Published online Jul 27, 2025. doi: 10.4240/wjgs.v17.i7.105503
Revised: April 15, 2025
Accepted: May 16, 2025
Published online: July 27, 2025
Processing time: 126 Days and 3.2 Hours
Conventional reusable endoscopes have high disinfection costs because of their large size. In this study, we compared the effectiveness, safety, and operation performance of the portable disposable large-channel endoscope that we de
To compare two gastroscopes in ESD for effectiveness and safety.
Ten Bama pigs were subjected to gastroscopy and ESD after general anesthesia. The experiment was completed by four experienced endoscopists. First, two endoscopists randomly selected the portable disposable large-channel or conventional gastroscope to complete gastroscopy procedures. The other two endosco
No significant differences in gastroscopy duration or in the integrity, sharpness, saturation, and brightness of the gastroscopic images were observed between the gastroscopes. For ESD, no significant differences in endoscopic operation performance, incision time, submucosal dissection time, total procedure time, total submucosal injection volume, specimen size, or success rate of en bloc resection were ob
The portable disposable large-channel endoscope can be used safely and effectively for gastroscopy and treatment.
Core Tip: The aim of this study was two-fold: (1) To evaluate the safety and feasibility of the portable disposable large-channel endoscope for gastrointestinal examination and endoscopic submucosal dissection through animal experiments; and (2) To evaluate the quality of the endoscopic images, operational performance, and treatment efficiency. The results showed that the portable disposable large-channel endoscope can be used safely and effectively for gastroscopy and treatment.
- Citation: Zhao CY, Ning B, Feng XX, Li HK, Zhang WG, Dong H, Chai NL, Linghu EQ. Comparison of a portable disposable large-channel gastroscope and a conventional reusable gastroscope in gastric endoscopic submucosal dissection. World J Gastrointest Surg 2025; 17(7): 105503
- URL: https://www.wjgnet.com/1948-9366/full/v17/i7/105503.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i7.105503
Gastrointestinal endoscopy is an important tool for diagnosing and treating digestive system diseases. Gastrointestinal endoscopy procedures are performed tens of millions of times each year in China. However, a conventional gastroscope system is expensive and bulky and requires cumbersome cleaning and disinfection steps and specific operation en
Due to the widespread application of gastrointestinal endoscopy, endoscopy-related iatrogenic infections should be addressed. The most common cause of endoscopy-related iatrogenic infections is inadequate procedures related to endoscope cleaning, disinfection, and drying[1]. Microbes can remain in an endoscope even after specialized cleaning and disinfection and thus can lead to the spread of infections. Therefore, an increasing number of teams have sought to develop disposable endoscopes, such as disposable bronchoscopes, disposable duodenoscopes, and disposable ureterorenoscopes, and the clinical benefits of such equipment have been confirmed[2].
Due to advances in medical device technology and the increasing demand for medical devices in clinical use, medical device miniaturization and portability have been prioritized, and portable endoscopes for various applications (e.g., portable laparoscopes, portable laryngoscopes, and portable colposcopies) have been developed. Portable medical devices can be used in a broad range of places and contexts and allow for the immediate diagnosis and rapid treatment of diseases.
To date, the research and development of portable disposable gastrointestinal endoscopes are relatively limited, and portable disposable gastrointestinal endoscopes can be applied only to the examination of the digestive tract and cannot be used for the treatment of digestive tract diseases. Therefore, we developed a portable disposable large-channel endoscope that can be used not only to examine the digestive tract but also to treat digestive system diseases. Our design includes a large-diameter working channel, which improves treatment capacity and efficiency. The aim of this study was two-fold: (1) To evaluate the safety and feasibility of using the developed portable disposable large-channel endoscope in gastrointestinal examination and endoscopic submucosal dissection (ESD) through animal experiments; and (2) To evaluate the quality of endoscopic images, operational performance, and treatment efficiency.
