Published online Jul 27, 2025. doi: 10.4240/wjgs.v17.i7.105033
Revised: March 18, 2025
Accepted: May 21, 2025
Published online: July 27, 2025
Processing time: 195 Days and 9.2 Hours
Hereditary spherocytosis (HS), a common inherited hemolytic anemia, is characterized by red blood cell membrane protein defects leading to chronic hemolysis. This condition significantly predisposes patients to gallstone disease, including both gallbladder and bile duct stones, due to excessive bilirubin production from hemolysis. Gallstones in HS patients, primarily composed of bilirubin, can lead to complications such as cholecystitis, cholangitis, and obstructive jaundice. This review provides a comprehensive landscape of the pathophysiological mecha
Core Tip: Hereditary spherocytosis predisposes patients to gallstone disease due to chronic hemolysis and elevated bilirubin levels. This review explores the pathophysiological mechanisms, clinical manifestations, and diagnostic strategies for hereditary spherocytosis-related gallstones. Key insights include the importance of ultrasonography and magnetic resonance cholangiopancreatography for early detection, tailored management strategies such as splenectomy and cholecystectomy, and emerging preventive approaches, including lifestyle modifications, pharmacological therapies, and novel treatments like nanoprodrugs and probiotics. Addressing research gaps in genetic predisposition, microbial influences, and biomarkers will further enhance prevention and treatment, particularly in pediatric populations, emphasizing a multidisciplinary approach for optimized outcomes.
- Citation: Cong S, Wang YN, Wang JR, Duan RH. Association between hereditary spherocytosis and gallstone disease: Pathophysiology, diagnosis, and management. World J Gastrointest Surg 2025; 17(7): 105033
- URL: https://www.wjgnet.com/1948-9366/full/v17/i7/105033.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i7.105033
Hereditary spherocytosis (HS) is a prevalent inherited hemolytic anemia caused by red blood cell membrane protein defects that lead to chronic hemolysis. This condition is characterized by extravascular hemolysis, where red blood cells are destroyed in the spleen, leading to increased bilirubin production. The breakdown of these cells releases unconjugated bilirubin, which can accumulate in the gallbladder and precipitate as pigment gallstones. Among its complications, gallstone disease is particularly significant due to its potential to cause substantial morbidity, including biliary colic, cholecystitis, and bile duct obstruction. Studies indicate a high incidence of gallstones in HS patients, with detection rates ranging from 37% to 43% in adults and significant rates observed in children and young adults. The risk of gallstone formation in HS can be further exacerbated by genetic modifiers, such as co-inheritance of Gilbert syndrome, which impairs bilirubin conjugation and increases bilirubin levels. Exploring the relationship between HS and gallstone disease provides crucial insights into better clinical management and prevention strategies. Regular ultrasound examinations are recommended for early detection of gallstones in HS patients, particularly those with additional risk factor. This review synthesizes current evidence on the pathophysiology, clinical features, diagnosis, and management of gallstone disease in HS, identifying gaps for future research.
