Published online Jul 27, 2025. doi: 10.4240/wjgs.v17.i7.104777
Revised: April 21, 2025
Accepted: June 6, 2025
Published online: July 27, 2025
Processing time: 117 Days and 3.3 Hours
Ultrasound classification can be used to determine the severity of adhesive inte
To explore the value of ultrasound classification in disease judgment and treat
The medical records of 120 patients with adhesive intestinal obstruction pre
Among the 120 patients, P > 0.05, compared with the general data (sex, age, body quality index, time to onset, and history of onset), the proportion of bowel dis
Ultrasound typing can aid in the clinical evaluation of the severity of adhesive intestinal obstruction and provide an imaging reference for clinicians to develop targeted treatment plans.
Core Tip: This study highlights the clinical value of ultrasound classification in assessing the severity of adhesive intestinal obstruction. By categorizing cases into simple, complex, and critical types based on ultrasound findings, clinicians can more accurately determine the appropriate treatment approach - conservative or surgical. The results support ultrasound as a non-invasive, practical tool to guide personalized treatment plans and improve clinical decision-making in managing adhesive ileus.
- Citation: Wang F, Liu C, Wang H. Value analysis of ultrasound classification in disease judgment and treatment plan formulation of patients with adhesive intestinal obstruction. World J Gastrointest Surg 2025; 17(7): 104777
- URL: https://www.wjgnet.com/1948-9366/full/v17/i7/104777.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i7.104777
Adhesive intestinal obstruction is one of the most common types of intestinal obstruction, accounting for approximately 40%-60% of all cases. This condition results from adhesions within the abdominal cavity and is characterized by abdominal pain, distension, and vomiting. If not treated promptly and effectively, the condition can progress, leading to dehydration and shock, posing a threat to the patient’s life[1,2]. The clinical treatment options for this disease include surgical and nonsurgical methods. However, the selection of the most appropriate treatment plan for patients with varying degrees of adhesive intestinal obstruction is challenging in clinical practice. Poor treatment outcomes can lead to high recurrence rates and poor prognosis[3]. Therefore, it is crucial to use effective methods to accurately assess the severity of the condition at an early stage in order to provide a basis for formulating targeted clinical treatment plans.
Computed tomography (CT) is commonly used to diagnose adhesive intestinal obstructions in clinical settings. CT scans can provide radiological characteristic data of the “transition zone” between dilated and collapsed bowel loops, which can help determine the cause of the intestinal obstruction. However, CT scans without contrast cannot assess the blood supply to the mesentery, which limits their application in judging the severity of the condition[4]. Ultrasound, a medical imaging technique that uses ultrasonic waves, can accurately reflect the anatomical structures of the various layers of human tissues. In the examination of adhesive intestinal obstruction, ultrasound can not only detect the adhesion bands in the “transition zone” but also display the blood supply of the intestinal wall, making it more valuable in application[5]. However, there are few reports on the value of ultrasound typing in judging the condition of patients with adhesive intestinal obstruction and formulating treatment plans. Therefore, this retrospective study was conducted using the medical records of 120 patients who were pathologically diagnosed with adhesive intestinal obstruction at Taihe Hospital Affiliated with Hubei Medical College between January 2022 and January 2024. The details are as follows.
This study was a retrospective review of 120 patients diagnosed with adhesive intestinal obstruction at Taihe Hospital Affiliated with Hubei Medical College from January 2022 to January 2024. Among them, there were 54 males (45.00%) and 66 females (55.00%). The age range was from 23 years to 70 years, with an average age of (46.50 ± 6.34) years. The body mass index ranged from 17 kg/m2 to 24 kg/m2, with an average of (20.50 ± 1.23) kg/m2. The time from onset of symptoms to visit was 1 days to 10 days, with an average of (5.50 ± 1.45) days. Medical history included a history of abdominal surgery in 103 patients (85.83%), gynecological surgery in 10 patients (8.33%), and a history of acute or chronic inflammation of the abdomen or intestine in seven patients (5.83%).
The inclusion criteria were as follows: (1) Diagnosis of adhesive intestinal obstruction according to clinical practice guidelines[6]; (2) All patients presenting with symptoms such as abdominal pain, distension, and vomiting; (3) All patients who underwent ultrasound examination; and (4) Patients who provided informed consent for their medical records to be included in the study. The exclusion criteria were as follows: (1) Patients with malignant tumors; (2) Patients unable to tolerate surgery; and (3) Patients who withdrew from the study midway.
A color doppler ultrasound diagnostic device (Manufacturer: General Electric Company, United States, Model: VOLUSON P8, Approval Number: National Medical Device Registration 20152061495) was used. Before the examination, it was confirmed that the patients had fasted for > 12 hours. Routine scanning of the abdominal organs was performed and patients with other diseases were excluded. A standard abdominal probe was used to comprehensively scan the intestines from top to bottom and left to right to examine the stomach, duodenum, small intestine, colon, abdominal cavity, and pelvis. A high-frequency probe was used to further inspect whether a lesion was detected during the examination.
Based on previous clinical ultrasound diagnostic experience, patient condition, and ultrasound image characteristics, and through multicenter research and expert consensus, ultrasound typing standards for the severity of adhesive intestinal obstruction were established. Further details are listed in Table 1.
| The severity of the condition | Ultrasound typing criteria |
| Simple type (mild) | Local intestinal adhesion: Local adhesion of the intestinal wall and intestinal wall and abdominal wall, no obvious abdominal-pelvic effusion, local intestinal expansion |
| Complex type (moderate) | There are extensive intestinal adhesions in the abdominal cavity, with adhesion band formation, adhesive masses, extensive intestinal dilatation, and a small amount of effusion in the abdominal and pelvic cavity |
| Critical condition type (severe type) | There were extensive abdominal adhesions, with intestinal ischemia and necrosis, and more effusion in the abdominal and pelvic cavity |
Conservative treatment for mild patients: This includes fasting, gastrointestinal decompression, enemas, anti-infection, use of acid suppressants and somatostatin, correction of water and electrolyte imbalances, and acid-base balance. All necessary examinations were performed during the treatment period. The emergency observation time ranged from 12 hours to 24 hours.
Surgical treatment for moderate and severe cases: Laparoscopic adhesiveness is performed for patients with adhesive intestinal obstruction; if the adhesions are too severe to be released, partial intestinal resection is performed. Emergency laparotomy was performed in cases of strangulation of the intestinal obstruction.
Based on the severity of ultrasound images, patients were classified as simple (mild), complex (moderate), or severe (severe), and the imaging characteristics of patients with different ultrasound types were analyzed. Treatment plans corresponding to the ultrasound typing results were formulated, including conservative and surgical treatments. The ultrasound signs of patients in the conservative and surgical treatment groups were compared.
The data for this study were processed using the statistical software SPSS 26.0. Qualitative data are presented as n (%) and analyzed using the χ2 test. Quantitative data are expressed as the mean ± SD and analyzed using the t-test. Statistical significance was set at P < 0.05.
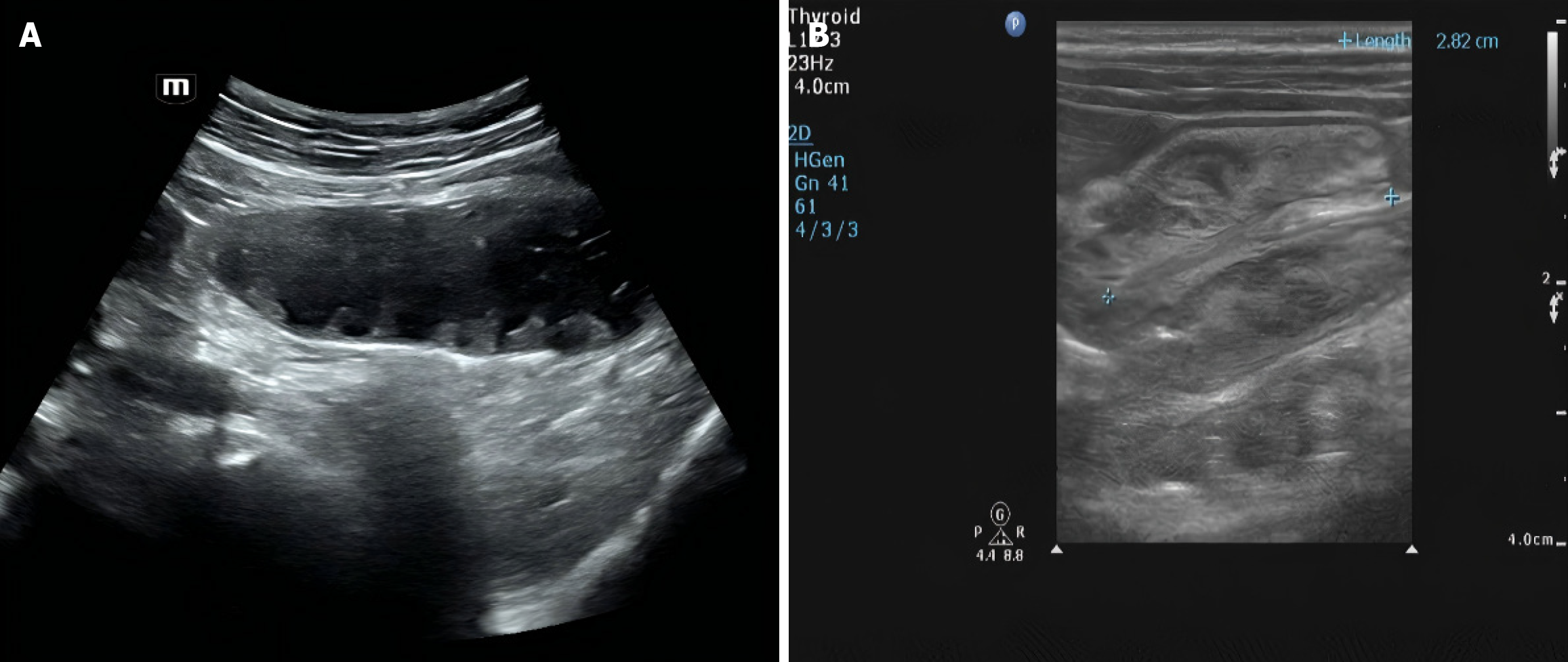
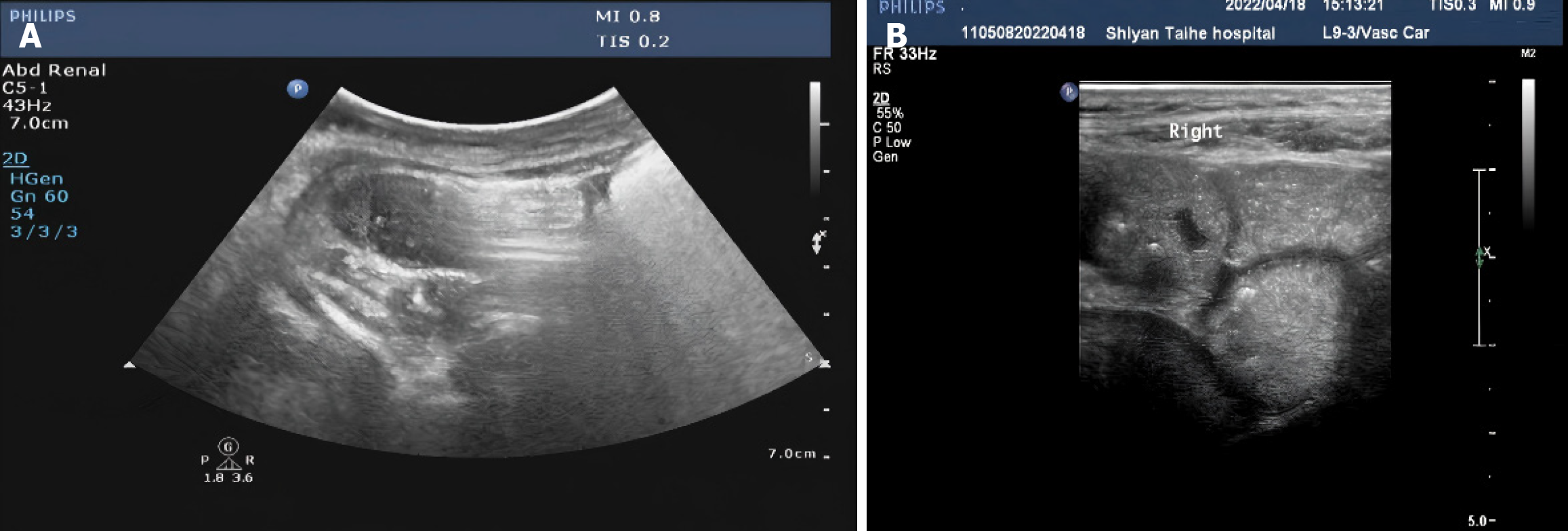
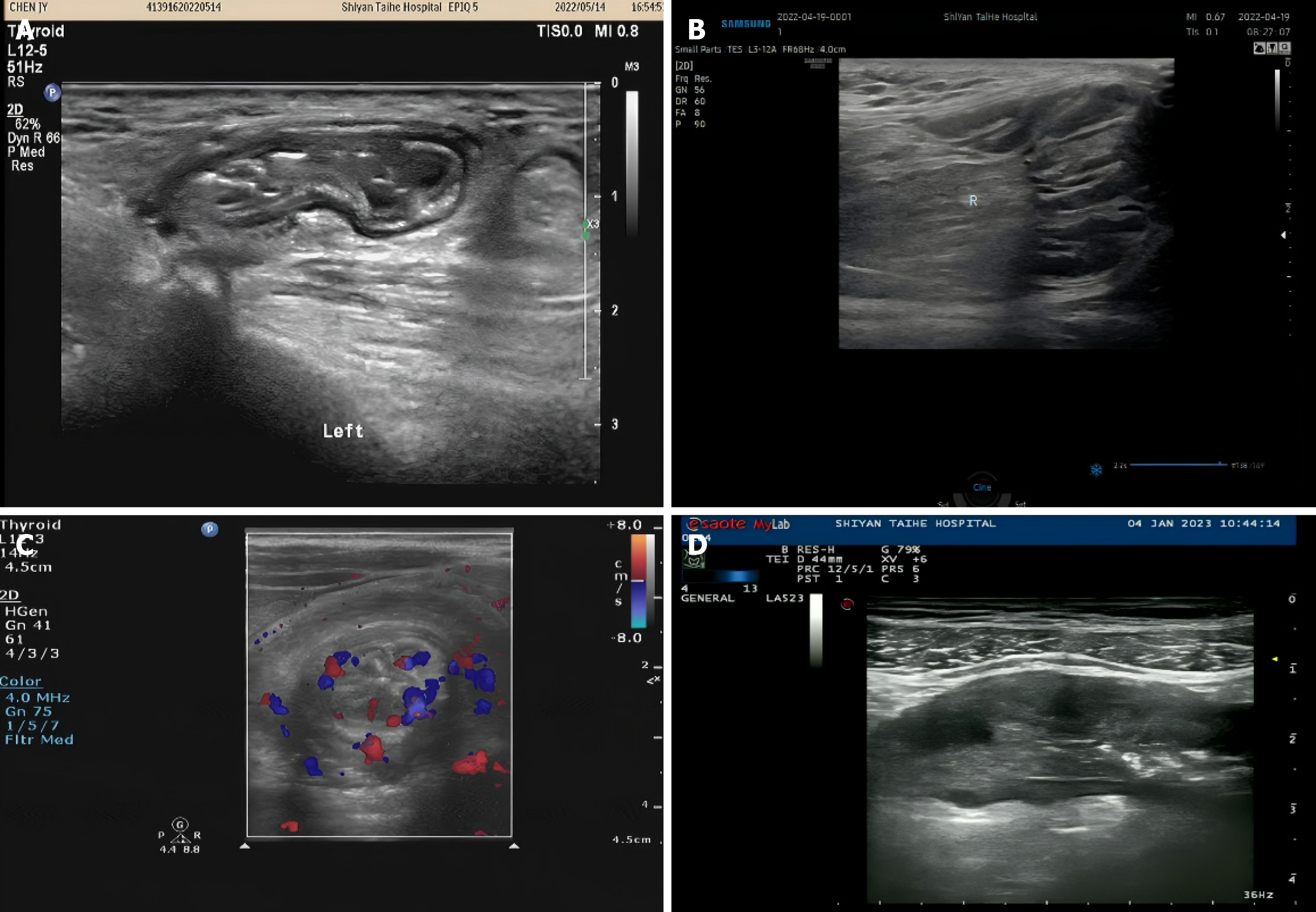
Among the 120 patients, 58 had the simple type (mild), 40 had the complex type (moderate), and 22 had the severe type (severe). In the mild patients, 52 cases had adhesion of the intestinal wall to the intestinal wall (Figure 1A), and 52 cases had adhesion of the intestinal wall to the abdominal wall (Figure 1B); in the moderate patients, 40 cases had adhesion of the intestinal wall to the intestinal wall, 20 cases had adhesion of the intestinal wall to the abdominal wall, 20 cases had adhesion bands (Figure 2A), and 20 cases had adhesive masses (Figure 2B); in the severe patients, 22 cases had adhesion of the intestinal wall to the intestinal wall, 22 cases had adhesion of the intestinal wall to the abdominal wall, 10 cases had formation of adhesion bands, 6 cases had adhesive masses, and 22 cases had complications of adhesive intestinal obstruction, with internal hernias/intestinal volvulus/internal hernias with volvulus/intussusception/intestinal ischemic necrosis occurring in 6 cases, 2 cases, 2 cases, 1 case, and 12 cases, respectively (Figure 3).
Among the 120 patients, 58 mild cases underwent conservative treatment and 62 moderate and severe cases underwent surgical treatment. There were no significant differences in general data (sex, age, body mass index, and duration from onset to consultation/medical history) between the conservative and surgical treatment groups (P > 0.05). When comparing the ultrasound signs of bowel dilatation and abdominal effusion between the two groups, P > 0.05. However, the proportions of adhesion masses and cross signs in the surgical treatment group were significantly higher than those in the conservative treatment group (P < 0.05) (Table 2).
| Item | Conservative treatment group (n = 58) | Surgical treatment group (n = 62) | χ2 (t) | P value | |
| Gender | Male | 25 (43.10) | 29 (46.77) | 0.163 | 0.686 |
| Female | 33 (56.90) | 33 (53.23) | |||
| Age (year), mean ± SD | 46.50 ± 6.34 | 46.35 ± 6.40 | (0.129) | 0.898 | |
| Body mass index (kg/m2), mean ± SD | 20.50 ± 1.23 | 20.40 ± 1.30 | (0.432) | 0.666 | |
| Time of onset to presentation (day), mean ± SD | 5.50 ± 1.45 | 5.48 ± 1.46 | (0.075) | 0.940 | |
| Medical history of the disease | History of abdominal surgery | 50 (86.21) | 53 (85.48) | 0.012 | 0.909 |
| History of gynecological surgery | 5 (8.62) | 5 (8.06) | 0.048 | 0.825 | |
| History of acute and chronic inflammation in the abdominal cavity or bowel | 3 (5.17) | 4 (6.45) | 0.008 | 0.927 | |
| Ultrasonic sign | Dilatation of intestine | 49 (84.48) | 59 (95.16) | 3.796 | 0.051 |
| Pyoperitoneum | 38 (65.52) | 50 (80.65) | 3.506 | 0.061 | |
| Adhesion block | 35 (60.34) | 58 (93.55) | 12.958 | 0.000 | |
| Decussation | 5 (8.62) | 54 (87.10) | 73.840 | 0.000 | |
Intestinal obstruction is a common acute abdominal condition encountered in clinical surgery and is often caused by intestinal adhesions, tumors, intestinal inflammation, and hernias, with adhesive intestinal obstruction being the most common[7,8]. Adhesive intestinal obstruction has a sudden onset and rapidly changing condition, making the early selection of the best treatment plan crucial. Early determination of the lesion site and severity of the condition are key to deciding whether to adopt conservative or surgical treatment[9]. Combining the patient's typical manifestations with the results of abdominal radiographic examinations can roughly determine whether the patient has an intestinal obstruction and its specific location; however, it cannot accurately assess the progression of the condition. CT is also a commonly used imaging technology in clinical management, providing doctors with more condition information; however, this examination technique requires strict control over the radiation dose and usage frequency, which have limitations[10].
The widespread adoption and continuous advancement of ultrasound technology has led to its increasingly broad application in clinical practice. It has been reported that the sensitivity of ultrasound for diagnosing intestinal obstruction reaches 92.40%, with a specificity as high as 96.60%[11]. However, there are few reports on the value of ultrasound typing in determining the severity of adhesive intestinal obstruction and treatment plans. This article conducts a retrospective study aimed to provide guidance for the clinical assessment of disease severity and formulation of treatment plans. In this study, 120 patients with adhesive intestinal obstruction were classified based on their clinical experience and ultrasound signs, resulting in 58 cases of simple obstruction, 40 cases of complex obstruction, and 22 cases of severe obstruction. By analyzing the imaging characteristics of patients with different ultrasound types, we found that patients with the simple type (mild) mainly exhibited adhesion of the intestinal wall to the intestinal wall and adhesion of the intestinal wall to the abdominal wall. Patients with the complex type (moderate) also showed adhesion bands and adhesive masses, whereas those with the severe type (severe) had complications such as internal hernias (6 cases), intestinal volvulus (2 cases), internal hernias with volvulus (2 cases), intussusception (1 case), and intestinal ischemic necrosis (12 cases) on imaging[12]. The analysis suggests that in severely ill patients, the occurrence of intestinal volvulus can also lead to the corresponding obstruction of the mesenteric vessels. Internal hernias and intestinal volvuli often lead to a closed loop and strangulated intestinal obstruction[13,14]. If the contents of the closed-loop intestine cannot be expelled, bloody transudates will increase in the intestinal lumen (due to strangulation). In more severe cases, adhesion bands further compress the intestines, leading to local vascular obstruction, and ultimately causing internal hernias. It is evident that ultrasound typing imaging characteristics are closely related to the progression of a patient's condition, and clinicians can judge the severity of the condition based on the results of ultrasound typing[15-17].
Treatment methods for adhesive intestinal obstruction include conservative and surgical treatments. The use of effective factors to guide the formulation of preoperative treatment plans can ensure better therapeutic effects[18-20]. This study also found that the proportion of bowel dilatation and abdominal effusion between the two groups (P > 0.05), and the proportion of adhesion masses and cross-signs in the surgical treatment group were higher than those in the conservative treatment group (P < 0.05), indicating that there was a difference in ultrasound signs between patients who underwent conservative or surgical treatment[21]. The conclusions of section 2.1 of this study showed that patients with the complex type (moderate) and severe type (severe) have adhesion masses and cross-signs on their ultrasound images[22]. Table 2 suggests that patients undergoing surgical treatment had a higher proportion of adhesion masses and cross signs on their ultrasound images. As patients undergoing surgical treatment are mostly those with severe conditions, it is speculated that ultrasound typing can guide clinical physicians in formulating treatment plans. However, clinical practice has not yet reached an accurate conclusion and further exploration is required[23,24].
In conclusion, this study demonstrated that ultrasound classification holds significant value in both condition judgment and formulation of treatment plans for patients with adhesive intestinal obstruction. Specifically, ultrasound typing criteria established through multicenter research and expert consensus have proven reliable and effective in guiding clinical decision-making. These criteria not only allow for a more accurate assessment of disease severity but also provide a solid basis for clinicians to tailor treatment plans according to specific ultrasound findings.
| 1. | Kuremu RT, Jumbi G. Adhesive intestinal obstruction. East Afr Med J. 2006;83:333-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Xie Y, Zheng C, Tan X, Li Z, Zhang Y, Liu Y. Clinical efficacy of acupuncture in patients with adhesive intestinal obstruction: A meta-analysis. Medicine (Baltimore). 2022;101:e30257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 3. | Takamizawa Y, Kobayashi Y. Adhesive intestinal obstruction caused by extragastrointestinal anisakiasis. Am J Trop Med Hyg. 2015;92:675-676. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Borisenko VB, Kovalev AN, Denysiuk TА. Role and place of ultrasonography in diagnostics of adhesive intestinal obstruction. Wiad Lek. 2020;73:83-86. [PubMed] |
| 5. | Bevan PG. Adhesive obstruction. Ann R Coll Surg Engl. 1984;66:164-169. [PubMed] |
| 6. | Alavi K, Poylin V, Davids JS, Patel SV, Felder S, Valente MA, Paquette IM, Feingold DL; Prepared on behalf of the Clinical Practice Guidelines Committee of the American Society of Colon and Rectal Surgeons. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Management of Colonic Volvulus and Acute Colonic Pseudo-Obstruction. Dis Colon Rectum. 2021;64:1046-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 81] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 7. | Mikhin IV, Kosivtsov OA, Abramyan EI, Ryaskov LA. [Application of anti-adhesive barrier for recurrent acute adhesive intestinal obstruction]. Khirurgiia (Mosk). 2019;90-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Kono J, Yoshimaru K, Kondo T, Takahashi Y, Toriigahara Y, Fukuta A, Obata S, Kawakubo N, Nagata K, Matsuura T, Tajiri T. The Volume of Intestinal Decompression can Predict the Necessity of Surgical Intervention for Adhesive Small Bowel Obstruction. J Pediatr Surg. 2023;58:1252-1257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Nguyen ATM, Holland AJA. Paediatric adhesive bowel obstruction: a systematic review. Pediatr Surg Int. 2021;37:755-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Saklani AP, Naguib N, Shah PR, Mekhail P, Winstanley S, Masoud AG. Adhesive intestinal obstruction in laparoscopic vs open colorectal resection. Colorectal Dis. 2013;15:80-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Zins M, Millet I, Taourel P. Adhesive Small Bowel Obstruction: Predictive Radiology to Improve Patient Management. Radiology. 2020;296:480-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 58] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 12. | Tyagunov AE, Tyagunov AA, Nechay TV, Vinogradov VN, Kurashinova LS, Sazhin AV. Timing of surgery, intestinal ischemia and other real factors of mortality in acute adhesive small bowel obstruction: a multiple-center study. Khirurgiia (Mosk). 2021;26-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Beglaibter N, Mazeh H. Adhesive Small-Bowel Obstruction-Surgery for All? JAMA Surg. 2019;154:1075-1076. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Behman R, Nathens AB, Karanicolas P. Adhesive Small-Bowel Obstruction-Surgery for All?-Reply. JAMA Surg. 2019;154:1076-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 15. | Podda M, Khan M, Di Saverio S. Adhesive Small Bowel Obstruction and the six w's: Who, How, Why, When, What, and Where to diagnose and operate? Scand J Surg. 2021;110:159-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (1)] |
| 16. | Osifo OD, Ovueni ME. Is nonoperative management of adhesive intestinal obstruction applicable to children in a resource-poor country? Afr J Paediatr Surg. 2010;7:66-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Tseng CC, Tseng A. Effect of acupuncture on postoperative adhesive intestinal obstruction. Acupunct Med. 2015;33:338-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Fujii K, Washida N, Arai E, Tsuruta M, Wakino S, Itoh H. Adhesive intestinal obstruction increases the risk of intestinal perforation in peritoneal dialysis patients: a case report. BMC Nephrol. 2018;19:153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Ha GW, Lee MR, Kim JH. Adhesive small bowel obstruction after laparoscopic and open colorectal surgery: a systematic review and meta-analysis. Am J Surg. 2016;212:527-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 20. | Fliegner MA, Finn D, Wilhelm S, Keeley J, Stallion A, Novotny N, Akay B, Brahmamdam P. My thoughts: The role of water-soluble contrast challenge for adhesive small bowel obstruction in children. Am J Surg. 2024;236:115838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Sisodia V, Sahu SK, Kumar S. Clinical Profile of Patients with Postoperative Adhesive Intestinal Obstruction and its Association with Intraoperative Peritoneal Adhesion Index. Chirurgia (Bucur). 2016;111:251-258. [PubMed] |
| 22. | Scotté M, Mauvais F, Bubenheim M, Cossé C, Suaud L, Savoye-Collet C, Plenier I, Péquignot A, Yzet T, Regimbeau JM. Use of water-soluble contrast medium (gastrografin) does not decrease the need for operative intervention nor the duration of hospital stay in uncomplicated acute adhesive small bowel obstruction? A multicenter, randomized, clinical trial (Adhesive Small Bowel Obstruction Study) and systematic review. Surgery. 2017;161:1315-1325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 23. | Timofeev ME, Larichev SE, Fedorov ED, Polushkin VG, Shapoval'iants SG. [Laparoscopic diagnosis and treatment of acute early adhesive intestinal obstruction]. Khirurgiia (Mosk). 2015;46-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Kim J, Lee Y, Yoon JH, Lee HJ, Lim YJ, Yi J, Jung WB. Non-strangulated adhesive small bowel obstruction: CT findings predicting outcome of conservative treatment. Eur Radiol. 2021;31:1597-1607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/