Published online Jul 27, 2025. doi: 10.4240/wjgs.v17.i7.105925
Revised: March 31, 2025
Accepted: May 26, 2025
Published online: July 27, 2025
Processing time: 163 Days and 4.8 Hours
Retrocecal appendicitis, the most common anatomical type, presents diagnostic and surgical challenges. Single-port laparoscopic appendectomy (SPLA) has been proposed as an alternative to multi-port laparoscopic appendectomy (MPLA) with advancements in minimally invasive surgery. However, few studies have compared the perioperative outcomes between the SPLA and MPLA for retrocecal appendicitis.
To compare the efficacy and safety between the SPLA and MPLA in treating retrocecal appendicitis, focusing on perioperative outcomes.
This retrospective study analyzed data from 1041 patients who underwent SPLA or MPLA at Konyang University Hospital between October 2011 and February 2023. Propensity score matching (PSM) was used to minimize selection bias, resulting in 235 patients in each group. Additionally, non-inferiority tests, post-hoc analysis, and multivariable regression analysis were performed to validate the results and assess factors affecting postoperative outcomes.
After PSM, SPLA showed shorter operation time (43.8 ± 15.8 minutes vs 51.6 ± 18.7 minutes; P < 0.001) and lower estimated blood loss (EBL, 6.5 ± 7.8 mL vs 8.6 ± 8.3 mL; P < 0.001) than MPLA. No significant differences were observed in complications, pain scores, or length of hospital stay. SPLA was not inferior to MPLA in the main outcomes, except for the complication rate, where statistical power was insufficient. Multivariable regression confirmed SPLA as an independent factor for operation time and EBL.
SPLA is more feasible than MPLA for retrocecal appendicitis, offering advantages in operation time and estimated blood loss. This study supports SPLA as a viable alternative that enhances postoperative recovery.
Core Tip: This study compared the efficacy and safety between the single-port laparoscopic appendectomy (SPLA) and multi-port laparoscopic appendectomy (MPLA) for retrocecal appendicitis, focusing on perioperative outcomes. After propensity score matching, SPLA was associated with a shorter operation time and lower estimated blood loss. No significant differences were observed in the other perioperative outcomes. Therefore, this study supports the feasibility of SPLA compared with MPLA for retrocecal appendicitis, suggesting that SPLA may be a viable alternative for improving postoperative recovery.
- Citation: Woo SA, Roh SJ, Sung NS, Choi WJ. Feasibility of single-port laparoscopic appendectomy for retrocecal appendicitis: A propensity score-matched study with multi-port laparoscopic appendectomy. World J Gastrointest Surg 2025; 17(7): 105925
- URL: https://www.wjgnet.com/1948-9366/full/v17/i7/105925.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i7.105925
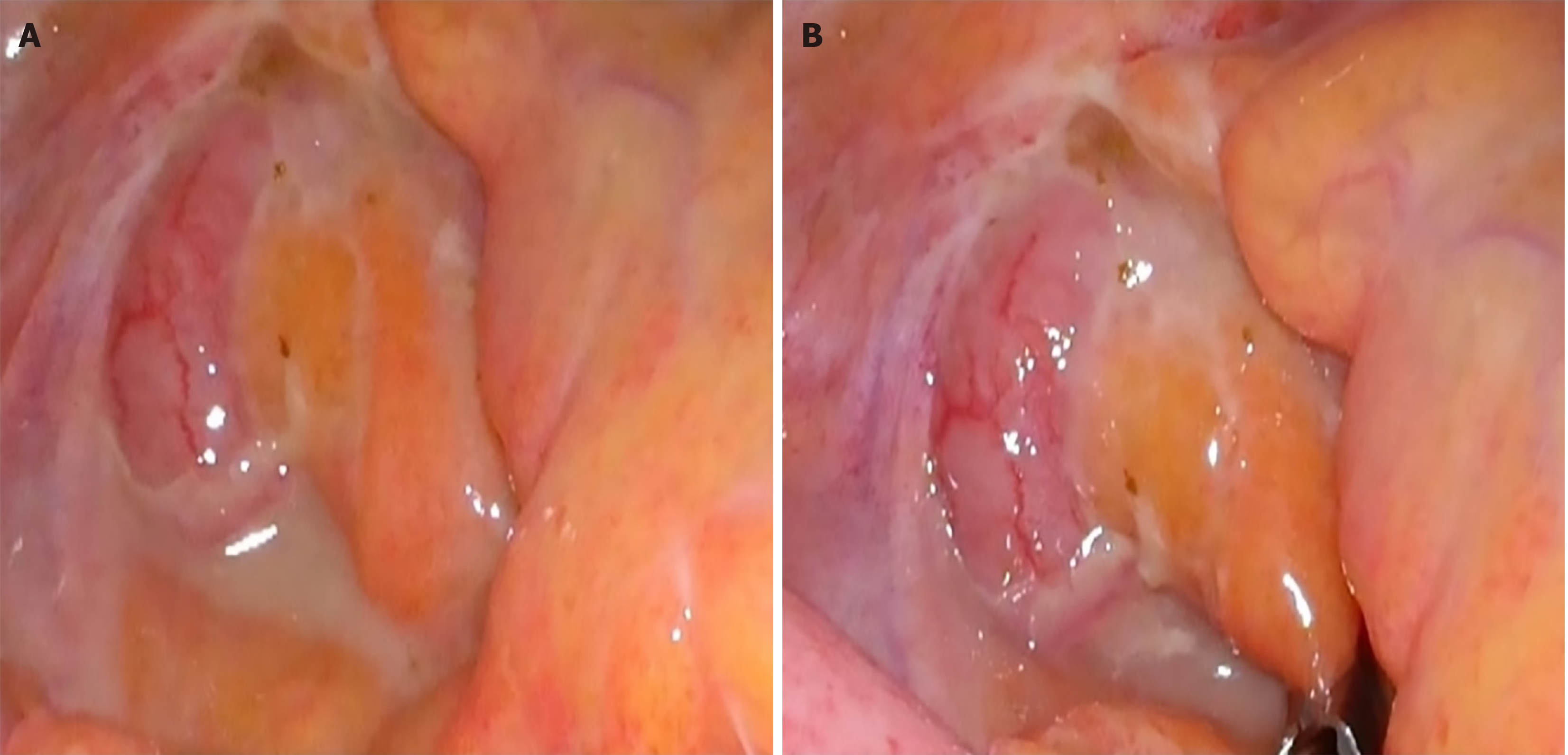
Acute appendicitis is considered a common cause of acute abdomen that could lead to emergency surgical intervention[1-3]. The appendix can be found in various anatomical positions, with the retrocecal position (25%-65%) being the most common, followed by the pelvic (16%-31%), post-ileal (18-23%), subcecal (2%-20%), and pre-ileal (1%-4%) positions[4-7]. The position of acute appendicitis affects clinical presentation[4]. Typically, it presents with specific symptoms, including periumbilical pain migrating to the right lower quadrant, along with mild fever, nausea, vomiting, and anorexia[8,9]. However, in retrocecal appendicitis, pain may be less pronounced because of the overlying bowel, and tenderness in the right lower quadrant may be absent[8,9]. Atypical signs and symptoms can delay diagnosis, resulting in severe complications such as perforation and abscess, which increase morbidity and mortality[6,9-12] (Figure 1).