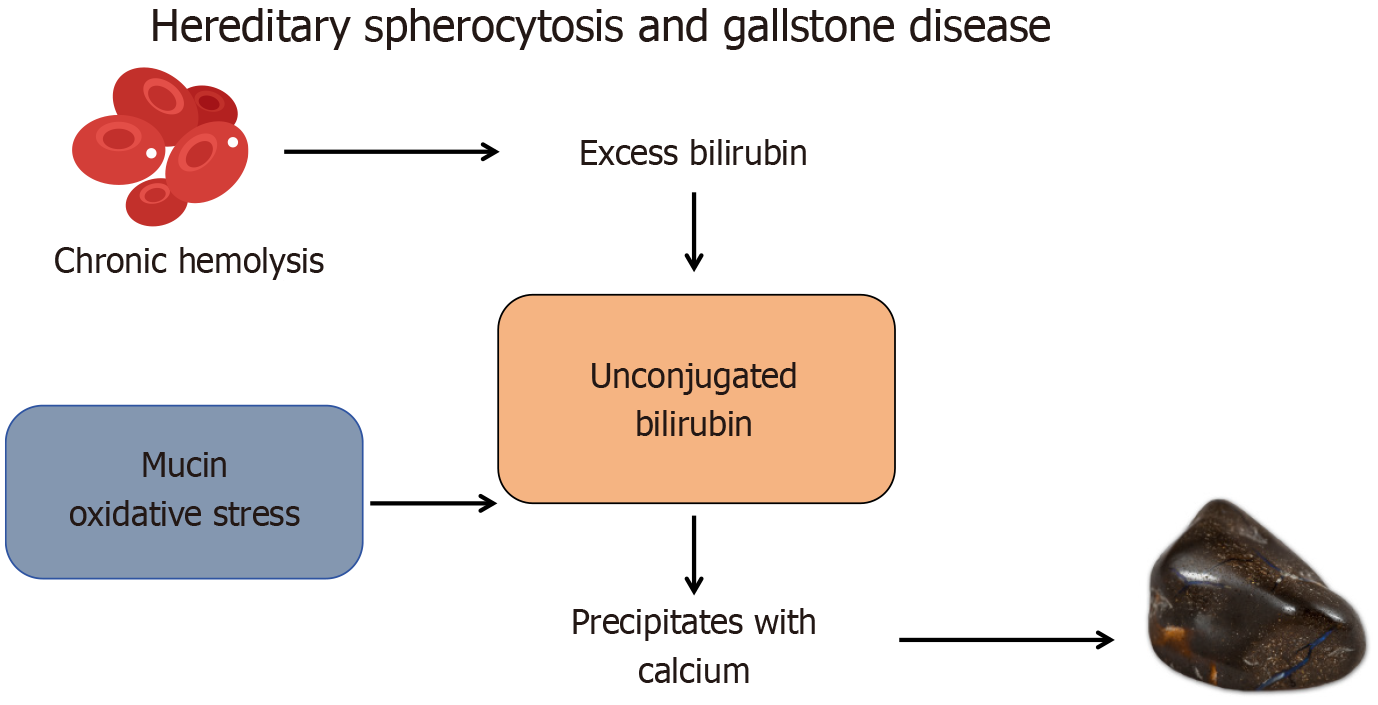
The development of gallstones in HS is closely linked to the chronic hemolysis inherent to this condition. Hemolysis leads to the excessive release of heme, which is metabolized into unconjugated bilirubin in the liver. The elevated bilirubin levels can overwhelm the liver’s conjugation capacity, resulting in an accumulation of unconjugated bilirubin in bile. This unconjugated bilirubin, along with monoconjugated bilirubin, precipitates in the gallbladder and contributes to the formation of bilirubin gallstones. Studies have highlighted the role of monoconjugated bilirubin in gallstone formation, noting its coprecipitation with unconjugated bilirubin under hemolytic conditions.
Bile composition plays a critical role in gallstone formation. In HS, bile often contains elevated hydrogen ion concentrations, bilirubin, and calcium ions, creating an environment conducive to the precipitation of bilirubin as calcium bilirubinate, a key component of pigment stones[1]. Additionally, bilirubin’s chemical properties, including its tendency to form free radicals, promote oxidative changes, polymerization, and calcification, further facilitating stone development[2]. The altered bile environment in HS is compounded by structural changes in the gallbladder. Mucin plug formation, a common feature in HS patients, has been implicated as a nidus for stone accretion. Histological studies suggest that these plugs, laden with concentrated pigment, initiate and accelerate gallstone development[1].
Genetic predispositions further contribute to gallstone formation in HS. Mutations in the uridine diphosphate glucuronosyl transferase 1A1 gene impair bilirubin conjugation, increasing the proportion of unconjugated bilirubin in bile and promoting gallstone nucleation. Additionally, variations in the ATP-binding cassette transporters G5 (ABCG5)/ABCG8 transporter genes have been associated with altered bile cholesterol secretion, further modifying gallstone risk. The co-inheritance of Gilbert syndrome in HS patients exacerbates the imbalance in bilirubin metabolism, increasing the likelihood of gallstone development at a younger age.
Recent research has identified oxidative stress as a significant factor in gallstone pathogenesis in HS patients. Chronic hemolysis induces oxidative damage, leading to altered bile composition and increased susceptibility to calcium bilirubinate precipitation. Free radical-mediated damage to biliary lipids may enhance cholesterol crystallization and gallstone growth, further complicating disease progression. These mechanisms collectively highlight the intricate relationship between hemolysis, bilirubin metabolism, bile composition, and gallstone formation in HS patients. However, variability in clinical presentation underscores the influence of factors such as age, sex, genetic variability, and coexisting conditions, which can modify the risk and severity of gallstone disease in HS[1].
Gallstone disease in HS patients presents with diverse clinical manifestations, ranging from asymptomatic cases to severe biliary complications. Unlike the general population, where cholesterol gallstones predominate, HS patients are more likely to develop pigment gallstones due to chronic hemolysis, which significantly increases bilirubin production and alters bile composition[3].
Recurrent jaundice is a hallmark symptom in HS patients and is often exacerbated during episodes of increased hemolysis. These patients frequently present with biliary colic, characterized by episodic upper abdominal pain, typically after meals, and acute cholecystitis, which occurs more frequently in HS due to the rapid formation and growth of pigment stones[4]. The increased frequency of acute cholecystitis in HS patients is linked to the higher concentration of unconjugated bilirubin in bile, which accelerates pigment stone nucleation and aggregation.
Gallstone disease in HS also tends to present at a younger age compared to the general population, reflecting the early onset of hemolytic activity in these patients[5]. This early manifestation underscores the need for routine ultrasound screening in pediatric HS patients to facilitate early detection and timely intervention. Complications are common in untreated cases. Acute cholecystitis, resulting from gallstone impaction in the cystic duct, presents with fever, right upper quadrant tenderness, and leukocytosis. Additionally, due to the frequent presence of multiple small pigment stones, HS patients have a higher risk of bile duct obstruction, leading to choledocholithiasis, cholangitis, and pancreatitis.[6]. The incidence of severe complications, such as gallstone ileus and biliary-enteric fistulas, may also be higher in HS patients due to the chronic nature of their condition and the continuous formation of stones[4].
In contrast to HS, the general population experiences a higher prevalence of asymptomatic cholesterol gallstones, with only a small percentage developing complications. Furthermore, while conservative management may be suitable for asymptomatic stones in the general population, HS patients often require early cholecystectomy to prevent recurrent symptoms and complications[7]. The differences in stone composition and underlying pathophysiology between HS patients and the general population necessitate distinct clinical approaches and management strategies. Recognizing these differences is critical for optimizing treatment and preventing long-term morbidity in HS patients.
Accurate and early diagnosis of gallstone disease in HS relies on a combination of imaging modalities and laboratory evaluations. Ultrasonography is the first-line imaging tool due to its non-invasiveness, accessibility, and high sensitivity for gallstones. It is particularly effective in identifying gallstones within the gallbladder, as they appear as highly reflective echoes with posterior acoustic shadowing[8,9]. Pocket-size ultrasound devices have demonstrated high diagnostic accuracy, with sensitivity and specificity reaching up to 93.75% and 100%, respectively, when operated by experienced clinicians[10]. For more complex cases, including bile duct stones, magnetic resonance cholangiopancreatography (MRCP) offers superior imaging resolution. MRCP is a non-invasive imaging technique with excellent sensitivity and specificity for detecting bile duct stones and biliary pathologies. It is particularly useful when ultrasound results are inconclusive or when a detailed image of the biliary tract is required.
Endoscopic retrograde cholangiopancreatography (ERCP) is considered the gold standard for diagnosing choledocholithiasis, as it provides direct visualization and allows for therapeutic interventions such as stone removal during the procedure[11,12]. However, it is an invasive procedure associated with risks such as pancreatitis and perforation[12]. Alternatively, endoscopic ultrasound (EUS) is a minimally invasive procedure that provides high-resolution images of the biliary tract. Its diagnostic accuracy is comparable to ERCP, and it is particularly effective in detecting small stones that might be missed by other imaging modalities[12,13].
