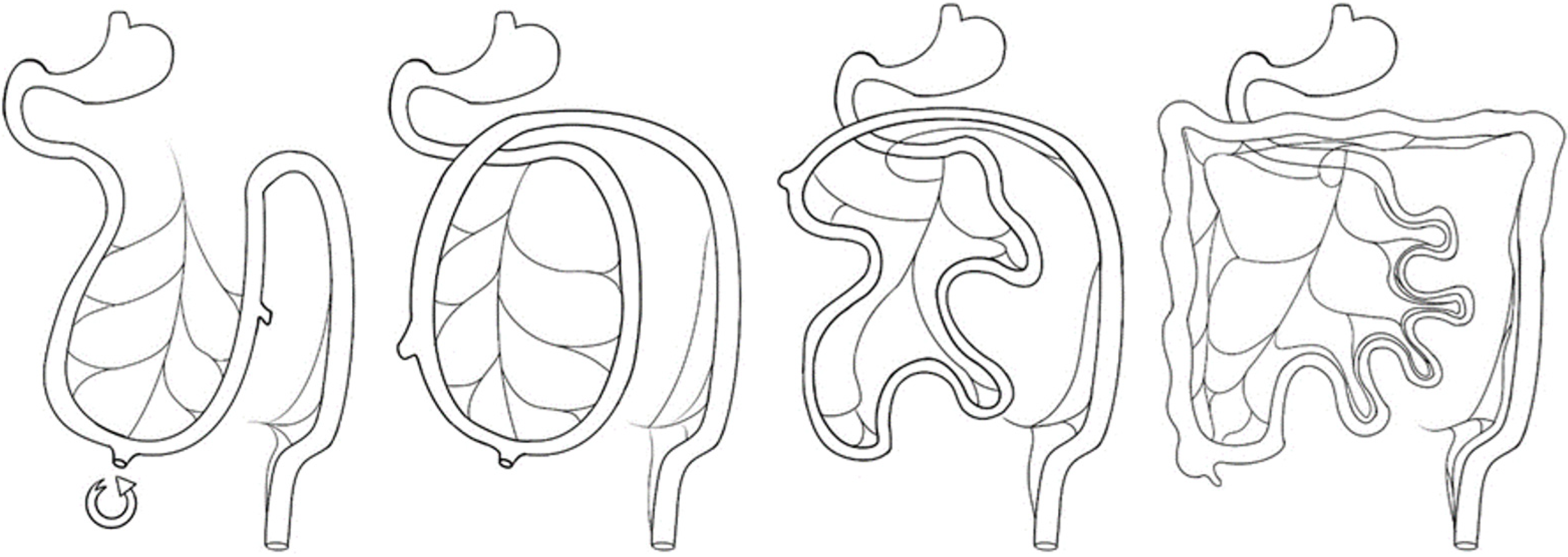
Our analysis suggests that during the 6th-8th weeks of embryonic development, the patient’s midgut underwent a 90° anticlockwise rotation around the superior mesenteric artery. Subsequently, between the 10th and 12th weeks of embryonic development, the midgut retracted into the abdominal cavity and rotated 180° clockwise around the superior mesenteric artery. This resulted in the superior mesenteric artery and transverse colon being located in the posterior part of the duodenum, while the cecum, ascending colon and jejunal mesentery remained unattached to the posterior abdominal wall, existing in a free state. The rotation process is shown in Figure 5. Intestinal malrotation, as a congenital disease, can lead to midgut volvulus in patients during the 10th-12th weeks of embryonic development, potentially impacting me
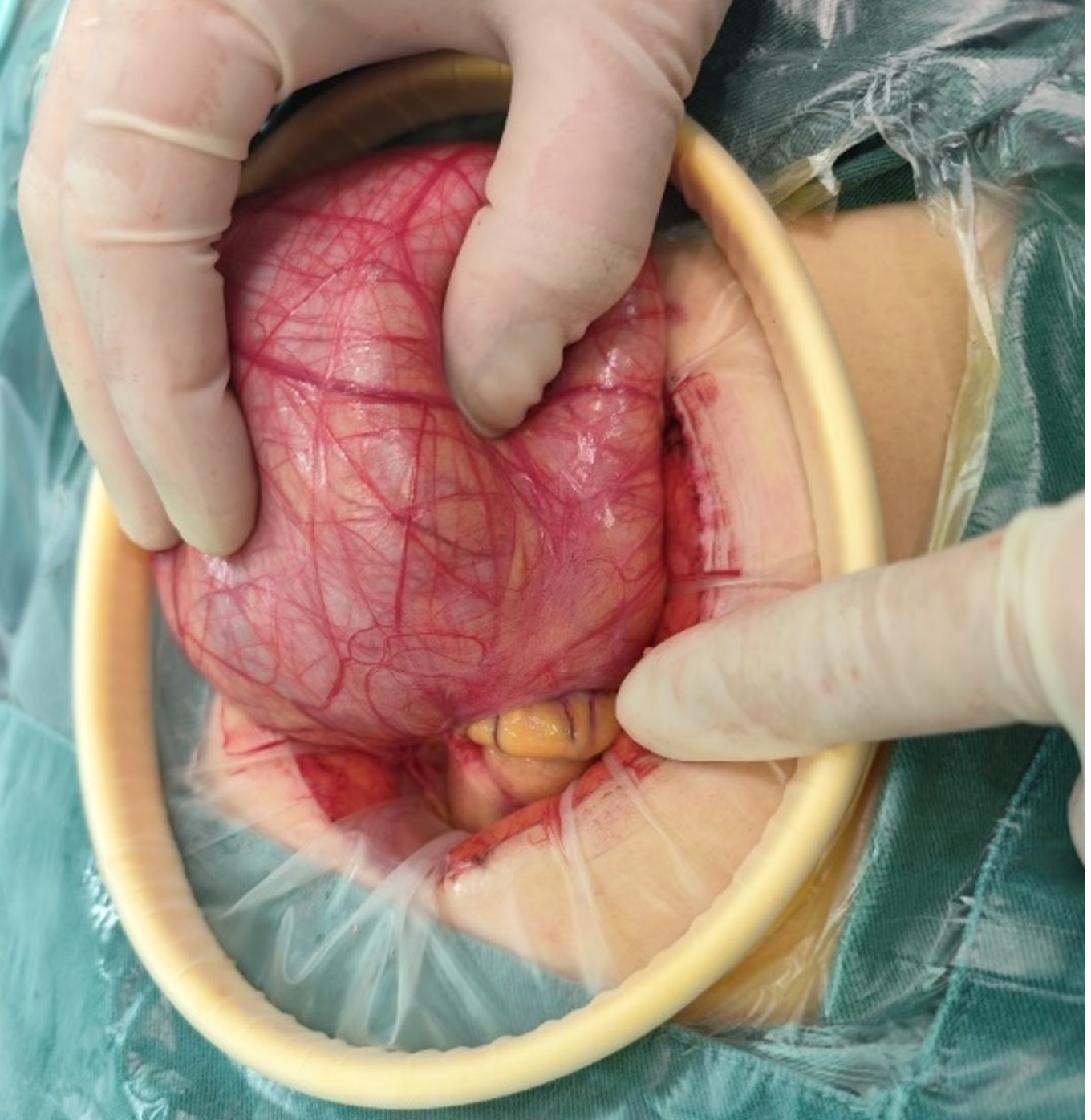
The patient developed a hernia sac of the omentum adjacent to the duodenum, with the upper jejunum herniating to form an intra-abdominal hernia. In normal midgut rotation, the transverse colon and mesentery typically cover the duodenum, while the greater omentum covers the transverse colon, reducing the likelihood of omental herniation. However, in cases of midgut malrotation, the duodenum is positioned anterior to the transverse colon, creating a gap between these structures. The greater omentum primarily covers the left side of the transverse colon, leaving the right side exposed. This anatomical configuration can lead to mental enlargement and subsequent herniation through these gaps. The development of an intra-abdominal hernia may occur when the intestinal canal herniates and the hernia sac envelops the upper small intestine, resembling a cocoon. In general, there is an immature development of the omentum during embryonic development, making it challenging to form a hernia sac around the intestinal canal. However, as the omentum matures in adulthood, the formation of the hernia sac becomes more likely. In this case, recurrent abdominal pain persisted for over 10 years, likely due to the gradual increase in intestinal hernias and associated tension.