Ten Bama miniature pigs weighing approximately 25-30 kg were used in this study. After 2 days of fasting and 6 hours of water deprivation, the pigs were anesthetized with sodium pentobarbital (intravenous injection, 20 mg/kg) and mechanically ventilated. During the procedure, the pigs were kept in the left lateral position, and an experienced anesthesiologist maintained anesthesia and monitored vital signs. This study was reviewed and approved by the animal experiment committee of the Chinese PLA General Hospital (Beijing, China).
The portable disposable large-channel endoscope system was developed by the Department of Digestive Diseases of the Chinese PLA General Hospital. The system is composed of an endoscopic host and a disposable large-channel gas
Experimental method: Two experienced endoscopists randomly selected (coin toss) the portable disposable large-channel endoscope or conventional gastroscope to perform gastroscopy on each Bama miniature pig. A total of 31 standardized endoscopic images were obtained, namely, the oropharynx, upper and middle esophagus, lower esophagus, esophagogastric junction, gastric fundus, four walls of the upper gastric body (anterior wall, posterior wall, lesser curvature, greater curvature), four walls of the middle gastric body, four walls of the lower gastric body, anterior wall of the gastric angle, posterior wall of the gastric angle, lesser curvature of the gastric angle, greater curvature of the gastric angle, four walls of the gastric antrum, pylorus, four walls of the duodenal bulb, and descending part of duodenum. The total duration of each gastroscopy procedure was recorded. Images collected during each gastroscopy were independently evaluated and scored by the other two endoscopists, and any discrepancy was resolved by a third researcher.
Evaluation indicators: For each image, we referred to some articles[3-5] and evaluated the following aspects: (1) Image integrity-an image received one point when the anatomical structure in the image was intact; otherwise, the image received zero points; (2) Sharpness-an image received one point when the details of the anatomical structure in the image were clearly discernible; otherwise, the image received zero points; (3) Saturation-an image received one point when the colors were vibrant and met the clinical requirements; otherwise, the image received zero points; and (4) Brightness-an image received one point when the image was uniformly and fully illuminated; otherwise, the image received zero points.
Experimental method: Four endoscopists with ESD experience completed the ESD. Four hypothetical lesions with a diameter of approximately 2 cm in the gastric body and gastric antrum were examined for each pig. The hypothetical lesions were resected using a conventional or portable disposable large-channel gastroscope. Before the experiment, the four endoscopists first used the lottery method to determine the order in which they would operate, and then each endoscopist was given a sealed envelope containing the type of gastroscope to be used (disposable or conventional gastroscope) and operation site (gastric body or antrum). During the operation, the submucosal dissection time, total procedure time of ESD, total submucosal injection volume, specimen size, success rate of en bloc resection, muscular injury rate, and complications were recorded. After the operation, each surgeon scored the performance of the en
Evaluation indicators: The submucosal dissection time was defined as the time from the start of dissection after the end of the circumferential resection to the complete dissection of the specimen. The total procedure time of ESD was defined as the time from the start of the submucosal injection to the completion of the removal of the resection specimen. The total submucosal injection volume was defined as the total volume of fluid injected during the entire ESD operation. Mo
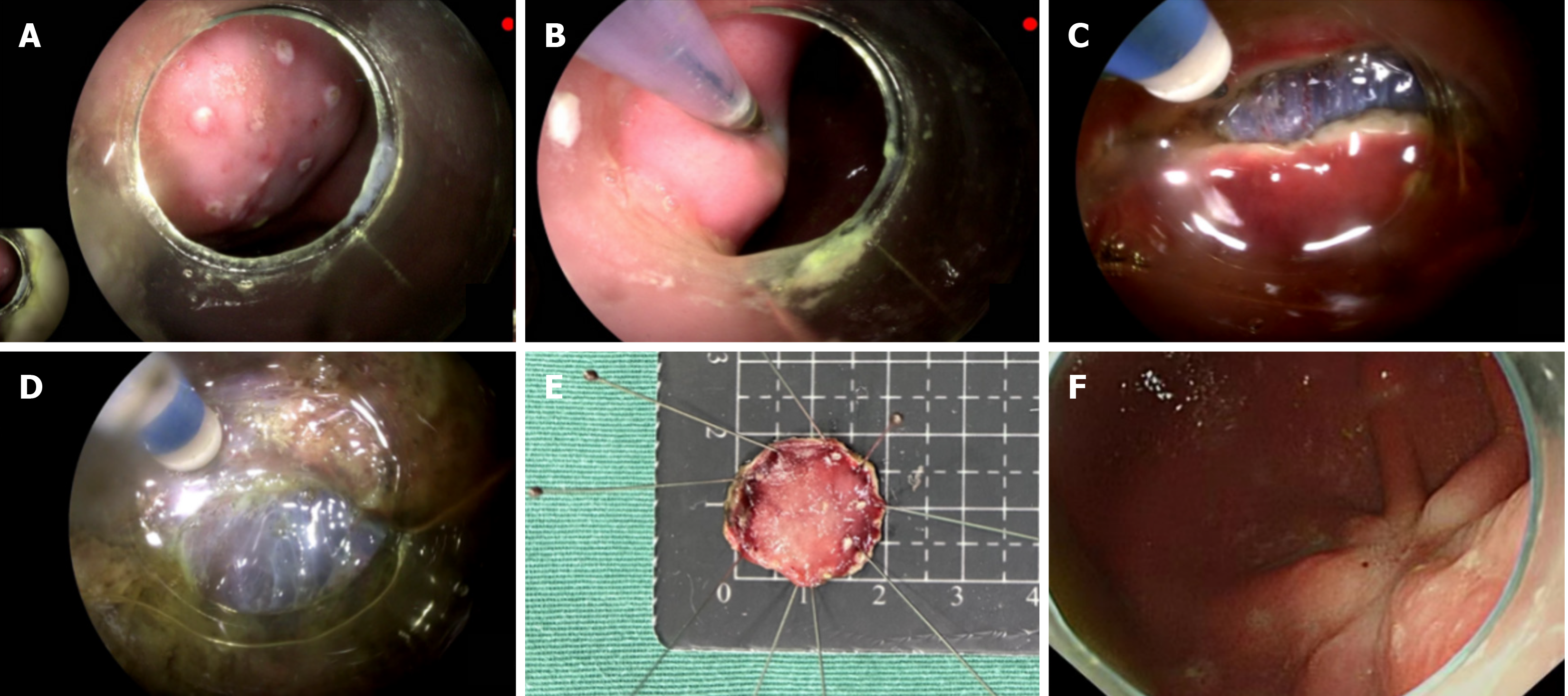
Operation procedure for ESD: The entire procedure included five steps: Marking, lifting, circumferential resection, dissection, and wound management. First, a transparent cap was installed on the front end of the gastroscope. After the gastroscope reached the hypothetical lesion site, the lesion was marked with an electrosurgical knife. Then submucosal injection (normal saline and a small amount of methylene blue solution) was performed at multiple sites on the periphery of the lesion to lift the lesion up completely. Subsequently, an electrosurgical knife was used in making an incision along the edge of the mucosa. After the circumferential resection was complete, the lesion was dissected until the specimen was completely removed. During the operation, the lesion was fully lifted up by multiple submucosal injections. When bleeding occurred, an electrosurgical knife or hot biopsy forceps were used to stop the bleeding. After the complete dissection of the lesion, the wound was observed for complications such as active bleeding, muscular injury, and perforation. When active bleeding, muscular injury, or perforation occurred, further hemostasis or closure of the per
We used SPSS version 25.0 (IBM SPSS Statistics, Chicago, IL, United States) for data analyses. The t-test, χ2 test, and Mann-Whitney U test were performed for the appropriate data types. P < 0.05 was considered statistically significant.
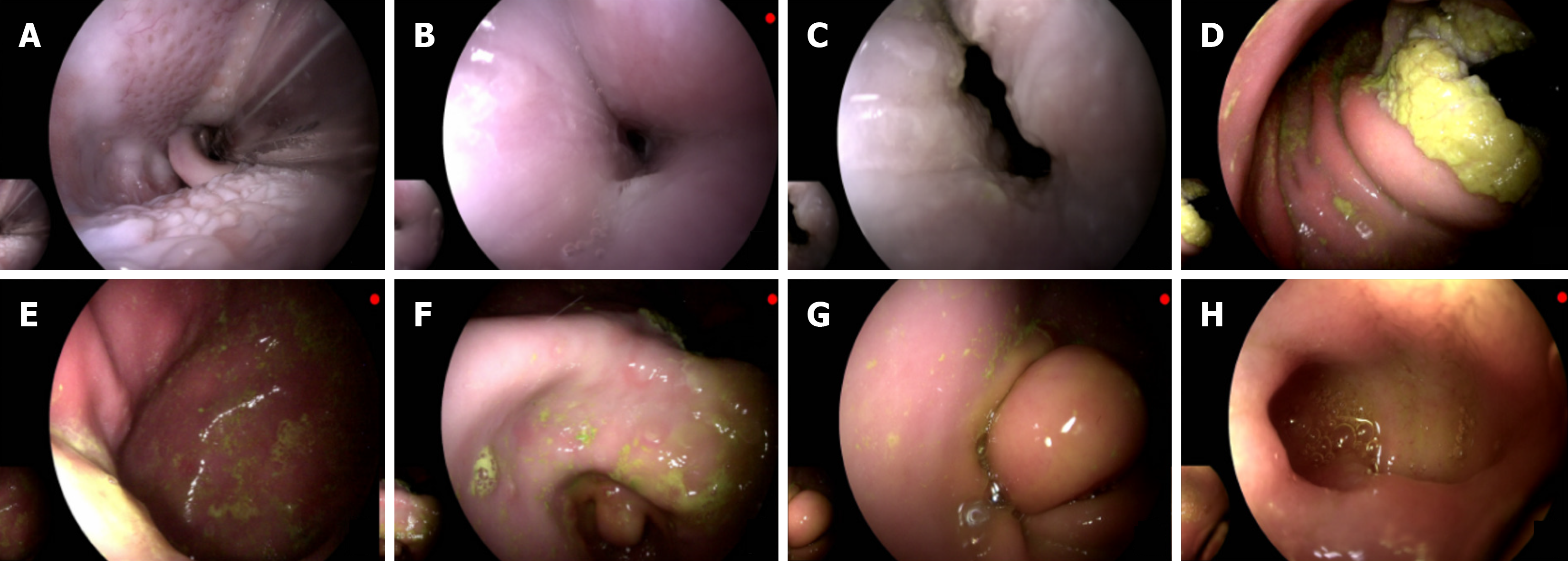
Gastroscopy was performed 10 times with the portable disposable large-channel gastroscope and 10 times with the conventional gastroscope. Each gastroscopy was successfully completed, and endoscopic images were successfully collected (Figure 2). No significant differences in the duration of gastroscopy (287.33 ± 38.15 s vs 284.78 ± 70.75 s; P = 0.673), image integrity scores (30.80 ± 0.42 points vs 30.90 ± 0.32 points; P = 0.739), image sharpness scores (30.50 ± 0.71 points vs 30.80 ± 0.42 points; P = 0.436), image contrast scores (30.10 ± 1.20 points vs 30.80 ± 0.42 points; P = 0.218), and image brightness scores (29.67 ± 1.23 points vs 30.67 ± 0.50 points; P = 0.203) (Table 1) were found between the portable disposable large-channel endoscope group and Olympus endoscope group (i.e. conventional gastroscope group).
| Experimental group (n = 10)1 | Control group (n = 10)2 | P value | |
| Duration of gastroscopy | 287.33 ± 38.15 | 284.78 ± 70.75 | 0.673 |
| Image integrity scores | 30.80 ± 0.42 | 30.90 ± 0.32 | 0.739 |
| Image sharpness scores | 30.50 ± 0.71 | 30.80 ± 0.42 | 0.436 |
| Image contrast scores | 30.10 ± 1.20 | 30.80 ± 0.42 | 0.218 |
| Image brightness scores | 29.67 ± 1.23 | 30.67 ± 0.50 | 0.203 |
ESD was performed 20 times with the portable disposable large-channel gastroscope (Figure 3) and 20 times with the conventional gastroscope. No significant differences in operational performance scores (image acquisition, water supply, air supply, suction, large-knob operation, small-knob operation, body rigidity, FOV, light illumination, tip flexibility, and working channel; all were P > 0.05) were found between the endoscopes. In the conventional gastroscope group, image acquisition, air supply, large-knob operation, small-knob operation, body rigidity, FOV, tip flexibility, and working channel completely met the clinical operation requirements in all 20 operations (all four points). Regarding the disposable portable gastroscope group, image acquisition, suction, FOV, light illumination, tip flexibility, and working channel completely met the clinical operation requirements in all 20 operations (all four points); small-knob operation was obviously defective in one operation, but the clinical operation was completed (two points; Table 2).
| Operational performance | Score | Experimental group | Control group | P value |
| Image acquisition | 0 | 0 | 0 | |
| 1 | 0 | 0 | ||
| 2 | 0 | 0 | ||
| 3 | 0 | 0 | ||
| 4 | 20 | 20 | ||
| Water supply | 0 | 0 | 0 | 0.602 |
| 1 | 0 | 0 | ||
| 2 | 0 | 0 | ||
| 3 | 3 | 1 | ||
| 4 | 17 | 19 | ||
| Air supply | 0 | 0 | 0 | 0.602 |
| 1 | 0 | 0 | ||
| 2 | 0 | 0 | ||
| 3 | 2 | 0 | ||
| 4 | 18 | 20 | ||
| Suction | 0 | 0 | 0 | 0.289 |
| 1 | 0 | 0 | ||
| 2 | 0 | 0 | ||
| 3 | 0 | 4 | ||
| 4 | 20 | 16 | ||
| Large-knob operation | 0 | 0 | 0 | 0.602 |
| 1 | 0 | 0 | ||
| 2 | 0 | 0 | ||
| 3 | 2 | 0 | ||
| 4 | 18 | 20 | ||
| Small-knob operation | 0 | 0 | 0 | 0.108 |
| 1 | 0 | 0 | ||
| 2 | 1 | 0 | ||
| 3 | 5 | 0 | ||
| 4 | 14 | 20 | ||
| Body rigidity | 0 | 0 | 0 | 0.183 |
| 1 | 0 | 0 | ||
| 2 | 0 | 0 | ||
| 3 | 5 | 0 | ||
| 4 | 15 | 20 | ||
| Field of view | 0 | 0 | 0 | |
| 1 | 0 | 0 | ||
| 2 | 0 | 0 | ||
| 3 | 0 | 0 | ||
| 4 | 20 | 20 | ||
| Light illumination | 0 | 0 | 0 | 0.183 |
| 1 | 0 | 0 | ||
| 2 | 0 | 0 | ||
| 3 | 0 | 5 | ||
| 4 | 20 | 15 | ||
| Tip flexibility | 0 | 0 | 0 | |
| 1 | 0 | 0 | ||
| 2 | 0 | 0 | ||
| 3 | 0 | 0 | ||
| 4 | 20 | 20 | ||
| Working channel | 0 | 0 | 0 | |
| 1 | 0 | 0 | ||
| 2 | 0 | 0 | ||
| 3 | 0 | 0 | ||
| 4 | 20 | 20 |
The en bloc resection of all hypothetical lesions was successfully completed using the portable disposable large-channel gastroscope and the conventional gastroscope. There were no significant differences in submucosal dissection time (median: 9.92 min [interquartile range (IQR): 8.19–16.30] vs 11.21 minutes [IQR: 9.06–13.25]; P = 0.864], total procedure time of ESD (median: 18.00 minutes [IQR: 12.11–23.80] vs 17.99 minutes [IQR: 14.82–20.51]; P = 0.938), total submucosal injection volume (median: 20.50 mL [IQR: 11.50–39.00] vs 20.50 mL [IQR: 14.00–23.00]; P = 0.767), and specimen size (median: 20.35 mm [IQR: 16.45–24.43] vs 18.72 minutes [IQR 17.04–21.12]; P = 0.501] between the portable disposable large-channel and conventional gastroscope groups. For both groups, no muscle layer injury occurred during ESD, and no complications occurred during or after ESD (Table 3).
| Experimental group | Control group | P value | |
| En bloc resection rate (%, n/n) | 100% (20/20) | 100% (20/20) | - |
| Submucosal dissection time (minutes) | 9.92 (8.19, 16.30) | 11.21 (9.06, 13.25) | 0.864 |
| Total procedure time of endoscopic submucosal dissection, minutes | 18.00 (12.11, 23.80) | 17.99 (14.82, 20.51) | 0.938 |
| Total submucosal injection volume (mL) | 20.50 (11.50, 39.00) | 20.50 (14.00, 23.00) | 0.767 |
| Specimen size, mm | 20.35 (16.45, 24.43) | 18.72 (17.04, 21.12) | 0.501 |
| Muscle layer injury | - | - | - |
| Complications | - | - | - |
Our team developed a portable disposable large-channel endoscope. In this study, we compared the effectiveness, safety, and operation performance of the portable disposable large-channel gastroscope and those of a reusable conventional gastroscope in gastroscopy and ESD.
Successful gastric examination is the most basic function of a gastroscope. In this study, both types of gastroscope facilitated the successful completion of endoscopic examinations without causing any intraoperative complication. The gastroscopes were used in the standardized examination of the esophagus, cardia, gastric fundus, gastric body, gastric angle, gastric antrum, pylorus, and duodenum. No significant difference in the duration of gastroscopy was found, indicating that the portable disposable large-channel endoscope is highly ergonomic and compatible. Endoscopists successfully completed endoscopic operations at first use, demonstrating the potentially wide application of the portable disposable large-channel endoscope. Obtaining the high-quality endoscopic images of various parts is an important component of endoscopic examinations. The obtained endoscopic images were evaluated for integrity, sharpness, saturation, and brightness. The images obtained using the portable disposable large-channel endoscope were basically intact, and their sharpness, saturation, and brightness were not different from those obtained using the conventional gastroscope. This result indicates that the portable disposable large-channel endoscope system can meet the performance requirements of upper gastrointestinal examinations.
Furthermore, we compared the application of two types of gastroscope in ESD. We focused on evaluating the performance of the portable disposable large-channel endoscope. The quality of the operating system directly affected the use of an endoscope, and the endoscopes were evaluated in terms of image acquisition, water supply, air supply, suction, large-knob operation, small-knob operation, body rigidity, FOV, lighting illumination, tip flexibility, and working channel. No statistically significant differences in the abovementioned aspects were found between the gastroscopes. However, the endoscopist gave an evaluation score of two points for small-knob operation in one operation involving the portable disposable large-channel endoscope because he believed that although he was able to complete the endoscopic operation, he found obvious defects in small-knob operation. The endoscopists gave an evaluation score of three points for small-knob operation in five endoscopic operations because of defects in the small-knob operation. Although the statistical results indicated that the gastroscopes showed no differences in small-knob operation, the sample size may have been extremely small for identifying a difference. Had the sample size been further expanded, the difference would have become noticeable. The endoscopists who reported defects in the small-knob operation noted that solely adjusting the small knob can cause the slight rotation of the large knob, resulting in the failure of the endoscope tip to accurately reach the expected position. Therefore, in subsequent research and development, we will further optimize the per
Out-of-hospital rescue, bedside diagnosis and treatment, on-site treatment in battlefield military operations, and remote and accompanying health care have introduced new requirements (simplified structure and high portability) for the development of endoscopic technology beyond complete functionality, such as the development of compact, portable, and intelligent endoscopes[6]. The outbreak of the coronavirus disease 2019 pandemic and the emergence of monkeypox virus have made reducing the risk of cross-infection an important medical goal. The United States Food and Drug Administration recommend that “health care facilities and manufacturers begin transitioning to duodenoscopes with disposable components to reduce risk of patient infection”[7]. To reduce the risk of infection, hospitals have further refined endoscope cleaning and disinfection procedures. According to the guidelines provided by the Gastroenterological Nurses College of Australia and Gastroenterological Society of Australia[8], reprocessing typically consists of eight steps: Precleaning, leak testing, manual cleaning, rinsing after cleaning, visual inspection, high-level disinfection, rinsing after high-level disinfection, and drying. However, although detailed cleaning and disinfection procedures have been de
Previous studies on portable disposable gastroscopes are limited[3,14,15], only focusing on the application of dis
This study had some limitations: (1) The sample size was small; thus, the performance of the disposable large-channel endoscope needs to be verified by studies with a larger sample size; (2) We preliminarily explored the application of the portable disposable large-channel endoscope in animals and will apply it clinically to verify its clinical efficacy; and (3) Although we expanded the working channel of the endoscope, the benefits of the large channel were not fully reflected in this study. Further experiments are needed to verify the benefits of this modification.
Using Bama miniature pigs as experimental subjects in this study offers several advantages. Bama miniature pigs have a gastrointestinal tract structure and physiological functions that are relatively similar to those of humans. Their stomach and intestinal anatomy, mucosal characteristics, and digestive processes share many similarities with human coun
To address the issue of the small sample size, in future studies, we plan to collaborate with multiple research centers. This multicenter approach will allow us to recruit a significantly larger number of experimental animals, such as increasing the number of Bama miniature pigs to at least 50. Additionally, we aim to include a diverse range of animal species, including other pig breeds and potentially nonporcine models with similar gastrointestinal characteristics to humans, like certain primates. This will enhance the generalizability of our findings and provide more robust evidence for the performance of the portable disposable large - channel endoscope.
For clinical verification of the endoscope's efficacy, we will design a prospective, randomized controlled clinical trial. We will enroll a sufficient number of patients with appropriate digestive tract diseases, such as early-stage gastric cancer or precancerous lesions suitable for ESD. The trial will be carefully monitored to assess not only the safety and effectiveness of the portable disposable large-channel endoscope but also patient-reported outcomes, such as comfort during the procedure. We will also closely observe any potential long-term complications, such as wound healing issues or recurrence of the disease.
Regarding the un-fully-realized benefits of the large-channel design, we will conduct a series of in vitro and in vivo experiments. In vitro, we will simulate various endoscopic scenarios, such as different levels of bleeding and the presence of different types of debris, to test the suction efficiency and the ability of the large-channel to prevent blockages more comprehensively. In vivo, we will perform ESD on a larger number of animals and use advanced imaging techniques, such as high-resolution confocal endomicroscopy, to visualize the treatment process in real-time and accurately evaluate how the large-channel affects the treatment efficiency and quality. Based on the results of these experiments, we will further optimize the design of the large-channel, for example, by adjusting its diameter, shape, or the material of the inner lining to enhance its performance.
The developed portable disposable large-channel endoscope can be used safely and effectively for gastroscopy procedures and treatment, can reduce iatrogenic infections, and broadens the location and context in which endoscopy is useful.
| 1. | Kovaleva J. Infectious complications in gastrointestinal endoscopy and their prevention. Best Pract Res Clin Gastroenterol. 2016;30:689-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | Ho E, Wagh A, Hogarth K, Murgu S. Single-Use and Reusable Flexible Bronchoscopes in Pulmonary and Critical Care Medicine. Diagnostics (Basel). 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 3. | Luo X, Ji M, Zhang S, Chen X, Zong Y, Zhang X, Hu H, Hao X, Shao L, Sun C, Shi H, Wang J, Wang B, Li P. Disposable versus reusable gastroscopes: a prospective randomized noninferiority trial. Gastrointest Endosc. 2022;96:250-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Bang JY, Hawes R, Varadarajulu S. Equivalent performance of single-use and reusable duodenoscopes in a randomised trial. Gut. 2021;70:838-844. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 65] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 5. | Sasaki S, Nishikawa J, Yanai H, Nakamura M, Nishimura J, Goto A, Kiyotoki S, Saito M, Hamabe K, Tanabe R, Nakamura Y, Tokiyama H, Hashimoto S, Okamoto T, Higaki S, Kurai S, Ogihara H, Hamamoto Y, Sakaida I. Image quality of a novel light-emitting diode (LED)-illuminated colonoscope. Endoscopy. 2016;48:934-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Wang J, Xie S, Li W, Yu D. New approach for enlargement of medical electronic endoscopic images. Appl Opt. 2002;41:2158-2163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | United States Food and Drug Administration. FDA recommends health care facilities and manufacturers begin transitioning to duodenoscopes with disposable components to reduce risk of patient infection (August 29, 2019). Available from: https://www.fda.gov/news-events/press-announcements/fda-recommends-health-care-facilities-and-manufacturers-begin-transitioning-duodenoscopes-disposable. |
| 8. | Devereaux BM, Athan E, Brown RR, Greig SM, Jones DM, Bailey FK, Wallis DJ, Singh R. Australian infection control in endoscopy consensus statements on carbapenemase-producing Enterobacteriaceae. J Gastroenterol Hepatol. 2019;34:650-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | McCafferty CE, Aghajani MJ, Abi-Hanna D, Gosbell IB, Jensen SO. An update on gastrointestinal endoscopy-associated infections and their contributing factors. Ann Clin Microbiol Antimicrob. 2018;17:36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 62] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 10. | Liang Z, Zhou G, Li Y, Pan F, Zeng J, Luan Z, Zhu Q, Xu Y, Zhang N, Xiang L, Jia Y, Sun G, Yang Y. Evaluation of a new developed disposable and portable bronchoscopy system. BMC Pulm Med. 2022;22:136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Trindade AJ, Copland A, Bhatt A, Bucobo JC, Chandrasekhara V, Krishnan K, Parsi MA, Kumta N, Law R, Pannala R, Rahimi EF, Saumoy M, Trikudanathan G, Yang J, Lichtenstein DR. Single-use duodenoscopes and duodenoscopes with disposable end caps. Gastrointest Endosc. 2021;93:997-1005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (1)] |
| 12. | Patterson K, Yap LC, Elamin M, Maccraith E, Muheilan M, Sharif A, McGuinness G, Darcy F, Brady C, Hennessey D. Evaluation of a new disposable flexible ureterorenoscope and comparison to an established disposable flexible ureterorenoscope: a prospective, observational study. Int Urol Nephrol. 2021;53:875-881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 13. | Hennessey DB, Fojecki GL, Papa NP, Lawrentschuk N, Bolton D. Single-use disposable digital flexible ureteroscopes: an ex vivo assessment and cost analysis. BJU Int. 2018;121 Suppl 3:55-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 68] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 14. | Huynh DK, Toscano L, Phan VA, Ow TW, Schoeman M, Nguyen NQ. Ultrathin disposable gastroscope for screening and surveillance of gastroesophageal varices in patients with liver cirrhosis: a prospective comparative study. Gastrointest Endosc. 2017;85:1212-1217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Kang D, Lim CH, Choi MG, Lee H, Kim JS, Cho YK, Park JM, Cho YS, Lee BI, Lee IS. An Operable, Portable, and Disposable Ultrathin Endoscope for Evaluation of the Upper Gastrointestinal Tract. Dig Dis Sci. 2019;64:1901-1907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/