With advancements in minimally invasive surgery, laparoscopic appendectomy is preferred over open surgery[13,14]. Although multi-port laparoscopic appendectomy (MPLA) remains the gold standard procedure, single-port laparoscopic appendectomy (SPLA) has been proposed as a viable alternative[2,13]. However, its adoption remains controversial because the single-port laparoscopic procedure has disadvantages[1]. Indeed, SPLA is a challenging procedure with a longer learning curve, limited surgical visibility, instrument conflicts, and longer operation time[1,2,14,15]. Conversely, some advantages of SPLA have been reported, such as reduced postoperative pain, faster recovery, and improved cosmetic outcomes[2,13,14,16].
Comparative studies on perioperative outcomes of laparoscopic appendectomy based on appendix position are lacking. Currently, studies comparing between SPLA and MPLA procedures for retrocecal appendicitis, a common yet challenging diagnosis, are scarce. Therefore, this study aimed to evaluate the efficacy of SPLA compared to that of MPLA for retrocecal appendicitis, contributing to future advancements in minimally invasive surgery.
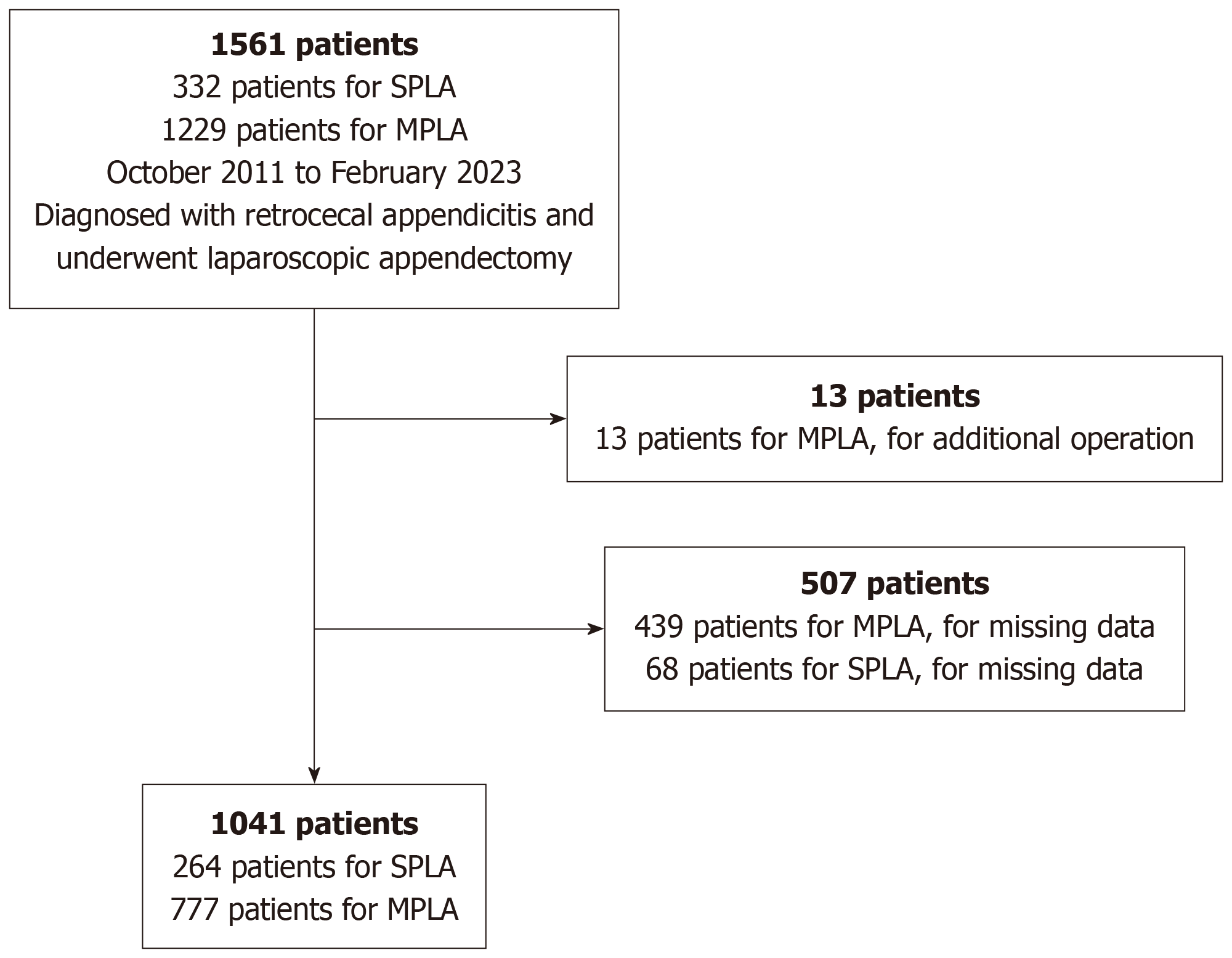
This retrospective study was conducted at Konyang University Hospital, a single center in Daejeon, Korea. Patients who underwent laparoscopic appendectomy for retrocecal appendicitis between October 2011 and February 2023 were enrolled. Of the initial 1,561 patients, 520 were excluded. Among the excluded patients, 13 who underwent MPLA required additional procedures: 6 underwent cecectomy, 5 underwent adhesiolysis, and 2 underwent primary serosal repair for iatrogenic serosal injury. A total of 507 patients were excluded because of insufficient perioperative data, including C-reactive protein (CRP) levels and postoperative pain scores [Numeric Rating Scale (NRS)] results. As a result, 439 patients were included in the MPLA group, with CRP missing in 422 patients and NRS missing in 17 patients. Similarly, 68 patients were included in the SPLA group, with CRP missing in 65 patients and NRS missing in 3 patients (Figure 2). These missing data did not show a clear systematic pattern, and were assumed to follow a Missing-at-Random mechanism. Because this study had a retrospective design and limited availability of auxiliary variables, imputation and sensitivity analyses were not performed. Therefore, we adopted a complete case analysis approach to ensure consistency across the statistical comparisons.
