Published online May 27, 2025. doi: 10.4240/wjgs.v17.i5.104893
Revised: March 8, 2025
Accepted: April 7, 2025
Published online: May 27, 2025
Processing time: 128 Days and 17.4 Hours
Transjugular intrahepatic portosystemic shunt (TIPS) is a highly effective treat
We report a 56-year-old male patient who underwent a TIPS procedure for re
Early recognition and prompt intervention are essential in managing stent fractures after TIPS creation to mitigate potential risks and ensure optimal patient outcomes.
Core Tip: Stent fracture is an uncommon yet a potentially serious complication following transjugular intrahepatic portosystemic shunt (TIPS), particularly among the bare metal stent/stent-graft combination. The optimal approach for managing stent fractures has not yet reached a consensus. The embedding of a second stent, surgery, and parallel TIPS are currently the most common methods used for managing stent fractures. Early recognition and prompt intervention are essential in managing stent fractures after TIPS to mitigate potential risks and ensure optimal patient outcomes.
- Citation: Zhou TY, Wang HL, Tao GF, Chen SQ. Stent fracture after transjugular intrahepatic portosystemic shunt: A case report. World J Gastrointest Surg 2025; 17(5): 104893
- URL: https://www.wjgnet.com/1948-9366/full/v17/i5/104893.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i5.104893
Transjugular intrahepatic portosystemic shunt (TIPS) represents a very effective treatment for complications of portal hypertension. Although TIPS creation is a minimally invasive interventional procedure, it is technically complex and may be accompanied by various complications[1,2]. Stent fracture is a rare and infrequently reported complication of TIPS. There are only a handful of published case reports describing this problem. Stent fracture can be a potentially dangerous event and usually requires additional interventional therapy or may unfortunately require surgery for retrieval of a distally migrated fragment[3]. Early recognition and prompt management may be able to prevent further problems. In this report, we describe a case of stent fracture after TIPS creation and review the available literature on stent fracture after TIPS creation to investigate the underlying mechanisms of this complication.
A 56-year-old male presented with recurrent melena for over 4 months.
Four months ago, the patient began experiencing recurrent melena without any apparent trigger, which prompted a visit to a local hospital. Abdominal ultrasound revealed cirrhosis, splenomegaly, and ascites. Gastroscopy examination showed severe varices in the mid and lower esophageal segments and gastric fundus, indicating portal hypertension-related gastric disease. The patient received symptomatic treatment, including hemostasis, blood transfusion, acid suppression, and fluid replacement at a local hospital. The patient sought further treatment with TIPS at our hospital, where he was admitted with a diagnosis of “cirrhosis with esophagogastric variceal bleeding” based on outpatient evaluation.
The patient had a history of hepatitis B cirrhosis for 6 years and had been regularly taking entecavir 0.5 mg/day for antiviral therapy.
The abdomen was flat without rebound pain, muscle tension, or palpable masses. The liver and spleen were nonpalpable below the costal margins. Murphy’s sign was negative, and there was no hepatic tenderness.
Laboratory tests revealed a positive hepatitis B surface antigen result, with hepatitis B virus-DNA levels below the lower detection limit. Renal function and coagulation tests were within normal ranges. The complete blood count showed a white blood cell count of 2.47 × 109/L, hemoglobin at 54 g/L, and a platelet count of 54 × 109/L. Blood biochemistry results included albumin at 44.0 g/L, alanine aminotransferase at 16 U/L, aspartate aminotransferase at 14 U/L, and total bilirubin at 10.3 μmol/L.
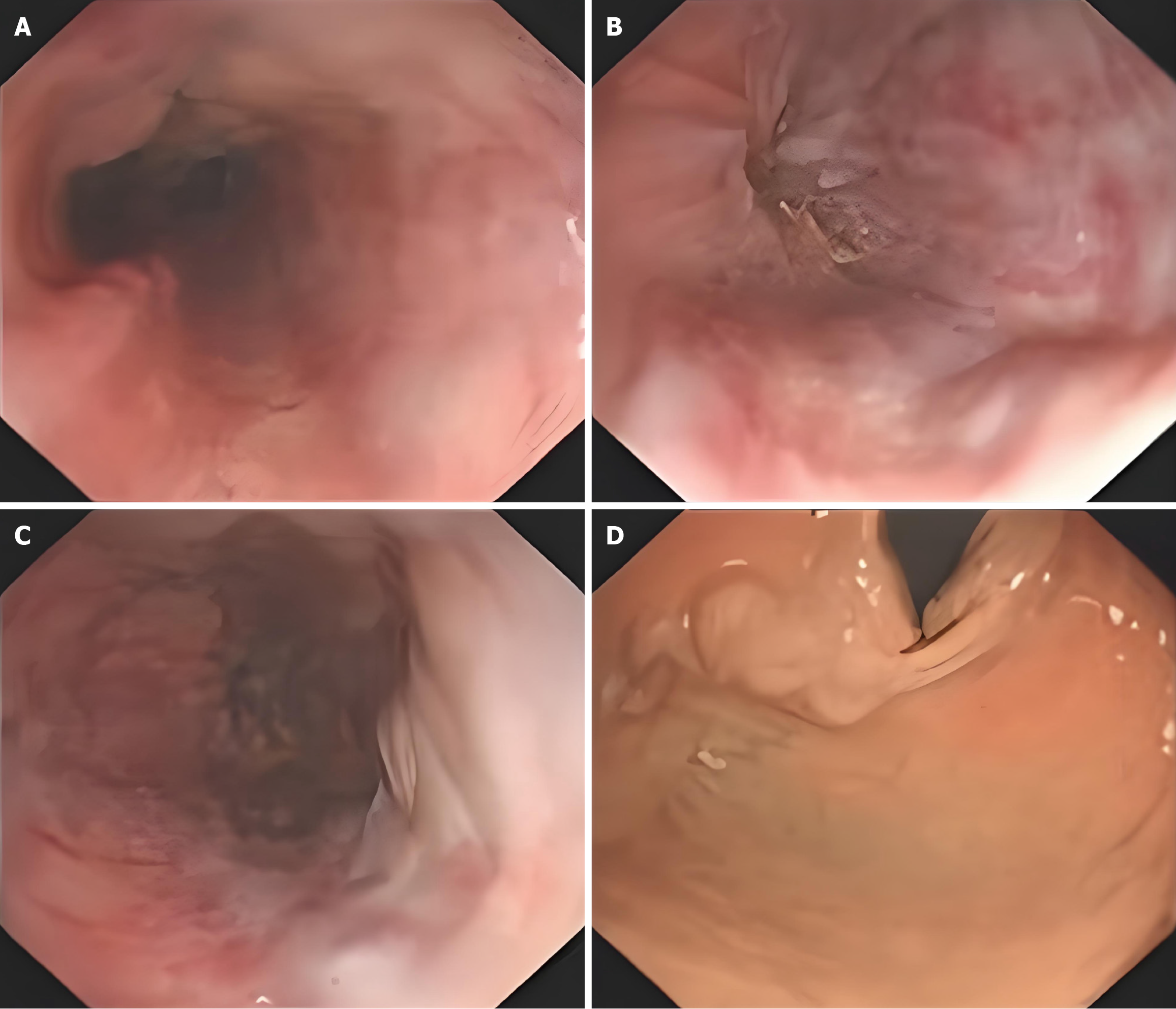
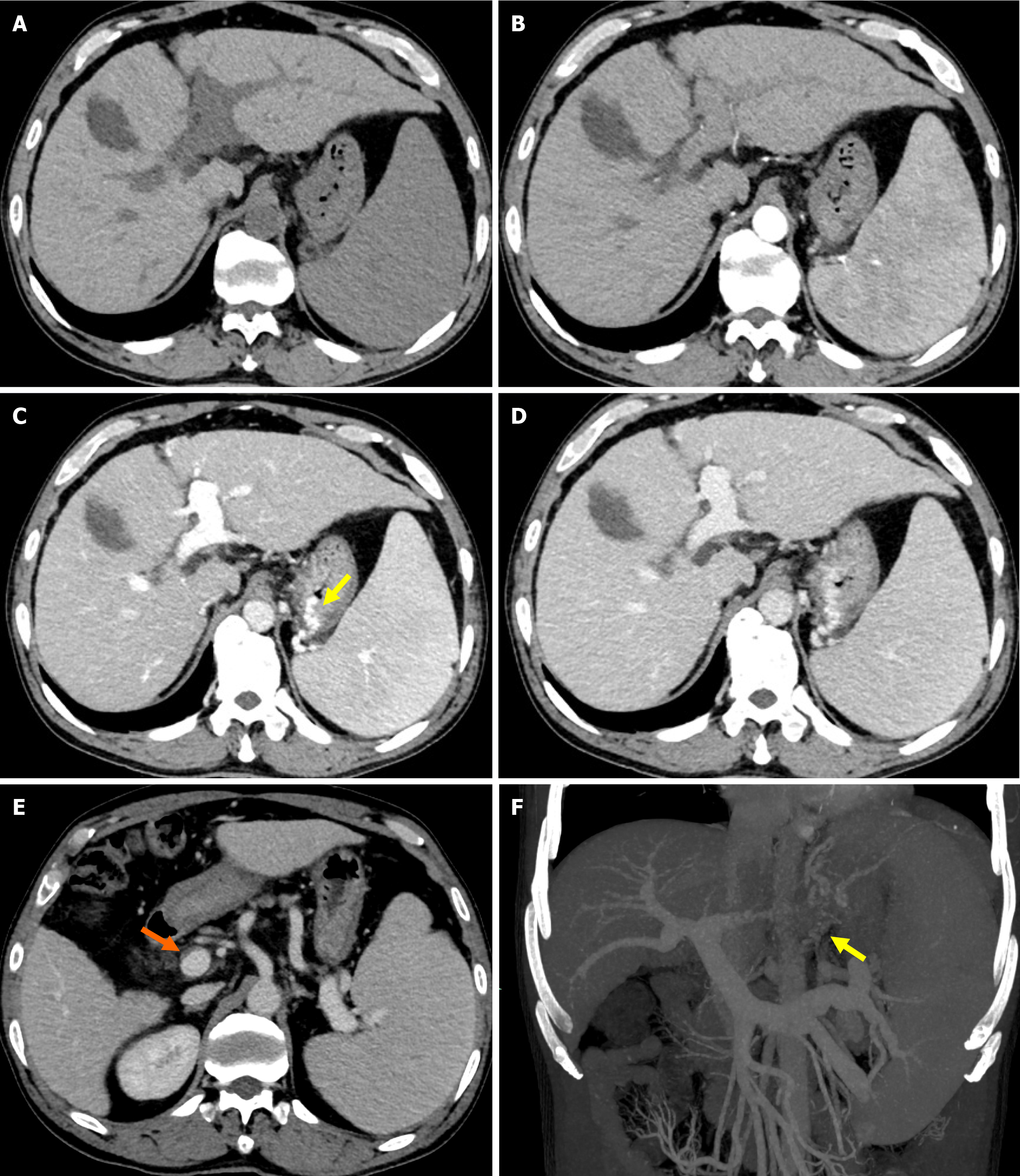
Gastroscopy examination showed severe varices in the mid and lower esophageal segments and gastric fundus, indicating portal hypertension-related gastric disease (Figure 1). Abdominal computed tomography (CT) examination revealed cirrhosis, splenomegaly, portal hypertension with collateral circulation formation, and a small amount of mural thrombosis in the main portal vein, superior mesenteric vein, and splenic vein (Figure 2).
