INTRODUCTION
In 1987, Phillipe Mouret introduced the first laparoscopic cholecystectomy (LC)[1], marking the advent of minimally-invasive techniques in general surgery. LC is now the gold standard for treating benign gallbladder diseases, surpassing laparotomy, and is widely adopted globally[2]. Advancements in laparoscopic instruments and technology have established "non-invasive" surgery, represented by natural orifice translumenal endoscopic surgery (NOTES) and laparoendoscopic single-site surgery (LESS), as the leading trend in minimally-invasive procedures[3]. Compared to NOTES, LESS is a promising "non-invasive" technique with less operational complexity, using the umbilicus to hide the scar and therefore achieving similar cosmetic results[4]. Navarra et al[5] documented the first single-incision LC (SILC) in 1997, and since then, a substantial body of clinical experience has been described[6,7]. Among the rapidly developing SILC techniques, transumbilical SILC is increasingly replacing the traditional LC, with advantages of minimal invasion, slight postoperative pain, faster recovery, and higher safety. It has even been predicted by some scholars that SILC will become a standard approach for cholecystectomy[8,9].
Despite the advantages mentioned above, the currently available specialized single-port laparoscopic instruments are hindered by high costs and limited applications, challenging their widespread use in medical facilities. Therefore, based on the anatomic features of the Calot's triangle (or cystohepatic triangle), we designed a two-point lifting/retracting (TPLR) technique for transumbilical single-port LC (TUSPLC), which enabled single-port LC utilizing conventional laparoscopic instruments. From June 2023 to June 2024, a total of 103 patients underwent TUSPLC in our hospital using this technique, which yielded favorable clinical outcomes.
MATERIALS AND METHODS
Clinical data
We performed TUSPLC using the TPLR technique in 103 patients diagnosed with gallbladder diseases between June 2023 and June 2024 at our hospital. Ethical approval was granted by the Hospital Ethics Committee (Approval No. 2023-001-05).
The inclusion criteria were as follows: (1) Age between 18 and 70 years; (2) With a body mass index (BMI) of 40 kg/m² or less; (3) With a preoperative diagnosis of cholelithiasis, gallbladder polyps, or gallbladder adenomyomatosis; and (4) Willing to adhere to the procedural protocols and provide written informed consent for surgical intervention. The exclusion criteria included: (1) An American Society of Anesthesiologists Physical Status level of IV or V; (2) Refusal to undergo laparoscopic surgical intervention; (3) Preoperative suspicion of Mirizzi syndrome, choledocholithiasis, or gallbladder malignancy; (4) Prior history of upper abdominal surgical procedures; (5) Long-term anticoagulant therapy; and (6) Concurrent acute cholangitis.
This study cohort included 45 males and 58 females, aged 22-67 years (mean: 47 ± 13.6 years). The diagnoses included cholelithiasis (n = 82), gallbladder polyps (n = 11), concurrent gallstones and polyps (n = 6), adenomyomatosis of the gallbladder (n = 4), and acute cholecystitis (n = 14). The onset of the disease was within 72 hours, and the patients concerned about cosmetic outcomes. The duration of the disease varied from 8 hours to 11 years, with an average disease duration of 7 months. The clinical presentations were recurrent right upper quadrant distension pain or completely asymptomatic. Preoperative assessments included a blood routine examination, liver and renal function tests, as well as abdominal color Doppler ultrasound and B-mode ultrasonography.
Surgical methods
Instruments and materials: The surgical equipment utilized included 5-mm and 10-mm trocars, non-absorbable clips (Kanger, Tonglu, Zhejiang, China), absorbable bioclips (Covidien, Shanghai, China), 3-0 absorbable sutures (Johnson & Johnson, Shanghai, China), a 30° laparoscope (Olympus, Japan) and various domestically made laparoscopic instruments including a suction device, dissecting forceps, release clamps, scissors, and hooks, each measuring 400 mm in length and 4.5 mm in diameter.
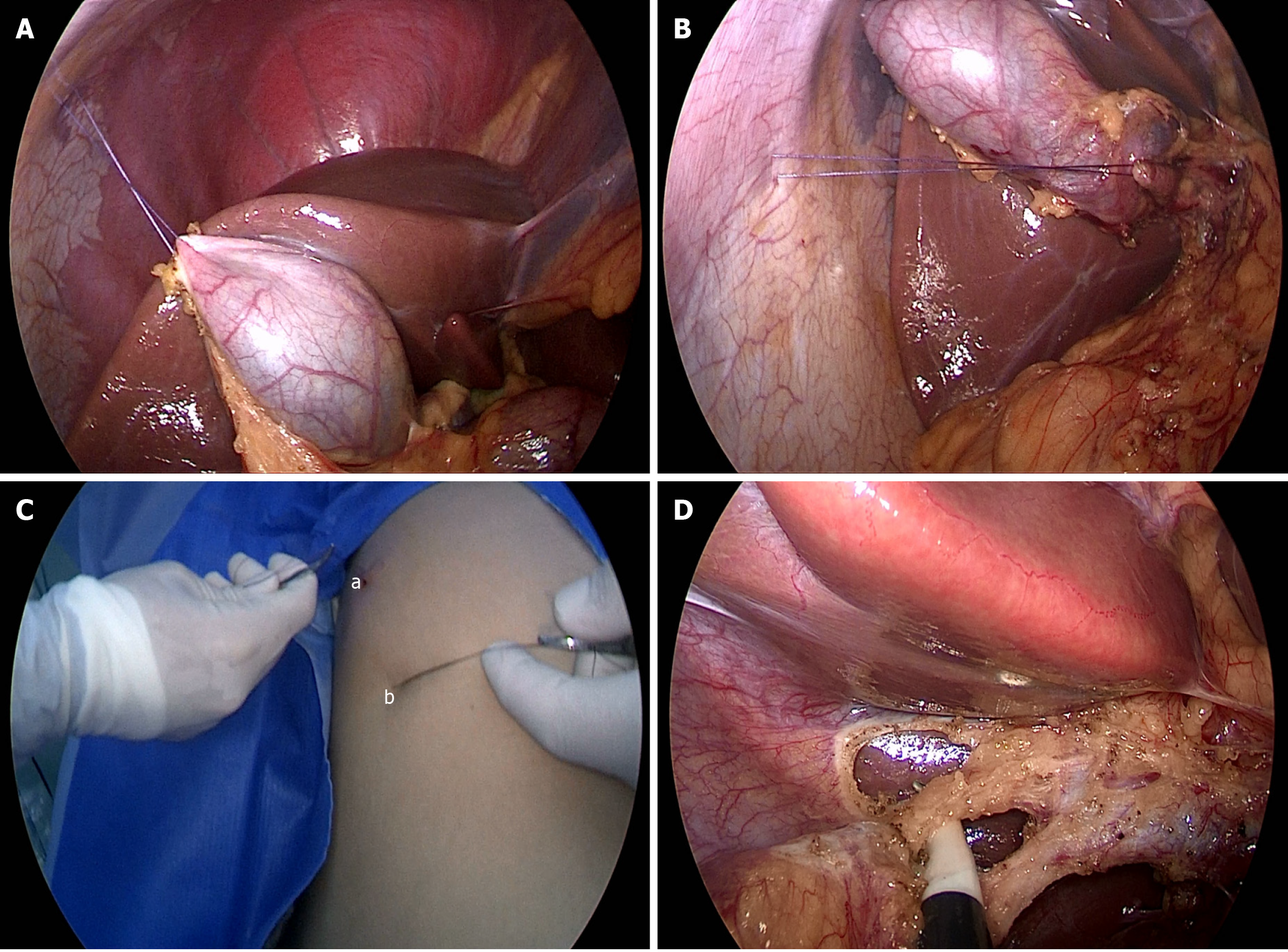
Surgical procedures: Under general anesthesia, the patient was positioned in the reverse Trendelenburg position. A pneumoperitoneum was established with CO2 at a pressure of 12 mm H2O. A 15-mm arcuate skin incision was made at the medial margin of the umbilical ring, through which a 10-mm trocar was inserted to facilitate laparoscopic entry. Subsequently, a 5-mm trocar was placed at an interval within the tissue to accommodate the manipulation of surgical instruments. The abdominal cavity was explored first and the degree of gallbladder inflammation was observed. In the event of adhesions, an electrocautery hook was employed to dissect the adhesions at the fundus of the gallbladder, thereby exposing the gallbladder's base. A 3-0 absorbable suture was placed after puncturing at the level of the 8th to 9th intercostal space along the right midclavicular line to lift the gallbladder fundus superiorly. The adhesions at the base and body of gallbladder were dissected one after another using the electrocautery hook to fully expose the ductal canal. Thereafter, a 3-0 absorbable suture was inserted via puncturing 5 cm inferior to the right costal margin along the anterior axillary line to retract the gallbladder's ampulla inferiorly and rightwards (Figure 1A-C). Following this dual-point lifting/retracting, the structure of the Calot's triangle was fully visualized. The anatomical landmarks of these two regions were then utilized to delineate the cystic duct, cystic artery, and common bile duct (Figure 1D). The cystic duct and artery were carefully dissected using an electrocautery hook through a trocar at the left lateral umbilical aspect. Subsequently, the 5-mm trocar positioned on the left side of the umbilicus was replaced with a 10-mm trocar to facilitate the manipulation of clamps and serve as a conduit for the extraction of the gallbladder. The cystic artery was disconnected after being clamped with absorbable bioclips. After an absorbable clip was placed on the proximal end of the cystic duct and a non-absorbable clip on the distal end, the cystic duct was transected, and the gallbladder was removed both anterogradely and retrogradely. Following electrocoagulation of the gallbladder bed to ensure hemostasis, the gallbladder was then divided (Video 1). Postoperatively, a long-acting ropivacaine solution was administered around the umbilical incision.
Figure 1 Transumbilical single-port laparoscopic cholecystectomy using the two-point lifting/retracting technique.
A: The gallbladder fundus is lifted superiorly; B: The gallbladder ampulla is retracted inferiorly and rightwards; C: A-the external puncture site is located at the 8-9th intercostal space along the right midclavicular line; b-the external puncture site is located 5 cm below the right costal margin along the anterior axillary line; D: A-cystic duct; b-common bile duct; c-cystic artery.
DISCUSSION
With advances in minimally-invasive surgical techniques, LC has increasingly supplanted open cholecystectomy as the gold standard for the management of benign gallbladder disorders[10]. In response to the rising demand for cosmetic outcomes and the rapid advancement of minimally invasive procedures, LC has evolved through various stages, including four-port, three-port, two-port techniques, and robotic surgery. However, the realization of a scar-free surgical approach has remained elusive[11]. Consequently, it has become inevitable to explore minimally-invasive surgical techniques that utilize a single incision or even zero port. In 2006, Ko and Kalloo[12] documented that an animal study employing NOTES resulted in the successful elimination of surface scarring postoperatively. Nevertheless, NOTES has numerous limitations and drawbacks, including challenges related to the surgical approach, instruments, and infections[13]. LESS represents a further refinement in minimally-invasive techniques beyond conventional laparoscopic methods. It reduces puncture sites and conceals them within the umbilical fold, thereby achieving a similar scar-free outcome as NOTES while effectively circumventing many of the drawbacks associated with NOTES[14]. Currently, LESS has been applied in general surgery, gynecology, and urology, with cholecystectomy being the most established procedure among those applications[15,16]. According to the literature, unfortunately, most SILC procedures employed specialized single-port laparoscopic instruments, which are highly expensive and also non-reusable, posing challenges to their widespread application in clinical settings[17,18]. In some SILCs where surgeons use conventional instruments, there is excessive concentration of the device placement site, resulting in the instruments interfering with each other outside the body; in addition, the concentration of instruments inside the body can also interfere with the operation and affect the exposure of the surgical field. These factors are frequently cited as contributors to the failure of SILC procedures[19]. Hence, by leveraging the anatomical features of the Calot's triangle and drawing upon the experience documented in the literature, we have developed an economical, practical, and promotionally viable TPLR technique for TUSPLC.
The Calot's triangle is an anatomical region delineated by the cystic duct, common hepatic duct, and the inferior border of the right liver lobe. It is traversed by the right hepatic artery, cystic artery, and para-right hepatic duct. Laparoscopic surgery within the Calot's triangle permits clear visualization of the anatomical structures, thereby reducing the likelihood of inadvertently damaging adjacent vital tissues[20]. Within this region, the maximal visualization of the dimensions of Calot's triangle allows for clear demarcation of the cystic duct, common hepatic duct, common bile duct, and the ampulla of Vater, thereby significantly diminishing the risk of iatrogenic bile duct injury[21]. Furthermore, the posterior Calot's triangle exhibits broader anatomical features in comparison to the anterior Calot's triangle. Its surface is enveloped by a serous membrane, devoid of the main trunk of the cystic artery. The tissue within the posterior Calot's triangle is relatively loose and therefore is easy to separate. In instances where the gallbladder exhibits significant adhesion to the surrounding tissues, dissection from the posterior Calot's triangle is much more easy to perform[22]. Thus, based on the anatomical features of the Calot's triangle and to address the challenges associated with exposing the Calot's triangle during single-port laparoscopic procedures, we introduced the concept of TPLR, which involves lifting the gallbladder fundus with sutures and retracting the gallbladder ampulla during the procedure. This maneuver ultimately yields a clearly-defined three-point structure comprising the gallbladder fundus, gallbladder ampulla, and the confluence between the cystic duct and common hepatic duct, which configures an obtuse-angled triangle. Consequently, the three ducts and one ampulla are effectively visualized. In cases where there is a minimal degree of adhesion between the gallbladder and its surrounding tissues, the TPLR technique enables the elevation (upwards) and retraction (rightwards and downwards) of the two suspension points. As a result, the anterior Calot's triangle is dilated, positioning the cystic duct and common bile duct at approximately right angles to each other. At this juncture, the gallbladder neck can be effectively dissected using an electrocautery hook, which facilitates improved manipulation and a safer dissection of the adipose tissue and cystic duct within the Calot's triangle[23]. In summary, the TPLR technique not only ensures complete exposure of the Calot's triangle but also reduces instruments required within the abdominal cavity. By addressing the issue of instrument cross-interference during SILC when utilizing conventional instruments, it significantly increases the operational workspace and mitigates the challenges associated with the surgical procedure.
In the cohort of 103 patients in the present study, three cases required the addition of an operative port beneath the xiphoid process due to profound local tissue adhesion involving the gallbladder. Two cases were converted to conventional three-port LC as a result of acute cholecystitis. Hence, careful selection of indications is crucial for the success of SILC. Despite the lack of documentary evidence, the potential indications for SILC may include a normal BMI, absence of comorbidities such as acute infection, and aged 60 years or younger[24]. However, it has also been proposed that the procedure may also be indicated in individuals with a BMI exceeding 30 or in patients who present with symptoms of acute cholecystitis[25]. Although we prefer broader indications for SILC, SILC is contraindicated at our center for patients who are obese (with a BMI greater than 40), have a tall stature, have a recent history of recurrent gallbladder inflammation, have experienced acute cholecystitis for a duration exceeding 72 hours, and/or have a previous history of abdominal surgery.
In contrast to the conventional three-port LC, the TUSPLC using TPLR technique has the advantages of quick recovery, markedly diminished incisional pain, and an enhanced aesthetic outcome, basically realizing a "scar-free" appearance. Additionally, this technique shortens hospital stay without a considerable escalation in hospitalization expenses. In addition, the procedure exhibits a reduced dependence on specialized surgical instrumentation, we investigated the use of disposable specialized single port laparoscopic instruments for cholecystectomy in China, with an average hospitalization cost of 1600 to 2000 USD. In contrast, the TUSPLC using TPLR technique for transumbilical single port LC had an average hospitalization cost of 1100 to 1300 USD[26,27], thereby circumventing the economic constraints imposed by the utilization of disposable specialized single-port laparoscopic devices.
Furthermore, it has a short learning curve. For institutions that have introduced LC, this new technique is simple, safe, feasible, and cost-effective, justifying its promotion in clinical settings. However, for patients with severe pericholecystic adhesions and those who are obese, TUSPLC using TPLR technique remains difficult. It is expected that with the accumulation of surgical experience, TUSPLC using TPLR technique will gain broader applications.