While ERCP remains the definitive diagnostic and therapeutic modality for bile duct stones, it carries a considerable risk of complications, including post-ERCP pancreatitis and duodenal perforation, limiting its use primarily to therapeutic rather than purely diagnostic purposes. In contrast, EUS provides comparable sensitivity for detecting common bile duct stones while avoiding ERCP-related complications, making it a safer initial assessment tool. However, EUS requires specialized expertise and equipment availability, which may not be feasible in all healthcare settings. MRCP, as a non-invasive alternative, is ideal for patients in whom an invasive procedure is contraindicated. Nevertheless, MRCP has limitations in detecting small stones or sludge, potentially leading to false-negative results. Therefore, a tailored approach that considers patient-specific risk factors, symptomatology, and institutional resources is essential in selecting the most appropriate diagnostic tool for HS-associated gallstone disease.
The choice of diagnostic tool depends on clinical presentation, patient condition, and available resources. Emerging technologies, such as machine learning and deep learning models, are being explored to enhance diagnostic accuracy and efficiency, though they require further validation before widespread clinical adoption[9,14]. When combined, these diagnostic approaches enable clinicians to identify gallstone disease in HS patients effectively, guiding appropriate management strategies.
The management of gallstone disease in HS patients is tailored to the severity of symptoms and the extent of underlying hemolysis. Splenectomy, often a cornerstone treatment for HS, significantly reduces hemolysis and bilirubin production, indirectly lowering the risk of gallstone formation. However, recent studies suggest that despite splenectomy, residual hemolysis may still contribute to gallstone formation, necessitating continued surveillance in post-splenectomy patients. Prophylactic cholecystectomy is recommended in asymptomatic HS patients with a high risk of gallstone-related complications, particularly those undergoing planned splenectomy, given the increased likelihood of future biliary events.
For symptomatic gallstones, laparoscopic cholecystectomy (LC) is the definitive treatment. Early elective chole
For patients with bile duct stones, ERCP is the preferred intervention. ERCP should be performed preoperatively or postoperatively in patients with suspected choledocholithiasis to ensure complete biliary clearance and prevent recurrent obstruction. For bile duct stones, ERCP plays a central role, offering over 90% efficacy in stone clearance while allowing for both diagnostic and therapeutic interventions[15,16]. To further optimize management, preoperative EUS is now considered as a non-invasive screening tool to identify bile duct stones prior to ERCP, reducing unnecessary invasive procedures. Preoperative ERCP may be employed in cases where bile duct stones are suspected; however, it is associated with higher complication rates compared to intraoperative or postoperative ERCP[17]. When ERCP fails or is not feasible, percutaneous techniques provide an alternative route for stone removal, particularly in complex cases[15].
Laparoscopic common bile duct exploration can be performed in conjunction with LC as part of a one-stage approach for managing bile duct stones. This method reduces hospital stays and costs compared to the two-stage approach of separate LC and ERCP procedures[18,19]. The transcystic approach for laparoscopic common bile duct exploration is preferred when feasible, as it has lower complication rates than the transductal approach[19]. In rare cases where laparoscopic methods are not feasible, such as with large stones or anatomical challenges, open surgery remains a viable option[20].
In HS patients, minimizing surgical stress is crucial due to their heightened risk of hemolysis and complications. Non-surgical approaches, such as bile acid dissolution therapy with ursodeoxycholic acid, remain largely ineffective for pigment gallstones and are not routinely recommended. However, emerging therapies, including nanoprodrugs and probiotics, show potential in modifying bile composition and reducing gallstone risk. Probiotic-based therapies that modulate gut microbiota to influence enterohepatic circulation and bile metabolism may help reduce bilirubin stone formation. The choice of management strategy should be individualized based on patient factors such as gallstone size, symptom severity, and overall HS disease burden. A multidisciplinary approach involving hematologists, gastroenterologists, and surgeons is recommended to optimize outcomes in these patients.
