Published online Jul 27, 2025. doi: 10.4240/wjgs.v17.i7.105308
Revised: May 8, 2025
Accepted: May 20, 2025
Published online: July 27, 2025
Processing time: 117 Days and 3.5 Hours
Gallstones are frequently observed in patients with cholecystitis, but the mi
We report a case of a 72-year-old woman who experienced recurring fever and abdominal pain following laparoscopic cholecystectomy for acute cholecystitis, during which gallbladder rupture was noted. Despite initial conservative ma
This case highlights the potential long-term complications of retained free gallstones and the importance of thorough surgical retrieval.
Core Tip: This case report details an exceptionally rare complication following laparoscopic cholecystectomy: Chronic abdominal wall sinus formation due to free gallstone migration. Despite initial conservative management, including T-tube placement for gallbladder rupture, the patient developed a persistent subcutaneous abnormality with ulceration and purulent discharge 9.5 years later. Surgical exploration confirmed the presence of a yellow-green stone-like material at the base of the sinus tract. This case highlights the importance of thorough surgical retrieval of all gallstones during cholecystectomy and underscores the potential long-term complications of retained free gallstones. Early recognition and appropriate management are crucial.
- Citation: Yang L, Wang T, Li XL, Wang YL. Cholecystitis with gallbladder rupture leading to free gallstone migration causing chronic abdominal wall sinus formation: A case report. World J Gastrointest Surg 2025; 17(7): 105308
- URL: https://www.wjgnet.com/1948-9366/full/v17/i7/105308.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i7.105308
Laparoscopic cholecystectomy is the gold standard treatment for symptomatic cholelithiasis and acute cholecystitis, occurring in 10%-15% of the general population[1,2]. Of these cases, around 10% progress to acute cholecystitis requiring surgical intervention. The procedure has been widely adopted due to its minimally invasive nature and lower com
The delayed onset and unusual presentation of this condition pose significant diagnostic challenges. Understanding the underlying mechanisms and recognizing the potential for long-term complications can help clinicians provide improved care and enhance patient outcomes.
A 72-year-old woman with a medical history of hypertension and type 2 diabetes mellitus presented to our clinic with an already formed chronic sinus and ulceration in her abdominal wall, which had been developing for six months.
The patient reported that the mass had progressively increased in size, eventually ulcerating and discharging pus. She had undergone multiple debridements at an outside facility, but the wound failed to heal.
Notable for a laparoscopic cholecystectomy performed 10 years earlier due to acute cholecystitis. During the surgery, gallbladder rupture was noted, and a T-tube was inserted via endoscopic retrograde cholangiopancreatography for drainage. The patient initially improved with conservative management and opted against further surgical intervention. The T-tube was removed after 1 month, and the patient remained asymptomatic for the next 9.5 years.
Upon physical examination at the time of presentation to our hospital, the patient was noted to have a draining sinus tract with purulent discharge but without a significant subcutaneous mass. The area around the sinus tract was tender on palpation. No signs of systemic infection or sepsis were present.
Laboratory results were within normal limits, including glucose (95 mg/dL), creatinine (0.9 mg/dL), sodium (137 meq/L), potassium (4.0 meq/L), white blood cell count (9800/μL with 73.8% neutrophils, 14% lymphocytes, and 7.4% monocytes), platelets (300000 cells/mm3), hemoglobin (11.5 g/dL), and hematocrit (34.8%).