The therapeutic approach for congenital intestinal malrotation in adults aims to relieve obstruction and restore intestinal patency[2]. In this particular case, a hernia sac formed due to a malformed omentum between the duodenum and transverse colon, leading to the herniation of the upper jejunum into the abdominal cavity, resulting in an intra-abdominal hernia without intestinal impaction or strangulation. To prevent recurrence, the herniated intestinal canal was reduced, a portion of the omentum was resected, and any gaps were sutured and closed. The patient also experienced midgut volvulus, with the superior mesenteric artery and transverse colon positioned behind the duodenum, posing a risk of duodenal compression on the transverse colon and potential intestinal obstruction. Three treatment strategies were considered: Complete dissociation of the duodenum and transverse colon, transection of the transverse colon for re-anastomosis in the anterior part of the duodenum, and side-to-side anastomosis of the left and right sides of the transverse colon to establish a shorter pathway. However, in this case, no specific intervention was required as intraoperative examination revealed no obstruction or compression at the intersection of the transverse colon and duodenum.
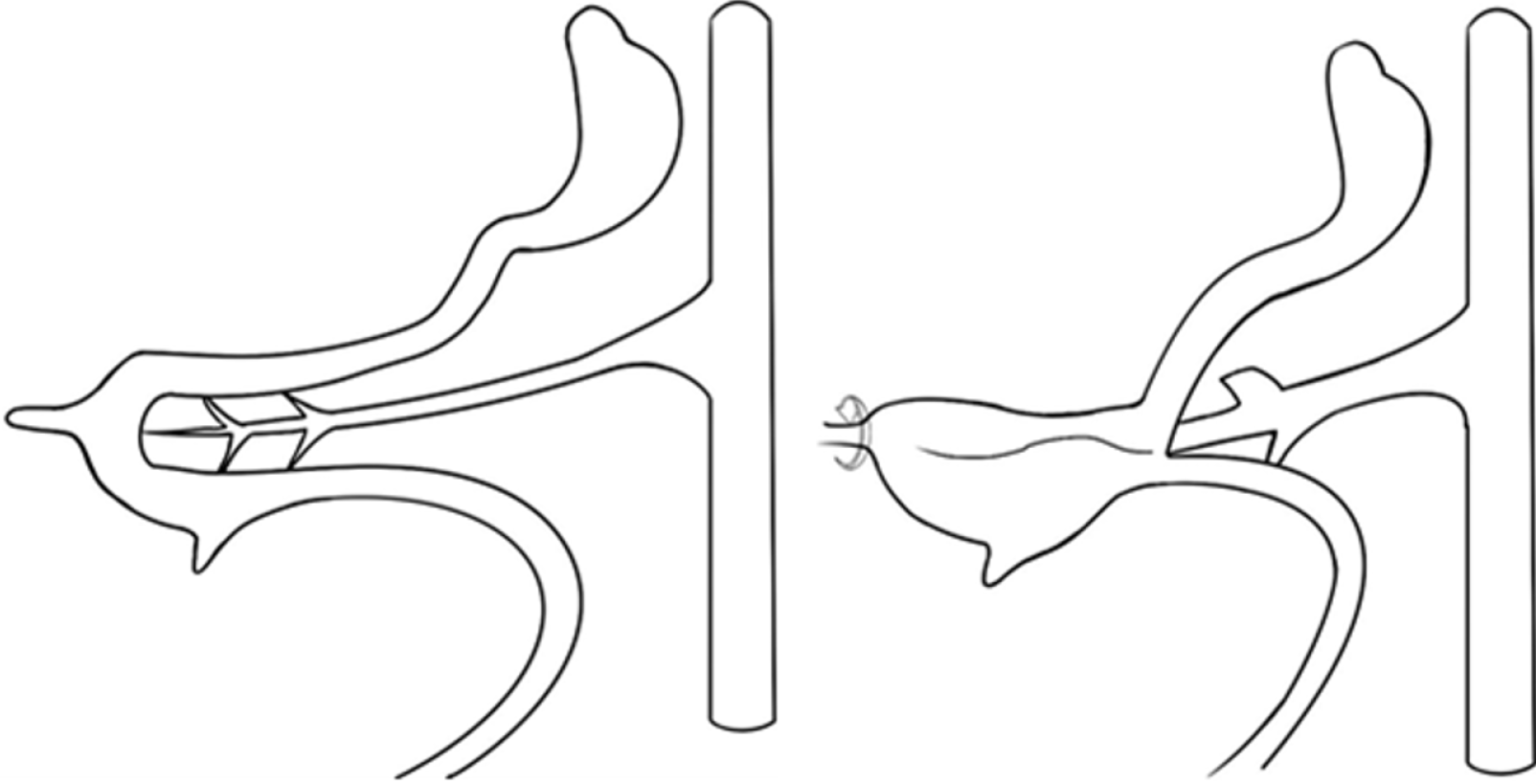
There may be a risk of volvulus due to midgut malrotation, which can lead to failure of mesenteric fixation. Previous reports have described methods of fixation for volvulus surgery, including linear fixation and fan-shaped fixation of the mesentery[3]. Specifically, fan-shaped fixation is recommended for cases with a relatively narrow attachment site of the small intestinal mesentery root and a relatively longer mesentery radius. This technique