Published online May 27, 2025. doi: 10.4240/wjgs.v17.i5.101414
Revised: March 9, 2025
Accepted: April 17, 2025
Published online: May 27, 2025
Processing time: 251 Days and 23 Hours
Gastrointestinal foreign bodies represent a significant clinical challenge in em
We present a novel application of magnetic-assisted localization in managing a complex case of intentional ingestion of 30 metallic sewing needles in a psy
Magnetic-assisted localization represents an effective and safe technique to manage multiple magnetic gastrointestinal foreign bodies. This approach offers significant advantages in complex cases, particularly for needle-like metallic objects, and warrants consideration as a valuable tool in gastrointestinal surgery.
Core Tip: In cases involving the ingestion of multiple scattered magnetic needle-like foreign bodies in the digestive tract, cylindrical magnetic rods can be utilized to explore physiological bends or narrow areas prone to obstruction, facilitating precise localization and removal of the foreign bodies.
- Citation: Liu SQ, Li YF, Quan DW, Liu W. Magnetic-assisted detection and extraction of dispersed metallic foreign bodies in the abdominal cavity: A case report. World J Gastrointest Surg 2025; 17(5): 101414
- URL: https://www.wjgnet.com/1948-9366/full/v17/i5/101414.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i5.101414
Gastrointestinal foreign bodies are frequently encountered in emergency and gastrointestinal surgery departments. While accidental ingestion is more common among healthy adults, intentional ingestion is often observed in infants, psychiatric patients, and prisoners. Metallic sewing needles, due to their slender, sharp, and highly penetrative nature, pose a significant risk of migration and organ damage caused by gastrointestinal motility. Although preoperative imaging can assist in locating foreign bodies, needle migration—particularly in cases involving multiple needles—complicates treatment and increases clinical risks.
This report describes a rare case of a psychiatric patient who ingested 30 metallic sewing needles of varying lengths and sizes, dispersed throughout the gastrointestinal tract. The large quantity and widespread distribution of the needles rendered intraoperative retrieval particularly challenging. To ensure accurate localization and complete removal, cylindrical magnetic-assisted positioning technology was utilized during surgery, successfully extracting all foreign bodies. This article highlights the clinical approach and treatment experience associated with this unusual case, offering valuable insights into the management of similar high-risk scenarios.
A 55-year-old woman presented with upper abdominal pain following the ingestion of foreign objects.
The patient reported swallowing metallic sewing needles 5 days prior but was unable to specify the exact number. She experienced intermittent upper abdominal pain, accompanied by nausea, vomiting, and melena. The vomitus consisted primarily of gastric contents, without regurgitation or belching. She denied symptoms such as fever, diarrhea, or jaundice.
Past medical history included visual impairment, with the patient being blind in the left eye and only having light perception in the right eye. Information provided by family members showed that the patient had a history of depression and anxiety for nearly 10 years, but had not received standardized psychological treatment.
No significant clinical findings were reported.
The patient had stable vital signs, a symmetrical and flat abdomen, and no visible peristaltic waves. The abdomen was soft with tenderness but without rebound tenderness, and no palpable masses were detected. Bowel sounds were decreased and absent in some areas.
Laboratory tests did not reveal a significant inflammatory response.
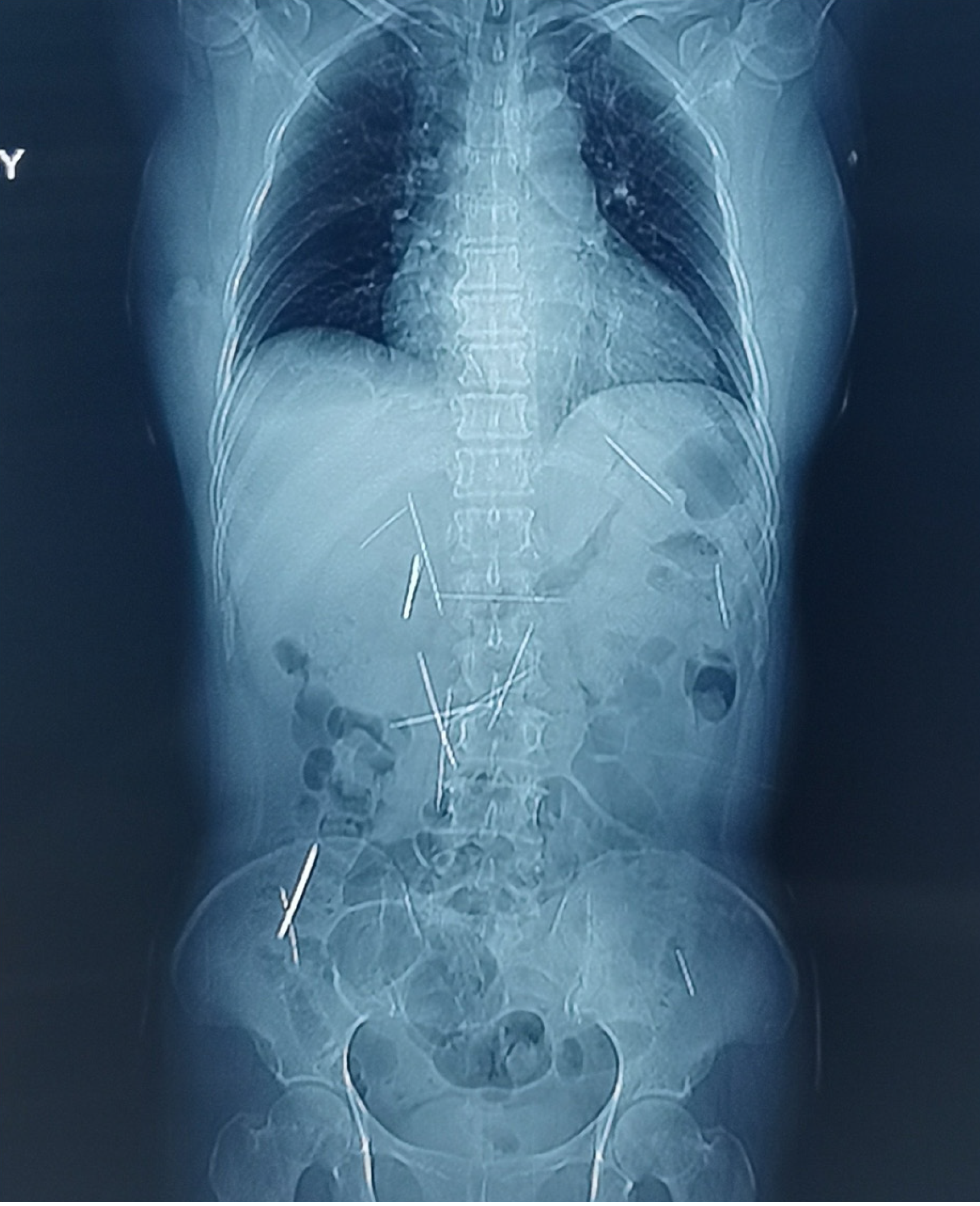
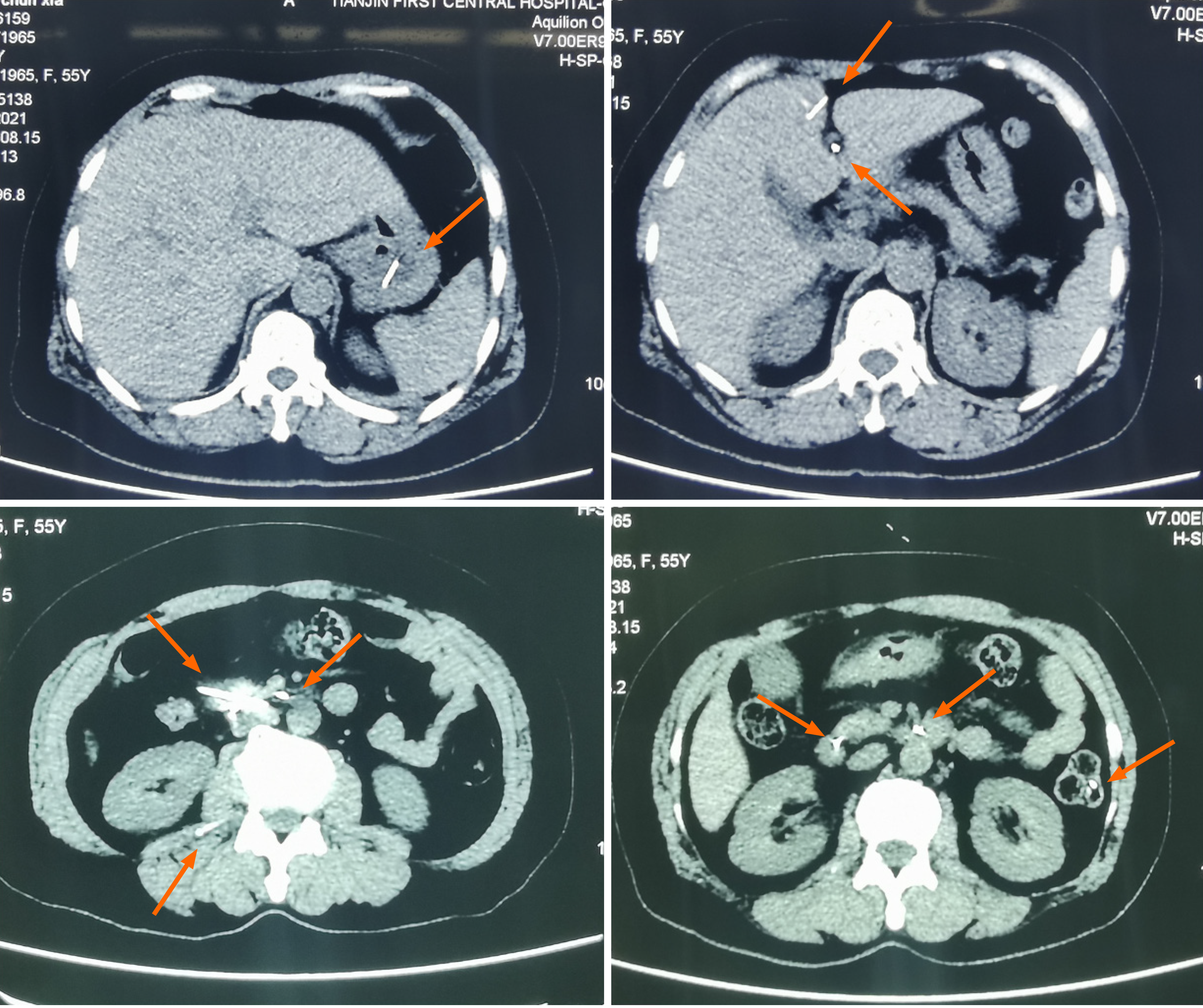
Four days after foreign body ingestion, an upright abdominal X-ray revealed multiple high-density metallic foreign bodies in the abdomen. A subsequent chest X-ray showed no obvious abnormalities. A repeat upright abdominal X-ray (Figure 1) displayed numerous scattered high-density metallic sewing needles in the abdominal cavity. Abdominal computed tomography (CT) scanning and three-dimensional localization confirmed that some needle-like objects had penetrated the gastrointestinal wall into the peritoneal cavity (Figure 2). Since the onset of symptoms, the patient had experienced poor mental status and sleep quality, decreased appetite, but normal urination, with no significant weight change.
Foreign bodes distributed throughout the entire digestive tract.
Comprehensive preoperative evaluations were conducted, revealing no surgical contraindications. Preoperative imaging indicated an uncertain number and widespread distribution of metallic sewing needles within the gastrointestinal tract, complicating intraoperative localization. A cylindrical neodymium-iron-boron magnet, (20 cm in height, 1 cm in diameter) was selected for magnetic-assisted localization. The magnet was sterilized using high-pressure steam prior to surgery.
Under general anesthesia, a midline abdominal incision was made. Referring to preoperative imaging examination for the location of the needle-like foreign bodies, systematic exploration of the abdominal cavity was conducted in a sequential manner.
Initial exploration revealed a metallic needle, approximately 4 cm in length, lodged between the liver and stomach ligaments. The needle was carefully removed, and hemostasis was achieved on the liver surface. A second metallic needle, also approximately 4 cm in length, was found penetrating the greater curvature of the stomach into the liver. After extraction, the gastric wall was closed with full-thickness sutures.
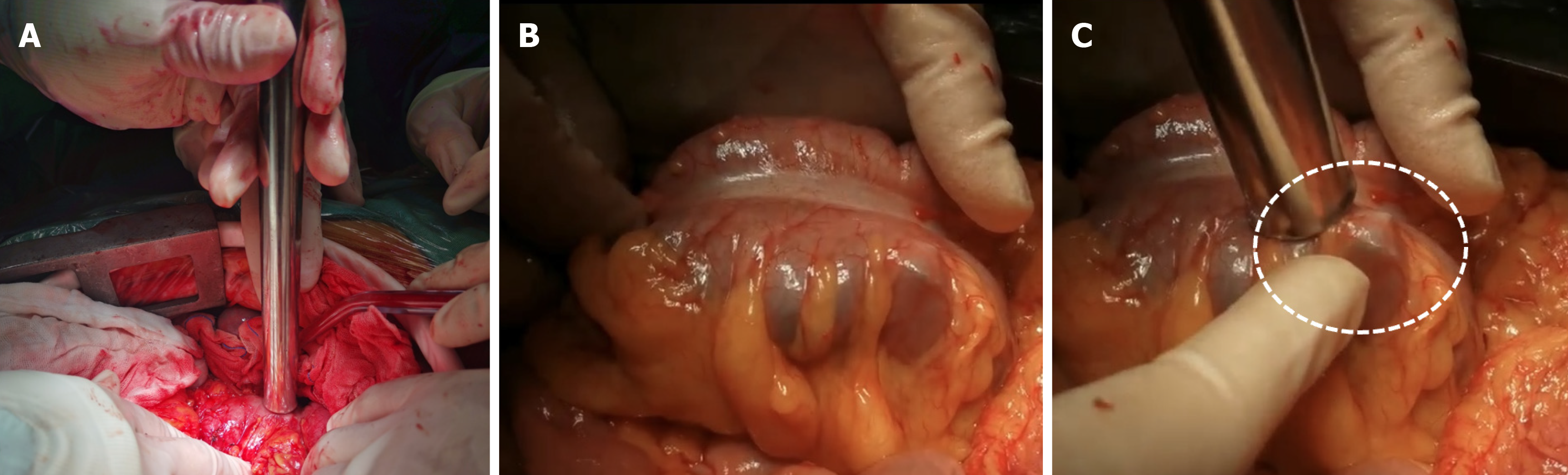
Further dissection and exposure of the duodenum identified four metallic needles protruding from the descending portion of the duodenum, with two oriented toward the abdominal side and two toward the posterior side, penetrating the peritoneum. All four needles were cautiously removed. A cylindrical magnet was then utilized to explore the duodenal descending portion and junction with the horizontal portion. Slight bulging of the intestinal wall near the magnet indicated the presence of metallic needles. Two additional needles were extracted from the original perforation site and the two perforation sites, which were subsequently sutured and reinforced.
The cylindrical magnet was further employed to explore the gastric body, revealing several metallic needles that had not caused perforation. Six metallic needles were identified exiting the anterior wall of the stomach, away from blood vessels. All puncture sites were closed with full-thickness sutures and reinforced.
Exploration of the small intestine using the cylindrical magnet revealed no significant bulging or tension in the intestinal wall. Attention was then directed to the colon (Figure 3), where multiple metallic needles were identified in the cecum and ascending colon. Ten needles were removed from the hepatic flexure of the ascending colon, and the perforations were sutured using the same technique. Further exploration of the colon identified one metallic needle at the junction of the descending colon and sigmoid colon, which was removed, and the perforation sutured.
Following complete exploration of the pelvic cavity, intraoperative C-arm X-ray imaging was performed to identify any missed metallic foreign bodies. High-density shadows were detected at the lower end of the esophagus, upper abdomen midline, left upper abdomen, right upper abdomen, and right lower abdomen. These areas were meticulously explored using the cylindrical magnet, resulting in the extraction of five additional needles from the lower esophagus, horizontal segment of the duodenum, hepatic flexure of the colon, splenic flexure of the colon, and cecum. Repeat C-arm imaging confirmed the absence of any remaining metallic foreign bodies in the chest, abdomen, or pelvis.
The abdominal cavity was irrigated, and hemostasis was confirmed. All gastrointestinal incisions were re-examined to ensure precise closure and intestinal patency. The procedure was successfully completed in 3 hours and 15 minutes, with an estimated blood loss of 30 mL. A total of 30 metallic needles were removed (Figure 4).
Enteral nutrition was initiated on postoperative day 5, and the patient was discharged 10 days after surgery. After a follow-up period of 3 years and 8 months, the patient remains in good health, with no surgery-related complications.
The epidemiology of gastrointestinal foreign bodies exhibits significant geographic and demographic variations, with needle ingestion representing a particularly rare clinical entity. The clinical manifestations and complications associated with such foreign bodies are influenced by multiple factors, including their physical properties, chemical composition, and duration of retention duration. Specific patient populations, particularly those with psychiatric comorbidities or developmental disorders, demonstrate distinct clinical presentations[1-3]. While metallic needle ingestion is uncommon compared to other sharp objects (e.g., fish bones), it carries substantial risk of severe complications[4,5]. Pediatric cases typically result from accidental ingestion, whereas adolescent and adult cases often correlate with underlying psychiatric conditions.
Current diagnostic modalities primarily include radiographic imaging, CT, and endoscopy. Radiography remains the first-line diagnostic tool, though CT provides superior spatial resolution for precise localization. Notably, magnetic resonance imaging is contraindicated due to potential ferromagnetic displacement risks. Contemporary management strategies achieve successful non-surgical removal in 90%-95% of cases through spontaneous passage or endoscopic intervention[6-10]. Surgical management is reserved for cases refractory to conservative approaches or those presenting with complications.
The management of multiple needle foreign bodies presents unique challenges due to their widespread distribution and potential for transmural migration. Our magnetic localization technique capitalizes on the ferromagnetic properties of metallic needles, allowing for precise intraoperative identification through characteristic intestinal wall protrusion upon magnetic approximation. This approach requires meticulous technique to prevent iatrogenic injury during ex
Intraoperative endoscopy (including gastroscopy and colonoscopy) assistance provides multiple advantages beyond diagnostic confirmation, including real-time monitoring, complication assessment, and minimally invasive extraction capabilities[11]. The integration of endoscopic techniques with traditional surgical approaches has been shown to reduce operative morbidity while maintaining high success rates[12,13].
The present case illustrates several critical considerations in managing multiple metallic foreign bodies. The patient’s psychiatric history and the sheer volume of ingested needles (n = 30) represent an exceptionally rare clinical scenario. The needles’ distribution throughout the gastrointestinal tract, coupled with their sharp morphology, created substantial risk of perforation and adjacent organ injury. Preoperative imaging, while essential for initial localization, was limited by metallic artifact and needle superposition, underscoring the need for advanced intraoperative localization techniques.
Current guidelines emphasize that foreign body impaction typically occurs at anatomical narrowings or angulations, with sharp objects posing particular perforation risks[14]. In our case, intraoperative findings confirmed this pattern, with > 70% of needles located at high-risk anatomical sites. Notably, the absence of radiographic pneumoperitoneum did not exclude perforation, likely due to the self-sealing nature of small-caliber needle punctures.
The implementation of magnetic-assisted localization addressed several critical challenges: (1) Real-time dynamic tracking of mobile foreign bodies; (2) Minimization of gastrointestinal incisions through transmural magnetic attraction; (3) Reduction of radiation exposure compared to fluoroscopic guidance; and (4) Enhanced surgical precision and safety.
While magnetic localization has been described in other surgical contexts[15,16], the application thereof to multiple gastrointestinal needle foreign bodies represents a novel advancement. Previous reports have demonstrated the utility of magnetic techniques in pediatric cases[17,18] and airway management[19], while others have highlighted its advantages in extremity foreign body removal[20]. The compass-assisted detection method described by Liu et al[21] shares con
Technical considerations include the use of non-ferromagnetic surgical instruments to minimize interference[22-24]. The integration of magnetic localization with minimally invasive principles offers multiple benefits: reduced operative time; minimized tissue trauma; enhanced postoperative recovery; and improved clinical outcomes.
This case demonstrates that magnetic-assisted localization represents a significant advancement in the management of multiple gastrointestinal metallic foreign bodies. The technique’s safety profile, combined with its technical advantages, suggests its potential as a standard approach in similar challenging cases. Future studies should focus on optimizing magnetic parameters and developing specialized instrumentation to further enhance the efficacy and safety of this promising technique.
For patients with a significant number of ingested magnetic gastrointestinal foreign bodies, traditional imaging techniques may be insufficient for accurate localization. Intraoperative magnetic-assisted exploration enhances the efficiency of foreign body extraction and minimizes risk. Prompt surgical intervention is essential to prevent further damage to vital organs.
We sincerely thank the Northwest Institute for Nonferrous Metal Research for their support in processing the Nv-Fe-P material and manufacturing the intraoperative magnetic-assisted equipment. We also extend our gratitude to the staff of the Medical Record Information Management Department for their valuable assistance.
| 1. | Li ZS, Sun ZX, Zou DW, Xu GM, Wu RP, Liao Z. Endoscopic management of foreign bodies in the upper-GI tract: experience with 1088 cases in China. Gastrointest Endosc. 2006;64:485-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 162] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 2. | Magalhães-Costa P, Carvalho L, Rodrigues JP, Túlio MA, Marques S, Carmo J, Bispo M, Chagas C. Endoscopic Management of Foreign Bodies in the Upper Gastrointestinal Tract: An Evidence-Based Review Article. GE Port J Gastroenterol. 2016;23:142-152. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | Guelfguat M, Kaplinskiy V, Reddy SH, DiPoce J. Clinical guidelines for imaging and reporting ingested foreign bodies. AJR Am J Roentgenol. 2014;203:37-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 103] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 4. | Liu S, Li Q, Li Y, Lv Y, Niu J, Xu Q, Zhao J, Chen Y, Wang D, Bai R. Ileocecal junction perforation caused by a sewing needle in incarcerated inguinal hernia: An unusual case report. Medicine (Baltimore). 2018;97:e10787. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Pante L, Brito LG, Franciscatto M, Brambilla E, Soldera J. A rare cause of acute abdomen after a Good Friday. World J Clin Cases. 2022;10:9539-9541. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | ASGE Standards of Practice Committee; Ikenberry SO, Jue TL, Anderson MA, Appalaneni V, Banerjee S, Ben-Menachem T, Decker GA, Fanelli RD, Fisher LR, Fukami N, Harrison ME, Jain R, Khan KM, Krinsky ML, Maple JT, Sharaf R, Strohmeyer L, Dominitz JA. Management of ingested foreign bodies and food impactions. Gastrointest Endosc. 2011;73:1085-1091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 468] [Cited by in RCA: 540] [Article Influence: 36.0] [Reference Citation Analysis (1)] |
| 7. | Ambe P, Weber SA, Schauer M, Knoefel WT. Swallowed foreign bodies in adults. Dtsch Arztebl Int. 2012;109:869-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 138] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 8. | Birk M, Bauerfeind P, Deprez PH, Häfner M, Hartmann D, Hassan C, Hucl T, Lesur G, Aabakken L, Meining A. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:489-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 439] [Article Influence: 43.9] [Reference Citation Analysis (0)] |
| 9. | Kyaw MH, Chan FKL. Managing Antithrombotic Agents in the Setting of Acute Gastrointestinal Bleeding. Gastrointest Endosc Clin N Am. 2018;28:351-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Tambakis G, Schildkraut T, Delaney I, Gilmore R, Loebenstein M, Taylor A, Holt B, Tsoi EH, Cameron G, Demediuk B, Miller A, Connell W, Wright E, Thompson A, Holmes J. Management of foreign body ingestion in adults: Time to STOP and rethink endoscopy. Endosc Int Open. 2023;11:E1161-E1167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 11. | Quintero RP, Esteban MB, de Lucas DJ, Navarro FM. The utility of intraoperative endoscopy in esophagogastric surgery. Cir Esp (Engl Ed). 2023;101:712-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 12. | Borgogni R, Gaiani F, Di Mario F, Fornaroli F, Leandro G, Bizzarri B, Ghiselli A, De' Angelis GL, Casolari E. Usefulness of intraoperative endoscopy in pediatric surgery: state of the art. Acta Biomed. 2018;89:77-81. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 13. | Schulz HJ, Schmidt H. Intraoperative enteroscopy. Gastrointest Endosc Clin N Am. 2009;19:371-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 14. | Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, Mallery JS, Raddawi HM, Vargo JJ 2nd, Waring JP, Fanelli RD, Wheeler-Harbough J; American Society for Gastrointestinal Endoscopy. Guideline for the management of ingested foreign bodies. Gastrointest Endosc. 2002;55:802-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 399] [Cited by in RCA: 368] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 15. | Prasad R, Amstutz HC, Sparling EA. Use of a magnet to retrieve a broken scalpel blade. J Arthroplasty. 2000;15:806-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Kandioler-Eckersberger D, Niederle B, Herbst F, Wenzl E. A magnetic probe to retrieve broken metallic parts of instruments during laparoscopic procedures. Surg Endosc. 2002;16:208-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Choe JY, Choe BH. Foreign Body Removal in Children Using Foley Catheter or Magnet Tube from Gastrointestinal Tract. Pediatr Gastroenterol Hepatol Nutr. 2019;22:132-141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Volle E, Hanel D, Beyer P, Kaufmann HJ. Ingested foreign bodies: removal by magnet. Radiology. 1986;160:407-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 19] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Sarafi M, Rouzrokh M, Sadr S, Mahdavi SA, Mahdavi NS, Ebrahimian M. The usage of a magnet-powered instrument in the extraction of metallic or magnetic aspirated foreign bodies: A case report. Int J Surg Case Rep. 2022;99:107629. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 20. | Sarıhan A, Can C. Soft tissue foreign body removal with magnet in ED settings. Am J Emerg Med. 2014;32:952.e3-952.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Liu S, Li J, Lv Y. Gastrointestinal damage caused by swallowing multiple magnets. Front Med. 2012;6:280-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Cakir B, Akan M, Yildirim S, Aköz T. Localization and removal of ferromagnetic foreign bodies by magnet. Ann Plast Surg. 2002;49:541-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Feofilov RN, Chirkov VK, Levin MV. [Use of titanium alloys for medical instruments]. Med Tekh. 1977;50-55. [PubMed] |
| 24. | Ho HS. Safety of metallic implants in magnetic resonance imaging. J Magn Reson Imaging. 2001;14:472-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 42] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/