Published online May 27, 2025. doi: 10.4240/wjgs.v17.i5.105894
Revised: March 15, 2025
Accepted: April 3, 2025
Published online: May 27, 2025
Processing time: 103 Days and 1.9 Hours
The management of pediatric choledocholithiasis is complicated by anatomical constraints and the subsequent risks of conventional therapies requiring external drainage. This case report introduces a novel laparoscopic microincision tech
A 12-year-old girl with a 5-year history of recurrent upper abdominal pain was diagnosed with choledocholithiasis, cholelithiasis, and biliary pancreatitis based on imaging and laboratory tests. After failed conservative management, laparoscopic cholecystectomy with a microincision at the cystic duct confluence enabled choledochoscopic extraction of seven stones without T-tube placement. Primary closure using absorbable sutures with cystic duct confluence preserved biliary integrity. Postoperatively, liver function and amylase levels normalized by day 3, and abdominal ultrasonography confirmed no complications. The patient promptly resumed normal activity with no recurrence observed at the 16-month follow-up visit. This approach avoids external drainage, minimizes ductal manipulation, and optimizes recovery, which are key advantages for pediatric patients.
Microincision at the cystic duct confluence safely eliminates T-tubes, ensures stone clearance, and accelerates pediatric recovery.
Core Tip: We present a novel microincision technique at the cystic duct confluence during laparoscopic common bile duct exploration for pediatric choledocholithiasis. By avoiding T-tube placement, critical for active children requiring unrestricted movement and timely return to school, this approach minimizes ductal trauma, preserves biliary integrity, and accelerates recovery. A 12-year-old patient achieved rapid normalization of liver function and symptom resolution with no recurrence at the 16-month follow-up visit. This innovation addresses pediatric-specific anatomical and lifestyle challenges, offering a safer, minimally invasive alternative to conventional methods. This technique underscores the need for surgical strategies tailored to the unique needs of children.
- Citation: Chen GB, Sha YG, Wang ZL, Wang DB, Tang RM, Chen YS. Laparoscopic micro-incision technique at cystic duct confluence for pediatric choledocholithiasis management: A case report. World J Gastrointest Surg 2025; 17(5): 105894
- URL: https://www.wjgnet.com/1948-9366/full/v17/i5/105894.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i5.105894
Pediatric choledocholithiasis, characterized by stones within the common bile duct (CBD), is a rare condition (prevalence: 0.15%-0.22%) with distinct challenges in children[1]. Anatomical constraints such as narrow ductal lumens, fragile bile duct walls, and developmental vulnerability require minimally invasive strategies that balance efficacy with the preservation of biliary integrity[2,3]. Furthermore, pediatric patients require a rapid postoperative recovery to resume school and physical activity, emphasizing the need for interventions that avoid external devices and prolong hospitalization. Current treatments for pediatric choledocholithiasis, including endoscopic retrograde cholangiopancreatography (ERCP), laparoscopic CBD exploration (LCBDE), and laparoscopic transcystic CBD exploration (LTCBDE)[4-6], are extrapolated from adult protocols but carry certain limitations in children[7]. These shortcomings highlight the unmet need for pediatric-specific techniques that eliminate external drainage, minimize ductal trauma, and align with developmental requirements. Herein, we present a novel laparoscopic microincision technique at the cystic duct confluence during LCBDE designed to address these challenges. By using the natural dilation of the cystic duct junction, this approach enables direct choledochoscopic stone extraction without a CBD incision or T-tube placement. We report its successful application in a 12-year-old patient with choledocholithiasis and demonstrate its feasibility and potential to advance pediatric biliary surgery.
A 12-year-old girl presented with recurrent upper abdominal pain that had persisted for > 5 years.