The patient was finally diagnosed with portal hypertension, esophagogastric variceal bleeding, decompensated hepatitis B cirrhosis, splenomegaly, and hypersplenism.
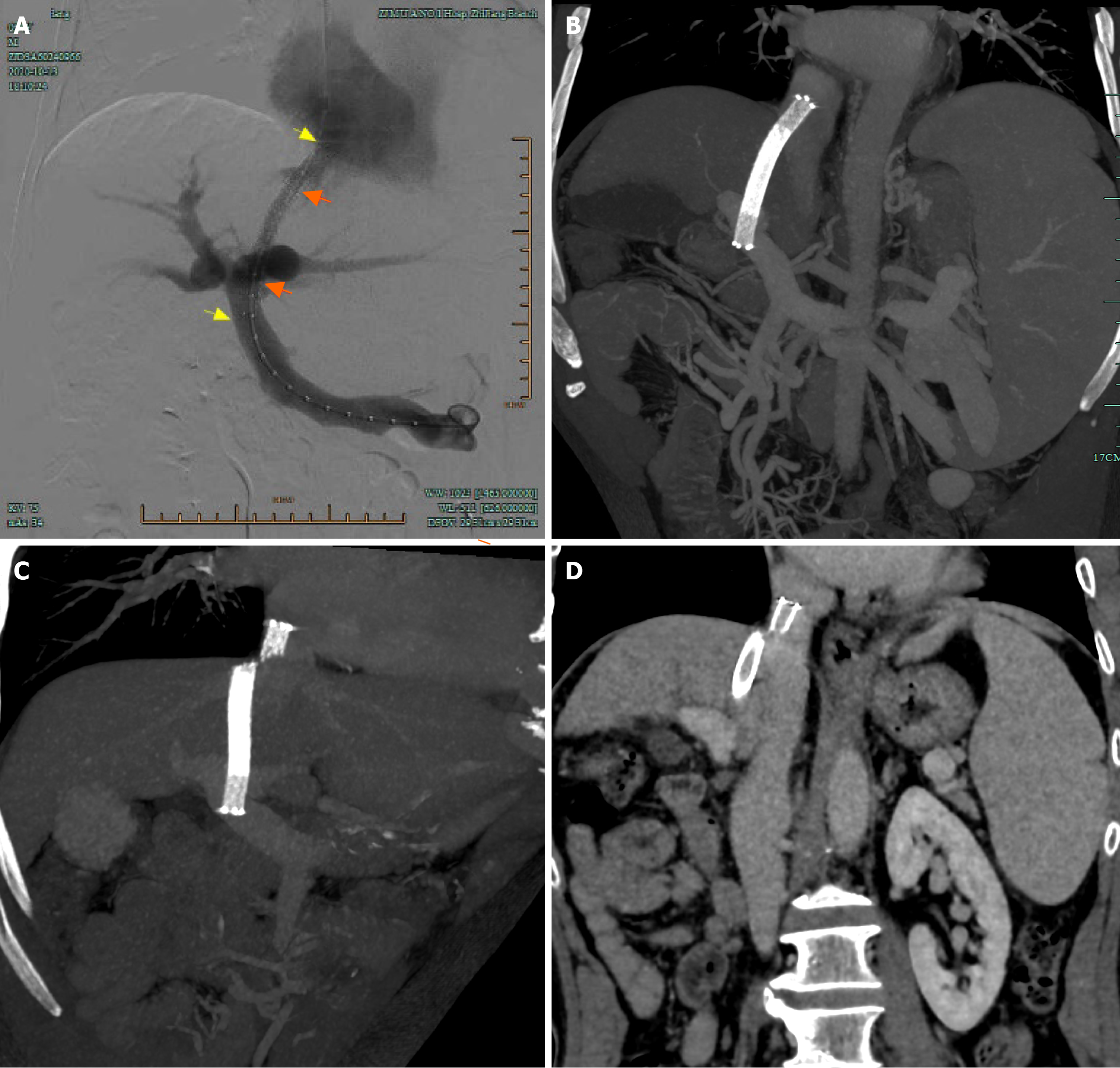
A TIPS was created with a bare metal stent/stent-graft combination as the Viator stent was not covered by National Health Insurance at that time, although it is available in China. First, a TIPS was created with an 8 mm × 80 mm self-expanding bare Nitinol stent (Epic Vascular Stent: Boston Scientific, United States) from the right hepatic vein to the left portal vein. Subsequently, an 8 mm × 50 mm Viabahn stent-graft (WL Gore Associates, Inc., Flagstaff, AZ, United States) was placed to cover the entire intraparenchymal portion of the shunt tract. The distal portion of the bare metal stent overlapped the stent-graft, while its proximal portion of approximately 25 mm protruded into the inferior vena cava (IVC) (Figure 3A). The final portography demonstrated a patent shunt (Figure 3A). Portal pressure decreased from 35 to 25 mmHg, and portocaval pressure gradient (PPG) decreased from 25 to 11 mmHg.
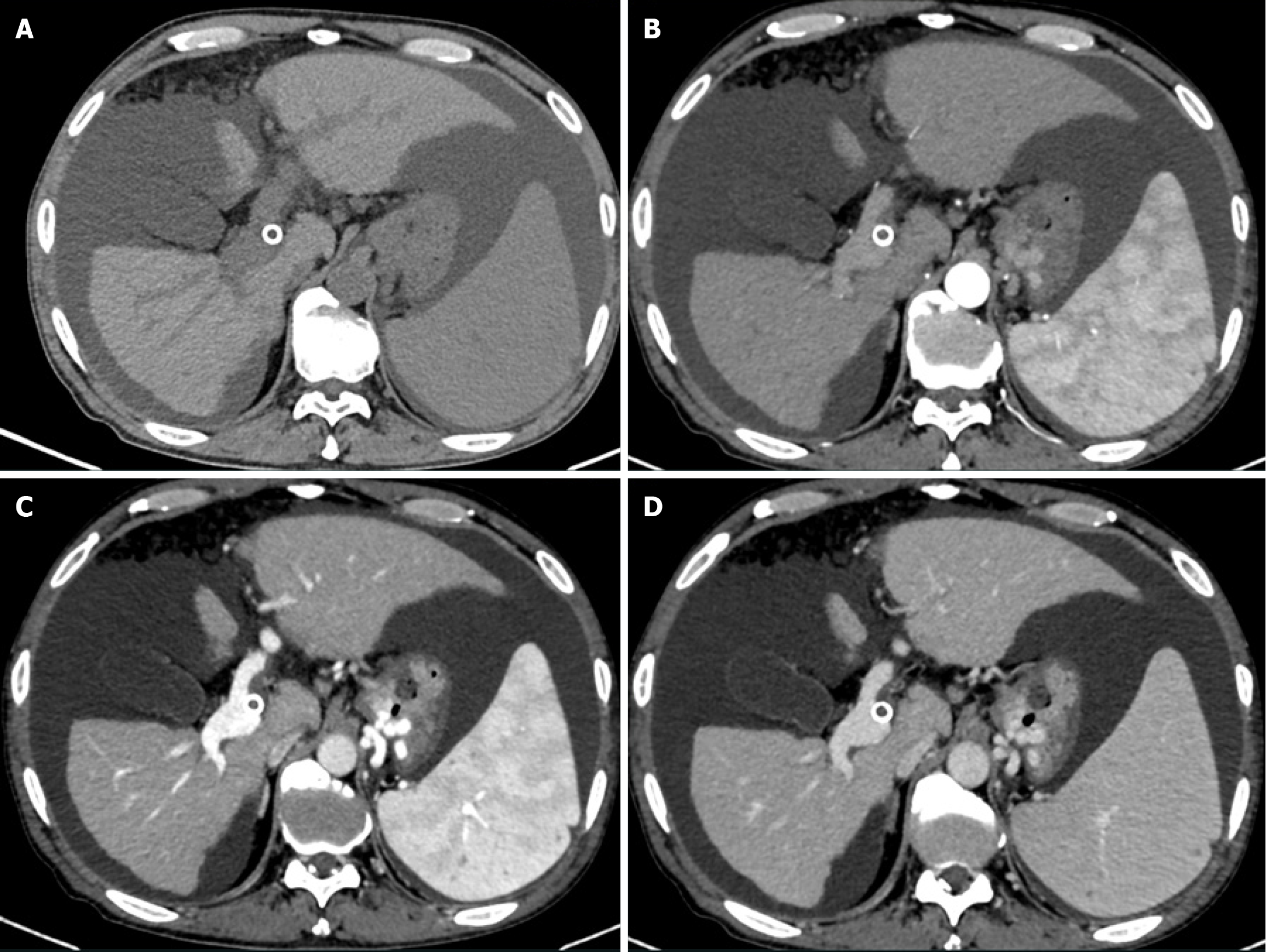
Following the procedure, melena disappeared immediately and the patient was transferred out on day 3. And the patient was advised to undergo follow-up liver CT angiography at 1 and 3 months postoperatively to assess shunt patency and monitor for the development of hepatocellular carcinoma. Subsequent evaluations should then be performed every six months thereafter. CT images one month after TIPS creation revealed metallic continuity of the stents (Figure 3B). However, follow-up CT imaging at 15 months post-procedure demonstrated stent fracture at the hepatocaval confluence (Figure 3C), although notably, the stent lumen remained patent (Figure 3D). A 20 mm stent fragment was radiologically confirmed to be lodged within the infra-diaphragmatic segment of the IVC, exhibiting positional stability without evidence of proximal migration toward the right atrium on serial imaging surveillance. The patient was treated conservatively as he was asymptomatic. CT images and color Doppler ultrasound 14 months after the procedure demonstrated neither further stent fracture nor further dislocation of the stent fragment. No symptoms associated with the stent fracture were observed for 15 months. However, the patient was readmitted 30 months post-TIPS due to recurrent esophagogastric variceal bleeding and ascites. Enhanced abdominal CT indicated occlusion of the original shunt (Figure 4). An attempt to revise the dysfunctional shunt via a stent-in-stent approach was conducted but was unsuccessful. Con
Although current clinical guidelines recommend the use of the specialized Viatorr® stent for TIPS procedures[4], in some regions of China and other parts of the world where these Viatorr® stents are unavailable, a bare metal stent/stent-graft combination is still used to complete TIPS. Cohort studies indicate comparable efficacy between the Viatorr® stent and bare metal stent/stent-graft combinations, with no significant differences in shunt patency rates, technical success, hemodynamic outcomes, or encephalopathy incidence[5-7]. These findings suggest that a bare metal stent/stent-graft combination may serve as a practical alternative in regions lacking access to Viatorr® stents. Furthermore, even when employing specialized Viatorr® stents during TIPS procedures, supplemental bare stents might be required to extend undersized shunt constructs. However, this hybrid approach carries inherent risks of subsequent device integrity complications, particularly stent fracture. Therefore, it is still of great clinical significance for TIPS surgeons and physicians in the field of liver and gastrointestinal diseases to understand and recognize the types, potential risks, treatment strategies, and clinical outcomes of TIPS stent fractures.
Stent fracture may occur late as a result of mechanical fatigue or early in association with suboptimal deployment[8]. There are various risk factors or theories that have been ascribed to the causes of stent fracture, such as longer stents, multiple overlap stents, stents across bends or joints, and a variety of mechanical stresses leading to fatigue failure of Nitinol stents[9]. Grimme et al[10] observed that uncovered stents exhibited a higher incidence of fracture compared to covered counterparts, attributing this phenomenon to potential mechanical stressors, including cardiac cycle-induced motion and anatomical mismatch-derived forces between the graft and native vasculature. Zabicki et al[11] were convinced that high bending stress was a cause of stent fracture in an atypical angulated TIPS which was created between the left hepatic and left portal vein. Ding et al[12] presumed that stress against the bare metal stent at the trailing end of the stent-graft was another cause of stent fracture. Komaki et al[13] considered the material and design of the stent, along with friction of the stent edge against the contralateral wall of the IVC induced by diaphragmatic movement can also cause stent fracture. In our case, movement of the diaphragm induces significant displacement of the liver during respiration which can cause both bending and torsional forces on the hepatic vein. Therefore, the part of the stent inserted in the hepatic vein will result in mechanical fatigue over time and lead to fracture. Furthermore, the utilization of a bare metal stent/stent-graft combination with overlapping placement of two stents, as observed in our case, may contribute to increased stiffness at the overlapped region. This heightened stiffness could potentially be an additional factor leading to stent fracture[14].
There is no consensus on the management of stent fractures. Treatment mainly depends on the type of stent fracture, clinical symptoms and potential risks[3,13]. Stent fracture can be classified as type I (no loss of stent integrity), type II (loss of stent integrity), and type III (separation or embolization of the fractured segment)[15]. Treatment of type I and type II stent fractures is typically performed using interventional procedures to insert a second stent to stabilize the fractured parts (stent-in-stent maneuver)[16]. However, surgery may be required to retrieve the distally migrated fragment in type III stent fractures, as the fragment can move into the right atrium, right ventricle and the pulmonary artery resulting in conduction abnormalities, valvular damage, perforation and possible death[17]. Fortunately, this rarely occurs. Komaki et al[13] reported a patient with a type III stent fracture after TIPS who was treated conservatively as he was asymptomatic for 15 months and follow-up CT images demonstrated neither further stent fracture nor further dislocation of the stent fragment. Two similar cases with type III stent fractures caused no acute mechanical complications and were managed conservatively[3,12]. In our case, the patient developed a type III stent fracture but the fragment did not migrate distally. He was treated conservatively as he was asymptomatic. Unfortunately, the patient was hospitalized due to recurrent esophagogastric variceal bleeding and ascites caused by shunt thrombosis 30 months later. Following failed attempts to recanalize the original shunt, a successful parallel TIPS was established via the proximal end of the fractured stent to decompress the portal venous system, effectively mitigating the variceal bleeding and ascites. Additionally, the anchoring effect of the newly implanted stent minimized the risk of stent fragment migration into the right atrium, right ventricle, and pulmonary artery. After parallel TIPS, the patient experienced no further episodes of bleeding or ascites, and is currently under follow-up observation.
TIPS stent fracture is rare and the presence of TIPS stent angulation and the use of overlapping stent-graft and bare stent increase the risk of stent fracture with the most common site being the junction of stent-graft and bare stent. The treatment for stent fracture mainly depends on the type of stent fracture, clinical symptoms and potential risks. Conservative treatment is feasible in asymptomatic patients under close follow-up; however, early intervention should also be considered for patients at risk of stent fragment displacement or shunt occlusion.
The authors would like to thank the patient for his participation and his consent to the publication of the case details and associated images.
| 1. | Shah RP, Sze DY. Complications During Transjugular Intrahepatic Portosystemic Shunt Creation. Tech Vasc Interv Radiol. 2016;19:61-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 2. | Suhocki PV, Lungren MP, Kapoor B, Kim CY. Transjugular intrahepatic portosystemic shunt complications: prevention and management. Semin Intervent Radiol. 2015;32:123-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 99] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 3. | Grewal S, Sidhu R, Elhassan M. Rings Flying Around: A rare complication of Transjugular Intrahepatic Portosystemic Shunt. Respir Med Case Rep. 2022;36:101586. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Lee EW, Eghtesad B, Garcia-Tsao G, Haskal ZJ, Hernandez-Gea V, Jalaeian H, Kalva SP, Mohanty A, Thabut D, Abraldes JG. AASLD Practice Guidance on the use of TIPS, variceal embolization, and retrograde transvenous obliteration in the management of variceal hemorrhage. Hepatology. 2024;79:224-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 86] [Article Influence: 43.0] [Reference Citation Analysis (0)] |
| 5. | Bai Y, Liu J, Wang C, Yao W, Ju S, Wang Y, Zhou C, Dong X, Zheng C. Comparison of specialized stent versus generic stent and bare stent combination for transjugular intrahepatic portosystemic shunt creation. Sci Rep. 2024;14:14439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Saad WE, Darwish WM, Davies MG, Waldman DL. Stent-grafts for transjugular intrahepatic portosystemic shunt creation: specialized TIPS stent-graft versus generic stent-graft/bare stent combination. J Vasc Interv Radiol. 2010;21:1512-1520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Li W, Liu M, Guan S, Ding P, Yuan J, Zhao Y, Li P, Ma F, Xue H. Comparison of outcomes for transjugular intrahepatic portosystemic shunt creation: Viatorr versus Fluency versus a bare stent/Fluency stent combination. CVIR Endovasc. 2024;7:76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 8. | Malla S, Razik A, Yadav R, Gamanagatti S. Endovascular Management of Stent Fracture Causing Trans-jugular Intrahepatic Portosystemic Shunt Stent Malfunction. Tropical Gastroenterology. 2022;43:46-49. [DOI] [Full Text] |
| 9. | Lin Y, Tang X, Fu W, Kovach R, George JC, Guo D. Stent fractures after superficial femoral artery stenting: risk factors and impact on patency. J Endovasc Ther. 2015;22:319-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (1)] |
| 10. | Grimme FA, Zeebregts CJ, Verhoeven EL, Bekkema F, Reijnen MM, Tielliu IF. Visceral stent patency in fenestrated stent grafting for abdominal aortic aneurysm repair. J Vasc Surg. 2014;59:298-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 58] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 11. | Zabicki B, Ricke J, Dudeck O, Pech M. CT-assisted transfemoral intrahepatic portosystemic shunt in a long duration follow-up: A case report. Pol J Radiol. 2014;79:39-41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Ding PX, Han XW, Hua ZH, Liu C. Stent Fracture and Fragment Migration to Chordae Tendineae of the Tricuspid Valve after Transjugular Intrahepatic Portosystemic Shunt Procedure. J Vasc Interv Radiol. 2017;28:1293-1295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 13. | Komaki T, Hiraki T, Uka M, Fujiwara H, Iguchi T, Kanazawa S. A Case of Stent Fracture After Transjugular Intrahepatic Portosystemic Shunt. Cardiovasc Intervent Radiol. 2018;41:976-978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Krajina A. Stent Fracture After Transjugular Intrahepatic Portosystemic Shunt: Reply. Cardiovasc Intervent Radiol. 2018;41:1636-1637. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Nordmeyer J, Khambadkone S, Coats L, Schievano S, Lurz P, Parenzan G, Taylor AM, Lock JE, Bonhoeffer P. Risk stratification, systematic classification, and anticipatory management strategies for stent fracture after percutaneous pulmonary valve implantation. Circulation. 2007;115:1392-1397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 147] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 16. | Knirsch W, Haas NA, Lewin MA, Uhlemann F. Longitudinal stent fracture 11 months after implantation in the left pulmonary artery and successful management by a stent-in-stent maneuver. Catheter Cardiovasc Interv. 2003;58:116-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 51] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 17. | Li Y, Sun J, Zhou T, Wang W, Wang G, Hou Q, Chen Z, Wang Q, Xu K, Ye Y, Bao J. Untimely surgery for stent-fracture-related death after transjugular intrahepatic portosystemic shunt: a case report. Ther Adv Chronic Dis. 2024;15:20406223241243258. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |