Published online Jul 27, 2025. doi: 10.4240/wjgs.v17.i7.105387
Revised: April 2, 2025
Accepted: May 27, 2025
Published online: July 27, 2025
Processing time: 138 Days and 3.5 Hours
Surgical resection is the primary treatment for gastric cancer, but it often leads to slow recovery, high complications, and poor psychological health. The effectiveness of enhanced recovery after surgery (ERAS) as a new nursing model post-surgery remains uncertain.
To investigate the clinical effect of accelerated recovery nursing program based on multidisciplinary collaboration model in gastric cancer surgery.
A total of 120 patients who underwent radical gastrectomy at our hospital from January 2023 to December 2024 were included in the study. They were divided into two groups of 60 each: The control group, which received routine care, and the study group, which received ERAS based on multidisciplinary collaboration. Both groups received care until discharge. We compared gastrointestinal reco
The study group had significantly shorter defecation time, bowel sound recovery time, and flatus time compared to the control group (P < 0.05). The Hamilton Anxiety Scale and Hamilton Depression Rating Scale scores were also signi
The ERAS based on multidisciplinary collaboration in patients undergoing radical gastrectomy can accelerate postoperative recovery, reduce the occurrence of complications, and improve psychological state, quality of life, sleep quality and nursing satisfaction.
Core Tip: This study evaluates the clinical effects of an enhanced recovery after surgery program based on a multidisciplinary collaboration model in gastric cancer patients undergoing radical gastrectomy. A total of 120 patients were divided into a control group receiving routine care and a study group receiving enhanced recovery after surgery. Results showed that the study group had significantly shorter recovery times for defecation, bowel sounds, and flatus, along with lower anxiety and depression scores, improved sleep quality, fewer complications, and higher Short Form 36 Health Survey scores and nursing satisfaction, indicating enhanced postoperative recovery and overall well-being.
- Citation: Tang YH, Zhang J. Clinical effect of enhanced recovery after surgery based on multidisciplinary collaboration model in postoperative gastric cancer surgery. World J Gastrointest Surg 2025; 17(7): 105387
- URL: https://www.wjgnet.com/1948-9366/full/v17/i7/105387.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i7.105387
Gastric cancer (GC) is the fifth most common cancer globally, with over a million new cases diagnosed in 2020[1]. It is also the third leading cause of cancer-related deaths, resulting in approximately 768000 fatalities that year. Multiple factors contribute to GC, including genetics, Helicobacter pylori infection, diet, socioeconomic status, and lifestyle[2]. Unfortunately, its prognosis is poor, as most patients are diagnosed at an advanced stage, particularly in developing countries[3]. GC is a highly prevalent and deadly cancer in China[4]. GC ranks second in both incidence and mortality rates among malignant tumors in China[5]. Additionally, in China, GC is the second most common malignant tumor in men and the third in women, and it ranks third in mortality for both sexes[6]. The high incidence of GC not only has a serious impact on the quality of life of patients, but also brings a heavy economic burden to families and society[7].
At present, the treatment of GC mainly includes surgery, chemotherapy and radiotherapy. Among them, surgery is considered to be the only effective way to cure GC, especially in patients in the early and intermediate stages[8]. However, although surgery can effectively remove the tumor, the occurrence of postoperative complications and the patient’s recovery process often affect the treatment effect and the patient’s quality of life[9,10]. Therefore, the importance of post-operative care is becoming increasingly prominent. Proper postoperative care can not only promote early recovery, but also improve prognosis and quality of life.
Introduced in 2001, the enhanced recovery after surgery (ERAS) protocol emphasizes patient recovery over quick discharge[11]. Over the last decade, various surgical subspecialties across the United States have embraced ERAS protocols to boost patient recovery[12]. ERAS programs are evidence-based multimodal protocols aimed at accelerating postoperative recovery[13]. Key components include preoperative counseling, nutritional optimization, standardized pain management, and early mobilization. Since its introduction in 1997, ERAS has been extensively studied, demonstrating a reduction in operative complications and promoting rapid recovery[14]. In gynecology, ERAS has been widely adopted for patients with both cancer and benign conditions[15]. This model emphasizes not only the collaboration of multidisciplinary teams such as surgeons, anesthesiologists, and nursing staff, but also the individualized care and psychological support of patients[16]. Studies have shown that accelerated recovery surgery protocols can accelerate functional recovery and improve postoperative outcomes after gynecologic surgery[17]. In addition, GC patients often face a variety of adverse reactions after surgery, including pain, nausea, vomiting, malnutrition, etc., which not only affect the patient’s physical recovery, but also may lead to psychological anxiety and depression[18]. Studies have shown that Chinese GC patients are anxious and anxious before surgery and/or the prevalence of depression is 20.75%[19], which further aggravates the patient’s distress. Therefore, the rapid recovery care program can provide a systematic solution to these problems through multidisciplinary collaboration. In summary, this study aimed to evaluate the clinical effects of rapid recovery nursing program based on multidisciplinary collaboration model for patients with GC in terms of improving postoperative recovery, reducing the incidence of complications, and improving quality of life. Previously provided a nursing rationale for postoperative care for patients with GC.
A retrospective study was performed on 120 patients with radical gastrectomy with complete clinical data admitted to our hospital from January 2023 to December 2024, and were divided into control group and study group according to different nursing methods, with 60 cases in each group. The control group received routine care, the study group received ERAS based on multidisciplinary collaboration, and the two groups continued nursing until the patients were discharged.
Inclusion criteria: (1) The patients met the diagnostic criteria for GC and received radical gastrectomy treatment; (2) The patient had no history of mental illness and normal cognitive function; and (3) Complete clinical data.
Exclusion criteria: (1) Patients with systemic chronic diseases, such as hypertension, diabetes, etc.; (2) Patients with severe organ dysfunction (such as kidney, heart, liver); and (3) The clinical data are incomplete.
The study was approved by the Research Ethics Committee of our institute and was carried out in accordance with the Declaration of Helsinki and its subsequent amendments. Since it is a retrospective study, the Ethics Committee exempts informed consent for this study.
Control group: The control group was given routine care measures. Before surgery, explain to the patient and their family relevant knowledge about GC, treatment measures, etc., introduce the surgical procedure, precautions, and key points of postoperative recovery, and advise the patient to relax and actively cooperate with treatment. Develop a perioperative diet plan. Postoperatively, explain recovery knowledge to the patient, guide patient activity based on voluntary participation, or have nurses assist with passive exercise. Strengthen postoperative monitoring to prevent complications. After bowel sounds return, remove the gastric tube and guide the patient to gradually start eating. Allow water intake 8 hours post-surgery, introduce liquid foods at 12 hours, and gradually transition to a regular diet. Provide routine pain management and psychological counseling, as well as other basic nursing care services. Communicate to alleviate negative emotions, and administer medications scientifically and rationally according to doctor’s orders.
Study group: The study group receives ERAS based on multidisciplinary collaboration. Including: (1) Establish a multidisciplinary intervention team: The team members include doctors, head nurses, nurses (wards and operating rooms), anesthesiologists, dietitians and rehabilitation therapists. A rapid recovery nursing program based on multidisciplinary collaboration was developed for patients undergoing radical gastrectomy, with two team members responsible for the collection of various clinical data, the head nurse leading the multidisciplinary communication, decision-making and promotion of the nursing plan, and the nurse being responsible for the specific implementation of the program; (2) Preoperative assessment, health education and psychological counseling: After the patient is admitted to the hospital, the patient and his family are introduced to the rapid recovery surgical nursing measures based on multidisciplinary collaboration through oral education, health handbooks, exhibition boards and WeChat platform, etc., and the active cooperation of the patient and family is obtained. Through communication, we can grasp the psychological situation of patients in a timely manner and provide them with humanized psychological guidance; (3) Nutrition management: Evaluate the nutritional status of patients, understand the overall nutritional status of patients, and provide a basis for doctors to formulate intervention plans; (4) Sleep management: Evaluate the cause and degree of sleep disorders in patients, strengthen communication with patients with insomnia caused by psychological reasons, improve the environment and services, enhance patients’ sense of security, enhance their sense of pleasure, and then improve their sleep quality; for patients with simple insomnia, sedative-hypnotic drugs should be applied according to the doctor’s instructions, and the patient’s drug response should be observed to ensure that the patient has enough sleep; (5) Diet management: Instruct patients to fast protein-rich food for 6 hours before anesthesia, carbohydrates for 4 hours before anesthesia, and water for 2 hours before anesthesia. After surgery, the dietary guidance of patients should be strengthened, and the gastrointestinal reactions should be observed to determine whether there is digestive discomfort, such as abdominal distension and abdominal pain, and be dealt with in time once found. Generally speaking, you can be fed some liquid diet 6 hours after surgery, and then gradually transition to a normal diet, mainly high-vitamin and high-protein foods; (6) Early activity nursing: 3 days after surgery, after the patient’s condition is stable, guide the patient to get out of bed as soon as possible and move slightly, when fully awake, try to maintain the semi-lateral decubitus position, oblique lateral decubitus position, carry out some simple voluntary activities on the bed, and get out of bed when the body is in good condition, but the amount of activity needs to be controlled, and slowly increase according to the changes in the condition until it returns to normal activity; and (7) Pain nursing: Patients complaining of pain are treated with self-controlled intravenous analgesic pumps to relieve pain and increase comfort.
Postoperative gastrointestinal function recovery: Time to recovery of bowel sounds, time to gas, time to first bowel movement.
Mental status: Hamilton Anxiety Scale (HAMA) and Hamilton Depression Rating Scale (HAMD)[20]: In the HAMA scale, there are 14 items on a 5-point scale from 0 to 4. The higher the score, the greater the level of anxiety. In the HAMD scale, there are 17 items, each of which is scored (1, 2, 3, 7, 8, 9, 10, 11, 15, 17 on a scale of 0-4, 4, 5, 6, 12, 13, 14, 16 on a scale of 0-2). The higher the score, the more severe the level of depression.
Short Form 36 Health Survey score[21]: The higher the final score, the better the patient’s quality of life (out of 100). The Short Form 36 Health Survey (SF-36) has eight items (general health, social functioning, physical functioning, emotional functioning, physiological functioning, physical pain, mental health, and vitality).
Sleep quality[22]: To assess the patient’s sleep quality by the Pittsburgh Sleep Quality Index (PSQI), which includes 7 dimensions of sleep efficiency, quality, interference, time, hypnotic drugs, time to sleep onset, and daytime dysfunction (19 items in total). A four-point scale is used to score a maximum of 21 points. The higher the score, the worse the sleep quality. The Cronbach α coefficient of this scale is 0.710, indicating good reliability and validity.
Postoperative complications: Postoperative complications include incision infection, bleeding, and intestinal obstruction.
Nursing satisfaction[23]: Patients’ nursing satisfaction was assessed using our self-made nursing satisfaction questionnaire. A score below 60 is “unsatisfactory”, indicating that patients do not perceive clinical care to have a significant effect on their improvement in psychological state, comfort, and pain levels; 60-85 points of “basically satisfied”: Patients believe that clinical nursing work has a certain impact on the improvement of their psychological condition, comfort and pain level; a score of more than 85 is “very satisfied”: Indicates that patients perceive clinical care work to have a significant impact on their psychological well-being, comfort, and improvement in pain levels. Total satisfaction rate = [(basic satisfaction + satisfaction) number of cases/total number of cases] × 100% of 100%.
Use SPSS version 26.0 to conduct data analysis. Continuous variables are reported as mean ± SD and compared between groups using independent t-tests to identify significant differences. Categorical variables are expressed as counts and percentages [n (%)] and analyzed with the χ2 test for group comparisons. A P value of less than 0.05 is considered statistically significant.
Among the 60 patients in the study group, there were 36 males and 24 females, with a median age of 49 years (interquartile range: 33-57). In the control group, 35 were males and 25 were females, with a median age of 48 years (interquartile range: 32-58). Baseline characteristics between the two groups were similar and comparable, as shown in Table 1.
| Index | Study group (n = 60) | Control group (n = 60) | P value |
| Median age (25th-75th IQR), years | 49 (33-57) | 48 (32-58) | 0.943 |
| Sex | 0.865 | ||
| Male | 36 (60.0) | 35 (58.3) | |
| Female | 24 (40.0) | 25 (41.7) | |
| BMI (kg/m2) | 23.51 ± 3.32 | 23.46 ± 3.21 | 0.673 |
| Smoking history (n) | 0.534 | ||
| Yes | 25 (41.7) | 23 (38.3) | |
| No | 35 (58.3) | 37 (61.7) | |
| Drinking history (n) | 0.476 | ||
| Yes | 22 (36.7) | 20 (33.3) | |
| No | 38 (63.3) | 40 (66.7) | |
| Concomitant diseases | 0.817 | ||
| Diabetes | 12 (20.0) | 11 (18.3) | |
| Hypertension | 16 (26.7) | 18 (30.0) | |
| Lung disease | 10 (16.7) | 9 (15) | |
| Education level | 0.653 | ||
| High school and below | 26 (43.3) | 27 (45.0) | |
| University and above | 34 (56.7) | 33 (55.5) |
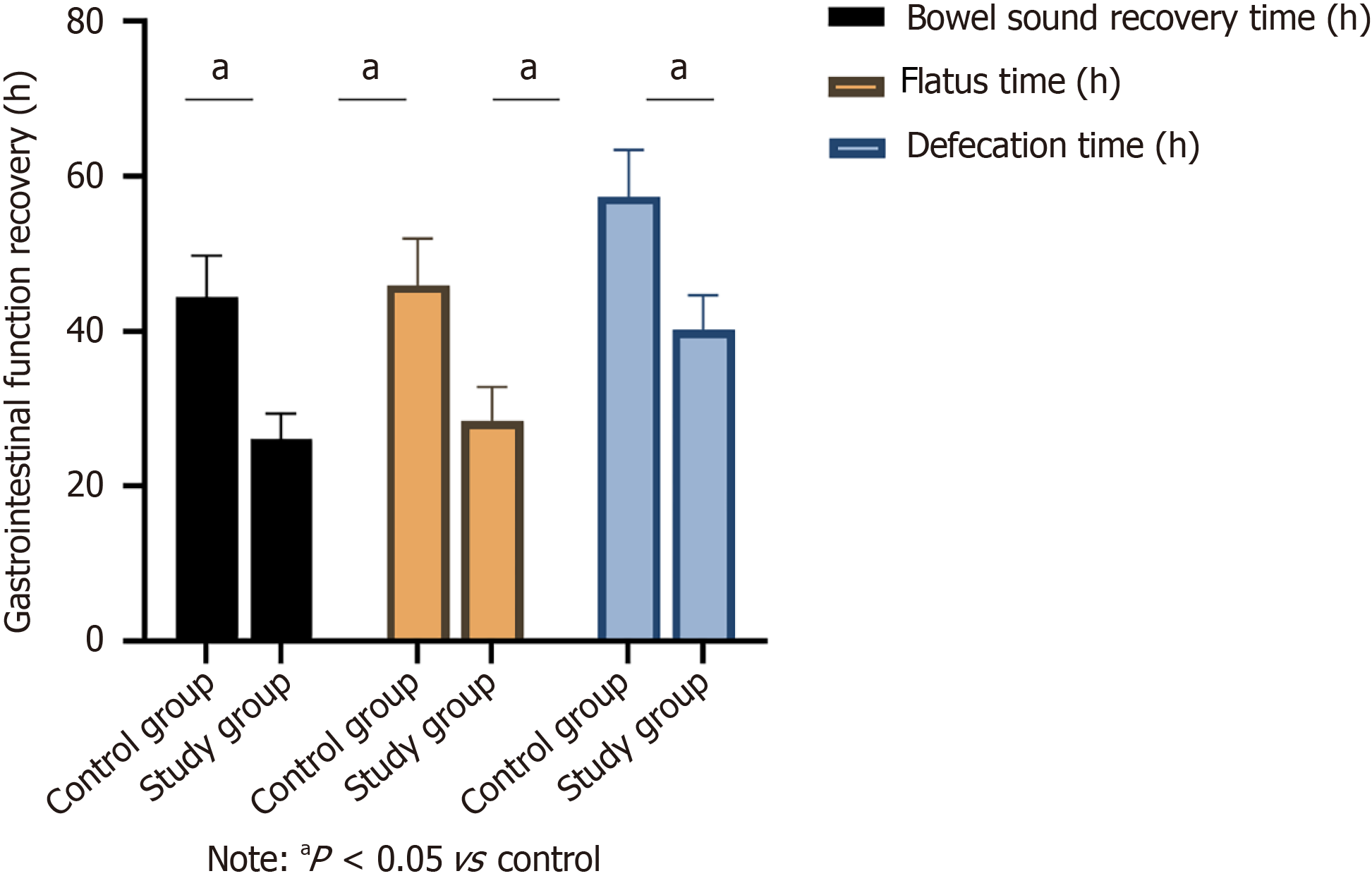
After the nursing intervention, the study group had shorter recovery times for defecation time, bowel sound recovery time and flatus time compared to the control group, with statistically significant differences (P < 0.05), as illustrated in Figure 1.
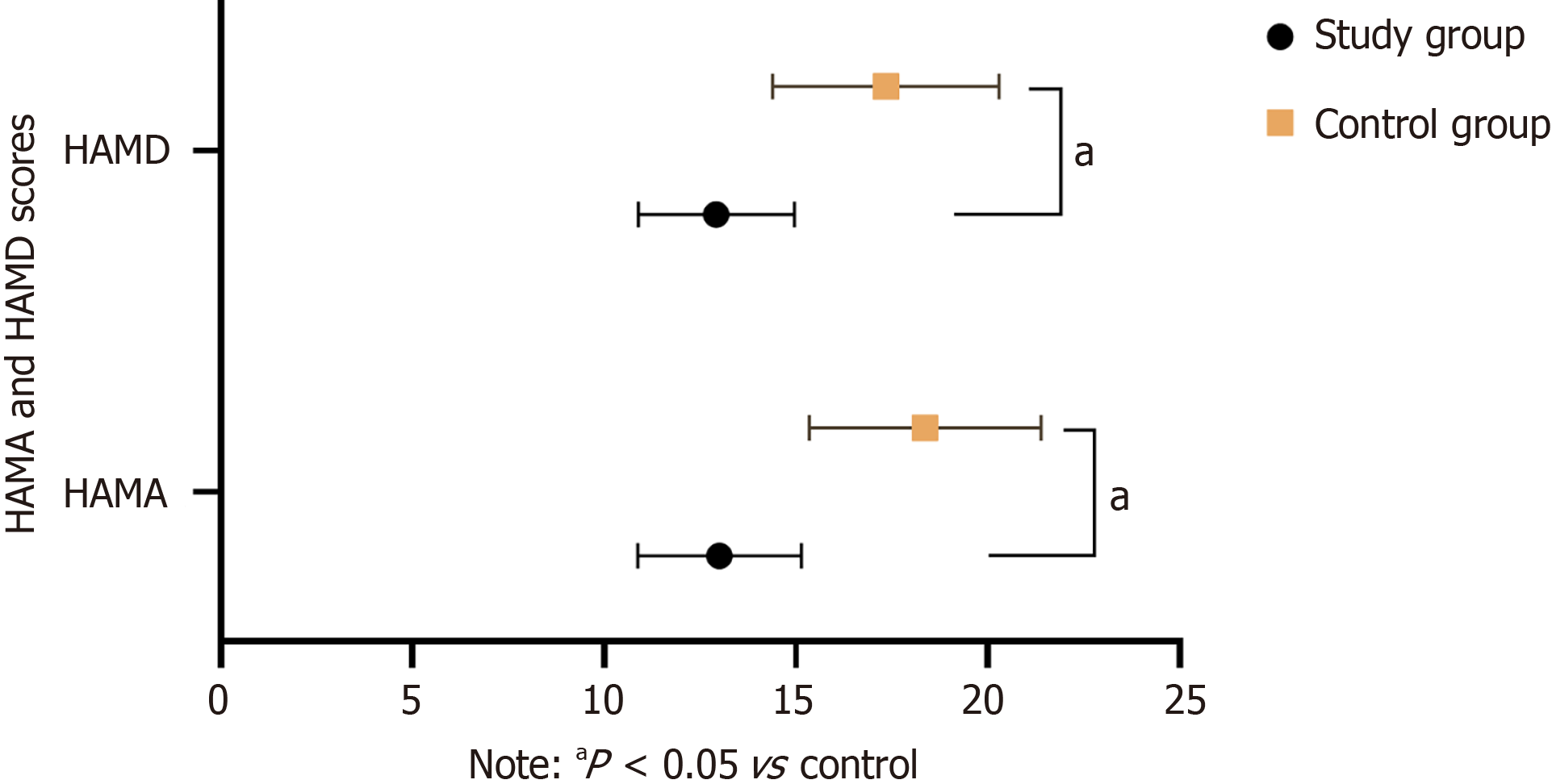
There was no significant difference in HAMA and HAMD scores between the two groups before nursing (P > 0.05). The scores of HAMA and HAMD in the two groups were significantly lower than those before nursing, and those in the study group were significantly lower than those in the control group (13.01 ± 3.02 vs 18.37 ± 3.02 points, 12.93 ± 2.04 vs 17.35 ± 2.95 points; Figure 2).
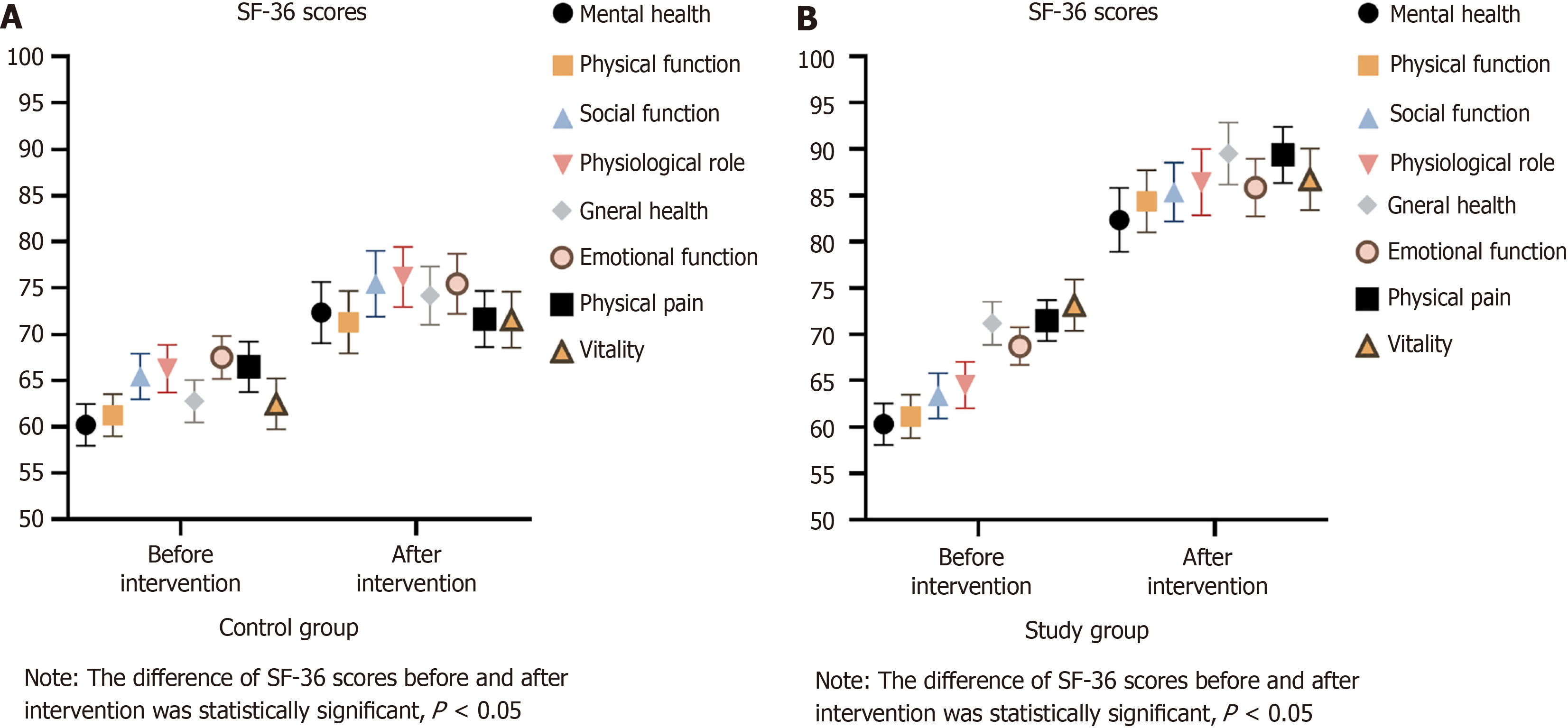
There was no statistically significant difference in pre-care visual analogue scale scores between the two groups (P > 0.05). The SF-36 score in the study group was significantly higher than that in the control group (P < 0.05; Figure 3).
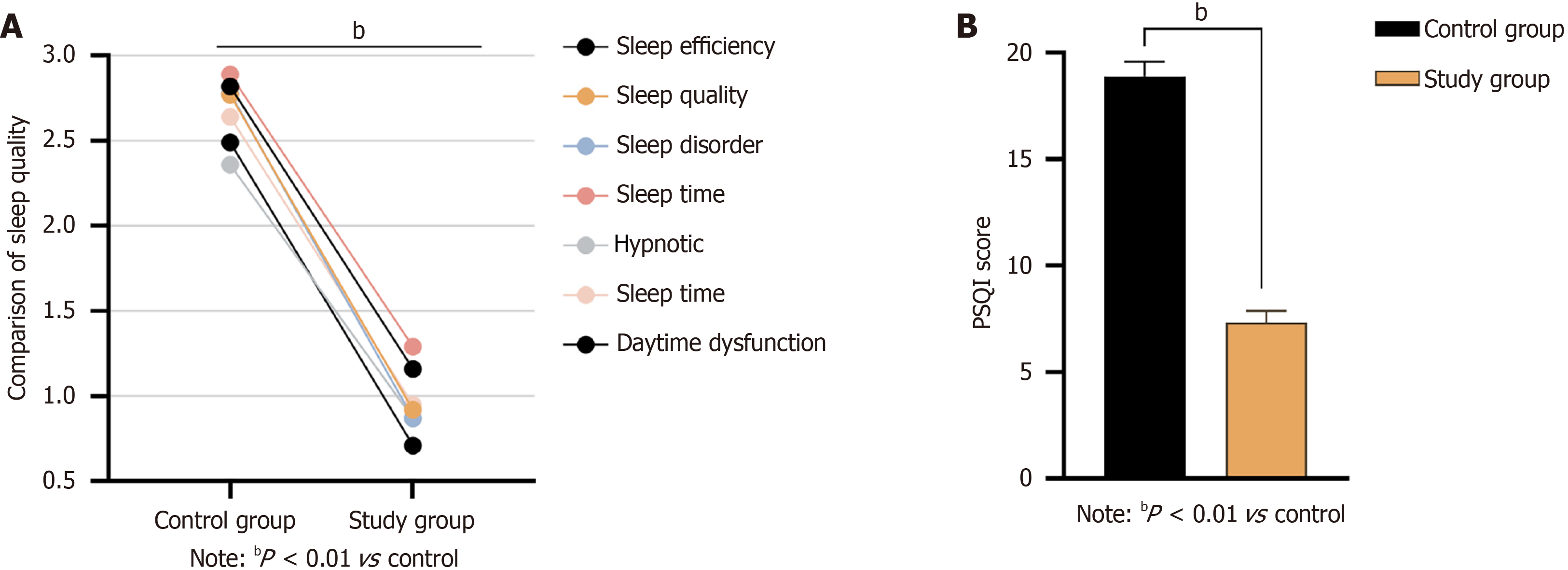
All PSQI scores and total scores in the study group were lower than those in the control group (P < 0.01), as shown in Figure 4.
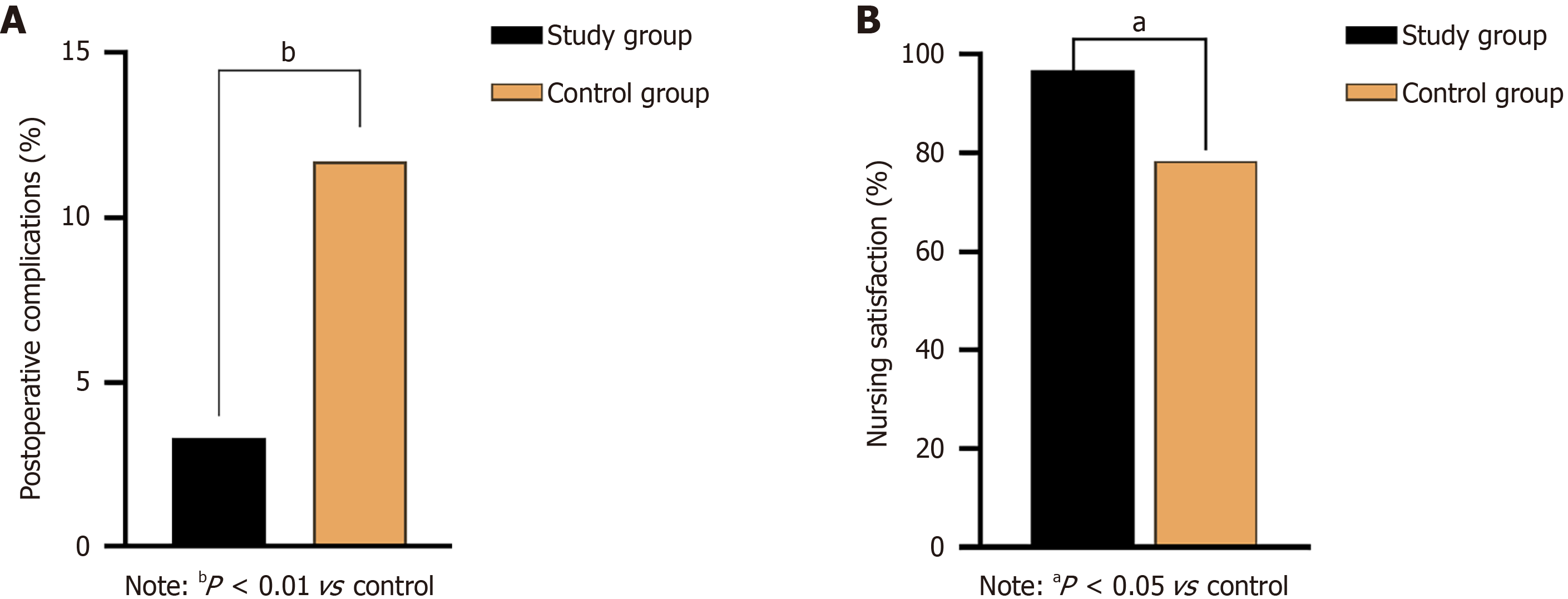
The postoperative complication rate in the study group was 3.3% (2/60), which was significantly lower than that in the control group [11.7% (7/60), P < 0.01; Figure 5A].
The satisfaction rate with care in the study group was 96.7% (58/60), which was higher than that in the control group [78.3% (47/60), P < 0.05; Figure 5B].
At present, the cause of GC is not clear, but studies have shown that Helicobacter pylori infection, regional environment, precancerous lesions, genetic factors and dietary habits may all be related to the occurrence of GC. Radical gastrectomy is a common treatment for the disease, however, patients tend to recover slowly due to the trauma of surgery, and the risk of malnutrition increases significantly due to the inability to eat normally[24]. This not only affects the healing of the incision, but may also reduce the patient’s immunity and increase the incidence of complications[25,26]. Therefore, it is particularly important to strengthen the postoperative care of patients undergoing radical gastrectomy. With the deepening of perioperative nursing research, the multidisciplinary collaboration model has been further integrated. In this model, nursing staff, as an important member of the rapid recovery surgical team, can effectively promote the rapid recovery of patients, improve the quality of care, and promote the development of nursing disciplines.
The results of this study showed that the defecation time, bowel sound recovery time and flatus time of the patients in the study group were significantly shorter than those in the control group (P < 0.05). In addition, the scores of the study group in each dimension of the SF-36 scale were also significantly higher than those of the control group (P < 0.05), indicating that the rapid recovery nursing model based on multidisciplinary collaboration can improve the quality of life of patients and accelerate the recovery process. This finding is consistent with the existing literature, indicating that the rapid recovery nursing model based on multidisciplinary collaboration can accelerate the postoperative rehabilitation process of patients[27,28].
In terms of the assessment of anxiety and depression, there was no significant difference in the HAMA and HAMD scores between the two groups before nursing (P > 0.05), but the scores of both groups decreased significantly after care, and the improvement was greater in the study group. The results indicated that multidisciplinary nursing intervention had a significant effect in alleviating postoperative anxiety and depression. This further underscores the importance of psychological support in surgical recovery. This is generally consistent with the results of previous studies[29,30].
The results of this study also suggest that the SF-36 score of the study group was significantly higher than that of the control group (P < 0.05), indicating that the multidisciplinary nursing plan could effectively improve the quality of life of patients. In addition, all PSQI scores and total scores in the study group were lower than those of the control group (P < 0.01) in the assessment of sleep quality, which further reflects the positive impact of multidisciplinary care on improving the overall health of patients. Wang et al[31] demonstrated that enhanced postoperative nursing interventions significantly reduce hospitalization time and costs, accelerate gastrointestinal recovery, and improve postoperative nutritional status and quality of life for patients undergoing GC surgery, aligning with the findings of this research.
In addition, the results of this study also show that the incidence rate of postoperative complications in the study group was 3.3% (2/60), which was significantly lower than that in the control group [11.7% (7/60), P < 0.01], indicating the effectiveness of multidisciplinary collaborative care in reducing postoperative complications. Finally, the satisfaction rate of the study group was as high as 96.7% (58/60), which was significantly higher than that of the control group [78.3% (47/60), P < 0.05], indicating that patients had a high recognition and satisfaction with multidisciplinary collaborative nursing, which further verified the effectiveness and feasibility of this nursing model. Previous studies have reported similar results[32,33].
The possible reasons for this analysis are that the rapid recovery care model based on multidisciplinary collaboration can carry out targeted interventions. The rapid recovery concept aims to reduce undesirable stimuli in the perioperative period, reduce the risk of surgery, and alleviate the pain of the patient. Specific measures include strengthening thermal insulation management to maintain normothermia, promoting blood circulation in the lower extremities to prevent deep vein thrombosis, encouraging patients to perform voluntary activities as soon as possible, and gradually drinking water and resuming diet within 6 hours after surgery. In addition, analgesia with an analgesic pump and avoidance of opioid use can help reduce pain and promote recovery.
This study employs a multidisciplinary nursing approach, providing patients with health education, psychological intervention, and postoperative complication care measures, thereby offering optimal nursing intervention and postoperative rehabilitation from multiple perspectives. Compared to traditional nursing, it improves patients’ quality of life and nursing satisfaction, consistent with the findings of quality management studies. Our results indicate that multidisciplinary integrated nursing intervention can reduce negative emotions and postoperative complications in patients undergoing GC surgery, and aid in the recovery of gastrointestinal function. We recommend the clinical application of multidisciplinary integrated nursing for patients undergoing GC surgery.
There are some limitations to this retrospective single-center study. First, the sample size of this study was relatively small, including only 60 patients in each group, which may affect the extrapolation of the results. Second, there may be certain confounding factors, such as medication and blood pressure control, that may affect the accuracy of care outcomes. Thirdly, because it is a retrospective study, it is not possible to judge the influencing factors and causal relationships of nursing outcomes. Future studies will further use a multicenter, prospective, large-sample randomized controlled design to further validate the results of this study.
In conclusion, the application of the rapid recovery nursing program based on multidisciplinary collaboration after radical gastrectomy significantly promoted the recovery of gastrointestinal function, improved the quality of life, psychological state and sleep quality, reduced the incidence of complications, and improved nursing satisfaction. This provides strong support for the promotion of the multidisciplinary collaborative rapid recovery nursing model in clinical practice in the future.
| 1. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 68679] [Article Influence: 13735.8] [Reference Citation Analysis (201)] |
| 2. | Yusefi AR, Bagheri Lankarani K, Bastani P, Radinmanesh M, Kavosi Z. Risk Factors for Gastric Cancer: A Systematic Review. Asian Pac J Cancer Prev. 2018;19:591-603. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 171] [Reference Citation Analysis (0)] |
| 3. | Necula L, Matei L, Dragu D, Neagu AI, Mambet C, Nedeianu S, Bleotu C, Diaconu CC, Chivu-Economescu M. Recent advances in gastric cancer early diagnosis. World J Gastroenterol. 2019;25:2029-2044. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 307] [Cited by in RCA: 314] [Article Influence: 44.9] [Reference Citation Analysis (3)] |
| 4. | Tan Z, Wang W, Peng J, Zhou Z, Pan J, Peng A, Cao H, Fan W. Impact of Amarogentin on Gastric Carcinoma Cell Multiplication, Apoptosis and Migration via circKIF4A/miR-152-3p. J Immunol Res. 2022;2022:2156204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 5. | Sun K, Xu MQ, Zhang HJ, Zhang DD, Yue W, Ma MM, Tao L, Zhang WJ. Active Stat3 and Her-2 as combined survival predictors show superiority to TNM staging system for postoperative patients with gastric cancer. Am J Transl Res. 2022;14:2317-2330. [PubMed] |
| 6. | Lazzarini PA, Cramb SM, Golledge J, Morton JI, Magliano DJ, Van Netten JJ. Global trends in the incidence of hospital admissions for diabetes-related foot disease and amputations: a review of national rates in the 21st century. Diabetologia. 2023;66:267-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 31] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 7. | Hamashima C. Current issues and future perspectives of gastric cancer screening. World J Gastroenterol. 2014;20:13767-13774. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 123] [Cited by in RCA: 142] [Article Influence: 11.8] [Reference Citation Analysis (1)] |
| 8. | Tan Z. Recent Advances in the Surgical Treatment of Advanced Gastric Cancer: A Review. Med Sci Monit. 2019;25:3537-3541. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 111] [Cited by in RCA: 325] [Article Influence: 46.4] [Reference Citation Analysis (0)] |
| 9. | Lyadov VK, Kozyrin IA, Kovalenko ZA. [Radical surgical treatment of elderly patients with gastric cancer]. Vopr Onkol. 2016;62:443-446. [PubMed] |
| 10. | Murakami Y, Saito H, Kono Y, Shishido Y, Kuroda H, Matsunaga T, Fukumoto Y, Osaki T, Ashida K, Fujiwara Y. Combined analysis of the preoperative and postoperative prognostic nutritional index offers a precise predictor of the prognosis of patients with gastric cancer. Surg Today. 2018;48:395-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Zhang JT, Tang YC, Lin JT, Dong S, Nie Q, Jiang BY, Yan HH, Wen ZW, Wu Y, Yang XN, Wu YL, Zhong WZ. Prophylactic air-extraction strategy after thoracoscopic wedge resection. Thorac Cancer. 2018;9:1406-1412. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Mark J, Argentieri DM, Gutierrez CA, Morrell K, Eng K, Hutson AD, Mayor P, Szender JB, Starbuck K, Lynam S, Blum B, Akers S, Lele S, Paragh G, Odunsi K, de Leon-Casasola O, Frederick PJ, Zsiros E. Ultrarestrictive Opioid Prescription Protocol for Pain Management After Gynecologic and Abdominal Surgery. JAMA Netw Open. 2018;1:e185452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 106] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 13. | Ljungqvist O, Scott M, Fearon KC. Enhanced Recovery After Surgery: A Review. JAMA Surg. 2017;152:292-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1487] [Cited by in RCA: 2432] [Article Influence: 270.2] [Reference Citation Analysis (1)] |
| 14. | Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78:606-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1691] [Cited by in RCA: 1817] [Article Influence: 62.7] [Reference Citation Analysis (4)] |
| 15. | Eskicioglu C, Forbes SS, Aarts MA, Okrainec A, McLeod RS. Enhanced recovery after surgery (ERAS) programs for patients having colorectal surgery: a meta-analysis of randomized trials. J Gastrointest Surg. 2009;13:2321-2329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 208] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 16. | Aarts MA, Rotstein OD, Pearsall EA, Victor JC, Okrainec A, McKenzie M, McCluskey SA, Conn LG, McLeod RS; iERAS group. Postoperative ERAS Interventions Have the Greatest Impact on Optimal Recovery: Experience With Implementation of ERAS Across Multiple Hospitals. Ann Surg. 2018;267:992-997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 138] [Article Influence: 19.7] [Reference Citation Analysis (1)] |
| 17. | Miralpeix E, Nick AM, Meyer LA, Cata J, Lasala J, Mena GE, Gottumukkala V, Iniesta-Donate M, Salvo G, Ramirez PT. A call for new standard of care in perioperative gynecologic oncology practice: Impact of enhanced recovery after surgery (ERAS) programs. Gynecol Oncol. 2016;141:371-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 119] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 18. | Lu S, Yan M, Li C, Yan C, Zhu Z, Lu W. Machine-learning-assisted prediction of surgical outcomes in patients undergoing gastrectomy. Chin J Cancer Res. 2019;31:797-805. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Xu L, Pan Q, Lin R. Prevalence rate and influencing factors of preoperative anxiety and depression in gastric cancer patients in China: Preliminary study. J Int Med Res. 2016;44:377-388. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 20. | Zheng JH, Sun WH, Ma JJ, Wang ZD, Chang QQ, Dong LR, Shi XX, Li MJ, Gu Q, Chen SY, Li DS. Differences in neuroanatomy and functional connectivity between motor subtypes of Parkinson's disease. Front Neurosci. 2022;16:905709. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 21. | Shang Y, Zhang Y, Liu J, Chen L, Yang X, Zhu Z, Li D, Deng Y, Zhou Z, Lu B, Fu CG. Decreased E2F2 Expression Correlates with Poor Prognosis and Immune Infiltrates in Patients with Colorectal Cancer. J Cancer. 2022;13:653-668. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 20] [Reference Citation Analysis (0)] |
| 22. | Xie G, Wu Q, Guo X, Zhang J, Yin D. Psychological resilience buffers the association between cell phone addiction and sleep quality among college students in Jiangsu Province, China. Front Psychiatry. 2023;14:1105840. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 20] [Reference Citation Analysis (0)] |
| 23. | Ye Y, Ge J. Clinical application of comfort nursing in elderly patients with advanced lung cancer. Am J Transl Res. 2021;13:9750-9756. [PubMed] |
| 24. | Ang TL, Fock KM. Clinical epidemiology of gastric cancer. Singapore Med J. 2014;55:621-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 278] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 25. | Thrift AP, El-Serag HB. Burden of Gastric Cancer. Clin Gastroenterol Hepatol. 2020;18:534-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 432] [Cited by in RCA: 1079] [Article Influence: 179.8] [Reference Citation Analysis (7)] |
| 26. | Hu J, Wang LL, Li Y. Effects of high-quality nursing intervention on negative emotions, postoperative complications and gastrointestinal function in patients with gastric cancer surgery. Am J Transl Res. 2022;14:1652-1662. [PubMed] |
| 27. | Cheng QM, Kong CQ, Chang SY, Wei AH. Effects of psychological nursing intervention on personality characteristics and quality of life of patients with esophageal cancer. Clin Res Hepatol Gastroenterol. 2013;37:283-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 28. | Wang J, Yuan T, Shi J. Application of Medical-Nursing Integration Multidisciplinary-Assisted Surgical Wound Nursing Mode in Improving the Quality of Wound Treatment. Emerg Med Int. 2022;2022:9299529. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 29. | Cao XL, Wang X, Li P, Ju W. Psychological effects of advanced care on patients received endoscopic gastric cancer resection. Medicine (Baltimore). 2019;98:e17497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 30. | Gaffney CJ, Pelt CE, Gililland JM, Peters CL. Perioperative Pain Management in Hip and Knee Arthroplasty. Orthop Clin North Am. 2017;48:407-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 142] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 31. | Wang LH, Zhu RF, Gao C, Wang SL, Shen LZ. Application of enhanced recovery after gastric cancer surgery: An updated meta-analysis. World J Gastroenterol. 2018;24:1562-1578. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 70] [Cited by in RCA: 66] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 32. | Xie FL, Wang YQ, Peng LF, Lin FY, He YL, Jiang ZQ. Beneficial Effect of Educational and Nutritional Intervention on the Nutritional Status and Compliance of Gastric Cancer Patients Undergoing Chemotherapy: A Randomized Trial. Nutr Cancer. 2017;69:762-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 33. | Cleland JFG, Clark RA. Telehealth: delivering high-quality care for heart failure. Lancet. 2018;392:990-991. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/