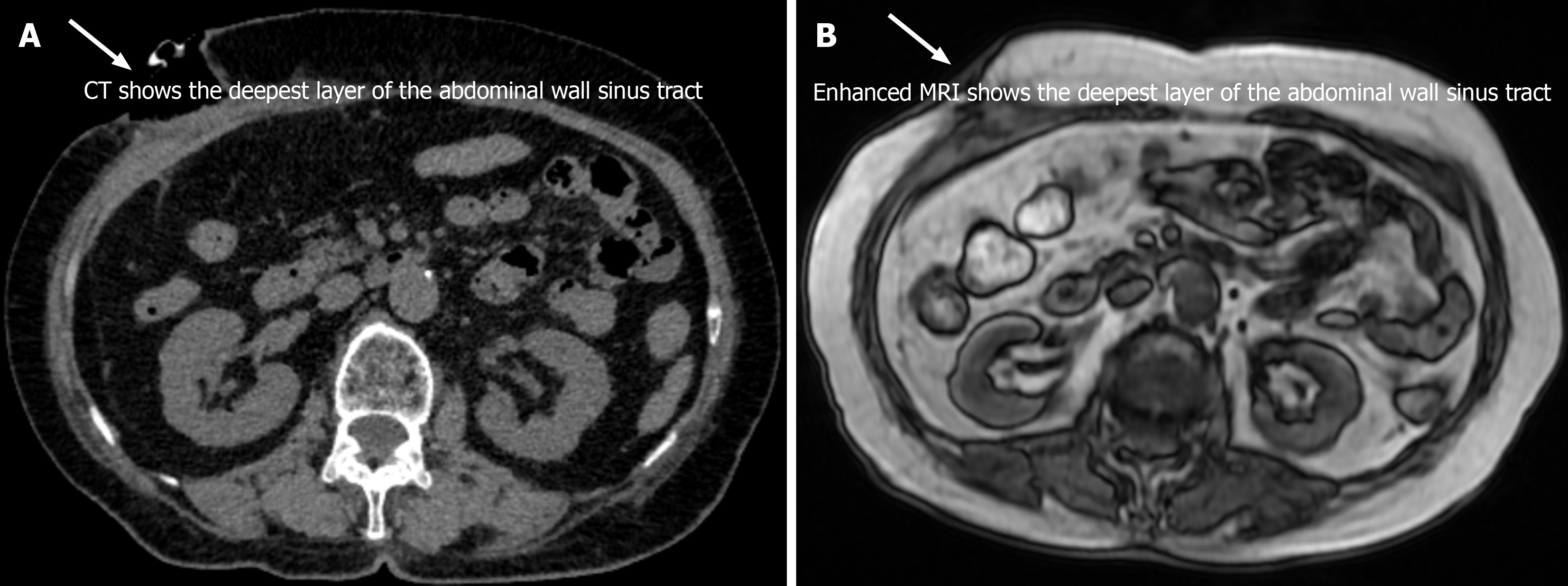
Imaging studies, including ultrasound and computed tomography (CT) of the abdomen, did not definitively demonstrate a connection between the sinus tract and the abdominal cavity. CT imaging revealed thickening and disordered structure of the soft tissues in the anterior abdominal wall, with evidence of a sinus tract that did not connect into the abdominal cavity. No gallbladder or gallstones were visible. Enhanced MRI also showed thickened tissue in the upper anterior abdominal wall, showing heterogeneous enhancement on T2-weighted images, without abnormal signals indicative of complications (Figure 1).
Given the complexity of the case, a multidisciplinary approach involving hepatobiliary surgeons was implemented.
The final diagnosis was chronic sinus formation due to migration of a free gallstone into the abdominal wall.
This study has been approved by the Ethics Committee of Zibo Central Hospital, and informed consent was obtained from the patient.
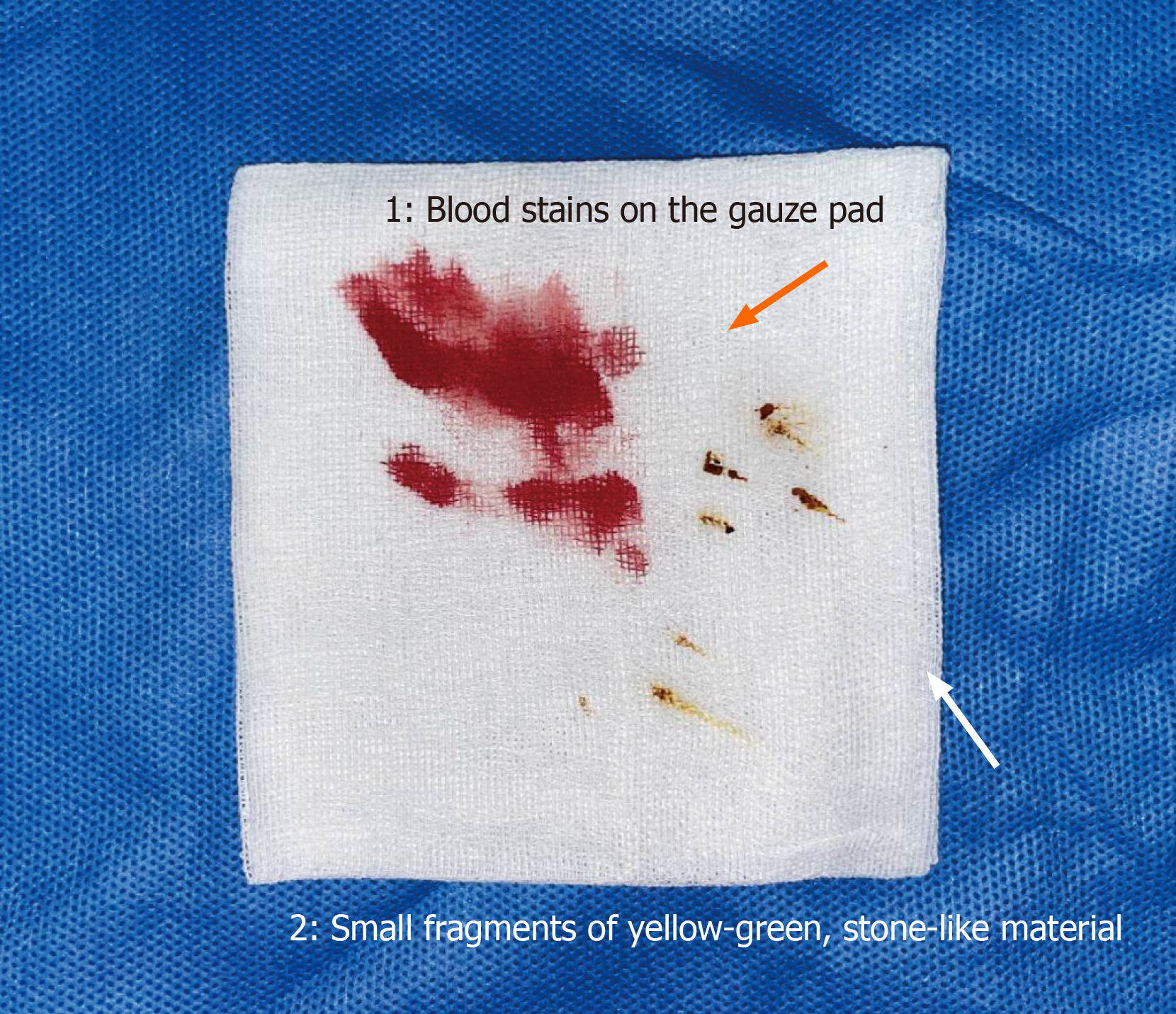
The patient underwent surgical exploration with general anesthesia. Intraoperative findings revealed significant adhesions from the previous surgery, which were carefully dissected. No obvious abnormalities were noted in the abdominal cavity. However, upon exploring the sinus tract, a yellow-green, stone-like material was discovered at its base (Figure 2). This finding was consistent with the hypothesis that a free gallstone had migrated from the site of the initial gallbladder rupture to the abdominal wall, leading to the formation of the chronic sinus. The stone was successfully extracted, and a negative pressure wound therapy (NPWT) device was applied to facilitate wound healing. Postoperatively, the patient was administered antibiotics to prevent infection and monitored closely for signs of wound healing. The NPWT device was maintained and regularly changed until the wound was completely healed.
The patient was discharged with instructions for wound care and follow-up appointments. At the one-year follow-up, the patient reported no recurrence of symptoms.
The migration of a free gallstone into the abdominal wall, leading to the development of a chronic sinus, is a rare complication of gallbladder disease. Previous studies have suggested several mechanisms that may contribute to this phenomenon. For instance, Salati et al[10] found that the initial retention of small gallstones during laparoscopic cholecystectomy, particularly in cases of gallbladder rupture, can lead to their subsequent migration. In our case, gallbladder rupture likely played a pivotal role in the release of a gallstone into the peritoneal cavity.
In contrast, gallstones causing intestinal obstruction typically involve larger stones that migrate through the biliary tract and enter the intestines, where they cause mechanical blockage[11]. While both conditions result from gallstone migration, the underlying mechanisms differ significantly. Gallstones migrating to the abdominal wall are more likely influenced by local inflammation and pressure from surrounding tissues, promoting their movement within the peritoneum[12]. Additionally, the natural movement of the abdominal wall, especially in areas with previous surgical adhesions, may facilitate the gradual migration of gallstones toward the abdominal wall[13]. The chronic inflammatory response triggered by the presence of a foreign body (the gallstone) can result in the formation of a sinus tract, as observed in our patient.
Furthermore, Tran et al[14] demonstrated that the delayed onset of symptoms, as seen in this case, can be attributed to the slow progression of the inflammatory process and the eventual erosion of the gallstone through the abdominal wall. These findings emphasize the importance of precise surgical technique, including the use of intraoperative cholangiography to identify and retrieve all gallstones, and the necessity of long-term follow-up in patients with a history of complicated cholecystitis.
This case highlights the critical importance of thorough surgical technique in laparoscopic cholecystectomy, specifically the need to ensure the complete retrieval of all gallstones. Techniques such as intraoperative cholangiography and careful inspection of the surgical field can significantly reduce the risk of residual free gallstones. Moreover, the case underscores the need for long-term follow-up in patients with a history of complicated cholecystitis, despite their early apparent recovery. Long-term monitoring can facilitate the early detection and management of potential complications, improving patient outcomes. A multidisciplinary approach, involving hepatobiliary surgeons, radiologists, and wound healing specialists, provides comprehensive care and improves outcomes for patients. Early recognition and appropriate management, including surgical exploration and the use of advanced wound care techniques such as NPWT, are essential for resolving such rare and challenging conditions.
Moreover, recent advances in medical technology have introduced new possibilities for the prevention and treatment of complications caused by free gallstone migration. For instance, novel minimally invasive techniques, such as endoscopic retrieval of spilled gallstones, may offer a less invasive alternative to traditional surgical approaches[15]. Additionally, emerging pharmacological therapies aimed at dissolving gallstones or reducing inflammation could play a crucial role in preventing long-term complications[16]. Future research should focus on exploring these new avenues, including personalized medicine approaches and the use of artificial intelligence to improve diagnostic accuracy and tailor treatment plans for individual patients.
The migration of a free gallstone into the abdominal wall resulting in chronic sinus formation is an extremely rare complication of gallbladder disease. This case highlights the potential long-term consequences of retained gallstones and underscores the importance of thorough surgical retrieval during cholecystectomy. Early recognition and appropriate management are critical for achieving a favorable outcome in such cases.
| 1. | Gallaher JR, Charles A. Acute Cholecystitis: A Review. JAMA. 2022;327:965-975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 226] [Article Influence: 56.5] [Reference Citation Analysis (0)] |
| 2. | Ukegjini K, Schmied BM. [Diagnosis and treatment of acute cholecystitis]. Ther Umsch. 2020;77:133-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Ahmed I, Hudson J, Innes K, Hernández R, Gillies K, Bruce R, Bell V, Avenell A, Blazeby J, Brazzelli M, Cotton S, Croal B, Forrest M, MacLennan G, Murchie P, Wileman S, Ramsay C; C-GALL Study Group. Effectiveness of conservative management versus laparoscopic cholecystectomy in the prevention of recurrent symptoms and complications in adults with uncomplicated symptomatic gallstone disease (C-GALL trial): pragmatic, multicentre randomised controlled trial. BMJ. 2023;383:e075383. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | Kalata S, Thumma JR, Norton EC, Dimick JB, Sheetz KH. Comparative Safety of Robotic-Assisted vs Laparoscopic Cholecystectomy. JAMA Surg. 2023;158:1303-1310. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 97] [Article Influence: 32.3] [Reference Citation Analysis (0)] |
| 5. | Warchałowski Ł, Łuszczki E, Bartosiewicz A, Dereń K, Warchałowska M, Oleksy Ł, Stolarczyk A, Podlasek R. The Analysis of Risk Factors in the Conversion from Laparoscopic to Open Cholecystectomy. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 6. | Xu Y, Wang H, Yang M. Preoperative nursing visit reduces preoperative anxiety and postoperative complications in patients with laparoscopic cholecystectomy: A randomized clinical trial protocol. Medicine (Baltimore). 2020;99:e22314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Arian R, Farwati R, Toutounji Z, Farho MA, Assi BE. Intestinal obstruction induced by gallstone migration through unusual location of a cholecystogastric fistula: A rare case report. Int J Surg Case Rep. 2024;122:110149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Lambe G, Murphy M, O'Neill H, Doran S, Donlon NE, McEniff N. The Rolling Stones: A case report of two surgical abdomens linked by migrating gallstones. Int J Surg Case Rep. 2021;80:105658. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Brunt LM, Deziel DJ, Telem DA, Strasberg SM, Aggarwal R, Asbun H, Bonjer J, McDonald M, Alseidi A, Ujiki M, Riall TS, Hammill C, Moulton CA, Pucher PH, Parks RW, Ansari MT, Connor S, Dirks RC, Anderson B, Altieri MS, Tsamalaidze L, Stefanidis D; Prevention of Bile Duct Injury Consensus Work Group. Safe cholecystectomy multi-society practice guideline and state-of-the-art consensus conference on prevention of bile duct injury during cholecystectomy. Surg Endosc. 2020;34:2827-2855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 77] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 10. | Salati SA, Alfehaid M, Alsuwaydani S, AlSulaim L. Spilled gallstones after laparoscopic cholecystectomy: a systematic review. Pol Przegl Chir. 2022;95:1-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 11. | Foss HL, Summers JD. INTESTINAL OBSTRUCTION FROM GALLSTONES. Ann Surg. 1942;115:721.b2-721735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 50] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Duhancioglu G, Arif-Tiwari H, Natali S, Reynolds C, Lalwani N, Fulcher A. Traveling gallstones: review of MR imaging and surgical pathology features of gallstone disease and its complications in the gallbladder and beyond. Abdom Radiol (NY). 2024;49:722-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Ikeno H, Kobayashi S, Kozaka K, Ogi T, Inoue D, Yoneda N, Yoshida K, Ohno N, Gabata T, Kitao A. Relationship between the degree of abdominal wall movement and the image quality of contrast-enhanced MRI: semi-quantitative study especially focused on the occurrence of transient severe motion artifact. Jpn J Radiol. 2020;38:165-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Tran A, Hoff C, Polireddy K, Neymotin A, Maddu K. Beyond acute cholecystitis-gallstone-related complications and what the emergency radiologist should know. Emerg Radiol. 2022;29:173-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Husnain A, Reiland A, Nemcek AA Jr, Salem R, Nagle AP, Teitelbaum E, Riaz A. Percutaneous Endoscopy and Image-guided Retrieval of Dropped Gallstones - A Case Series. Surg Laparosc Endosc Percutan Tech. 2024;34:361-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 16. | Di Ciaula A, Wang DQ, Wang HH, Bonfrate L, Portincasa P. Targets for current pharmacologic therapy in cholesterol gallstone disease. Gastroenterol Clin North Am. 2010;39:245-264, viii. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/