Published online Jul 27, 2025. doi: 10.4240/wjgs.v17.i7.103736
Revised: March 22, 2025
Accepted: May 27, 2025
Published online: July 27, 2025
Processing time: 140 Days and 4 Hours
Endoscopic colon polypectomy is a common procedure used to remove polyps that may develop into colorectal cancer if left untreated. Despite these advantages, patients frequently experience anxiety and other adverse reactions. Standardized evidence-based nursing practices are essential for enhancing patient care by addressing both physical and psychological health issues.
To analyze the impact of standardized evidence-based nursing on psychological status and adverse reactions of patients undergoing endoscopic colonic polypectomy.
Data from 200 patients who underwent endoscopic colonic polypectomy at the authors’ hospital between January and June 2024 were randomly assigned to two groups: Control [received routine nursing care (n = 100)] and study [received standardized evidence-based nursing intervention(s) (n = 100)]. Psychological status, visual analog scale, and Short-Form 36 Health Survey scores, adverse events, and satisfaction with nursing were compared between the two groups.
After the interventions, the study group exhibited significantly lower scores on the Hamilton Anxiety Rating Scale and Hamilton Depression Rating Scale, along with a reduced incidence of adverse events compared with the control group (P < 0.05). Short-Form 36 Health Survey scores and overall satisfaction with nursing care were also significantly higher in the intervention group (P < 0.05).
Standardized evidence-based nursing interventions effectively reduced negative patient emotions and enhanced quality of life and satisfaction, demonstrating high safety.
Core Tip: After undergoing endoscopic removal of colon polyps, patients often experience anxiety and other adverse reactions. Standardized evidence-based nursing practices are crucial for improving patient care by addressing both physical and mental health issues. To analyze the impact of standardized evidence-based nursing on the psychological status and adverse reactions of patients undergoing endoscopic colonic polypectomies. We found that standardized evidence-based nursing interventions effectively reduced negative patient emotions and enhanced the quality of life and satisfaction, demonstrating high safety.
- Citation: Tan C, Wu ZJ, He R, Feng L. Influence of standardized evidence-based nursing practices on mental state and adverse effects in patients undergoing endoscopic colon polypectomy. World J Gastrointest Surg 2025; 17(7): 103736
- URL: https://www.wjgnet.com/1948-9366/full/v17/i7/103736.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i7.103736
Colon cancer is a leading cause of mortality worldwide[1]. Despite significant advances in our understanding of its pathogenesis, the precise causes remain unclear. Community-based screening is vital for early diagnosis and significantly improves treatment outcomes[2]. The survival rate of patients with colon cancer is influenced by factors such as local recurrence, lymphatic metastasis, and hematogenous spread[3], whereas immune system and molecular dysregulation contribute to tumor recurrence and metastasis[4]. Colonic polyps are common and affect more than 50% of individuals over the age of 60[5]. Colonic polyps include hyperplastic, inflammatory, and adenomatous types, with specific types showing potential to grow rapidly and progress to cancer.
Endoscopic polypectomy of the colon is a new, minimally invasive surgical technique commonly used to treat colonic polyps[6]. Small adenomatous polyps can be resected directly using colonoscopic electrocoagulation. For pedicled polyps with a diameter of > 2 cm, the root of the polyp tissue can be lapped under colonoscopy and resected using electrocoagulation[7]. Compared with traditional surgery, endoscopic resection can significantly reduce damage to the patient’s body, and the procedure is simple, convenient, and easy to perform[8]. However, the essence of this technique remains within the surgical scope. As such, damage to the patient’s body is difficult to avoid, and patients are prone to fear invasive surgical treatment, resulting in physiological and psychological stress reactions that are not conducive to smooth surgical treatment. Therefore, it is necessary to perform appropriate nursing interventions according to the physical and mental characteristics of the patients during the perioperative period to minimize the impact of adverse reactions on surgical treatment and postoperative recovery.
Evidence-based nursing involves approaching clinical nursing problems based upon the most current, relevant research available[9]. As a model, this approach advocates for integrated care, disease management, and the use of evidence-based care guidelines[10]. Evidence-based nursing aims to identify address clinical problems in a structured manner using relevant scientific research and critically reviewing the effectiveness and practicability of scientific research evidence[11]. This approach to nursing involves the practical application of evidence from research, the formulation of implementation plans, and an evaluation of the effects of their application, which are subsequently used to review nursing plans to improve the scientific nature of nursing measures[12]. The application of standardized evidence-based nursing in the care of patients after endoscopic colon polypectomy has the potential to reform nursing practices for this procedure, ensuring that the implemented nursing interventions meet the current standards[13]. This study retrospectively analyzed the clinical data of patients who underwent endoscopic resection of colonic polyps. The application of standardized evidence-based nursing in the perioperative period is discussed with the objective of providing a reference for clinical treatment.
Data were retrospectively collected from 200 patients who underwent endoscopic colon polypectomy and received treatment at our hospital between January and June in 2024. Patients were randomly assigned to one of the two groups using the random number table method as follows: Control [received routine nursing care (n = 100)] and study [received standardized evidence-based nursing intervention (n = 100)].
The inclusion criteria were as follows[14]: Symptoms consistent with the diagnostic criteria for intestinal polyps in the diagnosis and treatment of gastroenterological diseases confirmed by colonoscopy, endoscopic resection of intestinal polyps for the first time, and complete clinical data. Individuals with severe liver and kidney dysfunction, malignant tumor(s), serious blood system diseases, coagulation disorders, or other gastrointestinal diseases were excluded.
This study was approved by the research ethics committee of the authors’ institution and conducted in accordance with the Declaration of Helsinki and its later amendments. All the patients provided written informed consent to participate in this study.
The control group received routine care by nurses, including: Assisting patients to improve preoperative examination, verbal explanations of intestinal polyp disease and endoscopic surgery-related knowledge, encouragement to cooperate with treatment, devoting attention to changes in patient vital signs during the procedure, cooperating with the surgeon to deliver instruments, closely monitoring changes in patient signs and conditions after the operation, encouraging patients to take their medication according to the physicians’ advice, and encouraging patients to resume their diet and ambulate as soon as possible.
The study group received standardized evidence-based nursing interventions based on the following criteria: (1) Setting up a standardized evidence-based nursing team: Nurses that had rich clinical experience were assigned to patients in this group to establish a standardized evidence-based nursing team to provide evidence-based nursing knowledge to patients. All team members had a clear division of labor, worked according to their respective tasks, and provided nursing services in strict accordance with team management standards to ensure that all patients received the best care; (2) Propose evidence-based problems: Identify prior problems in nursing practices, conduct a comprehensive analysis combined with clinical experience, and study each case through group discussions to determine the causes of the nursing problems. All analysis results were sorted into books and divided into common and rare problems according to the actual situation. Common problems that needed immediate improvement were analyzed to determine evidence-based solutions; (3) Search for evidence-based support in multiple ways according to evidence-based problems, including searching for relevant literature, consulting professionals, brainstorming, and striving to explore solutions comprehensively. The solution measures were sorted individually and reasonable modifications and adjustments were made according to the actual situation to ensure that each measure had an objective basis and was practical; (4) Implementation of standardized evidence-based nursing. Intestinal preparation: Two days before surgery, patients were placed on a diet of low-fat soft food with fasting on the day of surgery. Patients were placed in a left kneeling position to ensure comfort. Nurses quickly and accurately provided the physician with surgical instruments to avoid harm to the patient and closely observed their physiological indicators for signs of an abnormal report or a need for timely treatment. When the endoscope passed through the transverse colon, the patient was allowed to adjust to the right lateral position to ensure effective passage through the transverse colon and liver flexure. Once the patients were awake, they were transferred back to the ward and instructed to fast for 6 hours, and interventions such as fluid rehydration and hemostasis were performed. Patients were guided to maintain adequate sleep after surgery and gradually transition from a liquid diet to a common diet after no abnormal digestive reaction. Patients were placed on a diet of light and non-slag soft food and advised to maintain balanced nutrition, refraining from irritating food. The visual analog scale (VAS) score was used to evaluate patient pain levels every 6 hours after surgery, and analgesic drugs were used as required. Simultaneously, patients were encouraged to occupy their time by reading books or listening to music and relieve postoperative discomfort by adjusting their position or body massages; and (5) Testing the nursing effect: Evaluating the effect of implementing standardized evidence-based nursing, rationally applying the corresponding evaluation tools, clarifying the advantages and disadvantages of nursing measures, performing in-depth analysis and research on the problems, and further optimizing the nursing program.
Psychological state: The Hamilton Anxiety Rating Scale (HAM-A)[15] consists of 14 items scored on a five-point scale ranging from 0 to 4. A higher score indicates a greater degree of anxiety. The Hamilton Depression Rating Scale (HAM-D) consists of 17 items, with items 1, 2, 3, 7, 8, 9, 10, 11, 15, and 17 scored on a scale of 0-4 points and items 4, 5, 6, 12, 13, 14, and 16 scored on a scale of 0-2 points. The higher the score, the more severe the degree of depression.
VAS score: The VAS score ranges from 0 to 10, with higher scores indicating more severe pain[16].
Short Form-36 Health Survey score: The higher the final score, the better the patient’s quality of life (total score of 100 points). The Short Form-36 Health Survey (SF-36) has eight items: General health, social function, physical function, emotional function, physiological role, physical pain, mental health, and vitality[17].
Adverse reactions: Indicators of adverse reactions included perforation, bleeding, abdominal distension, abdominal pain, constipation, black stool, nausea, and vomiting.
Nursing satisfaction: Nursing satisfaction was assessed using a nursing satisfaction questionnaire administered to the patients. Scores < 60 were considered to be “unsatisfactory”, indicating that patients believed that clinical nursing had no significant effect on the improvement of their psychological status, comfort level, and degree of pain. Scores of 60-85 represented “fundamentally satisfied”, indicating that patients believed that the clinical nursing had some effect on the improvement of their own psychological condition, comfort and degree of pain. Scores > 85 represented “very satisfied”, indicating that patients believed that clinical nursing had a significant effect on the improvement of their psychological condition, comfort, and degree of pain: Total satisfaction rate = (satisfied + unsatisfied/total) × 100.
All statistical analyses were performed using the SPSS version 26.0 (IBM Corp., Armonk, NY, United States) for Windows (Microsoft Corp., Redmond, WA, United States). Continuous variables are expressed as the mean ± SD and were compared between groups using independent t-tests to assess statistically significant differences in the means. Categorical variables are expressed as counts and percentages [n (%)] and were compared using the χ2-test for group comparisons. Differences with P < 0.05 were considered to be statistically significant.
The baseline characteristics of the patients in the study group [67 male, 33 female; median age 59 years (interquartile range 53-67 years); disease duration, 0.3-7.1 years; mean disease duration, 2.45 ± 0.64 years; and mean polyp diameter, 1.36 ± 1.02 cm] were comparable with those in the control group [63 male, 37 female; median age 58 years (interquartile range 52-68 years); disease duration, 0.4-7.5 years; mean disease duration, 2.51 ± 0.70 years; and mean polyp diameter, 1.31 ± 0.97 cm] (P > 0.05, Table 1).
| Index | Study group (n = 100) | Control group (n = 100) | P value |
| Age, years, median (25th-75th IQR) | 59 (53-67) | 58 (52-68) | 0.432 |
| Sex | 0.553 | ||
| Male | 67 (67) | 63 (63) | |
| Female | 33 (33) | 37 (37) | |
| BMI, kg/m2 | 24.23 ± 3.05 | 24.26 ± 3.24 | 0.512 |
| Duration of disease, years | 0.3-7.1 | 0.4-7.5 | 0.264 |
| Mean duration of disease, years | 2.45 ± 0.64 | 2.51 ± 0.70 | 0.537 |
| Polyp diameter, cm | 0.163 | ||
| < 1 | 57 (57) | 53 (53) | |
| ≥ 1 | 43 (43) | 47 (47) | |
| Mean diameter, cm | 1.36 ± 1.02 | 1.31 ± 0.97 | 0.402 |
| Pathological types | 0.912 | ||
| Hyperplastic | 23 | 22 | |
| Inflammatory | 42 | 45 | |
| Adenomatous | 35 | 33 | |
| Comorbidities | 0.984 | ||
| Diabetes | 26 | 28 | |
| Hypertension | 52 | 49 |
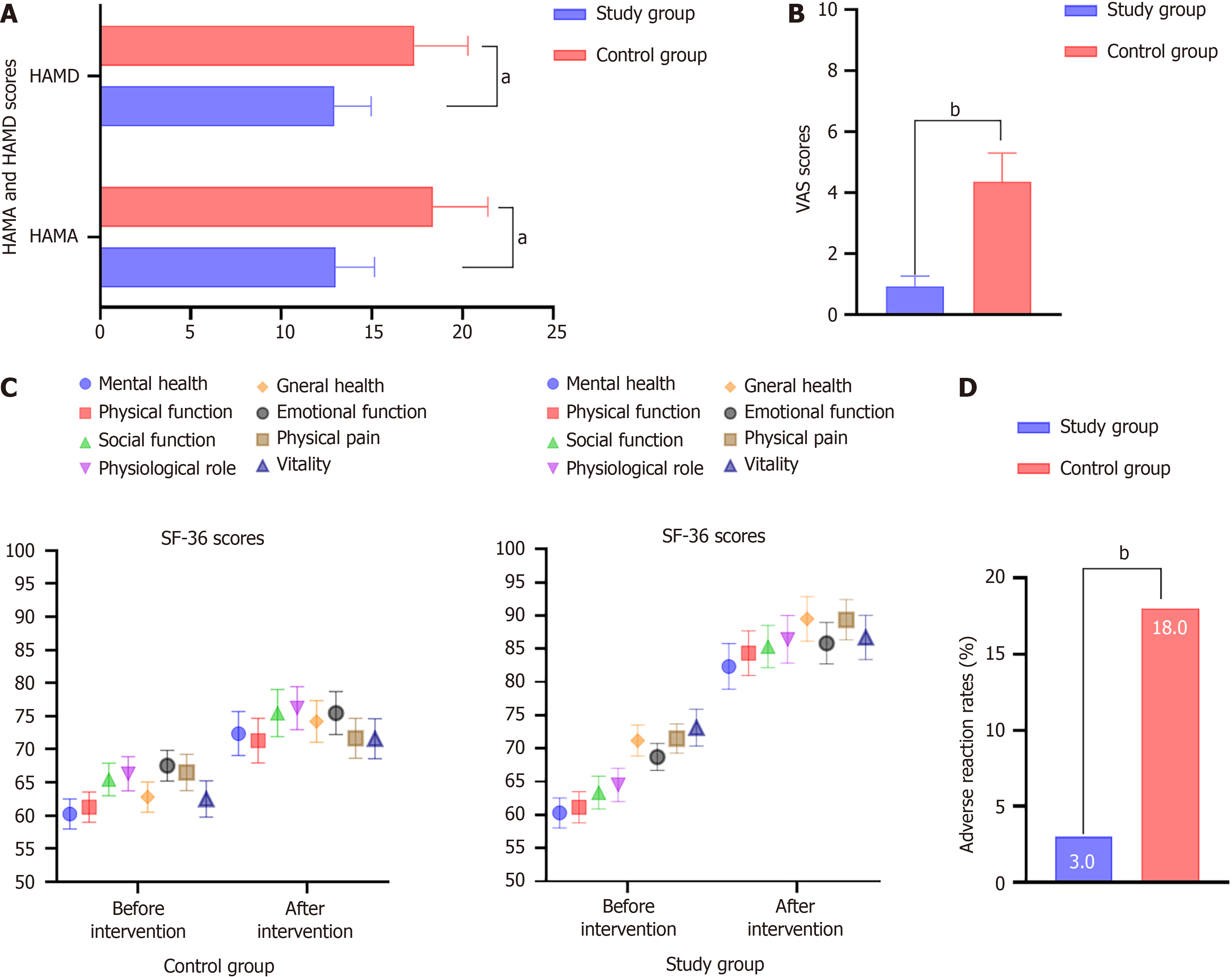
No significant differences were observed in the HAM-A and HAM-D scores between the two groups before nursing (P > 0.05). The scores of the two groups after nursing were significantly lower than those before nursing, and those of the intervention group were significantly lower than those of the control group (13.01 ± 3.02 vs 18.37 ± 3.02; 12.93 ± 2.04 vs 17.35 ± 2.95). The changes in HAM-A and HAM-D were sufficient to indicate that the patients’ anxiety and depression levels decreased after surgery compared to those before surgery. The degree of relief was higher in the experimental group than in the control group (Figure 1A).
Two weeks after nursing, the VAS scores of the study group were significantly lower than those of the control group (0.93 ± 0.34 vs 4.35 ± 0.95, respectively; P < 0.05). The changes in the VAS scores were sufficient to indicate that the patients’ pain levels decreased after surgery compared with those before surgery. The degree of relief was higher in the experimental group than in the control group (Figure 1B).
No significant differences were observed in the SF-36 scores between the two groups before nursing care (P > 0.05). The scores of the study group were significantly higher than those of the control group (P < 0.05). The changes in SF-36 scores were sufficient to indicate that the patients’ quality of life improved after surgery. The degree of increase was greater in the study group than in the control group (Figure 1C).
The incidence of adverse reactions in the study group was 3.0% (3/100), which was significantly lower than that in the control group [18.0% (18/100), P < 0.05]. The adverse reaction rates indicated that the study group was more effective in reducing complications than the control group (Figure 1D).
The satisfaction rate with nursing among patients in the intervention group was 95.0% (95/100), which was higher than that in the control group [72.00% (72/100), P < 0.05]. The satisfaction rate with nursing was sufficient to indicate that patients in the study group were more satisfied than those in the control group.
In recent years, environmental factors, genetics, and their interactions have been established as important factors in the development of colorectal cancer[18]. With continuous improvements in painless endoscopy and minimally invasive techniques, high-frequency endoscopic resection has become the preferred treatment option[19]. Although endoscopic resection is less invasive than abdominal surgery, patients are pressured to follow a strict diet and undergo various nursing interventions during the perioperative period. Conventional nursing measures are relatively simple and there is no unified standard for regulating nursing behavior. It is difficult to meet the nursing needs of patients, and safer and more effective nursing models need to be explored[20]. The application of standardized evidence-based nursing in the care of patients after colon polypectomy can reform nursing practice according to actual patient conditions and establish evidence through systematic reviews to ensure that nursing interventions are consistent with current standards[21]. The results of the present study demonstrate that standardized evidence-based nursing can not only improve the psychological state of patients undergoing endoscopic colon polypectomy but also effectively relieve postoperative pain and demonstrate obvious advantages in preventing postoperative complications, indicating that this nursing mode is better able to meet the needs of this patient population.
The assessment of anxiety and depression levels, as measured using HAM-A and HAM-D, revealed no significant differences between the two groups before the nursing intervention (P > 0.05). However, after the intervention, both groups exhibited a significant reduction in these scores, with the study group exhibiting notably lower values than the control group. These results suggest that standardized, evidence-based nursing not only enhances psychological well-being but also highlights the effectiveness of tailored interventions in alleviating anxiety and depression associated with medical procedures. This reduction in emotional distress can be linked to the consistent implementation of supportive nursing measures, including patient education, communication, and emotional support. Previous studies support these findings, indicating that structured nursing interventions can substantially reduce preoperative anxiety. For example, a meta-analysis by Dong et al[22] concluded that preoperative education and supportive nursing significantly reduced anxiety levels in patients undergoing various surgical procedures. Similarly, Gonella et al[23] found that improved nurse-patient communication and emotional support during the perioperative period effectively reduced anxiety and enhanced coping strategies.
The VAS scores confirmed the effectiveness of the evidence-based nursing model for pain management. The significant difference in pain scores between the study and control groups (0.93 ± 0.34 vs 4.35 ± 0.95, respectively; P < 0.05) underscores the importance of comprehensive nursing protocols. Patients receiving standardized care reported less pain, likely because of the proactive pain management strategies embedded in the protocol. This finding is consistent with those of other studies that have investigated the impact of systematic nursing care on pain management. For example, a randomized controlled trial by Puthoff et al[24] found that patients who underwent a structured pain management program experienced significantly lower postoperative pain levels.
The increase in SF-36 scores in the study group compared to the control group highlights the positive impact of standardized nursing on patient quality of life. The lack of significant differences in SF-36 scores before nursing suggests that quality of life is primarily influenced by nursing interventions rather than by pre-existing conditions. This improvement reflects not only enhanced physical well-being, but also better psychological and emotional health, emphasizing the importance of holistic patient care. The existing literature supports these findings, with a study by Cao et al[25] indicating that structured nursing interventions for patients with postsurgical gastric cancer can improve both psychological symptoms and quality of life.
The incidence of adverse reactions was significantly lower in the intervention group than in the control group (3.0% vs 18.0%, P < 0.05). This reduction was largely attributed to vigilant monitoring and proactive nursing interventions inherent in the evidence-based approach. The model ensured that patients received thorough pre-procedural asse
Patient satisfaction with nursing care was markedly higher in the intervention group than in the control group (95.0% vs 72.0%). High levels of patient satisfaction correlated with better adherence to medical advice, lower anxiety levels, and a more positive perception of healthcare experiences. The structured approach used by nurses, which included clear communication and emotional support, likely fostered a trusting relationship between nurses and patients, thereby enhancing overall satisfaction. The literature emphasizes the relationship between nursing practices and patient satisfaction. Ahmed et al[28] reported that patient satisfaction significantly improved when nursing staff communicated effectively and provided emotional support. Zhang et al[29] indicated that a positive patient-nurse rapport was correlated with increased satisfaction scores, further reinforcing the significance of nurturing relationships in healthcare settings.
The present study has several limitations, the first of which is its single-center retrospective design, which might have affected the reliability of the findings. Therefore, additional multicenter studies are required to validate our results. Second, while this study focused on the impact of refined nursing interventions on complications following endoscopic colon polyp resection, the duration of the nursing interventions was relatively short. Further investigation is required to assess the long-term effects of different nursing models on patient outcomes. Third, various confounding factors, including preexisting conditions, such as hypertension and diabetes, could influence postoperative complications. Although efforts were made to account for these variables in the analysis, it was not feasible to eliminate all potential confounders completely. Future research should include a comprehensive, prospective, multicenter, randomized controlled trial to verify the findings of the present study.
In conclusion, the findings of the present study support the implementation of standardized evidence-based nursing practices for the management of patients undergoing endoscopic colon polypectomies. This approach not only effectively reduced anxiety and pain but also reduced adverse reactions and improved patient satisfaction and quality of life. Future studies should explore the long-term effects of such interventions and integrate them into standard practice across various clinical settings to optimize patient outcomes.
| 1. | Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin. 2024;74:12-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2279] [Cited by in RCA: 6113] [Article Influence: 3056.5] [Reference Citation Analysis (4)] |
| 2. | Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, Jemal A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74:229-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5690] [Cited by in RCA: 12842] [Article Influence: 6421.0] [Reference Citation Analysis (8)] |
| 3. | He S, Xia C, Li H, Cao M, Yang F, Yan X, Zhang S, Teng Y, Li Q, Chen W. Cancer profiles in China and comparisons with the USA: a comprehensive analysis in the incidence, mortality, survival, staging, and attribution to risk factors. Sci China Life Sci. 2024;67:122-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 120] [Article Influence: 60.0] [Reference Citation Analysis (0)] |
| 4. | Braumüller H, Mauerer B, Andris J, Berlin C, Wieder T, Kesselring R. The Cytokine Network in Colorectal Cancer: Implications for New Treatment Strategies. Cells. 2022;12:138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 51] [Reference Citation Analysis (0)] |
| 5. | Sun M, Sun M, Zhang L, Shi S. Colorectal polyp risk is linked to an elevated level of homocysteine. Biosci Rep. 2018;38:BSR20171699. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Suzuki T, Kitagawa Y, Nankinzan R, Yamaguchi T. Usefulness of cold polypectomy under linked color imaging. Endosc Int Open. 2020;8:E87-E91. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Yan Z, Gao F, Xie J, Zhang J. Incidence and risk factors of colorectal delayed post-polypectomy bleeding in patients taking antithrombotics. J Dig Dis. 2021;22:481-487. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Giannino V, Salandin L, Macelloni C, Longo LM. Evaluation of Eleview(®) Bioadhesive Properties and Cushion-Forming Ability. Polymers (Basel). 2020;12:346. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 9. | Fu Y, Zhu LJ, Li DC, Yan JL, Zhang HT, Xuan YH, Meng CL, Sun YH. Evidence-based intervention on postoperative fear, compliance, and self-efficacy in elderly patients with hip fracture. World J Clin Cases. 2022;10:3069-3077. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (1)] |
| 10. | Raaijmakers LG, Kremers SP, Schaper NC, de Weerdt I, Martens MK, Hesselink AE, de Vries NK. The implementation of national action program diabetes in the Netherlands: lessons learned. BMC Health Serv Res. 2015;15:217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Morris ME, McConvey V, Wittwer JE, Slade SC, Blackberry I, Hackney ME, Haines S, Brown L, Collin E. Dancing for Parkinson's Disease Online: Clinical Trial Process Evaluation. Healthcare (Basel). 2023;11:604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 12. | Harrington CC. Evidence-Based Practice Guideline: Assessing Heart Failure in Long-Term Care Facilities. J Gerontol Nurs. 2019;45:18-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Li D, Wang L, Li Z, Li L, Wang Q, Zhang L, Guo Z. Application of CT Scan in Diagnosis of Iliac-Femoral Vein Thrombosis after Hip Replacement. Scanning. 2022;2022:8428963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 14. | Wang H, Wang S. Effect of submucosal injection of normal saline and glycerol fructose on endoscopic polypectomy in patients with colorectal polyps. Oncol Lett. 2019;17:4449-4454. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 15. | Zheng JH, Sun WH, Ma JJ, Wang ZD, Chang QQ, Dong LR, Shi XX, Li MJ, Gu Q, Chen SY, Li DS. Differences in neuroanatomy and functional connectivity between motor subtypes of Parkinson's disease. Front Neurosci. 2022;16:905709. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 16. | Zhou Y, Ma Y, Yu C, Chen Y, Ding J, Yu J, Zhou R, Wang X, Fan T, Shi C. Detection Analysis of Perioperative Plasma and CSF Reveals Risk Biomarkers of Postoperative Delirium of Parkinson's Disease Patients Undergoing Deep Brain Stimulation of the Subthalamic Nuclei. Clin Interv Aging. 2022;17:1739-1749. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 17. | Zhang Z, Cai X, Liang Y, Zhang R, Liu X, Lu L, Huang Y. Electroacupuncture as a rapid-onset and safer complementary therapy for depression: A systematic review and meta-analysis. Front Psychiatry. 2022;13:1012606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 18. | Yang T, Li X, Montazeri Z, Little J, Farrington SM, Ioannidis JPA, Dunlop MG, Campbell H, Timofeeva M, Theodoratou E. Gene-environment interactions and colorectal cancer risk: An umbrella review of systematic reviews and meta-analyses of observational studies. Int J Cancer. 2019;145:2315-2329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 56] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 19. | Yu S, Wang X, Chen X. Removal of giant spherical foreign body in the esophagus by double-forceps endoscope and double balloon. J Int Med Res. 2020;48:300060520941332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 20. | Bhattacharyya R, Chedgy FJ, Kandiah K, Longcroft-Wheaton G, Bhandari P. Knife-assisted snare resection (KAR) of large and refractory colonic polyps at a Western centre: Feasibility, safety and efficacy study to guide future practice. United European Gastroenterol J. 2016;4:466-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Linhart H, Bormann F, Hutter B, Brors B, Lyko F. Genetic and epigenetic profiling of a solitary Peutz-Jeghers colon polyp. Cold Spring Harb Mol Case Stud. 2017;3:a001610. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 22. | Dong Z, Li G, Wang M, Wang T, Jiang C. Effect of systematic nursing intervention on rehabilitation after colorectal polyps of endoscopic removal in children: A protocol for systematic review and meta-analysis. Medicine (Baltimore). 2021;100:e25109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 23. | Gonella S, Delfino C, Rolfo M, Rizzo A, Esposito V, Berchialla P, Campagna S. Effects of a Video-Based Preoperative Educational Intervention Plus Nurse-Led Reinforcement Discussion on Knowledge, Self-Efficacy, and Resilience in Patients Undergoing Major Surgery. Clin Nurs Res. 2021;30:753-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Puthoff TD, Veneziano G, Kulaylat AN, Seabrook RB, Diefenbach KA, Ryshen G, Hastie S, Lane A, Renner L, Bapat R. Development of a Structured Regional Analgesia Program for Postoperative Pain Management. Pediatrics. 2021;147:e20200138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Cao XL, Wang X, Li P, Ju W. Psychological effects of advanced care on patients received endoscopic gastric cancer resection. Medicine (Baltimore). 2019;98:e17497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 26. | Jiao J, Chen Y, Yang L, Li W, Zhou Z, Li L, Xiao Y, Zhao J, Li L, Xia Y. Nursing Practice Based on Evidence-Based Concepts to Prevent Enteral Nutrition Complications for Critically Ill Neurosurgical Patients. Front Surg. 2022;9:857877. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 27. | Dörschner M, Bollmann A, Dinov B, Richter S, Döring M, Arya A, Müssigbrodt A, Kircher S, Dagres N, Sommer P, Hindricks G, Bode K. Structured pain management reduces patient discomfort after catheter ablation and rhythm device surgery. Eur J Pain. 2017;21:1723-1731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Ahmed HM. Role of verbal and non-verbal communication of health care providers in general satisfaction with birth care: a cross-sectional study in government health settings of Erbil City, Iraq. Reprod Health. 2020;17:35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 29. | Zhang X, Pan X, Pan Y, Wang Y. Effects of preventive care on psychological state and complications in leukemia patients receiving chemotherapy. Am J Transl Res. 2023;15:184-192. [PubMed] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/