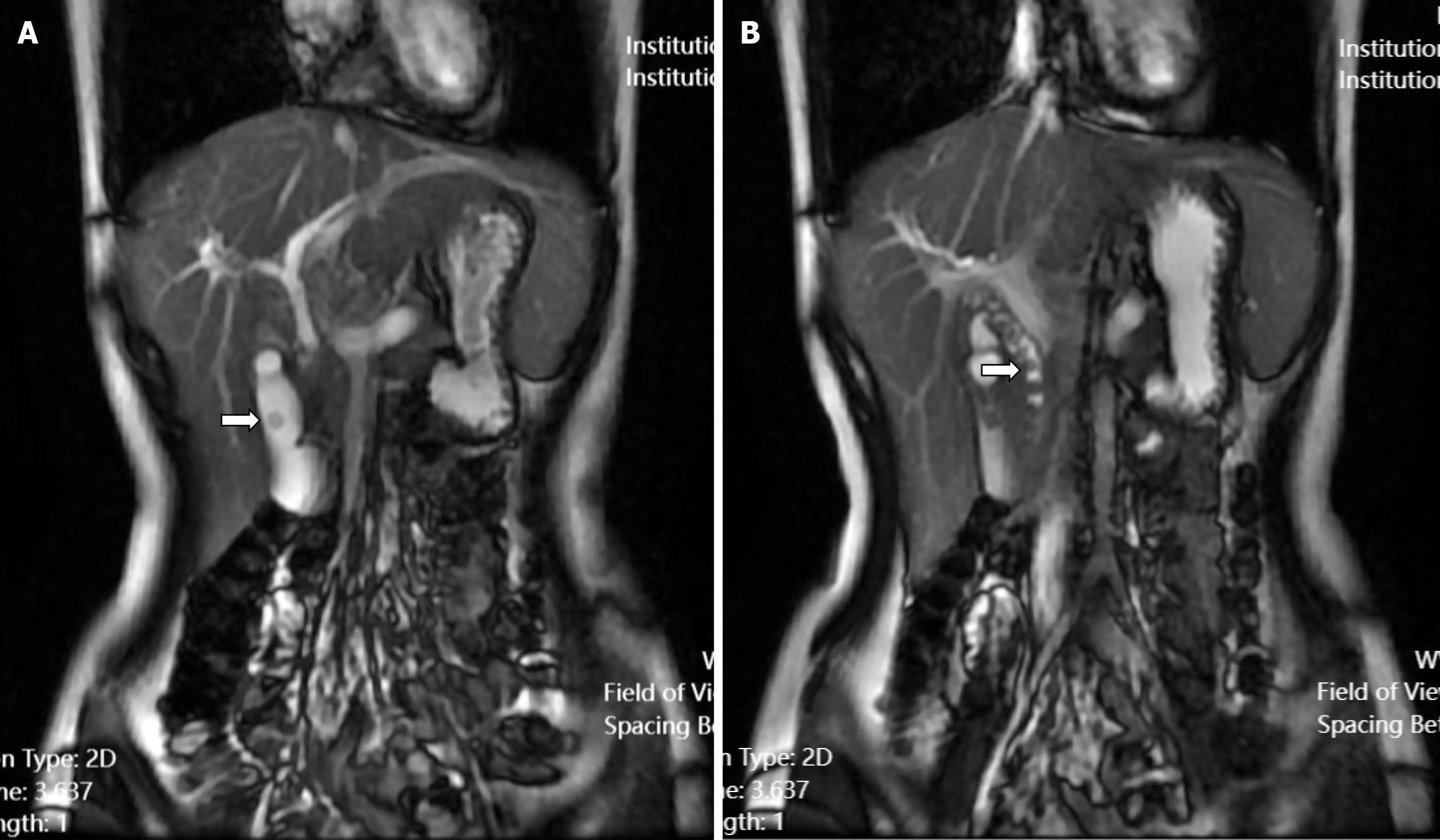
The patient experienced recurrence of upper abdominal pain and discomfort 2 weeks prior to admission, with symptoms worsening 3 days before presentation. On August 12, 2023, she was admitted to the Guangji Hospital. Abdominal ultrasonography revealed choledochal stones, dilated intra- and extrahepatic bile ducts, gallbladder stones, and cholecystitis. Subsequent magnetic resonance cholangiopancreatography confirmed the presence of a gallbladder stone and multiple CBD stones (Figure 1). The patient received symptomatic treatment including anti-infective therapy and rehydration, which resulted in symptom improvement.