The long-term outcomes of HS patients with gallstone disease depend on disease severity, surgical interventions, and ongoing hemolysis. While cholecystectomy resolves acute complications, recurrent pigment stone formation remains a risk due to persistent hemolysis, particularly in patients without splenectomy. Even after surgery, common bile duct stones (choledocholithiasis) can develop, necessitating long-term surveillance and potential ERCP intervention. Quality of life may be affected by residual symptoms such as episodic jaundice and fatigue, with studies indicating a lower health-related quality of life in HS patients with prior gallstone-related complications. Prophylactic splenectomy significantly reduces hemolysis and gallstone recurrence, improving long-term outcomes, though it requires careful patient selection due to associated risks. Lifelong follow-up, including liver function tests, imaging, and hemolysis markers, is recommended to monitor ongoing risks, while preventive strategies such as bile acid therapy and microbiome-targeted interventions may help reduce recurrence. These updates highlight the importance of continued surveillance and individualized management in HS patients with gallstone disease.
Preventive strategies for gallstone disease in HS focus on mitigating the risk factors associated with hemolysis and altered bile composition. Splenectomy remains the most effective preventive intervention, particularly when performed early in life, as it significantly reduces hemolysis and bilirubin production. Regular monitoring through imaging and laboratory evaluations facilitates the early detection of gallstones, enabling timely interventions.
Lifestyle modifications play a crucial role in improving bile composition and reducing stone formation. Adopting a plant-based diet, which excludes heme iron-rich foods such as meat and fish, while incorporating fruits, vegetables, whole grains, and legumes, can lower the risk of gallstone formation by reducing obesity, insulin resistance, and dietary cholesterol levels[21]. Weight management is also vital, as obesity is a significant risk factor for gallstone development. Avoiding rapid weight loss, which is associated with increased cholesterol levels and fat mobilization, is particularly important, especially in post-bariatric surgery patients[22].
Pharmacological interventions offer additional preventive options. Ursodeoxycholic acid has proven effective in preventing gallstone formation during periods of rapid weight loss by enhancing bile acid biosynthesis and inhibiting cholesterol absorption[22,23]. Ezetimibe, which targets the Niemann-Pick C1-like 1 protein to reduce intestinal cholesterol absorption, and hyodeoxycholic acid, which prevents cholesterol crystallization, are promising alternatives[24,25].
Novel therapeutic approaches are also emerging. Supramolecular nanoprodrugs, such as hydroxypropyl-β-cyclodextrin nanoparticles, have been developed to solubilize cholesterol in the gallbladder, effectively preventing gallstone formation. These nanoparticles leverage the established safety of cyclodextrin-based delivery systems[26]. Probiotics, shown to regulate cholesterol metabolism and alter bile composition more effectively than tauroursodeoxycholic acid alone, offer another innovative strategy[27].
Herbal and alternative treatments provide a side-effect-free approach to gallstone prevention by correcting bile composition and stimulating gallbladder contractions. Traditional herbal formulations have been used successfully in some populations, although their efficacy and safety require further validation[28]. These preventive measures underscore the importance of a multifaceted approach tailored to individual patient factors, such as genetic predispositions and comorbidities. While lifestyle and pharmacological interventions remain the cornerstone of prevention, emerging therapies targeting bile composition and cholesterol metabolism offer promising avenues for high-risk HS patients. Further research is needed to explore the long-term efficacy and safety of these interventions across diverse patient populations.
Despite advancements, significant gaps remain in understanding and managing gallstone disease in HS patients. Genetic links, such as the role of ABCG8 transporters, remain underexplored, necessitating genome-wide association studies to identify specific markers[29,30]. Environmental factors like diet and metabolic syndrome, commonly associated with HS, also require further investigation to clarify their interactions with genetic predispositions[31]. Emerging evidence highlights the role of biliary microbiota and bacterial biofilms in gallstone pathogenesis, particularly in HS, where microbial biomineralization processes may differ from the general population[32,33]. Diagnostic advancements, including biomarkers and imaging, could facilitate early detection and personalized interventions. Novel therapeutic strategies, such as probiotics, supramolecular nanoprodrugs, and non-invasive interventions, offer promising avenues for prevention and treatment[26]. Future research should focus on these areas, particularly in pediatric populations, where early interventions could profoundly impact long-term outcomes, requiring collaborative, multidisciplinary approaches.
The relationship between HS and gallstone disease is complex and multifaceted, encompassing pathophysiological, clinical, and management aspects (Figure 1). By synthesizing existing knowledge, this review highlights the importance of a multidisciplinary approach to improve patient outcomes. Early diagnosis, personalized management strategies, and targeted preventive measures are essential to addressing the unique challenges posed by this condition. Future research should aim to bridge existing gaps, advancing the care of patients with HS and gallstone disease.
| 1. | Trotman BW, Bernstein SE, Bove KE, Wirt GD. Studies on the pathogenesis of pigment gallstones in hemolytic anemia: description and characteristics of a mouse model. J Clin Invest. 1980;65:1301-1308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 47] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Liu XT, Hu J. Relationship between bilirubin free radical and formation of pigment gallstone. World J Gastroenterol. 2002;8:413-417. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Giridharan B, Madhivadhanam M. Clinical analysis on Gall Bladder Disease Cholecystitis and Cholelitheasis. Sch J App Med Sci. 2016;4:2480-2483. [DOI] [Full Text] |
| 4. | Tucker L, Tangedahl TN. Manifestations of gallstone disease. Postgrad Med. 1979;66:179-180, 183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Shafique M, Ahmad R, Ahmad S, Hassan S, Khan J. Gallstones in Young Population and Its Complications. Ulutas Med J. 2018;4:131-138. [DOI] [Full Text] |
| 6. | Wilson TG. Obstructive Jaundice and Cholangitis. In: Cox M, Eslick G, Padbury R. The Management of Gallstone Disease. Cham: Springer, 2018. [DOI] [Full Text] |
| 7. | Housset C. Gallstone disease, towards a better understanding and clinical practice. Curr Opin Gastroenterol. 2018;34:57-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Bortoff GA, Chen MY, Ott DJ, Wolfman NT, Routh WD. Gallbladder stones: imaging and intervention. Radiographics. 2000;20:751-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 100] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 9. | Ahmed AS, Ahmed SS, Mohamed S, Salman NE, Humidan AAM, Ibrahim RF, Salim RS, Mohamed Elamir AA, Hakim EM. Advancements in Cholelithiasis Diagnosis: A Systematic Review of Machine Learning Applications in Imaging Analysis. Cureus. 2024;16:e66453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 10. | Del Medico M, Altieri A, Carnevale-Maffè G, Formagnana P, Casella F, Barchiesi M, Bergonzi M, Vattiato C, Casazza G, Cogliati C. Pocket-size ultrasound device in cholelithiasis: diagnostic accuracy and efficacy of short-term training. Intern Emerg Med. 2018;13:1121-1126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Borysenko VB. Gallstone Disease Complicated by Choledocholithiasis: Modern Aspects of Diagnostics. Ukrainian J Med Biol Sport. 2021;6:66-70. [DOI] [Full Text] |
| 12. | Anwer M, Asghar MS, Rahman S, Kadir S, Yasmin F, Mohsin D, Jawed R, Memon GM, Rasheed U, Hassan M. Diagnostic Accuracy of Endoscopic Ultrasonography Versus the Gold Standard Endoscopic Retrograde Cholangiopancreatography in Detecting Common Bile Duct Stones. Cureus. 2020;12:e12162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Kumari S, Dutta KK, Karamchandani H, Kehkeshan JS. Diagnostic tools for gallstone. In: Gallstone Formation, Diagnosis, Treatment and Prevention. Amsterdam: Elsevier, 2024: 155-167. [DOI] [Full Text] |
| 14. | Niu Y, Li J, Xu X, Luo P, Liu P, Wang J, Mu J. Deep learning-driven ultrasound-assisted diagnosis: optimizing GallScopeNet for precise identification of biliary atresia. Front Med (Lausanne). 2024;11:1445069. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 15. | Strong AT, Ponsky JL. Non-operative Management of Common Bile Duct Stones: ERCP and Other Techniques (Lithotripsy). In: Asbun H, Shah M, Ceppa E, Auyang E. The SAGES Manual of Biliary Surgery. Cham: Springer, 2020. [DOI] [Full Text] |
| 16. | Lee SK, Kim MH. Updates in the treatment of gallstones. Expert Rev Gastroenterol Hepatol. 2009;3:649-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Nagaraja V, Eslick GD, Cox MR. Systematic review and meta-analysis of minimally invasive techniques for the management of cholecysto-choledocholithiasis. J Hepatobiliary Pancreat Sci. 2014;21:896-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Cianci P, Restini E. Management of cholelithiasis with choledocholithiasis: Endoscopic and surgical approaches. World J Gastroenterol. 2021;27:4536-4554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 99] [Cited by in RCA: 92] [Article Influence: 18.4] [Reference Citation Analysis (21)] |
| 19. | Pavlidis ET, Pavlidis TE. Current management of concomitant cholelithiasis and common bile duct stones. World J Gastrointest Surg. 2023;15:169-176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (2)] |
| 20. | Pieracci FM, Jaouen BM, Stovall RT. Management of Choledocholithiasis. In: Acute Cholecystitis. United States: Springer International Publishing. 2015: 169-186. [DOI] [Full Text] |
| 21. | Strombom AJ. Gall Stones – Prevention with a Plant-Based Diet. Adv Res Gastroentero Hepatol. 2020;14. [DOI] [Full Text] |
| 22. | Plotnikova EY, Sukhikh AS. Reduction of the risk of biliary lithiasis caused by various weight reduction options in obesity. Med Sov. 2024;. [DOI] [Full Text] |
| 23. | Son SY, Song JH, Shin HJ, Hur H, Han SU. Prevention of Gallstones After Bariatric Surgery using Ursodeoxycholic Acid: A Narrative Review of Literatures. J Metab Bariatr Surg. 2022;11:30-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 24. | Floreani A. A novel approach for prevention and dissolution of cholesterol gallstones. Liver Int. 2008;28:906-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | McSherry CK, Mosbach EH, Cohen BI, Une M, Stenger RJ, Singhal AK. Hyodeoxycholic acid: a new approach to gallstone prevention. Am J Surg. 1985;149:126-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Zhang X, Yang X, Wang Y, Xu Z, Yi S, Guo T, Liao Y, Tang X, Zhang J, Wang R. A supramolecular nanoprodrug for prevention of gallstone formation. Chinese Chem Lett. 2025;36:109854. [RCA] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 27. | Gao F, Guan D, Wang G, Zhang L, He J, Lv W, Zhang X, Tao W, Dai Y, Xu S, Chen Y, Lu B. Effects of oral tauroursodeoxycholic acid and/or intestinal probiotics on serum biochemical indexes and bile composition in patients with cholecystolithiasis. Front Pharmacol. 2022;13:882764. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 28. | Tendulkar R, Tendulkar M. Chemical and herbal treatment for gallstone treatment. In: Gallstone Formation, Diagnosis, Treatment and Prevention. Amsterdam: Elsevier, 2024: 189-206. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 29. | Lammert F. Gallstone Disease: Scientific Understanding and Future Treatment. In: Hirschfield G, Adams D, Liaskou E. Biliary Disease. Cham: Springer, 2017. [DOI] [Full Text] |
| 30. | Höblinger A, Lammert F. Genetics of biliary tract diseases: new insights into gallstone disease and biliary tract cancers. Curr Opin Gastroenterol. 2008;24:363-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 31. | Ahmed MH, Barakat S, Almobarak AO. The association between renal stone disease and cholesterol gallstones: the easy to believe and not hard to retrieve theory of the metabolic syndrome. Ren Fail. 2014;36:957-962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 32. | Shen H, Ye F, Xie L, Yang J, Li Z, Xu P, Meng F, Li L, Chen Y, Bo X, Ni M, Zhang X. Metagenomic sequencing of bile from gallstone patients to identify different microbial community patterns and novel biliary bacteria. Sci Rep. 2015;5:17450. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 81] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/