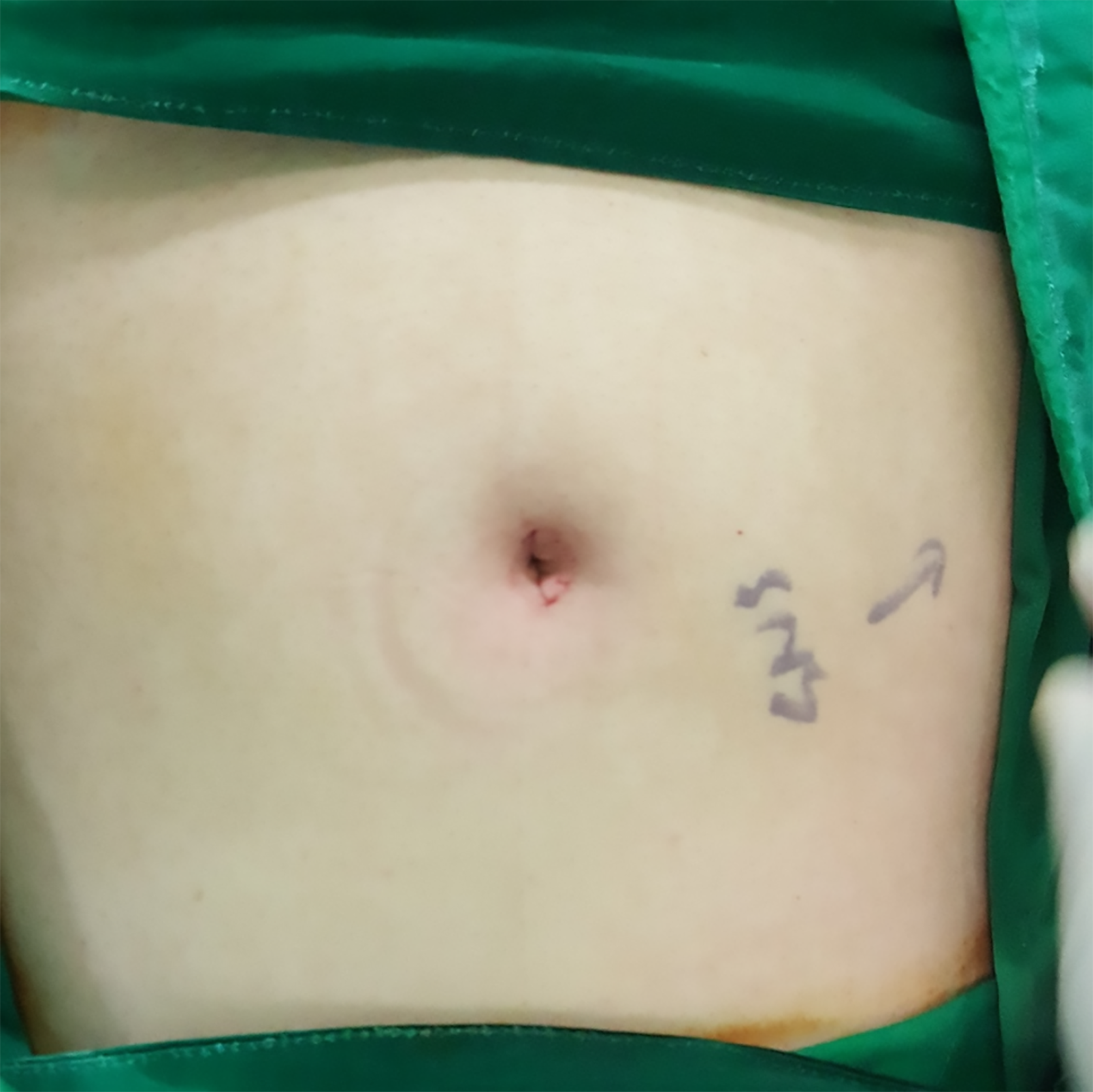
Several general surgeons at our center performed laparoscopic appendectomies. The choice between SPLA and MPLA was determined by each surgeon based on appendicitis conditions. SPLA was performed through a vertical incision approximately 2-2.5 cm long at the umbilicus using a single-port device with four channels (Glove Port, Nelis, Bucheon, Gyeonggi-do, Korea) (Figure 3). MPLA was performed with three incisions: A transumbilical vertical incision for an 11 mm trocar and two horizontal incisions in the left lower quadrant and suprapubic area for 5 mm trocars. Trocar placement followed the method depicted in figures from previous studies on SPLA and MPLA conducted at our institution[17].
We retrospectively reviewed medical records to obtain raw data for analysis. The patients’ basic demographic information, including age, sex, body mass index (BMI), medical and abdominal surgical history, smoking status, and the American Society of Anesthesiologists (ASA) classification, was collected. Perioperative clinical outcomes including laboratory test results, type of appendicitis, presence of abscess, and necessity of preoperative drainage insertion were obtained. Specifically, we recategorized the types of appendicitis into two groups based on the degree of inflammation: Mild and severe. Edematous, suppurative, and phlegmonous types were classified as mild, whereas gangrenous, perforated, and appendicitis with abscesses were classified as severe. Postoperative outcomes, including operation time, estimated blood loss (EBL), need for intra-abdominal drain insertion, open conversion rate, postoperative complications, postoperative pain score (NRS), antibiotic use, length of hospital stay, and readmission rate, were assessed.
To address selection bias due to differences in distributions between the two groups, propensity score matching (PSM) was performed. Variables included in the PSM were selected based on an assessment of data imbalance. Standardized mean difference (SMD) > 0.1, statistically significant differences (P < 0.05), and clinical relevance were considered. Therefore, the selected variables were age, sex, BMI, medical history (e.g., cardiogenic and pulmonary diseases), ASA classification, appendicitis type, and CRP levels. Propensity scores were estimated using logistic regression, and paired data were obtained through nearest-neighbor matching. The 95%CI was reported to indicate the precision of the estimates.
To evaluate the clinical feasibility of SPLA, additional statistical analyses were performed. A non-inferiority test was conducted after PSM to statistically validate that SPLA is not inferior to MPLA in terms of postoperative outcomes. The non-inferiority margin was determined based on previous literature.
Post-hoc analysis was performed to confirm statistical findings. Additionally, regression analysis was conducted to assess the effects of the number of ports on postoperative outcomes. Linear regression was applied for continuous variables, while logistic regression was used for categorical variables.
Continuous variables are presented as mean and standard deviation, and normality was assessed using the Shapiro-Wilk test. Before PSM, since all the continuous variables violated normality assumptions, the Mann-Whitney U test was applied. After PSM, age, BMI, and CRP still violated normality; therefore, the Mann-Whitney U test was used, whereas white blood cell (WBC) satisfied normality and was analyzed using Student’s t-test. Categorical variables are reported as counts and percentages, and the χ2 test was used for analysis. Statistical significance was set at P < 0.05.
All statistical analyses were performed using R software version 4.3.1 (R Project for Statistical Computing, Vienna, Austria).
This study included 1041 patients, of whom 264 underwent SPLA and 777 underwent MPLA. The basic demographic and perioperative clinical outcome data are presented in Table 1. Imbalances and statistically significant differences were observed in several variables, which were assessed using SMD and P values. Variables with SMD > 0.1 and P < 0.05 were considered statistically imbalanced and were selected for PSM.
| Pre-match | Post-match | |||||||
| SPLA (n = 264) | MPLA (n = 777) | P value | SMD | SPLA (n = 235) | MPLA (n = 235) | P value | SMD | |
| Age (year)a | 29.3 ± 18.5 | 38.0 ± 20.8 | < 0.001 | 0.444 | 31.1 ± 18.7 | 30.3 ± 18.7 | 0.646 | 0.044 |
| Sex | 0.523 | 0.051 | 0.854 | 0.026 | ||||
| Male | 134 (50.8) | 414 (53.3) | 122 (51.9) | 119 (50.6) | ||||
| Female | 130 (49.2) | 363 (46.7) | 113 (48.1) | 116 (49.4) | ||||
| BMI (kg/m²)b | 22.3 ± 4.3 | 22.8 ± 4.0 | 0.038 | 0.138 | 22.4 ± 4.1 | 22.3 ± 4.3 | 0.567 | 0.038 |
| Medical historyb | 0.041 | 0.152 | 0.923 | 0.018 | ||||
| No | 176 (66.7) | 461 (59.3) | 153 (65.1) | 151 (64.3) | ||||
| Yes | 88 (33.3) | 316 (40.7) | 82 (34.9) | 84 (35.7) | ||||
| Abdominal operation history | 0.288 | 0.087 | 1.000 | 0.015 | ||||
| No | 244 (92.4) | 699 (90.0) | 215 (91.5) | 214 (91.1) | ||||
| Yes | 20 (7.6) | 78 (10.0) | 20 (8.5) | 21 (8.9) | ||||
| Smoking | 0.105 | 0.056 | 0.830 | 0.016 | ||||
| No | 226 (85.6) | 630 (81.1) | 198 (84.3) | 195 (83.0) | ||||
| Yes | 33 (12.5) | 112 (14.4) | 32 (13.6) | 33 (14.0) | ||||
| Quit | 5 (1.9) | 35 (4.5) | 5 (2.1) | 7 (3.0) | ||||
| ASA classificationa | < 0.001 | 0.199 | 0.385 | 0.079 | ||||
| 1 | 119 (45.1) | 455 (58.6) | 119 (50.6) | 131 (55.7) | ||||
| 2 | 139 (52.7) | 296 (38.1) | 112 (47.7) | 98 (41.7) | ||||
| 3 | 6 (2.3) | 25 (3.2) | 4 (1.7) | 6 (2.6) | ||||
| 4 | 0 (0.0) | 1 (0.1) | 0 (0.0) | 0 (0.0) | ||||
| Pre-op WBC count (× 10³) | 13.0 ± 4.1 | 12.7 ± 4.3 | 0.676 | 0.056 | 12.9 ± 4.1 | 12.7 ± 4.2 | 0.744 | 0.030 |
| Pre-op CRPb | 2.9 ± 4.8 | 3.7 ± 5.9 | 0.030 | 0.147 | 3.1 ± 5.0 | 3.1 ± 5.3 | 0.794 | 0.005 |
| Type of appendicitisa | < 0.001 | 0.394 | 1.000 | 0.011 | ||||
| Mild | 218 (82.6) | 510 (65.6) | 190 (80.9) | 189 (80.4) | ||||
| Severe | 46 (17.4) | 267 (34.4) | 45 (19.1) | 46 (19.6) | ||||
| Presence of abscess | 0.791 | 0.035 | 0.285 | 0.132 | ||||
| No | 258 (97.7) | 755 (97.2) | 229 (97.4) | 233 (99.1) | ||||
| Yes | 6 (2.3) | 22 (2.8) | 6 (2.6) | 2 (0.9) | ||||
| Pre-op PCD insertion | 0.443 | 0.050 | 1.000 | 0.092 | ||||
| No | 263 (99.6) | 776 (99.9) | 234 (99.6) | 235 (100.0) | ||||
| Yes | 1 (0.4) | 1 (0.1) | 1 (0.4) | 0 (0.0) | ||||
Initially, PSM was performed, matching variables including age (29.3 ± 18.5 vs 38.0 ± 20.8; P < 0.001, SMD = 0.444), BMI (22.3 ± 4.3 vs 22.8 ± 4.0; P = 0.038, SMD = 0.138), medical history (yes, 66.7% vs 59.3%; P = 0.031, SMD = 0.152), ASA classification (P < 0.001, SMD = 0.199), CRP levels (2.9 ± 4.8 vs 3.7 ± 5.9; P = 0.030, SMD = 0.147) and type of appendicitis (mild, 82.6% vs 65.6%; P < 0.001, SMD = 0.394). After matching, a residual imbalance was observed in sex (P = 0.025). To further address this imbalance, sex was included as a matching variable in the final PSM.
After matching, 235 patients were included in each group (Table 1). No statistically significant differences were observed across the variables. Although an imbalance was noted in the presence of an abscess (SMD = 0.394), the difference was not statistically significant (P = 0.285). Furthermore, since the type of appendicitis was already included as a matching variable, the presence of an abscess was considered to have limited additional clinical significance.
The matched data showed balanced distributions in age (31.1 ± 18.7 vs 30.3 ± 18.7; P = 0.646, SMD = 0.044), sex (male, 51.9% vs 50.6%; P = 0.854, SMD = 0.026), BMI (22.4 ± 4.1 vs 22.3 ± 4.3; P = 0.567, SMD = 0.038), medical history (yes, 65.1% vs 64.3%; P = 0.923, SMD = 0.018), ASA classification (P = 0.385, SMD = 0.079), CRP levels (3.1 ± 5.0 vs 3.1 ± 5.3; P = 0.794, SMD = 0.005), and type of appendicitis (mild, 80.9% vs 80.4%; P = 1.000, SMD = 0.011). Moreover, no significant differences were observed between the two groups in abdominal operation history (yes, 91.5% vs 91.1%; P = 1.000, SMD = 0.015), WBC count (12.9 ± 4.1 vs 12.7 ± 4.2; P = 0.744, SMD = 0.030), and presence of abscess (yes, 97.4% vs 99.1%; P = 0.285).
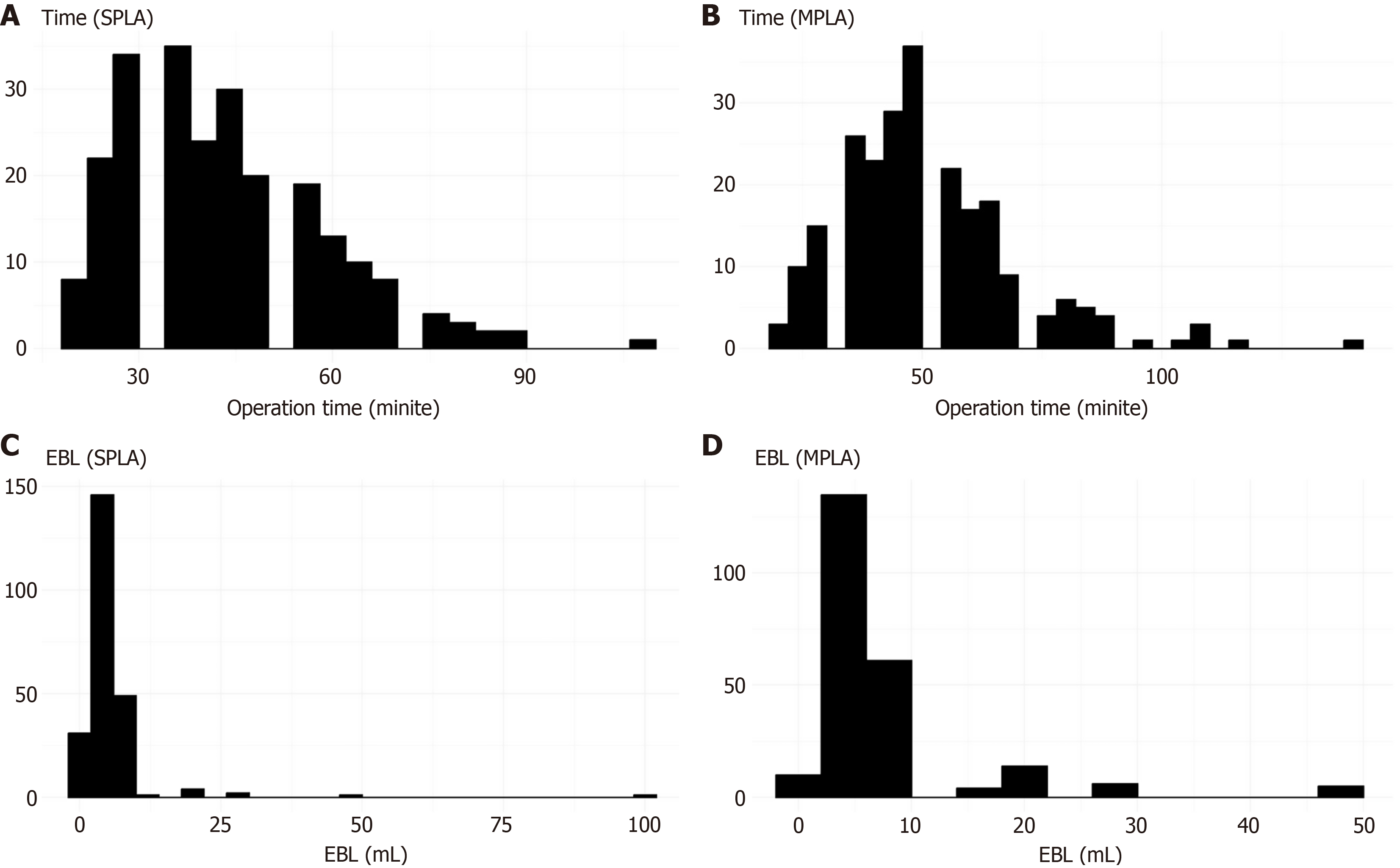
Postoperative outcomes are presented in Table 2. In the SPLA group, the operation time was shorter (43.8 ± 15.8 vs 51.6 ± 18.7; P < 0.001) and EBL was lower (6.5 ± 7.8 vs 8.6 ± 8.3; P < 0.001) than those in MPLA group, both showing statistically significant differences (Figure 4). Additionally, the necessity for postoperative drain insertion (yes, 1.7% vs 4.7%; P = 0.115) and length of hospital stay (2.7 ± 1.3 vs 2.9 ± 1.3; P = 0.176) were lower in the SPLA group; however, these differences were not statistically significant.
| SPLA (n = 235) | MPLA (n = 235) | P value | |||
| 95%CI | 95%CI | ||||
| Operation time (minute)a | 43.8 ± 15.8 | (41.8, 45.9) | 51.6 ± 18.7 | (49.2, 54.0) | < 0.001 |
| EBL (mL)b | 6.5 ± 7.8 | (5.4, 7.5) | 8.6 ± 8.3 | (7.5, 9.6) | < 0.001 |
| Drain insertion | 0.115 | ||||
| No | 231 (98.3) | 224 (95.3) | |||
| Yes | 4 (1.7) | 11 (4.7) | |||
| Complication | 0.315 | ||||
| No | 202 (86.0) | 214 (91.1) | |||
| Ileus | 2 (0.9) | 1 (0.4) | |||
| Wound complication | 24 (10.2) | 18 (7.7) | |||
| Intra-abdominal abscess | 6 (2.6) | 2 (0.9) | |||
| Others | 1 (0.4) | 0 (0.0) | |||
| Postoperative pain score | 3.2 ± 1.3 | (3.1, 3.4) | 3.1 ± 1.3 | (3.0, 3.3) | 0.178 |
| Antibiotics | 0.635 | ||||
| No | 2 (0.9) | 2 (0.9) | |||
| Cephalosporin | 191 (81.3) | 181 (77.0) | |||
| Cephalosporin + Metronidazole | 41 (17.4) | 50 (21.3) | |||
| Others | 1 (0.4) | 2 (0.9) | |||
| Hospital day (days) | 2.7 ± 1.3 | (2.6, 2.9) | 2.9 ± 1.3 | (2.7, 3.1) | 0.176 |
| Readmission | 1.000 | ||||
| No | 234 (99.6) | 234 (99.6) | |||
| Yes | 1 (0.4) | 1 (0.4) | |||
Conversely, the incidence of postoperative complications (yes, 14.0% vs 8.9%; P = 0.178) on the first postoperative day was lower in the MPLA group, although this difference was not statistically significant. The most common postoperative complications in the SPLA group were wound complications (10.2%), followed by intra-abdominal abscesses (2.6%) and ileus (0.9%). Similarly, in the MPLA group, wound complications (7.7%) were the most common, followed by intra-abdominal abscesses (0.9%) and ileus (0.4%).
Both groups reported similar antibiotic use (yes, 99.1% vs 99.1%; P = 0.635). Cephalosporin were the most commonly used antibiotics in both groups (81.3% vs 77.0%), followed by cephalosporin plus metronidazole (17.4% vs 21.3%). Carbapenem and penicillin were administered in both groups.
Neither group had any readmissions. Before PSM, one case of open conversion surgery occurred in the MPLA group because of severe inflammation and adhesion at the appendiceal base. However, this case was excluded from the matched data after PSM.
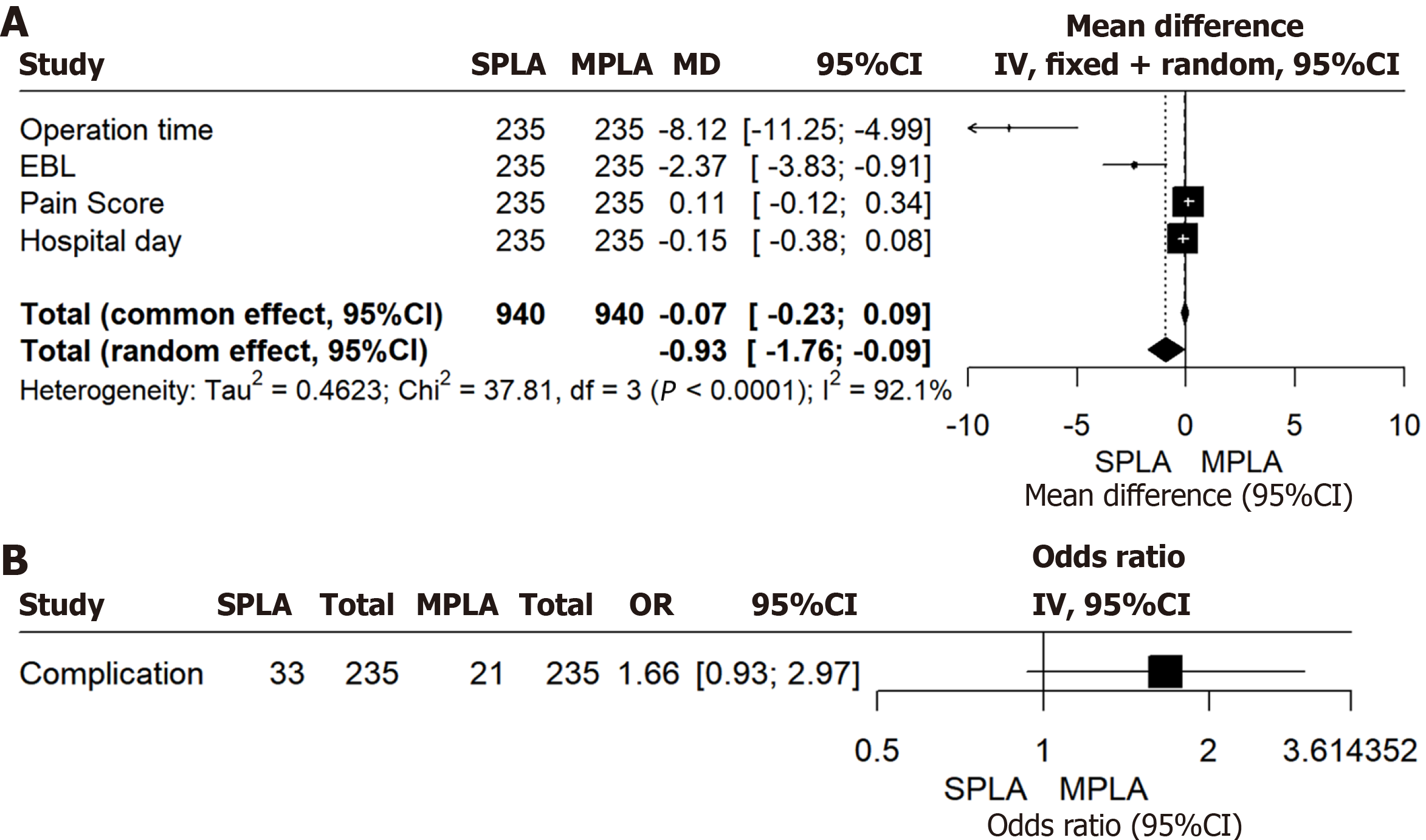
The results of the non-inferiority test for postoperative outcomes are represented in Figure 5. SPLA was confirmed to be non-inferior to MPLA in terms of operation time (mean difference: -8.12 minutes, 95%CI: -11.25 to -4.99) and EBL (mean difference: -2.37 mL, 95%CI: -3.83 to -0.91), since the upper bounds of the 95%CI remained below the predefined non-inferiority margins (10 minutes[2] and 10 mL[18], respectively). Similarly, the non-inferiority of SPLA was confirmed for postoperative pain score (mean difference: 0.11, 95%CI: -0.12 to 0.34, and margin: 1[1]) and length of hospital day (mean difference: -0.15 days, 95%CI: -0.38 to 0.08, and margin: 0.5 days[2]). However, in terms of complication rates, the non-inferiority of SPLA was not demonstrated [odds ratio (OR): 1.66, 95%CI: 0.93 to 2.97], because the upper bound of 95%CI exceeded the predefined non-inferiority margin (OR 1.65)[18].
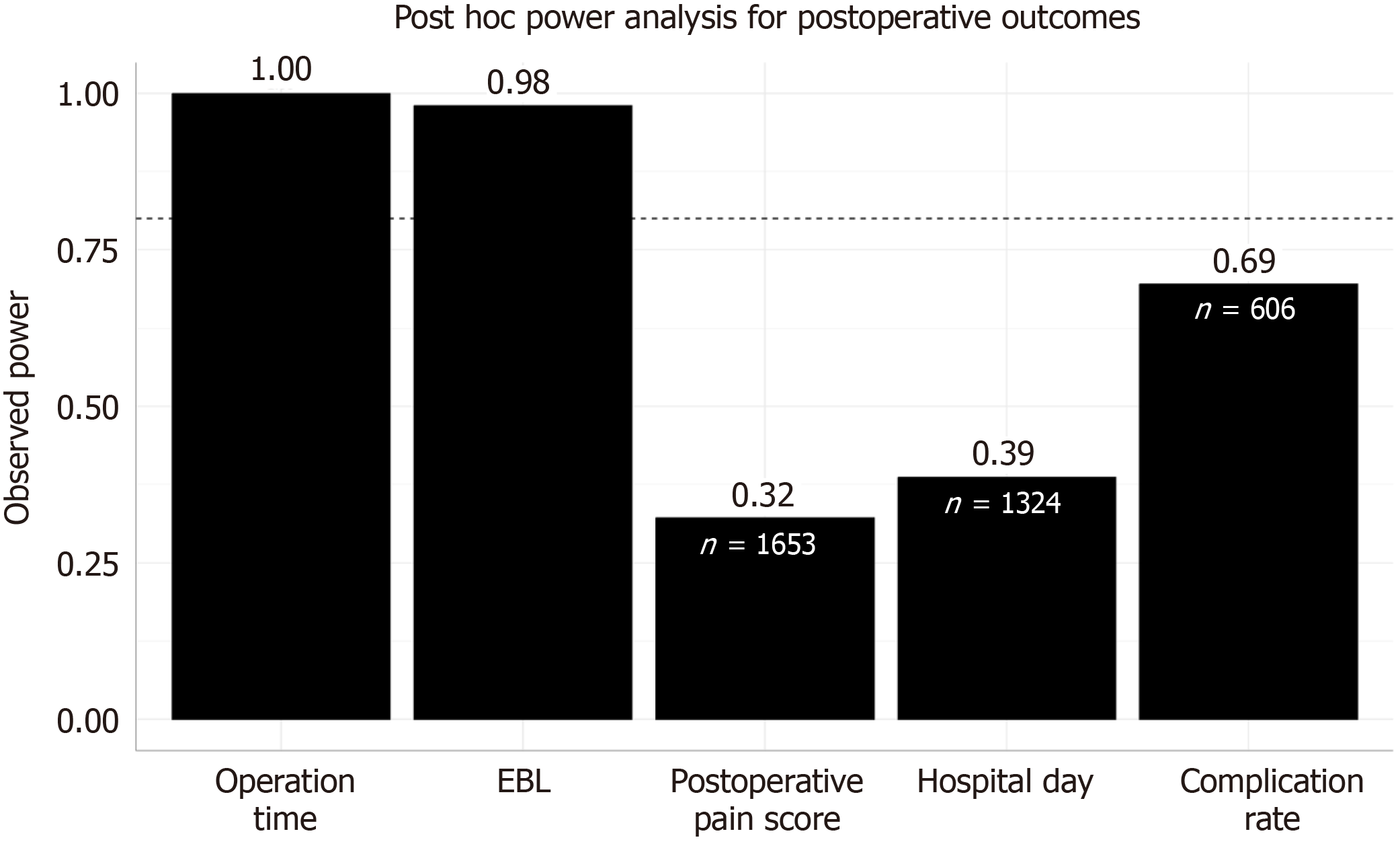
A post hoc analysis was performed to assess the statistical power of the tests (Figure 6). The power for operation time and EBL were 1.00 and 0.98, respectively, demonstrating sufficient power. However, the power for postoperative pain score (0.32), length of hospital day (0.39), and complication rate (0.69) was below the threshold of 0.8, suggesting insufficient power. The estimated sample sizes required to achieve a power of 0.8 were 1653 for postoperative pain score, 1324 for length of hospital day, and 606 for complication rate.
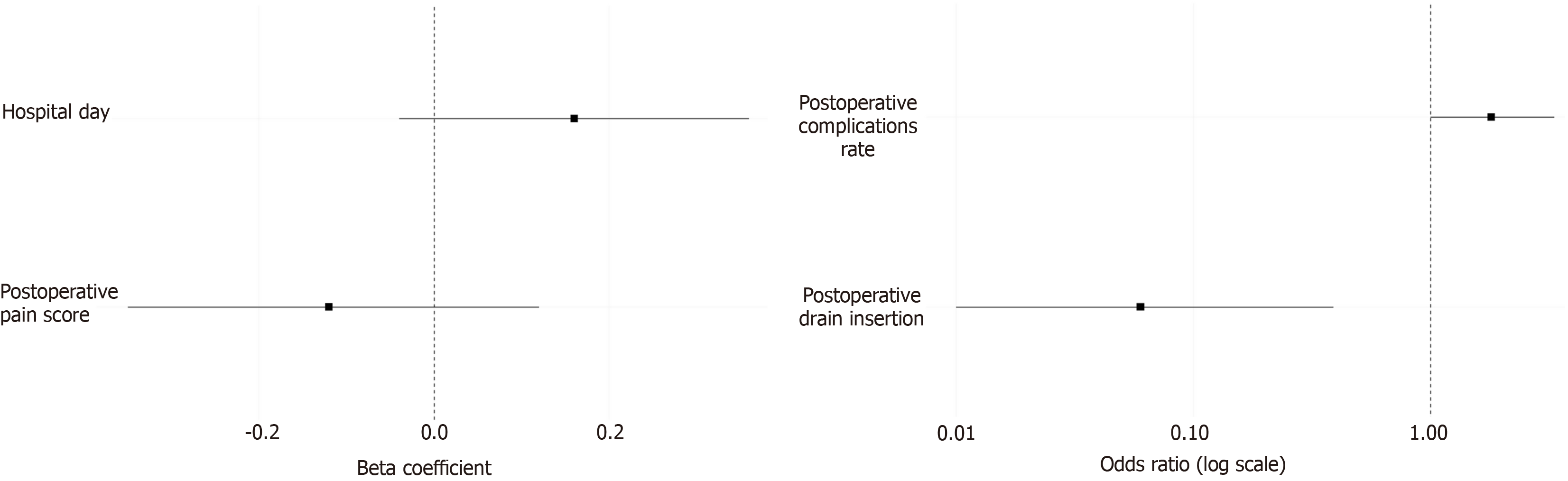
Multivariable regression analysis was performed to evaluate independent factors affecting postoperative outcomes (Table 3). SPLA was significantly associated with reduced operation time (β = 7.97, 95%CI: 4.97-10.97, P < 0.001) and lower EBL (β = 2.35, 95%CI: 0.96-3.74, P = 0.001). No significant association was observed between postoperative pain score (β = -0.12, 95%CI: -0.35 to 0.12, P = 0.311) and length of hospital day (β = 0.16, 95%CI: -0.04 to 0.36, P = 0.123). Although SPLA demonstrated a higher tendency for complication rates (OR = 1.80, 95%CI: 1.00-3.32, P: 0.052), the difference was not statistically significant. In contrast, SPLA was significantly associated with a lower tendency for postoperative drain insertion (OR = 0.06, 95%CI: 0.01-0.39, P = 0.010; Figure 7).
| Postoperative outcomes | Estimate (β/OR) | Standard error | 95%CI | P value |
| Operation time (min, β)a | 7.97 | 1.53 | (4.97, 10.97) | < 0.001 |
| EBL (mL, β)b | 2.35 | 0.71 | (0.96, 3.74) | 0.001 |
| Postoperative pain score (β) | -0.12 | 0.12 | (-0.35, 0.12) | 0.311 |
| Hospital day (days, β) | 0.16 | 0.10 | (-0.04, 0.36) | 0.123 |
| Complication rate (%, OR) | 1.80 | 0.30 | (1.00, 3.32) | 0.052 |
| JP drain insertion (%, OR)c | 0.06 | 1.07 | (0.01, 0.39) | 0.010 |
Since its introduction in 1983, laparoscopic appendectomy has replaced open appendectomy, with SPLA adopted in 1992, further reinforcing the benefits of minimally invasive surgery[2,13]. However, few studies have compared postoperative outcomes based on appendix position, particularly for retrocecal appendicitis, which is the most common but difficult to access because of its anatomy[1,4-7,13]. Therefore, we conducted a study over several years to evaluate the clinical usefulness of SPLA in retrocecal appendicitis, assessing its efficacy compared to MPLA.
Han et al[1] analyzed randomized clinical trials (RCTs) and argued that inserting multiple instruments and a camera through a single incision could cause operational restrictions and intraoperative visual disturbances, thereby prolonging the operation time. Similarly, Cirocchi et al[2] reviewed additional RCTs and attributed longer operation times to challenges, including instrument conflicts and difficulties in camera control. Jin et al[16] reported technical difficulties, such as longer operating times. Additionally, the technical challenges of SPLA in complicated appendicitis can extend operation times, making it crucial to efficiently select patients suitable for SPLA[2]. For example, Chen et al[15] recommended SPLA for mild inflammation and uncomplicated appendicitis, but advised caution in complicated appendicitis because of the higher risk of open conversion and the need for indwelling abdominal drainage.
However, our findings showed that the operation time for SPLA was significantly shorter than that for MPLA (Table 2). According to Cirocchi et al[2], surgeons’ variability in performing surgery may lead to statistical differences in postoperative outcomes. Siam et al[19] demonstrated that experienced surgeons, such as senior staff, performed appendectomies significantly faster than trainees. Ongoing surgical experience is expected to reduce these variations[1,14,20]. Similarly, Mönttinen et al[20] reported that appendectomies are often performed by surgeons with varying subspecialties and levels of experience in emergency surgery. Surgeons who routinely use laparoscopic techniques achieve improved outcomes. In our study, colorectal surgeons performed in approximately 45% of SPLA cases. These findings suggest that surgeons’ experiences in minimally invasive surgery could have influenced the favorable postoperative outcomes.
Kang et al[13] observed controversies regarding the superiority of SPLA and MPLA in postoperative pain outcomes. Cirocchi et al[2] suggested that prolonged umbilical muscle stretching due to longer operation times exacerbates postoperative pain, whereas Han et al[1] reported that minimizing tissue damage and reducing stimulation of the abdominal muscles during SPLA can decrease postoperative pain. Jin et al[16] suggested that easy suction of the residual intra-abdominal fluid during SPLA reduces postoperative abdominal pain. Although the SPLA group had numerically higher postoperative pain scores in our study, the difference was not statistically significant. The post-hoc power analysis demonstrated that the study was underpowered to detect significant differences in terms of postoperative pain and had the possibility of type II error presented. Therefore, further study with adequate power is needed to compare postoperative pain between the two groups.
Regarding postoperative complication rates, particularly wound complications, previous studies reported a lower wound complication rate in the SPLA group[2]. However, the opposite result was observed in our study, with a higher rate of wound complications in SPLA. This difference could be attributed to statistical limitations. Although the non-inferiority of SPLA was not statistically confirmed, the post-hoc power analysis suggested that the observed power was insufficient to detect a significant difference. A total of 606 patients were required to achieve a power of 0.8, and the unsatisfactory result of the non-inferiority test may have been due to the insufficient sample size. Furthermore, differences in wound closure techniques among surgeons or patient selection might have contributed to the wound complication rate.
Additionally, several studies have shown that SPLA has other advantages, such as faster recovery, leading to a shorter length of hospital stay[2] and reduced risk of intraoperative abdominal trauma[1]. Our study found that SPLA was associated with lower intraoperative EBL. Although not investigated in our study, previous research highlights patients’ cosmetic satisfaction[1,13] and low incidence of surgical site infections[14] as advantages of SPLA.
Several studies have suggested that intraoperative factors, such as operation time and EBL, affect postoperative outcomes. Cheng et al[21] demonstrated that prolonged operation time was associated with an increased risk of surgical complications, which could delay patient recovery and prolong healthcare utilization. Li et al[22] reported that higher intraoperative EBL increased the risk of postoperative complications. Additionally, surgeon fatigue during lengthy procedures may impair decision-making quality, negatively affecting patient outcomes[23]. Therefore, although absolute differences in operation time (8 minutes) and EBL (2.4 mL) were minor, they may have contributed to favorable postoperative outcomes. Moreover, these findings may also have practical value in real-world surgical decision-making, especially when selecting between SPLA and MPLA approaches.
This study had a few limitations. First, it was conducted at a single center. Although the study was investigated over 12 years and involved multiple surgeons, SPLA outcomes may vary depending on surgeon-specific procedures or preferences. This limitation could make generalizing the findings to other healthcare centers difficult. Therefore, further large-scale, multicenter studies, including surgeons from various sub-specialties, are required to validate these findings. Second, several perioperative data were missing owing to the retrospective nature of the study, which could have introduced selection bias. Since the missing data, such as CRP and postoperative pain scores, are clinically significant variables, the excluded patients may have affected outcomes in different ways, and as a result, our findings may not have been fully generalizable. Furthermore, owing to the limited availability of auxiliary data, imputation and sensitivity analyses were not performed. In addition, the study may have been underpowered to detect significant differences in some postoperative outcomes, including complication rates, pain scores, and length of hospital days, which limits the interpretation of these findings. Third, long-term outcomes, such as cosmetic satisfaction, incisional hernia, and chronic postoperative pain, were not evaluated in this study. Collecting more detailed and structured data could improve the study’s reliability and validity. Therefore, further prospective studies are needed to evaluate these detailed long-term outcomes.
Our study found that SPLA had a shorter operation time and lower EBL, whereas no significant differences were observed between MPLA and SPLA in terms of other postoperative outcomes. Therefore, SPLA can be considered clinically efficient and non-inferior to MPLA in treating retrocecal appendicitis.
The authors sincerely appreciate all participants in this study.
| 1. | Han Y, Yuan H, Li S, Wang WF. Single-incision versus conventional three-port laparoscopic appendectomy for acute appendicitis: A meta-analysis of randomized controlled trials. Asian J Surg. 2024;47:864-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 2. | Cirocchi R, Cianci MC, Amato L, Properzi L, Buononato M, Di Rienzo VM, Tebala GD, Avenia S, Iandoli R, Santoro A, Vettoretto N, Coletta R, Morabito A. Laparoscopic appendectomy with single port vs conventional access: systematic review and meta-analysis of randomized clinical trials. Surg Endosc. 2024;38:1667-1684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 3. | Hosokawa T, Tanami Y, Sato Y, Ishimaru T, Kawashima H, Oguma E. Association between the computed tomography findings and operative time for interval appendectomy in children. Afr J Paediatr Surg. 2021;18:73-78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 4. | Khatun S, Thakur D, Shah DK. Prevalence of Retrocaecal Appendix among Patients with Appendicitis in A Tertiary Care Hospital of Nepal. JNMA J Nepal Med Assoc. 2019;57:150-153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Singh N, Agrawal P, Singh DK, Agrawal GR. Computed tomography evaluation of variations in positions and measurements of appendix in patients with non-appendicular symptoms: time to revise the diagnostic criteria for appendicitis. Pol J Radiol. 2023;88:e407-e414. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 6. | Khatoon MA, Naeem S, Akmal U, Farid A, Ahmed Khan S. Retrocecal Ascending Appendix Attached to the Hepatic Flexure and Right Intra-abdominal Testis Identified During Open Appendicectomy: A Case Report. Cureus. 2024;16:e57484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Chao KH, Lin CY, Wang CT. A Rare Presentation of Chronic Appendicitis in the Right Upper Quadrant: A Case Report. Cureus. 2023;15:e40772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Seyedhosseini-Davarani S, Akhgar A. Atypical Presentation of Acute Appendicitis: A 32-year-old Man with Gastroenteritis Symptoms; an Educational Case. Adv J Emerg Med. 2018;2:e21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 9. | Börekçi H, Karacabey S, Sipahi M, Özdemir ZT, Erkoç MF. A rare case: Retrocecal appendicitis adherent to the liver capsule. Turk J Surg. 2017;33:227-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Evrimler S, Okumuser I, Unal N. Computed Tomography (CT) Findings of a Diagnostic Dilemma: Atypically Located Acute Appendicitis. Pol J Radiol. 2016;81:583-588. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Faizi FR, Farzam F. Perforated retrocecal appendicitis presenting with lung abscess-A case report. Radiol Case Rep. 2022;17:2754-2758. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 12. | Al Amri FS, Fihrah RS, Al Jabbar I, Alqahtani R, Alnujaymi B, Alshehri RM, Asiri SS. Accuracy of Neutrophil-to-Lymphocyte Ratio in Predicting the Severity of Acute Appendicitis: A Single-Center Retrospective Study. Cureus. 2023;15:e45923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 13. | Kang SI, Woo IT, Bae SU, Yang CS. Single-Incision Versus Conventional Laparoscopic Appendectomy: A Multi-Center Randomized Controlled Trial (SCAR trial). Int J Surg Protoc. 2021;25:201-208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Chen Y, Guo S, Liu Y, Yuan J, Fan Z. Single-port laparoscopic appendectomy using a needle-type grasping forceps compared with conventional three-port laparoscopic appendectomy for patients with acute uncomplicated appendicitis: a single-center retrospective study. J Int Med Res. 2022;50:3000605221119647. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (108)] |
| 15. | Chen Y, Fan Z, Zhang X, Fu X, Li J, Yuan J, Guo S. A brief overview of single-port laparoscopic appendectomy as an optimal surgical procedure for patients with acute appendicitis: still a long way to go. J Int Med Res. 2023;51:3000605231183781. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Jin SG, Cho SH, Kim KY, Ahn SK, Cho JWHW, Jung BW, Kim BC, Yoon SN. Transumbilical Single-Incision Laparoscopic-Assisted Appendectomy (TULAA) Is Useful in Adults and Young Adolescents: Comparison with Multi-Port Laparoscopic Appendectomy. Medicina (Kaunas). 2019;55:248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Song R, Sung NS, Roh SJ, Choi WJ, Choi IS, Yoon DS, Lee SE, Moon JI, Kwon SU, Bae IE, Lee SJ, Kim SG. The feasibility of single-port laparoscopic interval appendectomy for complicated appendicitis: A comparison study with multi-port laparoscopic appendectomy in a single institution in Korea. Clin Surg. 2022;7:3399. |
| 18. | Song Z, Liu K, Li Y, Shi Y, Jiang Y, Wang C, Chen X, Zhang T, Ji X, Zhao R. Short-Term Outcomes of Single-Incision Laparoscopic Surgery for Colorectal Cancer: A Single-Center, Open-Label, Non-Inferiority, Randomized Clinical Trial. Front Oncol. 2021;11:762147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Siam B, Al-Kurd A, Simanovsky N, Awesat H, Cohn Y, Helou B, Eid A, Mazeh H. Comparison of Appendectomy Outcomes Between Senior General Surgeons and General Surgery Residents. JAMA Surg. 2017;152:679-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 20. | Mönttinen T, Kangaspunta H, Laukkarinen J, Ukkonen M. Routine use of laparoscopic techniques in daily practice improves outcomes after appendectomy. Eur J Trauma Emerg Surg. 2023;49:1763-1769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Cheng H, Clymer JW, Po-Han Chen B, Sadeghirad B, Ferko NC, Cameron CG, Hinoul P. Prolonged operative duration is associated with complications: a systematic review and meta-analysis. J Surg Res. 2018;229:134-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 623] [Article Influence: 77.9] [Reference Citation Analysis (0)] |
| 22. | Li ZW, Shu XP, Wen ZL, Liu F, Liu XR, Lv Q, Liu XY, Zhang W, Peng D. Effect of intraoperative blood loss on postoperative complications and prognosis of patients with colorectal cancer: A metaanalysis. Biomed Rep. 2024;20:22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 23. | Reijmerink IM, van der Laan MJ, Wietasch JKG, Hooft L, Cnossen F. Impact of fatigue in surgeons on performance and patient outcome: systematic review. Br J Surg. 2024;111:znad397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 20] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/