increases the width of mesentery-retroperitoneum fixation, reduces the mesentery radius and ultimately reduces the risk of postoperative volvulus anatomically. Linear fixation is suitable for patients with a proper attachment site length and mesentery radius, aligning with physiological anatomy and the distribution of the superior mesenteric artery.
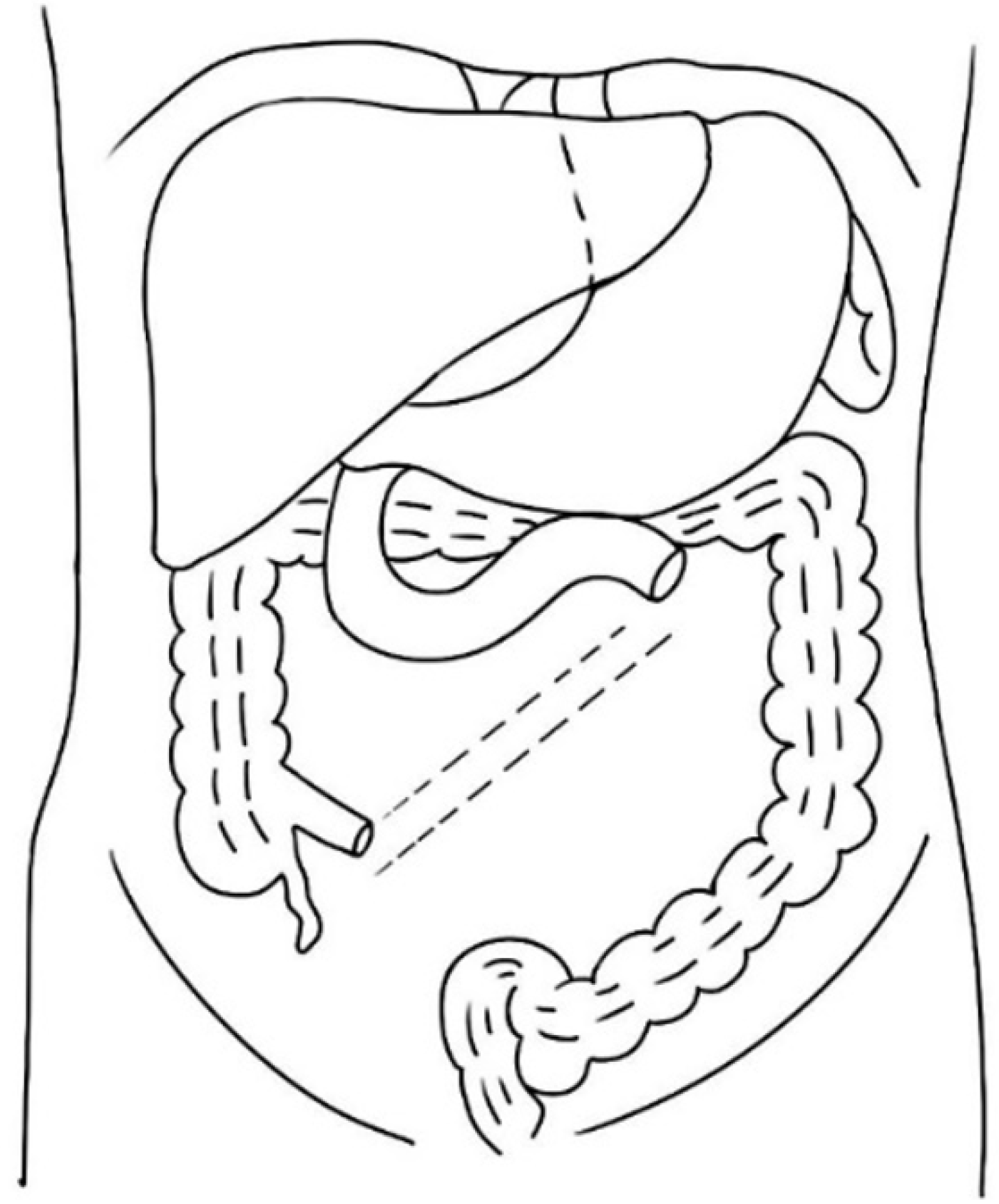
During surgery, the jejunum-ileum and ileocecal junction were positioned according to their normal anatomy, and the mesentery root was linearly fixed to the posterior abdominal wall. The fixation was made diagonally from the left side of the second lumbar vertebra to the lower right, crossing the spine and ending in the anterior part of the right sacroiliac joint. The mesentery was initially fixed with intermittent sutures, ensuring proper positioning and no compression on the transverse colon. The mesentery was then continuously and completely fixed to the posterior abdominal wall via continuous suturing, with gaps avoided. The right mesenteries of the ascending colon and transverse colon were also sutured and fixed to the posterior abdominal wall. This technique is termed as ‘linear mesenteric root fixation’, as shown in Figure 6.
Congenital midgut reverse transposition is a specific malrotation of the intestine that is often found in adulthood. It is prone to formation of intraabdominal epiploic hernias. Personalized surgical treatment can achieve better results. In this report, the patient was diagnosed with an intra-abdominal hernia and intestinal malrotation based on clinical symptoms, signs and CT imaging results. The patient also exhibited a complicated distribution of the intestinal canal and a possible abdominal cocoon at a higher position. The patient may require intestinal resection of the upper segment of the jejunum and colonic surgery. Adequate preoperative preparation was completed, including the placement of an ileus tube for bowel preparation. An open surgery was finally determined based on intraoperative exploration of the patency of the transverse colon behind the duodenum, placement of the ileus tube, and the complex condition of the patient. Previous reports have documented successful laparoscopic surgeries for similar conditions[4]. Future efforts will focus on summarizing and exploring practical experiences with laparoscopic surgery for the treatment of volvulus and intra-abdominal hernia to minimize surgical trauma and promote faster recovery for affected patients.
We would like to express our sincere gratitude to the patients’ families and patients for their support of our work.
| 1. | Schoenwolf GC, Bleyl SB, Brauer PR, Francis-West PH. Larsen’s Human Embryology. 6th ed. Amsterdam: Elsevier, 2020. |
| 2. | Ribeiro T, Greene B, Bennett S, Msallak H, Karanicolas P. Variations of intestinal malrotation in adults: A case report of midgut volvulus and literature review for the surgeon. Int J Surg Case Rep. 2022;91:106750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Jackson HM, Saed K, Adams T, Maturasingh MB, Vedros FD, Masri MM. An interesting twist: 90 year-old female with acute small bowel obstruction due to midgut volvulus. J Surg Case Rep. 2024;2024:rjae001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Miyano G, Fukuzawa H, Morita K, Kaneshiro M, Miyake H, Nouso H, Yamoto M, Fukumoto K, Urushihara N. Laparoscopic repair of malrotation: what are the indications in neonates and children? J Laparoendosc Adv Surg Tech A. 2015;25:155-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/