Published online May 27, 2025. doi: 10.4240/wjgs.v17.i5.104191
Revised: March 17, 2025
Accepted: April 3, 2025
Published online: May 27, 2025
Processing time: 161 Days and 18.8 Hours
Both stent placement and endoscopic nasobiliary drainage (ENBD) are commonly used for treating bile leakage following liver transplantation. However, little research has compared the advantages of both methods.
To compare the prognosis of stent placement and ENBD in treating bile leakage following liver transplantation.
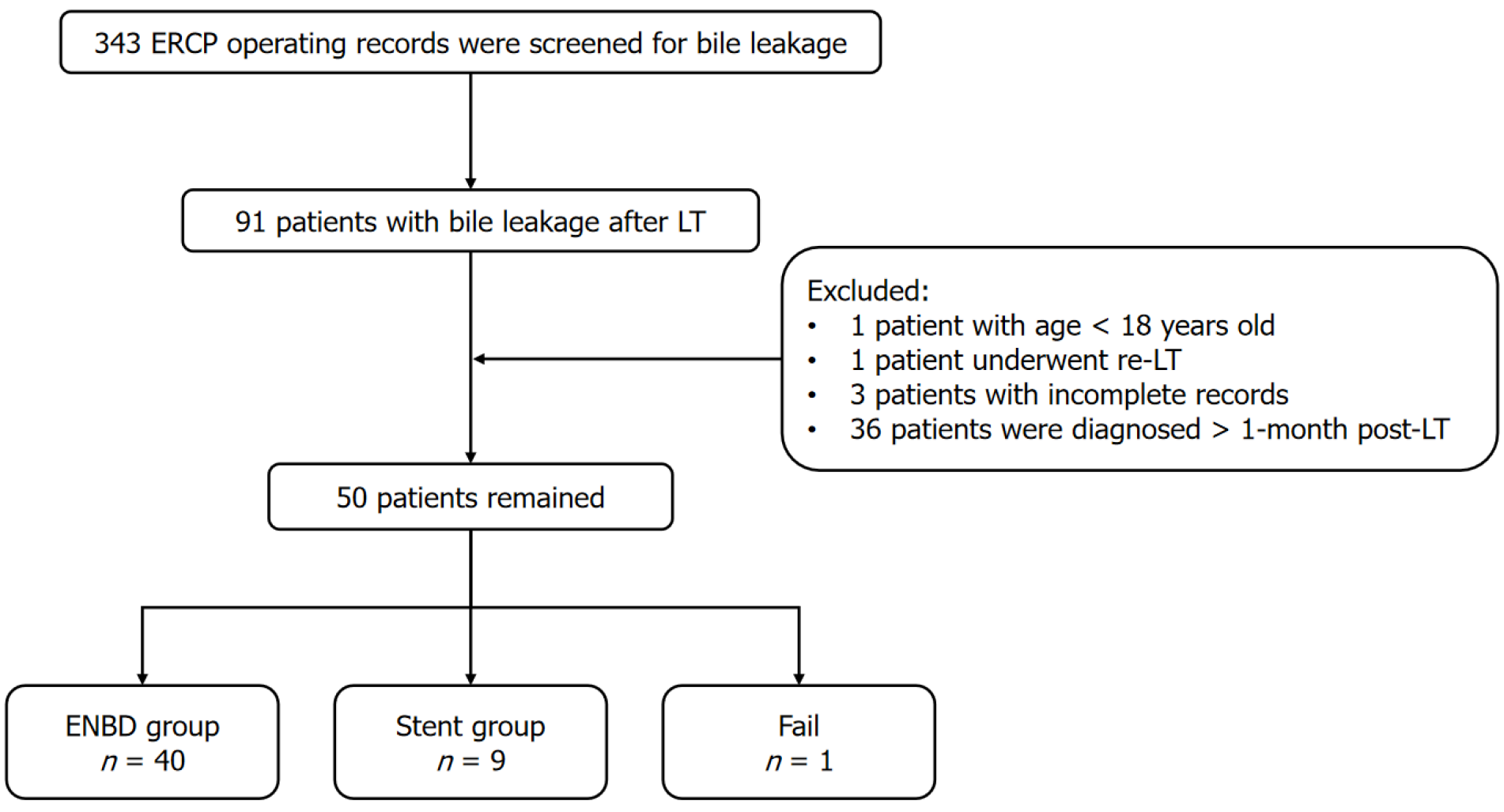
We retrospectively collected data for patients with bile leakage after liver tran
We retrospectively collected data from 50 patients diagnosed with bile leakage within 1 month after liver transplantation. Forty patients underwent ENBD and nine received stent placement. Baseline patient characteristics, except white blood cell count, total bilirubin and direct bilirubin levels, were comparable between the two groups. Additionally, there was no significant difference in the rates of re
Stent placement and ENBD are recommended for treating bile leakage after liver transplantation, with similar efficacy and prognosis.
Core Tip: Both stent placement and endoscopic nasobiliary drainage are effective for treating bile leakage after liver transplantation, with comparable efficacy and prognosis. Our retrospective study of 50 patients showed no significant differences in outcomes, except for variations in white blood cell count and bilirubin levels. Both methods are recommended based on similar success rates and post-operative complications.
- Citation: Gu YJ, Chen ZT, Li QY. Stent placement can achieve same prognosis as endoscopic nasobiliary drainage in treatment of bile leakage after liver transplantation. World J Gastrointest Surg 2025; 17(5): 104191
- URL: https://www.wjgnet.com/1948-9366/full/v17/i5/104191.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i5.104191
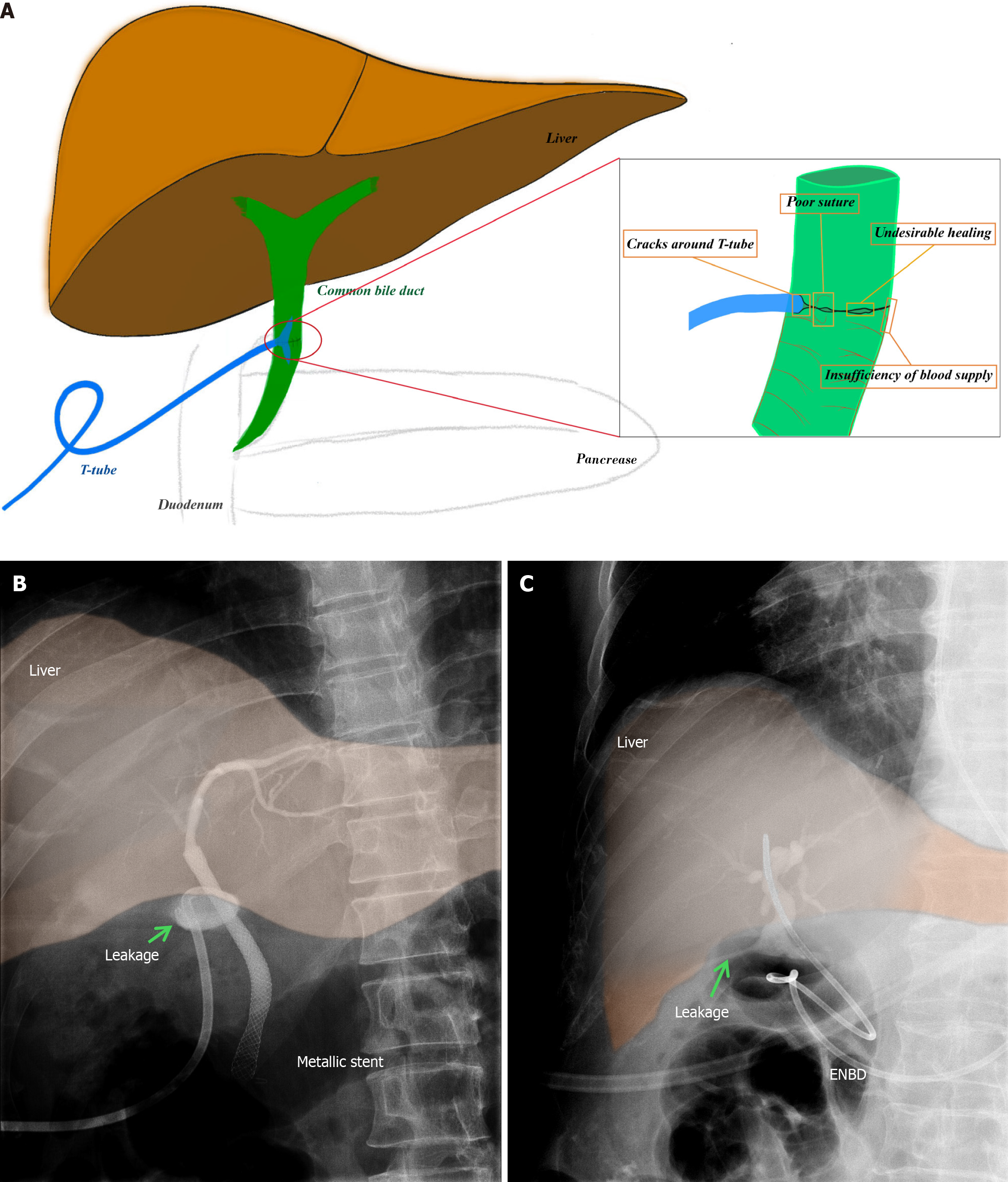
Biliary complications including biliary anastomotic stricture and bile leakage, are major source of morbidity after liver transplantation, with an incidence of 5%-32%[1]. According to the United Kingdom National Health Service, bile duct complications after liver transplantation include bile leakage, bile duct strictures, bile duct stones, and sphincter of Oddi dysfunction. Among these, bile leakage is one of the most common complications, with an incidence rate ranging from 2% to 25%, which is more common in living donor than in deceased donor liver transplantation[2]. Bile leakage is the second most common biliary complication of liver transplantation, which can be classified in two categories: Early (within 4 weeks of transplantation) and late (> 4 weeks after transplantation)[3]. Early bile leakage is considered as a result of technical problems rather than related to the type of biliary reconstruction (Figure 1)[3]. However, it is associated with planned or inadvertent T-tube removal[1]. Thus, early bile leakage usually occurs at the anastomotic or T-tube insertion site. It is often accompanied by infection, pain, and delayed graft function, posing a threat to patient survival and quality of life.
Endoscopy plays a pivotal role in the diagnosis and treatment of biliary diseases. Notably, endoscopic sphincterotomy, stenting, and drainage have been recommended for managing biliary leakage[4-6]. According to a systematic review, the success rate of endoscopic therapy for bile leak ranges from 68% to 98.3%[7]. In patients who have undergone liver transplantation, endoscopic nasobiliary catheter or plastic stent placement is a safe and effective treatment for bile duct strictures following bile leak resolution[8]. Favorable outcomes are more likely when the duct injury measures < 5 mm or occurs extrahepatically, and when there is no associated abscess or biloma[9]. However, the comparative efficiency and long-term prognosis of endoscopic nasobiliary catheter vs plastic stent placement have received limited attention in previous studies. Therefore, this comprehensive investigation aimed to analyze patient-related factors and compare the advantages and disadvantages of these two methods.
We retrospectively analyzed adult patients who underwent endoscopic retrograde cholangiopancreatography (ERCP) for bile leakage after liver transplantation at our center between June 2016 and January 2023. We included only those patients who underwent ERCP within 30 days after surgery. All patients had received piggyback or right lobe liver trans
We retrospectively included 50 patients after cadaveric liver transplantation. One patient was withdrawn due to difficult gastroscopic access. Forty patients underwent endoscopic nasobiliary drainage (ENBD) and nine received stent place
| ENBD (n = 40) | Stent (n = 9) | P value | |
| Age, years | 49.83 ± 10.25 | 51.56 ± 7.30 | 0.000 |
| Male | 35 (87.5) | 7 (77.8) | 0.451 |
| Cause for LT | 0.946 | ||
| Hepatocellular carcinoma | 18 (45.0) | 5 (55.6) | |
| Decompensated cirrhosis | 12 (30.0) | 2 (22.2) | |
| Acute-on-chronic liver failure | 4 (10) | 1 (11.1) | |
| Acute liver failure | 1 (2.5) | 1 (11.1) | |
| Others | 5 (12.5) | 0 | |
| TB | 57.77 ± 49.96 | 102.22 ± 98.45 | 0.000 |
| DB | 44.51 ± 42.61 | 78.33 ± 81.31 | 0.001 |
| WBC | 7.58 ± 4.11 | 9.18 ± 7.23 | 0.030 |
| CRP | 37.33 ± 39.18 | 31.30 ± 34.82 | 0.931 |
| PCT | 2.38 ± 5.25 | 1.20 ± 1.51 | 0.263 |
| Ab | 36.85 ± 3.61 | 38.64 ± 4.52 | 0.357 |
| AST | 134.82 ± 346.01 | 54.22 ± 29.24 | 0.198 |
| ALT | 177.90 ± 236.18 | 130.78 ± 152.20 | 0.460 |
| GGT | 162.08 ± 145.97 | 119.22 ± 59.37 | 0.089 |
| ALP | 134.95 ± 86.02 | 136.11 ± 66.70 | 0.230 |
| T-tube placement | 4 (10) | 2 (22.2) | 0.312 |
| Fever | 14 (35) | 3 (33.3) | 0.885 |
Incidence of fever was similar in both groups, with 35% in the ENBD group and 33.3% in the stent group. Laboratory values showed a higher white blood cell (WBC) count in the stent group (9.1778 ± 7.23356) compared to the ENBD group (7.5769 ± 4.10888, P = 0.030). Total bilirubin (TB) and direct bilirubin (DB) levels were significantly higher in the stent group (P = 0.000 for TB and P = 0.001 for DB), suggesting more severe liver function impairment in this group. No significant differences were noted in C-reactive protein, procalcitonin, albumin, aspartate aminotransferase, alanine aminotransferase, gamma-glutamyl transpeptidase, and alkaline phosphatase levels between the two groups. About 26 patients in the ENBD group underwent secondary operation within 1 month for stent placement, and leakage recurred in three of them. A dualistic logistic regression model was used to confirm the significance of types of operation in prognosis and postoperative biliary stricture, which also came out negative (P = 0.392 and 0.890).
T-tube placement is a risk factor for bile leakage. 10% of the patients in ENBD group and 22.2% in the stent group underwent T-tube placement. Fisher’s exact test was used as only one of the stent group failed to recover from leakage, and there was no significant difference between the groups (P = 0.412). Patients who died or underwent biliary surgery within 6 months after transplantation were not included in the analysis of biliary stricture. Three patients underwent biliary surgery due to failure of treatment, and 11 patients died due to infection and graft failure. Finally, nine patients in the ENBD group and two in the stent group result biliary stricture, and 17 patients in ENBD group and seven in the stent group were not. Fisher’s exact test showed no significant difference in biliary stricture between two groups (P = 1.0). Further, binary logistic regression was also performed, showing no significant difference between the two groups (P = 0.292 for recovery and P = 0.890 for biliary stricture) (Table 2). The significant variables in Table 1, including age, WBC count and TB, were taken as covariates. Although our study highlighted significant differences in age, WBC count, and TB and DB levels between the ENBD and stent groups, there was no significant difference in prognosis and postoperative biliary stricture.
| ENBD (n = 40) | Stent (n = 9) | P value | Binary logistic regression | |
| Recovery | 28 (70) | 8 (88.9) | 0.412 | 0.292 |
| Biliary stricture | 9 (28) | 2 (7) | 1.0 | 0.890 |
Bile leakage can be a postoperative complication of gallbladder removal or liver transplantation, or damage to the bile ducts and biliary system[10]. Around 2.7% of deceased donor liver transplantation recipients have bile leakage after surgery, which rises over 10% of patients undergoing living donor liver transplantation[10,11]. The rate of bile leakage can be higher in patients with cholangiojejunostomy. Endoscopic techniques are recommended as first-line treatment of biliary complications after liver transplantation, with a success rate of 70%-100%[12]. However, ERCP is limited in patients after cholangiojejunostomy, especially with Roux-en-Y gastric bypass[13]. Endoscopic ultrasound or endoscopic ultrasound-directed transgastric ERCP can help overcome the challenge of cholangiojejunostomy, However, it is a double-step technique, and only 40% patients completed conventional ERCP during the index procedure. Further, about 17% of patients ended up with metal stent dislodged. Bile leakage in patients after liver transplantation is always followed by infection, immune dysfunction and delayed wound healing. It is difficult to build a reliable and long-term monitoring method to ensure the success rate at the first attempt. A failed invasive procedure would significantly increase the risk of gastrointestinal perforation.
Research has confirmed the important role of endoscopic treatment in bile leakage after liver transplantation, but few studies have compared the difference between stent placement and ENBD. Stents provide a long-term solution and are less invasive compared to surgical options. They are often left in place for several weeks to months to ensure healing. Compared to ENBD, stents can provide internal biliary support, which help prevent bile duct stenosis. Covered re
ENBD allows for the direct external drainage of bile, which can be beneficial in managing the leak and in monitoring the volume and nature of the bile for diagnostic and therapeutic purposes. However, ENBD is temporary and can be uncomfortable for the patient due to passage of the tube through the nose. It also requires careful maintenance of the external drainage system and maintaining water-electrolyte balance. Although ENBD alone can rapidly cure posto
There were several limitations in this study. First, we did not assess the severity of bile leakage. ENBD contains the advantages of less damage, faster and can cooperate with external negative pressure device, thus patients with severe disease tend to choose ENBD rather than stents. Secondly, as this is a retrospective study, due to the data deficiency, it is difficult to compare the recovery duration between the two groups. Thirdly, insufficient follow-up duration prevented the assessment of long-term prognosis and survival analysis. Finally, the sample size was small, and the relatively lenient patient selection criteria may have introduced selection bias. Thus, more dates are required to verify our results.
This study showed that stent placement and ENBD are recommended for treating bile leakage after liver transplantation, as they exhibit similar efficacy and prognosis.
| 1. | Kochhar G, Parungao JM, Hanouneh IA, Parsi MA. Biliary complications following liver transplantation. World J Gastroenterol. 2013;19:2841-2846. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 186] [Cited by in RCA: 184] [Article Influence: 14.2] [Reference Citation Analysis (1)] |
| 2. | Jung DH, Ikegami T, Balci D, Bhangui P. Biliary reconstruction and complications in living donor liver transplantation. Int J Surg. 2020;82S:138-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 64] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 3. | Thuluvath PJ, Pfau PR, Kimmey MB, Ginsberg GG. Biliary complications after liver transplantation: the role of endoscopy. Endoscopy. 2005;37:857-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 154] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 4. | Londoño MC, Balderramo D, Cárdenas A. Management of biliary complications after orthotopic liver transplantation: the role of endoscopy. World J Gastroenterol. 2008;14:493-497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 61] [Cited by in RCA: 64] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Lisotti A, Fusaroli P, Caletti G. Role of endoscopy in the conservative management of biliary complications after deceased donor liver transplantation. World J Hepatol. 2015;7:2927-2932. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Larghi A, Tringali A, Rimbaş M, Barbaro F, Perri V, Rizzatti G, Gasbarrini A, Costamagna G. Endoscopic Management of Benign Biliary Strictures After Liver Transplantation. Liver Transpl. 2019;25:323-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 7. | Chon HK, Shin EJ, Kim SH. The Need for a Better-Designed Study of the Outcomes of Endoscopic Management of Bile Leak. Clin Endosc. 2020;53:633-635. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Liao JZ, Zhao Q, Qin H, Li RX, Hou W, Li PY, Liu NZ, Li DM. Endoscopic diagnosis and treatment of biliary leak in patients following liver transplantation: a prospective clinical study. Hepatobiliary Pancreat Dis Int. 2007;6:29-33. [PubMed] |
| 9. | de'Angelis N, Catena F, Memeo R, Coccolini F, Martínez-Pérez A, Romeo OM, De Simone B, Di Saverio S, Brustia R, Rhaiem R, Piardi T, Conticchio M, Marchegiani F, Beghdadi N, Abu-Zidan FM, Alikhanov R, Allard MA, Allievi N, Amaddeo G, Ansaloni L, Andersson R, Andolfi E, Azfar M, Bala M, Benkabbou A, Ben-Ishay O, Bianchi G, Biffl WL, Brunetti F, Carra MC, Casanova D, Celentano V, Ceresoli M, Chiara O, Cimbanassi S, Bini R, Coimbra R, Luigi de'Angelis G, Decembrino F, De Palma A, de Reuver PR, Domingo C, Cotsoglou C, Ferrero A, Fraga GP, Gaiani F, Gheza F, Gurrado A, Harrison E, Henriquez A, Hofmeyr S, Iadarola R, Kashuk JL, Kianmanesh R, Kirkpatrick AW, Kluger Y, Landi F, Langella S, Lapointe R, Le Roy B, Luciani A, Machado F, Maggi U, Maier RV, Mefire AC, Hiramatsu K, Ordoñez C, Patrizi F, Planells M, Peitzman AB, Pekolj J, Perdigao F, Pereira BM, Pessaux P, Pisano M, Puyana JC, Rizoli S, Portigliotti L, Romito R, Sakakushev B, Sanei B, Scatton O, Serradilla-Martin M, Schneck AS, Sissoko ML, Sobhani I, Ten Broek RP, Testini M, Valinas R, Veloudis G, Vitali GC, Weber D, Zorcolo L, Giuliante F, Gavriilidis P, Fuks D, Sommacale D. 2020 WSES guidelines for the detection and management of bile duct injury during cholecystectomy. World J Emerg Surg. 2021;16:30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 139] [Cited by in RCA: 135] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 10. | Fang C, Yan S, Zheng S. Bile Leakage after Liver Transplantation. Open Med (Wars). 2017;12:424-429. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Morelli J, Mulcahy HE, Willner IR, Baliga P, Chavin KD, Patel R, Payne M, Cotton PB, Hawes R, Reuben A, Cunningham JT. Endoscopic treatment of post-liver transplantation biliary leaks with stent placement across the leak site. Gastrointest Endosc. 2001;54:471-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Magro B, Tacelli M, Mazzola A, Conti F, Celsa C. Biliary complications after liver transplantation: current perspectives and future strategies. Hepatobiliary Surg Nutr. 2021;10:76-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 53] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 13. | Tyberg A, Nieto J, Salgado S, Weaver K, Kedia P, Sharaiha RZ, Gaidhane M, Kahaleh M. Endoscopic Ultrasound (EUS)-Directed Transgastric Endoscopic Retrograde Cholangiopancreatography or EUS: Mid-Term Analysis of an Emerging Procedure. Clin Endosc. 2017;50:185-190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 93] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 14. | Tabibian JH, Asham EH, Goldstein L, Han SH, Saab S, Tong MJ, Busuttil RW, Durazo FA. Endoscopic treatment with multiple stents for post-liver-transplantation nonanastomotic biliary strictures. Gastrointest Endosc. 2009;69:1236-1243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 40] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Park SY, Park CH, Cho SB, Yoon KW, Lee WS, Kim HS, Choi SK, Rew JS. The safety and effectiveness of endoscopic biliary decompression by plastic stent placement in acute suppurative cholangitis compared with nasobiliary drainage. Gastrointest Endosc. 2008;68:1076-1080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 16. | Johnson KD, Perisetti A, Tharian B, Thandassery R, Jamidar P, Goyal H, Inamdar S. Endoscopic Retrograde Cholangiopancreatography-Related Complications and Their Management Strategies: A "Scoping" Literature Review. Dig Dis Sci. 2020;65:361-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 59] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 17. | ASGE Standards of Practice Committee; Chandrasekhara V, Khashab MA, Muthusamy VR, Acosta RD, Agrawal D, Bruining DH, Eloubeidi MA, Fanelli RD, Faulx AL, Gurudu SR, Kothari S, Lightdale JR, Qumseya BJ, Shaukat A, Wang A, Wani SB, Yang J, DeWitt JM. Adverse events associated with ERCP. Gastrointest Endosc. 2017;85:32-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 405] [Cited by in RCA: 590] [Article Influence: 65.6] [Reference Citation Analysis (0)] |
| 18. | Ishii H, Ochiai T, Murayama Y, Komatsu S, Shiozaki A, Kuriu Y, Ikoma H, Nakanishi M, Ichikawa D, Fujiwara H, Okamoto K, Kokuba Y, Sonoyama T, Otsuji E. Risk factors and management of postoperative bile leakage after hepatectomy without bilioenteric anastomosis. Dig Surg. 2011;28:198-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Sokal A, Sauvanet A, Fantin B, de Lastours V. Acute cholangitis: Diagnosis and management. J Visc Surg. 2019;156:515-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 20. | Tajeddin E, Sherafat SJ, Majidi MR, Alebouyeh M, Alizadeh AH, Zali MR. Association of diverse bacterial communities in human bile samples with biliary tract disorders: a survey using culture and polymerase chain reaction-denaturing gradient gel electrophoresis methods. Eur J Clin Microbiol Infect Dis. 2016;35:1331-1339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (1)] |
| 21. | Cantù P, Mauro A, Cassinotti E, Boni L, Vecchi M, Penagini R. Post-operative biliary strictures. Dig Liver Dis. 2020;52:1421-1427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/