Five years prior, the patient had experienced recurrent pain and discomfort in the right upper abdomen without obvious triggers. The symptoms resolved with rest and no specific treatment was required.
The patient had no history of abdominal surgery or any other surgical contraindications. No history of residence in epidemic areas or contact with infected water sources or epidemic sources were noted.
Upon admission, vital signs showed a temperature of 36.5 °C, pulse of 70 beats/minutes, respiratory rate of 18 breaths/minutes blood pressure of 11.5/8.5 kPa, and body weight of 35 kg. Physical examination showed mild icteric discoloration of the skin and sclera. Palpation of the upper abdomen revealed deep tenderness without rebound tenderness or muscle guarding. No significant pain was detected in the hepatorenal region.
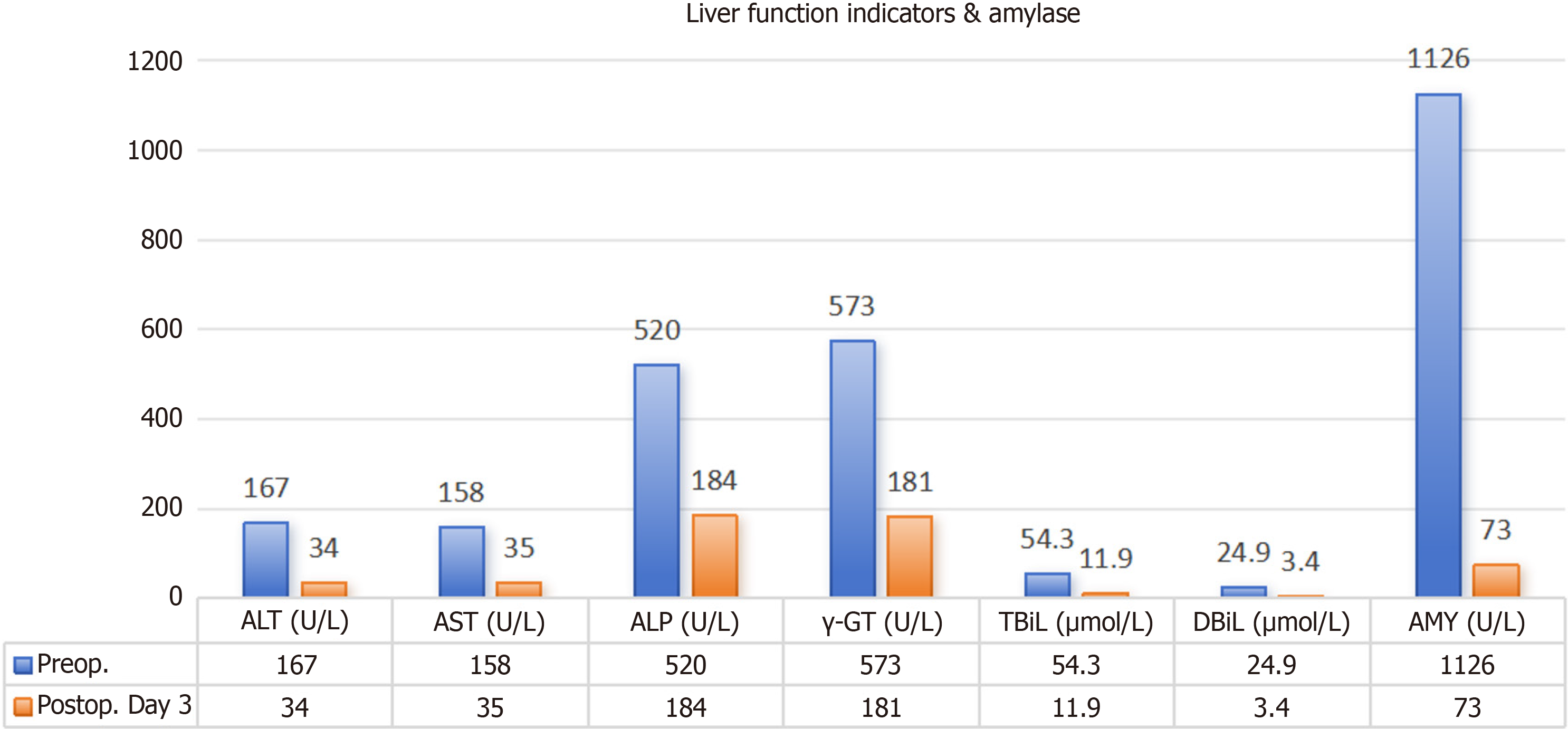
Initial laboratory tests revealed significantly elevated liver function and serum amylase levels (Figure 2, Table 1). White blood cell count, neutrophil percentage, and C-reactive protein levels were within normal ranges (Table 1).
| Parameter | Result | Reference range |
| White blood cells | 6.29 × 109/L | 4.0-11.0 × 109/L |
| Neutrophil percentage | 62.80% | 40%-70% |
| Red blood cells | 4.30 × 1012/L | 3.5-5.0 × 1012/L |
| Hemoglobin | 121 g/L | 110-150 g/L |
| Alanine aminotransferase | 167 U/L | 7-56 U/L |
| Aspartate aminotransferase | 158 U/L | 10-40 U/L |
| Gamma-glutamyl transferase | 573 U/L | 9-48 U/L |
| Alkaline phosphatase | 520 U/L | 44-147 U/L |
| Total bilirubin | 54.3 μmol/L | 5.1-17.1 μmol/L |
| Direct bilirubin | 29.4 μmol/L | 0-6.8 μmol/L |
| Indirect bilirubin | 24.9 μmol/L | 3.4-13.7 μmol/L |
| Amylase | 1126 U/L | 30-110 U/L |
| C-reactive protein | 1.98 mg/L | 0-8 mg/L |
Plain and enhanced upper abdominal computed tomography performed on August 17, 2023, demonstrated an enlarged gallbladder, a dilated CBD with a maximum diameter of approximately 1.3 cm, and a slightly dilated main pancreatic duct (Figure 3).
Based on the medical history, laboratory examination results, and imaging findings of the patient, the final diagnoses were CBD stones with cholangitis, gallbladder stones with cholecystitis, and biliary pancreatitis.
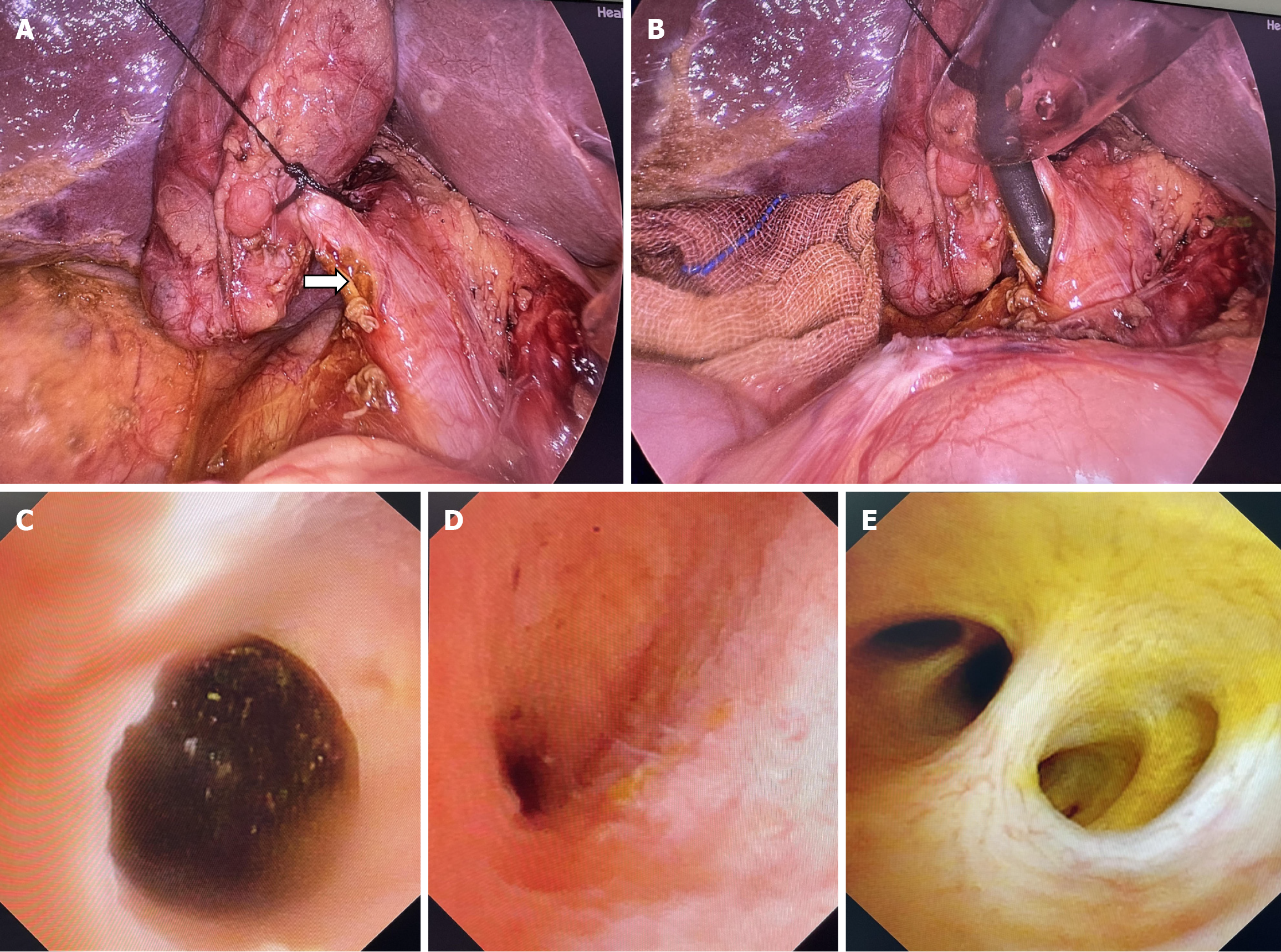
Following surgical and clinical research protocols and after obtaining informed consent, the modified laparoscopic surgical technique was performed on August 22, 2023. Under general anesthesia, a standard laparoscopic approach was initiated with four ports. The procedure involved dissection of the gallbladder adhesions and exposure of Calot’s triangle, followed by standard anatomical dissection with isolation of the cystic duct approximately 2 cm from the junction. The cystic arteries were ligated and divided. After complete exposure of the common hepatic duct, cystic duct, and CBD, the distal cystic duct was pre-ligated using a 4-0 silk suture. An incision was made in the cystic duct and its confluence with the CBD, which was approximately 1.5 cm (Figure 4A). Choledochoscopy revealed seven stones of varying sizes in the middle and lower CBD (Figure 4B and C), which were extracted using a basket. The biliary system was comprehensively examined, including visualization of the ampulla of Vater (Figure 4D) and the second- to third-order intrahepatic bile ducts (Figure 4E). The cystic duct confluence and proximal cystic duct were closed using 4-0 absorbable sutures and clamped with Hem-o-lok, and the cystic duct approximately 0.2 cm from the CBD. The procedure included cho
The postoperative recovery of the patient was uneventful. Liver function test results and serum amylase levels significantly improved on postoperative day 3 (Figure 2). Abdominal ultrasonography performed 1 week after surgery showed no significant free fluid. The drainage tube was removed (Figure 5), and the patient was discharged. No imaging abnormalities were detected during follow-up ultrasound examinations at 7 and 16 months postoperatively. The child had normal dietary habits, sleep patterns, and overall health status.
Choledocholithiasis, although well-established in adult surgical practice, presents unique complexities in pediatric populations owing to anatomical and developmental constraints. The rarity of this condition in children underscores the need for surgical innovation that addresses pediatric-specific challenges, including narrower ductal lumens, thinner bile duct walls, and the imperative for rapid recovery to accommodate school and physical activity. Our novel laparoscopic microincision technique at the cystic duct confluence during LCBDE offers a tailored solution, as evidenced by the successful management of a 12-year-old patient with choledocholithiasis.
Pediatric biliary anatomy requires meticulous precision[8]. The cystic duct confluence, often anatomically dilated compared with the adjacent CBD, serves as an optimal access point for choledochoscopy while minimizing direct trauma to the CBD. In this case, a 1.5 cm micro-incision at this junction allowed complete extraction of seven stones and thorough visualization of the biliary tree, including the ampulla of Vater and intrahepatic ducts. By avoiding direct CBD incision and suturing, this approach mitigates the risks of postoperative strictures, which are critical in growing children, and preserves the native ductal architecture.
Current therapeutic modalities for pediatric choledocholithiasis (ERCP), LCBDE with T-tube placement, LCBDE with primary CBD closure, and LTCBDE are adaptations of adult protocols, each with distinct limitations in children.
ERCP: Although minimally invasive and effective for stone extraction[5,9], ERCP in pediatric patients carries a 4% risk of pancreatitis[9] and technical challenges due to smaller anatomical dimensions[10,11]. Radiation exposure, duodenal papilla manipulation, and the need for specialized endoscopic expertise further limit its utility[9,11], particularly in younger children.
LCBDE: Conventional LCBDE often require T-tube drainage to prevent postoperative bile leakage. However, external drainage prolongs hospitalization, restricts mobility, and increases the difficulty of T-tube-related care[12]. For active children, T-tube management disrupts school attendance and physical activity, significantly affecting their quality of life.
LCBDE with primary CBD closure: Although T-tube avoidance is a theoretical advantage, primary CBD closure in children remains technically demanding. Pediatric bile duct walls are fragile, potentially leading to bile leakage even with meticulous suturing. Furthermore, direct CBD incision and suturing may interfere with longitudinal ductal growth, raising concerns regarding long-term stenosis or developmental anomalies.
LTCBDE: Transcystic exploration minimizes ductal trauma but is limited by anatomical constraints such as a narrow cystic duct diameter (< 3 mm) or unfavorable insertion angles[13,14]. Large stone burdens (> 8 mm) or impacted stones frequently require conversion to LCBDE or a complementary surgical intervention[15-17]. Our microincision technique bridges these gaps by combining direct choledochoscopic access via the cystic duct confluence with primary closure using absorbable sutures, thereby eliminating external drainage, avoiding CBD manipulation, and accelerating return to daily activities.
This approach introduces several pivotal refinements: (1) T-Tube avoidance: By circumventing external drainage, postoperative care is simplified, enabling unrestricted mobility and rapid reintegration into school life; (2) Anatomically targeted Access: Leveraging the natural dilation of the cystic duct confluence optimizes stone retrieval while minimizing iatrogenic injury to the CBD; (3) Comprehensive visualization: Direct choledochoscopic examination of the entire biliary system, including the second- and third-order intrahepatic ducts, ensures complete stone clearance, which is a critical factor for preventing recurrence; and (4) Developmental preservation: Avoiding CBD incision mitigates long-term risks of stenosis or growth-related complications, a paramount consideration in pediatric surgery.
The rapid biochemical normalization of the patient (liver enzymes and amylase by postoperative day 3) and the absence of complications (e.g., bile leakage and infection) underscore the safety of the technique. Sixteen months of follow-up imaging confirmed the absence of recurrence and further validated its efficacy. However, success of this approach depends on advanced laparoscopic and choledochoscopic proficiency, particularly in microincision creation, intracorporeal suturing, and choledochoscopic stone extraction. Additionally, while this single-case outcome is promising, multicenter studies with larger cohorts are warranted to evaluate the long-term ductal patency and recurrence rates.
The cystic duct confluence microincision technique is a promising alternative for the management of pediatric choledocholithiasis. By harmonizing anatomical precision, minimally invasive principles, and quality-of-life priorities, this study addresses the unique challenges of pediatric biliary surgery while offering a scalable model for future innovation.
| 1. | Al-Salem AH. Cholelithiasis and Choledocholithiasis. In: An Illustrated Guide to Pediatric Surgery. Cham: Springer, 2014: 277-281. [DOI] [Full Text] |
| 2. | Kasai Y, Aoki R, Nagano N, Kaneda H, Koshinaga T, Morioka I. Usefulness of Thin-Slice Contrast-Enhanced Computed Tomography in Detecting Perforation Site in Congenital Biliary Dilatation: A Case Report. J Nippon Med Sch. 2023;89:623-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Herrera-LeBlanc ID, Domínguez-Hernández MF, Palacios-Saucedo GC, Herrera-Rivera CG. Common bile duct diameter by age groups in adult patients without bile duct pathology. Cir Cir. 2022;90:503-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Reference Citation Analysis (0)] |
| 4. | Bosley ME, Zamora IJ, Neff LP. Choledocholithiasis-a new clinical pathway. Transl Gastroenterol Hepatol. 2021;6:35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 5. | Keil R, Drábek J, Lochmannová J, Šťovíček J, Koptová P, Wasserbauer M, Frýbová B, Šnajdauf J, Matouš J, Kotalová R, Rygl M, Hlava Š. ERCP in infants, children, and adolescents-Different roles of the methods in different age groups. PLoS One. 2019;14:e0210805. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 6. | Pogorelić Z, Lovrić M, Jukić M, Perko Z. The Laparoscopic Cholecystectomy and Common Bile Duct Exploration: A Single-Step Treatment of Pediatric Cholelithiasis and Choledocholithiasis. Children (Basel). 2022;9:1583. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 7. | Sha Y, Wang Z, Tang R, Wang K, Xu C, Chen G. Modern Management of Common Bile Duct Stones: Breakthroughs, Challenges, and Future Perspectives. Cureus. 2024;16:e75246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 8. | Simmons CL, Harper LK, Patel MC, Katabathina VS, Southard RN, Goncalves L, Tran E, Biyyam DR. Biliary Disorders, Anomalies, and Malignancies in Children. Radiographics. 2024;44:e230109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Hosseini A, Sohouli MH, Sharifi E, Sayyari A, Sridharan K, Tajalli S, Imanzadeh N, Fatahi S. Indications, success, and adverse event rates of pediatric endoscopic retrograde cholangiopancreatography (ERCP): a systematic review and meta-analysis. BMC Pediatr. 2023;23:596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 10. | Yıldırım AE, Altun R, Ocal S, Kormaz M, Ozcay F, Selcuk H. The safety and efficacy of ERCP in the pediatric population with standard scopes: Does size really matter? Springerplus. 2016;5:128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Makita S, Amano H, Kawashima H, Hinoki A, Shirota C, Tainaka T, Sumida W, Yokota K, Okamoto M, Takimoto A, Yasui A, Nakagawa Y, Uchida H. Utility of endoscopic retrograde cholangiopancreatography in management of pediatric pancreaticobiliary disease. BMC Pediatr. 2022;22:134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Li L, Zeng Z, Li L, Zhang J. Comparison of the therapeutic effects of three minimally invasive approaches for laparoscopic cholecystectomy combined with common bile duct exploration-- a 5-year retrospective analysis. BMC Surg. 2024;24:199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 13. | Zhu JG, Han W, Guo W, Su W, Bai ZG, Zhang ZT. Learning curve and outcome of laparoscopic transcystic common bile duct exploration for choledocholithiasis. Br J Surg. 2015;102:1691-1697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 14. | Sureka B, Bansal K, Patidar Y, Arora A. Magnetic resonance cholangiographic evaluation of intrahepatic and extrahepatic bile duct variations. Indian J Radiol Imaging. 2016;26:22-32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (2)] |
| 15. | Yoo D. Laparoscopic choledocholithotomy and transductal T-tube insertion with indocyanine green fluorescence imaging and laparoscopic ultrasound: A case report. World J Clin Cases. 2023;11:7193-7199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (1)] |
| 16. | Lei J, Wang J, Li Q, Wu P, Yuan R, Zhu H, Zou S, Shao J, Fang L. Laparoscopic Transcystic Common Bile Duct Exploration: T-Shaped Incision of Cystic Duct with FREDDY Laser Lithotripsy. J Laparoendosc Adv Surg Tech A. 2016;26:646-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Yang XB, Xu AS, Li JG, Xu YP, Xu DS, Fu CC, Deng DB, Li J, Zhang MZ. Dilation of the cystic duct confluence in laparoscopic common bile duct exploration and stone extraction in patients with secondary choledocholithiasis. BMC Surg. 2020;20:50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |