Published online Jun 27, 2025. doi: 10.4240/wjgs.v17.i6.106531
Revised: March 21, 2025
Accepted: May 8, 2025
Published online: June 27, 2025
Processing time: 91 Days and 15.2 Hours
Both the etiology and treatment of perianal fistulas present challenges, and there is no standard surgical approach.
To present the results of a modified fistulotomy technique that was implemented in a tertiary coloproctology reference center.
Seventy-two patients who underwent surgical intervention for perianal fistula between August 2019 and January 2023 were treated using a modified fistulotomy technique. In this approach, the fistula tract was excised from the external opening up to the external sphincter fibers. The internal orifice was widened, and the septic focus within the inter sphincteric space was curetted. Partial internal sphincterotomy was performed up to the inter sphincteric plane. The anoderm from the internal orifice to the inter sphincteric space was closed with absorbable suture material, and a loose seton was placed at the level of the external sphincter.
The 72 patients who underwent modified fistulotomy were 77.8% male and 22.2% female, with a mean age of 42.2 ± 11.5 years. The median follow-up period was 19 months. Preoperatively, 93.1% of patients had high trans sphincteric fistulas, and 6.9% were females with anterior low trans sphincteric fistulas. In all cases, setons were placed during surgery using vascular tape. A total of 12.5% of patients experienced incontinence, involving gas (6.9%) or soiling (5.6%). There were no reports of solid or liquid incontinences. Complete healing was achieved in 83.3% of the patients, with a recurrence rate of 4.2% and a non-healing rate of 12.5%.
Our preliminary analysis suggests that this modified fistulotomy technique that targets distalization of the internal orifice is a promising alternative management strategy for perianal fistulas.
Core Tip: This study introduces an innovative modification of the fistulotomy technique for perianal fistulas that focuses on distalizing the internal opening away from the high-pressure zone. By excising the fistula tract up to the external sphincter, widening the internal orifice, curetting the inter sphincteric septic focus, performing a partial internal sphincterotomy, and employing absorbable sutures with loose seton placement, this method achieved complete healing in 83.3% of the 72 patients treated with it, while maintaining low recurrence (4.2%) and minimal incontinence (12.5%) rates.
- Citation: Eray İC, Yavuz B, Aydin I, Gumus S, Topal U, Dalci K. Modified fistulotomy with internal orifice distalization for optimized perianal fistula management: Pressure zone transition. World J Gastrointest Surg 2025; 17(6): 106531
- URL: https://www.wjgnet.com/1948-9366/full/v17/i6/106531.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i6.106531
Perianal fistula is defined as an abnormal connection between the anal canal and perianal skin. While 90% of anal fistulas are idiopathic[1], they can cause pain, abscess, hemorrhage, and purulent discharge. Anal fistulas are classified according to their location, as follows: Inter sphincteric, trans sphincteric, supra sphincteric, or extra sphincteric[2].
Perianal fistulas are commonly categorized as ‘simple’ or ‘complex’ based on their anatomical course relative to the external anal sphincter[3]. Simple fistulas cross less than 30% of the external anal sphincter and have a low rate of recurrence after sphincterotomy. Although fistulotomy is the standard surgical treatment for simple fistulas, there remains a risk of postoperative complications[4]. Complex fistulas require more difficult surgeries and may require multiple surgeries to preserve bowel continence. The most commonly used methods for complex trans sphincteric fistulas are inter sphincteric fistula tract ligation and endorectal advancement flap methods; however, their failure rates are high, at 10%-40%[4-6].
Perianal fistula management strategies should be personalized on an individual patient basis. Because fistulotomies are associated with higher incontinence rates in complex fistula treatment, various methods to preserve the sphincter have been developed. Loose setons, collagen plugs, advancement flaps, inter sphincteric fistula tract ligation, laser closure, and stem cell therapies are currently used to treat perianal fistulas. The main disadvantage of sphincter-preserving surgery is the low success rate[5].
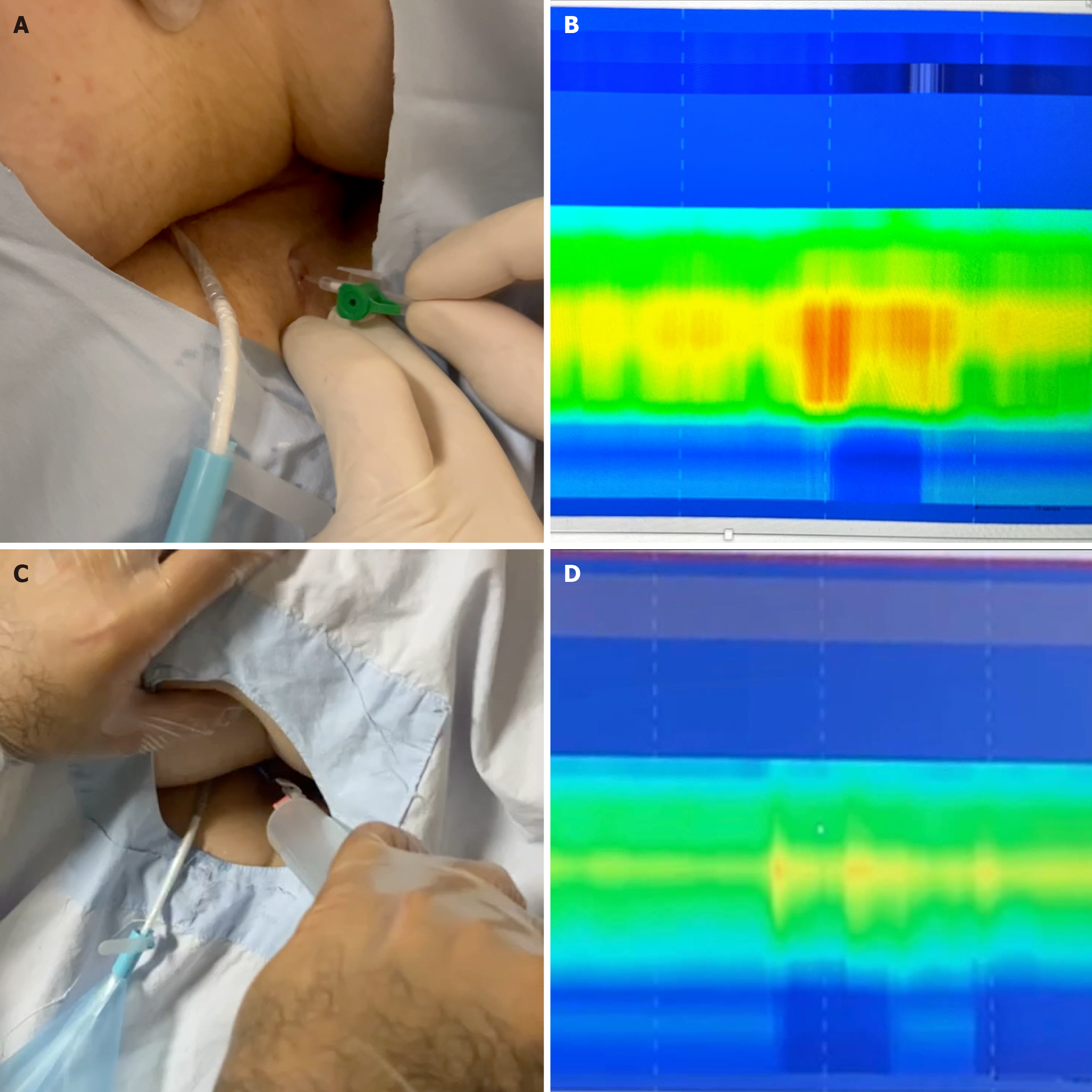
In cryptoglandular perianal fistulas, the internal opening is typically located at the dentate line within the high-pressure zone of the anal canal. Although existing literature does not explicitly address the adverse effects of retaining the internal opening within the high-pressure zone following fistula surgery, we hypothesized that relocating the opening to the low-pressure zone may enhance the healing process (Figure 1).
In this article, we present our novel surgical technique and its outcomes. This modified approach preserves the sphincter while aiming to reduce the recurrence rate typically associated with definitive surgery. The primary objective of our technique was to reposition the internal fistula opening as far as possible from the high-pressure zone of the anal canal and to shift the external opening closer to the external anal sphincter, thereby creating the shortest possible fistula tract.
This study was conducted with the approval of the Çukurova University Faculty of Medicine Ethics Committee, under decision number 138, dated March 11, 2023. In this study, the data of 72 patients who underwent surgical intervention for perianal fistula between August 2019 and January 2023 were analyzed. Data that were pertinent to the surgical intervention and the present conditions of the patients were analyzed. Parameters such as the patients’ age, sex, date of surgery, fistula classification, preoperative seton status, seton type, concomitant procedures, postoperative clinical status, incidents of incontinence, and the duration of post-surgical follow-up were evaluated comprehensively. Furthermore, the surgery outcomes and associated complications were examined thoroughly.
Female patients over 18 years of age with anterior low trans sphincteric fistulas, patients with low trans sphincteric fistulas unsuitable for fistulotomy, or patients with high fistulas [diagnosed through magnetic resonance imaging (MRI) or endoanal ultrasonography (EAUS)] were included in the study. Patients were excluded if they had tumors, tuber
Statistical analyses were conducted using the IBM SPSS Statistics version 22 software (Armonk, NY, United States). Descriptive statistics were expressed as mean ± SD for continuous variables and as frequencies (percentages) for categorical variables. The Shapiro-Wilk test was utilized to verify the normal distribution of continuous variables.
All patients were evaluated preoperatively by the same experienced surgeon in an outpatient clinic using EAUS and/or MRI, as well as rectoscopy and/or colonoscopy. Fistulas were classified into the following four types, according to Park’s classification: inter sphincteric, trans sphincteric, supra sphincteric, or extra sphincteric. Only patients who met the inclusion criteria underwent surgery.
All patients received a preoperative enema. Surgeries were performed under either spinal or general anesthesia, with patients positioned in the lithotomy or prone position based on the fistula’s location. Internal fistula orifices were identified during the examination with the aid of an anoscope.
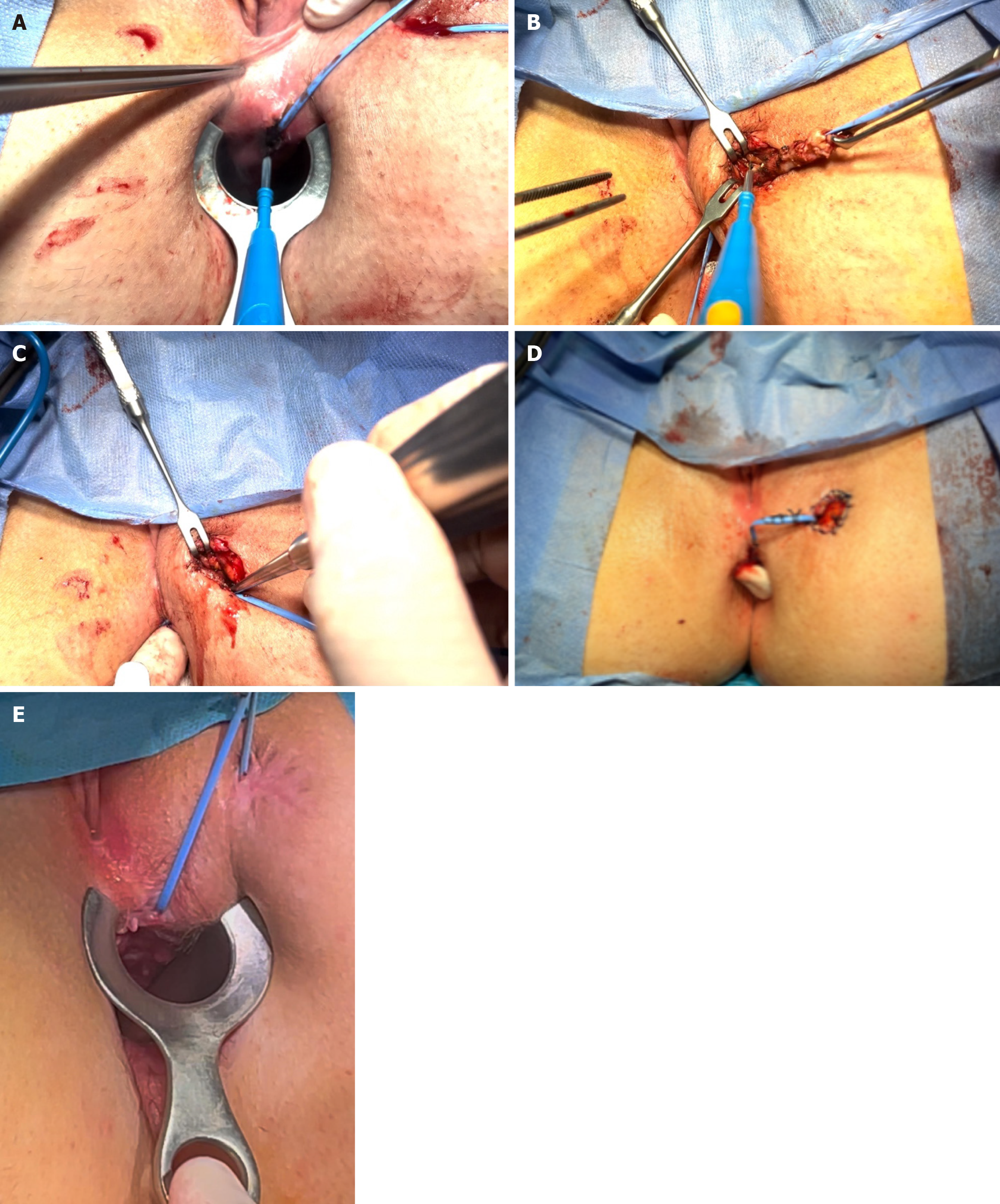
The goal of the surgical modification was to distalize the internal opening. To accomplish this, the fistula tract was first excised from the external opening up to the level of the external sphincter fibers. The internal orifice was then widened, and the septic focus within the inter sphincteric space was thoroughly curetted (Figure 2A and B). A partial internal sphincterotomy was performed up to the inter sphincteric plane (Figure 2C).
During the internal orifice distalization, the anal canal was closed using absorbable polyglactin 3-0 sutures, starting distally and progressing proximally toward the anoderm for a smooth closure (Figure 2D). Based on the clinical assessment, a loose seton made of vascular tape was placed in the remaining part of the fistula tract when needed.
Following application of the final modified technique, setons were removed in the outpatient setting between the 6th and 12th postoperative weeks. The timing of removal was based on clinical evaluation of wound healing after distalization (Figure 2E).
Following surgical treatment, the fistula tract was considered healed if it had fully closed. If the tract initially closed but a new tract formed within 3 months, it was classified as a relapse. If the original tract failed to close, it was categorized as unhealed.
We performed the modified fistulotomy technique on 72 patients. Of these, 77.8% were male and 22.2% were female. The average age was 42.2 ± 11.5 years. The median follow-up period was 19 months (IQR: 14-25.5 months).
Preoperatively, 93.1% of patients presented with high trans sphincteric fistulas. Among female patients, 6.9% had anterior fistulas. Preoperative seton placement was performed in 55.6% of cases.
We placed vascular tape setons in all cases. Details of previous surgeries are presented in Table 1. Spontaneous seton dislodgement occurred in 4.2% of patients, and 1 patient developed a perianal abscess during follow-up.
| Operation | n | % |
| Seton placement | 40 | 55.6 |
| Advancement flaps | 3 | 4.2 |
| Fournier’s gangrene | 2 | 2.8 |
| LIFT | 3 | 4.2 |
| Fistulotomy | 4 | 5.6 |
| Curettage of the fistula tract | 1 | 1.4 |
A total of 12.5% of patients reported incontinence, involving gas in 6.9% and soiling in 5.6%. There were no reports of solid or liquid incontinences.
A total of 83.3% of patients achieved complete healing, while 4.2% experienced recurrence and 12.5% had non-healing fistulas. The relationship between fistula type and current clinical status is presented in Table 2.
Our preliminary analysis suggests that the modified fistulotomy technique, which incorporates an innovative approach to distalizing the internal orifice, shows promise as an alternative treatment strategy for perianal fistulas.
The goal of perianal fistula treatment is to promote healing without compromising continence. While fistulotomy offers high success rates, it is not applicable to all fistula types. In patients at risk of incontinence or those with a large portion of the external sphincter involved, sphincter-preserving surgeries are preferred. However, these procedures are more complex than fistulotomy and tend to have lower and more variable success rates. As a result, ongoing research aims to develop simpler techniques that preserve the continence mechanism for cases that are unsuitable for fistulotomy.
Traditionally, loose setons are used in cases of complex fistulas with extensive sphincter involvement or when significant inflammation complicates the evaluation of sphincter involvement. The primary goal is to eradicate the septic focus and allow the fistula tract to mature, making it safer to perform complex sphincter-preserving procedures. However, recent studies have suggested that loose setons may also serve as a definitive treatment option. Although the exact mechanism remains unclear, it is thought that the distalization of the internal opening beyond the high-pressure zone contributes to healing[7]. When loose setons are used for definitive treatment, the fistula tract is excised from the external opening to the external sphincter, and the remaining tract is curetted. This process promotes migration of cells to the area, and subsequent wound contraction may facilitate distalization of the seton and the internal opening[8].
In a study of 38 patients with trans sphincteric and supra sphincteric fistulas, a silicone seton was applied loosely, and the migration of the fistula tract was monitored using MRI. Only 1 patient (3%) presented with a mid-level trans sphincteric fistula that transformed into a low trans sphincteric fistula. As a result, the authors of that study did not recommend this method as a primary treatment option[9]. One possible explanation for the lack of distalization in this study is that fistula tract excision, which typically promotes wound contraction, was not performed. This contrasts with other studies where better results were obtained with excision up to the external sphincter, followed by curettage and loose seton placement[10]. Nevertheless, loose setons continue to be used long-term in patients at a high risk of incontinence or those who refuse surgical intervention.
Endoanal advancement flap surgery is frequently performed for cryptoglandular complex fistulas and has been described by some authors as the ‘current gold standard’ technique[11]. Several studies have reported reduced resting anal pressures following this procedure. This decrease is thought to result from the inclusion of the internal sphincter muscle layer within the flap. Additionally, closure of the internal opening and positioning the lower margin of the flap within a lower-pressure zone may further contribute to improved healing outcomes[12].
Similarly, successful outcomes have been reported with a modified ligation of inter sphincteric fistula tract (commonly known as ‘LIFT’) procedure, in which a fistulotomy is performed on the internal sphincter to relocate the primary source of the fistula outside the high-pressure zone[13]. An important consideration in fistula treatment is the potential damage to the continence mechanism. During fistulotomy, the internal sphincter is often incised up to the dentate line, a practice generally well tolerated by patients. This observation suggests that focusing on procedures that preserve only the external sphincter, rather than full sphincter-preserving procedures, may be a viable approach[14].
In our study, we excised the external fistula tract up to the level of the external sphincter, along with the partial excision of the internal sphincter and anoderm extending up to the inter sphincteric groove. The goal was to relocate the internal fistula opening outside the high-pressure zone and to stimulate wound healing by creating a controlled surgical wound, thereby attracting the cellular components necessary for tissue repair and improved healing.
By distalizing the internal orifice, this modified approach has the potential to minimize the risk of sphincter damage, thereby enhancing the preservation of fecal continence. We believe that if these preliminary findings are validated in larger prospective studies, the modified fistulotomy technique could represent a significant advancement in the management of perianal fistulas, offering meaningful benefits for both patients and their treating clinicians.
| 1. | Iglay K, Bennett D, Kappelman MD, Zhang X, Aldridge M, Karki C, Cook SF. A Systematic Review of Epidemiology and Outcomes Associated with Local Surgical and Intersphincteric Ligation Procedures for Complex Cryptoglandular Fistulas. Adv Ther. 2023;40:1926-1956. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Parks AG. Pathogenesis and treatment of fistuila-in-ano. Br Med J. 1961;1:463-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 405] [Cited by in RCA: 330] [Article Influence: 11.8] [Reference Citation Analysis (1)] |
| 3. | Bhat S, Xu W, Varghese C, Dubey N, Wells CI, Harmston C, O'Grady G, Bissett IP, Lin AY. Efficacy of different surgical treatments for management of anal fistula: a network meta-analysis. Tech Coloproctol. 2023;27:827-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 4. | Włodarczyk M, Włodarczyk J, Sobolewska-Włodarczyk A, Trzciński R, Dziki Ł, Fichna J. Current concepts in the pathogenesis of cryptoglandular perianal fistula. J Int Med Res. 2021;49:300060520986669. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 5. | Charalampopoulos A, Papakonstantinou D, Bagias G, Nastos K, Perdikaris M, Papagrigoriadis S. Surgery of Simple and Complex Anal Fistulae in Adults: A Review of the Literature for Optimal Surgical Outcomes. Cureus. 2023;15:e35888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Balciscueta Z, Uribe N, Balciscueta I, Andreu-Ballester JC, García-Granero E. Rectal advancement flap for the treatment of complex cryptoglandular anal fistulas: a systematic review and meta-analysis. Int J Colorectal Dis. 2017;32:599-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 60] [Article Influence: 6.7] [Reference Citation Analysis (1)] |
| 7. | Johnson EK, Bernier G. Cryptoglandular Abscess and Fistula. In: Steele SR, Hull TL, Hyman N, Maykel JA, Read TE, Whitlow CB, editors. The ASCRS Textbook of Colon and Rectal Surgery. Switzerland: Springer Cham, 2022: 249-269. [DOI] [Full Text] |
| 8. | Daodu OO, O'Keefe J, Heine JA. Draining Setons as Definitive Management of Fistula-in-Ano. Dis Colon Rectum. 2018;61:499-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Verkade C, van Tilborg GFAJB, Stijns J, Wasowicz DK, Zimmerman DDE. Distalization of perianal fistulas after loose silicone seton drainage is a myth. Tech Coloproctol. 2023;28:16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Lentner A, Wienert V. Long-term, indwelling setons for low transsphincteric and intersphincteric anal fistulas. Experience with 108 cases. Dis Colon Rectum. 1996;39:1097-1101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Zimmerman DDE, Stijns J, Wasowicz DK, Gottgens KWA. Transanal Advancement Flap Repair: The Current Gold Standard for Cryptoglandular Transsphincteric Perianal Fistulas. Turk J Colorectal Dis. 2019;29:104-110. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Uribe N, Millán M, Minguez M, Ballester C, Asencio F, Sanchiz V, Esclapez P, del Castillo JR. Clinical and manometric results of endorectal advancement flaps for complex anal fistula. Int J Colorectal Dis. 2007;22:259-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 62] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Bastawrous A, Hawkins M, Kratz R, Menon R, Pollock D, Charbel J, Long K. Results from a novel modification to the ligation intersphincteric fistula tract. Am J Surg. 2015;209:793-8; discussion 798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Omar W, Alqasaby A, Abdelnaby M, Youssef M, Shalaby M, Anwar Abdel-Razik M, Emile SH. Drainage Seton Versus External Anal Sphincter-Sparing Seton After Rerouting of the Fistula Tract in the Treatment of Complex Anal Fistula: A Randomized Controlled Trial. Dis Colon Rectum. 2019;62:980-987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/