Published online Apr 27, 2025. doi: 10.4240/wjgs.v17.i4.100848
Revised: February 8, 2025
Accepted: March 10, 2025
Published online: April 27, 2025
Processing time: 105 Days and 21.1 Hours
Radical gastrectomy (RGE) for gastric carcinoma (GC) has exerted definite therapeutic efficacy in treating patients with GC. However, a notable risk of post
To analyze the association of multi-channel continuous nursing intervention with POCs, negative emotions (NEs), and quality of life (QoL) of patients undergoing RGE for GC.
This retrospective study selected 99 patients who underwent RGE for GC in our hospital from May 2020 to May 2023. Participants were categorized into the control (n = 49 cases) and research groups (n = 50 cases) receiving routine and multi-channel continuous nursing care, respectively. Comparative analysis involved data on postoperative rehabilitation (time to first anal exhaust, oral feeding and ambulation, and hospital stay), complications (nausea and vomiting, delayed gastric emptying, and abdominal distension), NEs [Self-rating Anxiety (SAS)/Depression Scale (SDS)], treatment compliance, self-efficacy, and QoL [World Health Organization QoL Brief Version (WHOQOL-BREF)].
Compared to the control group, the research group demonstrated earlier first postoperative anal exhaust, oral feeding, and ambulation, shorter hospital stay, lower POC rate, and more reduced SAS and SDS scores postintervention, which was significantly lower than the baseline. The treatment compliance scores were significantly higher in the research group than in the control group in terms of medication adherence, daily exercise, reasonable diet, and regular review. Further, the research group demonstrated increased self-efficacy scores in terms of positive attitude, self-stress relief, and self-decision-making, as well as the overall score postintervention, which were higher than the control group. Moreover, the research group reported notably higher WHOQOL-BREF scores in domains such as physiology, psychology, social relations, and environment.
Multi-channel continuous nursing intervention prevents POCs in patients undergoing RGE for GC as well as significantly alleviates patients’ NEs and boosts their QoL.
Core Tip: This study enrolled 99 patients who underwent radical gastrectomy (RGE) for gastric carcinoma (GC). A comprehensive analysis involved the clinical advantages of multi-channel continuous nursing intervention from multiple dimensions, including postoperative rehabilitation, complications, negative emotions, treatment compliance, self-efficacy, and quality of life. Our data support that the application of multi-channel continuous nursing intervention in patients post-RGE effectively facilitates postoperative recovery, reduces the risk of postoperative complications, alleviates negative psychological states, and significantly improves treatment compliance, self-efficacy, and the overall quality of life. The results provide effective measures and recommendations for treating patients post-RGE for GC. Moreover, it is considered a reference for providing more optimal nursing care alternatives in the postoperative nursing interventions for such patients, thereby contributing to overall quality of care and patient outcome improvements.
- Citation: Luo HL, Luo HL. Analysis of the effect of multi-channel continuous nursing intervention on patients post-radical gastrectomy. World J Gastrointest Surg 2025; 17(4): 100848
- URL: https://www.wjgnet.com/1948-9366/full/v17/i4/100848.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i4.100848
Gastric carcinoma (GC) is a gastrointestinal tumor that originates from the cardia or more distant gastric region, pathogenically caused by Helicobacter pylori infection, dietary habits, family history, alcohol abuse, smoking, genetic susceptibility, etc.[1,2]. Relevant epidemiological data indicated that the disease afflicted over 1.08 million individuals globally in 2020 and caused approximately 800000 deaths, with large geographical differences in the age-standardized incidence and mortality rates of GC worldwide[3,4]. At present, radical gastrectomy (RGE), perioperative chemotherapy, adjuvant chemotherapy, and adjuvant chemoradiotherapy are the primary treatment strategies for GC, among which RGE exerts a high advantage in reducing the risk of GC-related mortality[5]. This treatment demonstrates a certain effectiveness; however, it carries a certain risk of postoperative complications (POCs), especially among middle-aged and elderly patients with functional decline[6,7]. This may inevitably result in negative emotions (NEs) in patients, affecting their treatment outcomes and quality of life (QoL)[8]. Given this, providing a reliable nursing intervention is important for preventing POCs in patients with RGE, alleviating NEs, and boosting QoL.
The nursing service provided by routine nursing is basic but has difficulty playing a significant role in promoting postoperative rehabilitation or matching the increasing health requirements of patients[9]. Conversely, multi-channel continuous nursing intervention is a care mode that primarily provides diet, work and rest, psychology, rehabilitation, cognition, and other services for discharged patients. It provides multi-channel services for patients with the help of network platforms in addition to health education, telephone interviews, re-examination, etc.[10]. This model not only makes it easy to grasp patients’ physical conditions and potential problems but also helps nurses respond appropriately to the patient’s condition promptly to prevent symptoms from worsening[11,12]. Fan et al[13] revealed that multi-channel continuous nursing intervention effectively helped patients with GC to achieve symptom management and timely improved their postoperative gastrointestinal function and QoL. Besides the application in patients with GC, this care model has been applied to patients undergoing glioma surgery and those elderly with rectal cancer, demonstrating advantages in NE relief; QoL, self-efficacy, and sleep quality improvement; and POC prevention[14,15].
This report assumes that multi-channel continuous nursing intervention exerts a significant positive effect on POC and NE prevention and QoL improvement in patients with GC post-RGE, and is hereby analyzed, verified, and reported.
This retrospective study included 99 patients undergoing RGE for GC in our hospital from May 2020 to May 2023. The control group (Con; n = 49) received routine care, whereas the research group (Res; n = 50) received multi-channel continuous nursing interventions. The Con and Res demonstrated clinical comparability with no notable difference in baseline data.
Eligibility criteria: All patients were diagnosed with GC, underwent laparoscopic-assisted RGE, and met the Nutritional Risk Screening (NRS2002) criteria[16], with complete medical records. Further, patients had normal communication and cognitive abilities and agreed to cooperate with the study.
Exclusion criteria: Hospital referrals or patients who gave up treatment, with surgical contraindications, complicated with serious cardio-cerebrovascular diseases or renal dysfunction, suffering from coagulation dysfunction or autoimmune system defects, and with other malignancies.
Routine continuous nursing measures were implemented in the Con. Specific contents: According to the patient’s situation, the patient and his/her family received routine health education, including specific medication, diet rules, points for attention in activities and rest, and specific return visit times. Further, the patient’s daily exercise and dietary regimen was made into a detailed publicity material, which was distributed to the patient upon discharge. Telephone follow-ups were conducted at least twice a month within 3 months postoperatively.
The Res received multi-channel continuous nursing intervention, specifically the following: (1) Setting up a continuous nursing service group. The head nurse and attending physician were appointed as the team leaders, whereas the team members were composed of five specialist nurses, all of whom had more than 3 years of working experience. All team members received special training to master the relevant knowledge and skills post-RGE, with good communication skills and service awareness to proactively provide help to patients; (2) Mobile platform intervention. The network platform was utilized to conduct continuous nursing care for patients. The nursing staff fully used the flexibility of the network platform and the WeChat public account as well as established a WeChat group and let patients enter the group by scanning the QR code. Attending doctors and responsible nurses answered patients’ doubts online daily in the WeChat group and encouraged patients to express their condition every day as well as their experiences and feelings to meet their social needs and achieve mutual communication and mutual encouragement. Furthermore, the predominant problems were sorted out, relevant treatment measures were recommended through the public account, and the specific self-care methods were uploaded to the WeChat official account so that patients could inquire at any time. Moreover, regular diet and exercise were recommended to improve patients’ cognitive levels and compliance; and (3) Life guidance. The nursing staff strengthened the relevant health knowledge post-RGE and established a targeted health explanation program based on the complicated psychological changes of patients. Besides, the importance of a reasonable diet was emphasized to the patients, namely, avoiding spicy stimulation, eating more low-fat foods, ensuring a diverse diet, guaranteeing balanced nutrition intake, reducing salt intake, and encourage encouraging drinking water. For those with a history of smoking and drinking, the importance of quitting smoking and drinking was highlighted for those with a smoking and drinking history, and the family members were encouraged to supervise and give provide patients support.
Postoperative rehabilitation: The time to first postoperative anal exhaust, oral feeding, and ambulation, and the hospital stay of both groups were observed and documented.
POCs: Cases of adverse events, such as nausea and vomiting, delayed gastric emptying, and abdominal distension, were observed and recorded, and the incidence rate was calculated.
Nes: We utilized the Self-rating Anxiety Scale (SAS)/Self-rating Depression Scale (SDS)[17] to assess patients’ anxiety and depression pre- and postintervention. Both scales have 20 items and a total score of 80 points, with higher scores indicating more serious NEs.
Treatment compliance: Based on the self-made treatment compliance questionnaire for postoperative patients with GC developed by our hospital, patients were assessed for treatment compliance in terms of medication adherence, daily exercise, reasonable diet, and regular review. Each dimension has a maximum score of 20 points, and the score is directly proportional to treatment compliance.
Self-efficacy: The patients’ self-efficacy pre- and postintervention was assessed based on the General Self-Efficacy Scale[18], including positive attitude, self-stress relief, and self-decision-making. The total score ranges from 28 to 140 points, with the score positively related to self-efficacy.
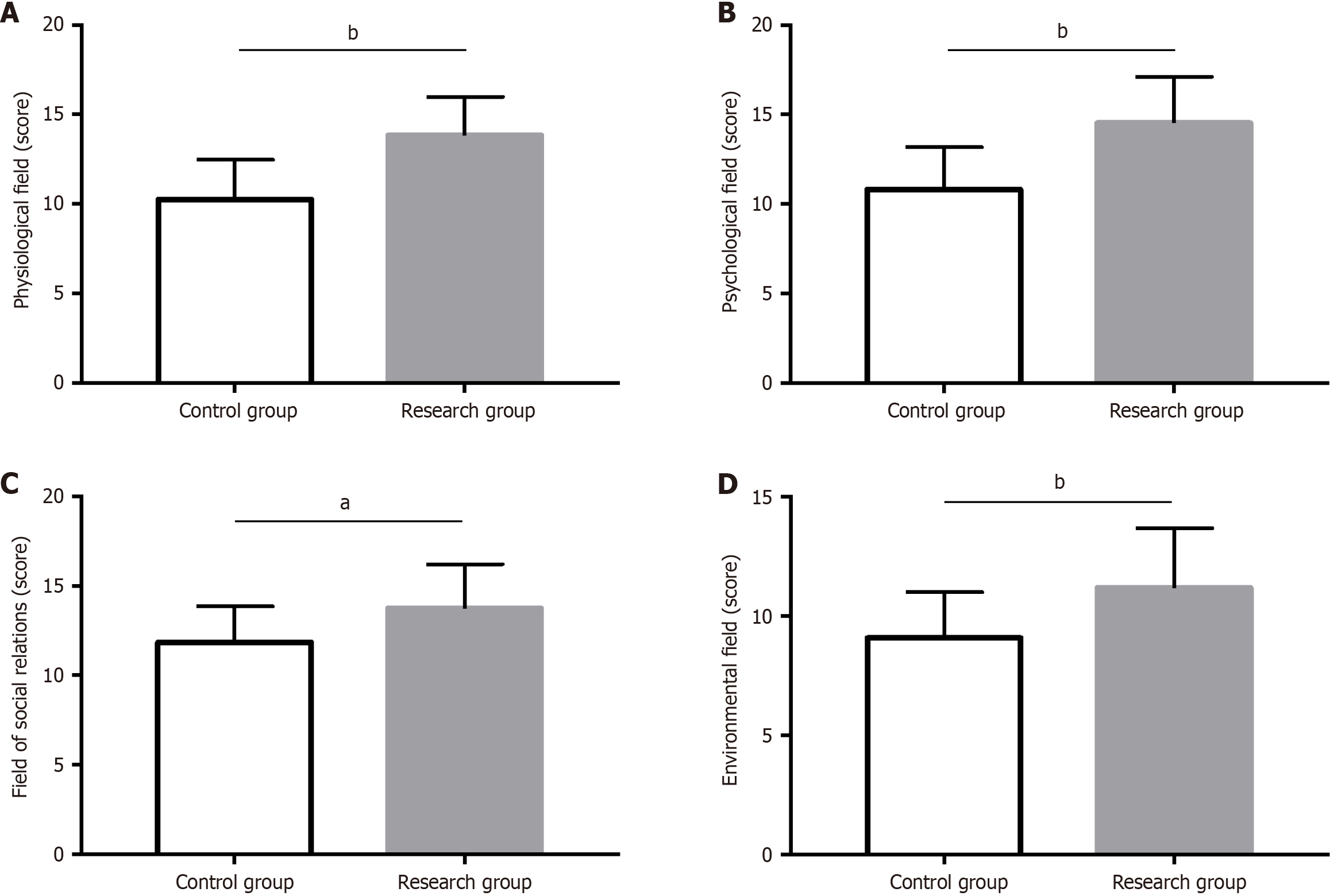
QoL: Patients’ QoL was evaluated with the World Health Organization QoL Brief Version (WHOQOL-BREF)[19], which primarily included 26 items in the fields of physiology, psychology, social relations, and environment. Each item was recorded with 1-5 points, and a higher score indicated a better QoL in each field.
In this study, both continuous (mean ± SE) and categorical [number of cases/percentage (n/%)] variables were imported into Statistical Package for the Social Sciences version 19.0 for statistical analyses. Among them, the χ2 test was utilized to compare categorical variables, and the independent sample t-test was used to compare continuous variables between groups. P values of < 0.05 indicated statistical significance.
Baseline data analysis revealed no obvious inter-group differences in terms of age, gender, body mass index, NRS2002, diabetes, hypertension, and hyperlipidemia (P > 0.05; Table 1).
| Classification | Control group (n = 49) | Research group (n = 50) | χ2/t | P value |
| Age (years) | 62.53 ± 5.56 | 64.32 ± 7.31 | 1.369 | 0.174 |
| Gender | 0.845 | 0.358 | ||
| Male | 30 (61.22) | 35 (70.00) | ||
| Female | 19 (38.78) | 15 (30.00) | ||
| Body mass index (kg/m2) | 22.18 ± 2.24 | 22.94 ± 2.56 | 1.571 | 0.120 |
| NRS2002 (points) | 3.08 ± 0.76 | 3.14 ± 1.11 | 0.313 | 0.755 |
| Diabetes | 0.260 | 0.610 | ||
| With | 15 (30.61) | 13 (26.00) | ||
| Without | 34 (69.39) | 37 (74.00) | ||
| Hypertension | 0.246 | 0.620 | ||
| With | 18 (36.73) | 16 (32.00) | ||
| Without | 31 (63.27) | 34 (68.00) | ||
| Hyperlipidemia | 0.845 | 0.358 | ||
| With | 19 (38.78) | 15 (30.00) | ||
| Without | 30 (61.22) | 35 (70.00) |
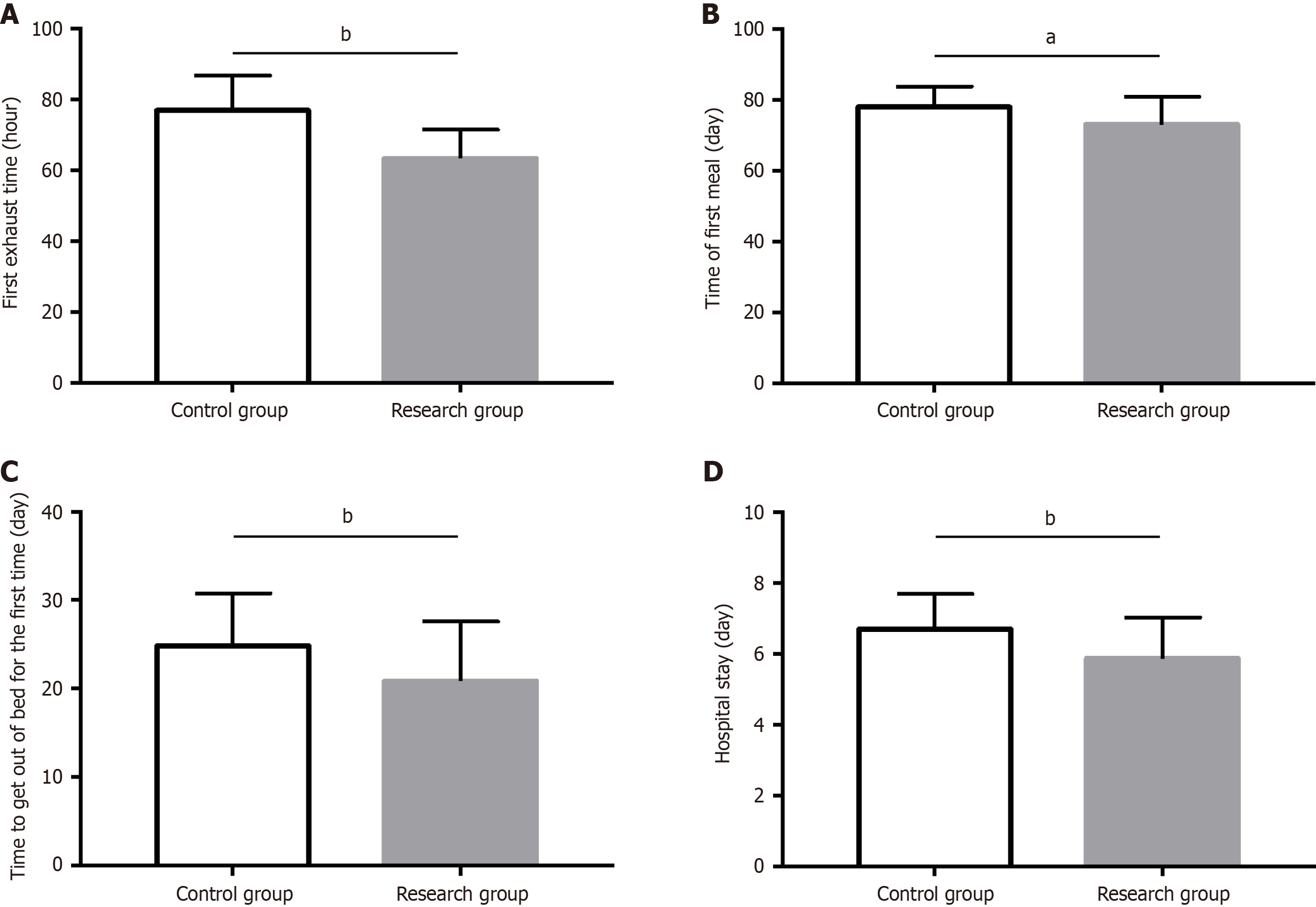
The postoperative rehabilitation assessment revealed that the Res had a markedly shorter time to first anal exhaust, oral feeding, and ambulation, as well as reduced hospital stay than the Con (P < 0.05; Figure 1).
The Con demonstrated a higher incidence of nausea and vomiting, delayed gastric emptying, and abdominal distension than the Res (P < 0.05; Table 2).
| Classification | Control group (n = 49) | Research group (n = 50) | χ2 | P value |
| Nausea and vomiting | 8 (16.33) | 1 (2.00) | ||
| Delayed gastric emptying | 1 (2.04) | 0 (0.00) | ||
| Abdominal distension | 0 (0.00) | 1 (2.00) | ||
| Total | 9 (18.37) | 2 (4.00) | 5.172 | 0.023 |
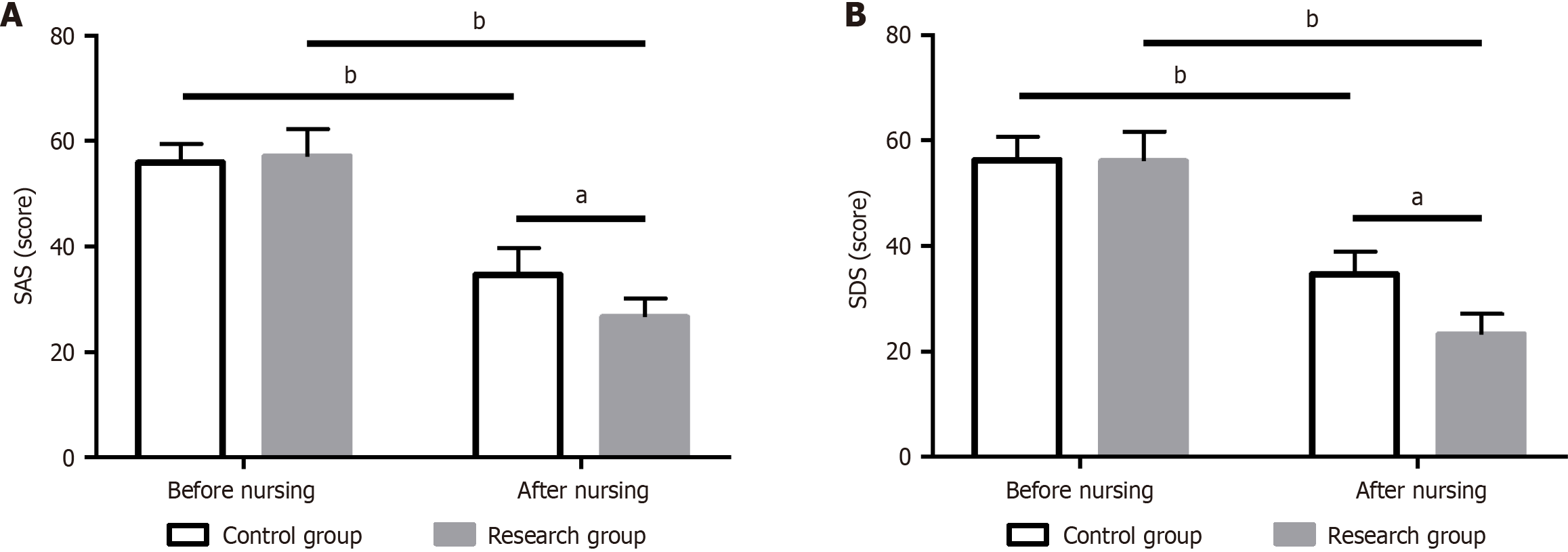
Anxiety and depression assessment revealed no marked inter-group difference in SAS and SDS preintervention (P > 0.05); however, the two scores were significantly reduced after nursing care, with even lower scores in the Res (P < 0.05; Figure 2).
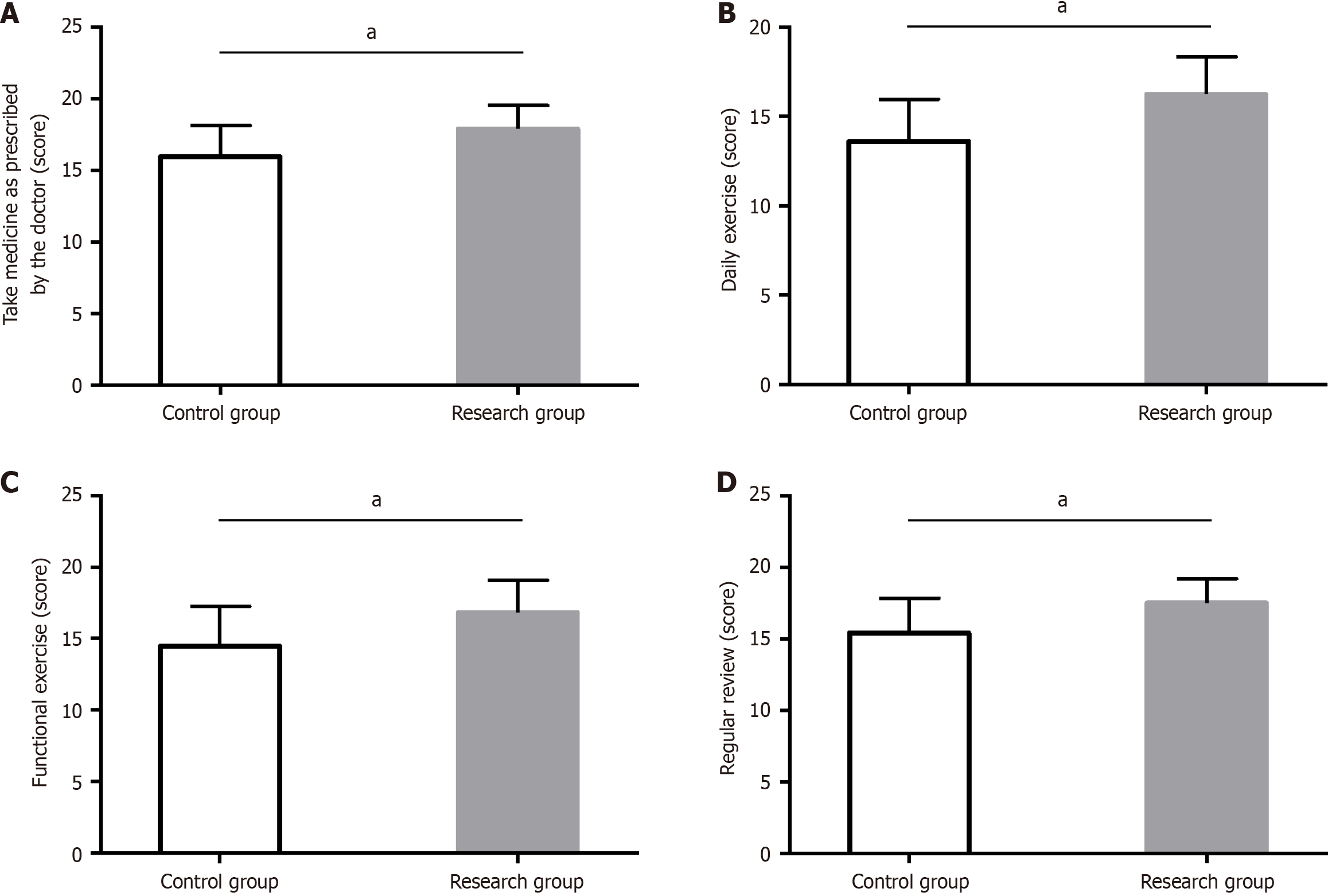
The Res demonstrated significantly higher treatment compliance in domains such as medication adherence, daily exercise, reasonable diet, and regular review, compared to the Con (P < 0.05; Figure 3).
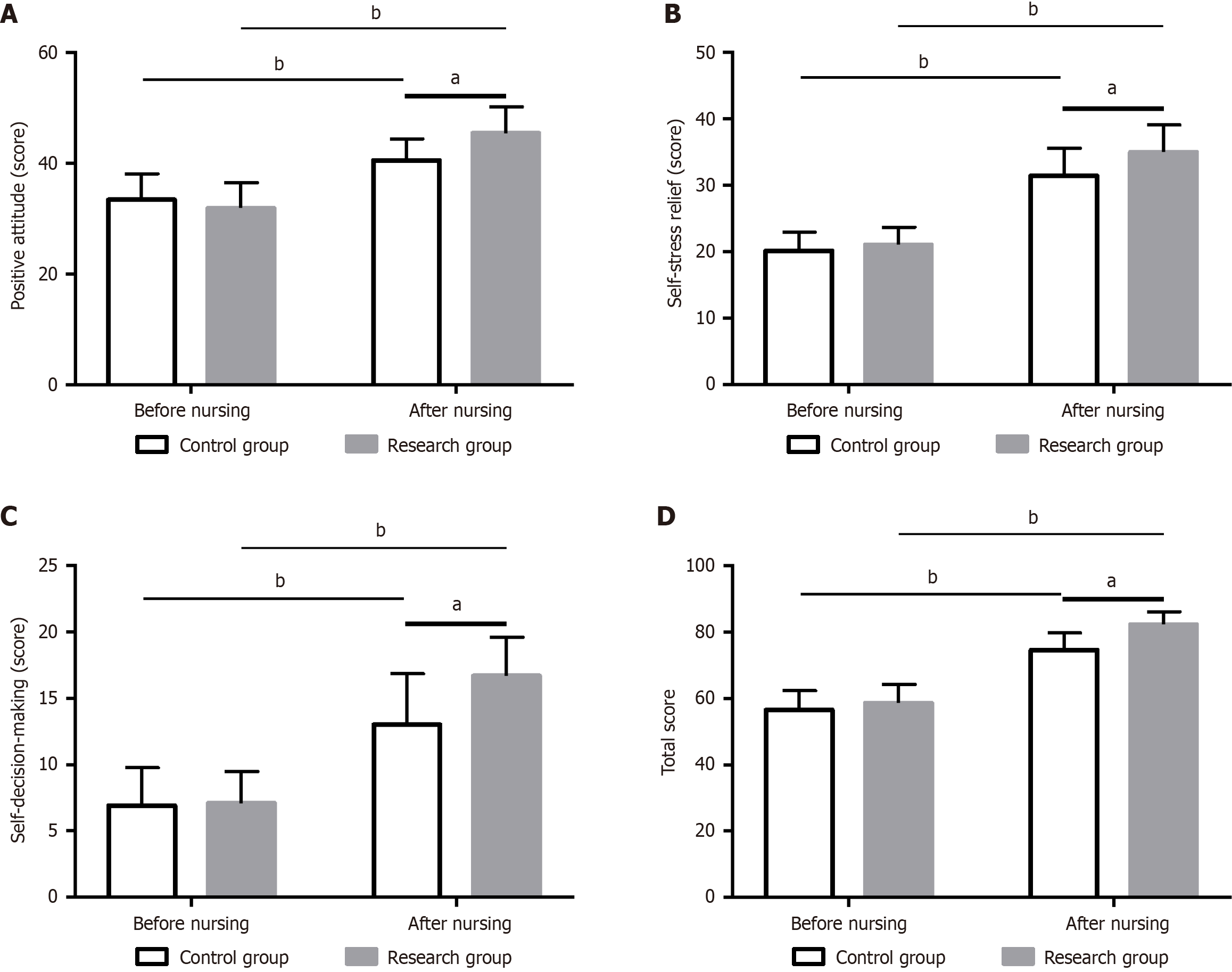
The General Self-Efficacy Scale was utilized to assess the self-efficacy of patients pre- and postintervention. The two groups did not differ much in preinterventional self-efficacy scores in positive attitude, self-stress relief, and self-decision-making domains as well as the total score (P > 0.05). Postintervention, the scores of both groups in all the above aspects significantly increased (P < 0.05), especially in the Res (P < 0.05; Figure 4).
The WHOQOL-BREF scale was utilized to assess patients’ QoL. The data revealed that the study group demonstrated significantly higher QoL scores in physiological, psychological, social relations, and environmental fields than the Con (P < 0.05; Figure 5).
So far, no study has confirmed the positive effects of multi-channel continuous care on POCs, NEs, and QoL of patients post-RGE. This report conducted a relevant analysis to fill this gap and confirm the effectiveness of its application in such patients.
In recent years, RGE has been continuously enhanced to preserve gastric function as much as possible[20]. However, the risk of complications in patients post-RGE remains as high as 25%, which not only impairs their QoL but also negatively affects their survival outcomes[21]. In this study, we first assessed postoperative rehabilitation and revealed that the Res had significant advantages in postoperative rehabilitation, mainly manifested as markedly shortened first postoperative anal exhaust, oral feeding, ambulation, and hospital stay than the Con, indicating the significant role of multi-channel continuous nursing intervention in promoting postoperative rehabilitation in patients with GC post-RGE. Furthermore, the total complication rates of nausea and vomiting, delayed gastric emptying, and abdominal distension were statistically lower in the Res than in the Con, indicating the significant preventive effect of multi-channel continuous nursing intervention against POCs in patients post-RGE. Hu et al[22] demonstrated that the use of multi-channel continuous care in patients undergoing GC surgery not only significantly shortened the time to anal exhaust, defecation, food intake, and bowel sound recovery to promote gastrointestinal recovery but also effectively reduced the risk of POCs, which is consistent with our research findings. Due to the convenience of the online platform, the multi-channel continuous nursing intervention strengthens disease understanding and POC prevention by answering questions online for patients daily, which helps patients achieve effective recovery and prevents some adverse event occurrences to a certain extent. The results of NEs revealed that the SAS and SDS in the Res postintervention were significantly lower than the baseline and the Con, indicating that NEs are significantly alleviated after multi-channel continuous nursing interventions. This may be associated with the humanistic care provided to patients post-RGE in the process of multi-channel continuous nursing intervention, which takes care of patient’s emotions and provides timely psychological counseling while helping them establish a correct disease understanding, thereby aiding in dispelling part of patients’ anxiety and establishing a positive mentality for them to overcome the disease[23,24]. Rui et al[25] revealed that the application of multi-channel continuous nursing intervention to patients with GC effectively reduced the generation of NEs and significantly improved their self-care ability, similar to our research results. We assessed treatment compliance from aspects such as medication adherence, daily exercise, reasonable diet, and regular review. The Res had significant clinical advantages compared to the Con in all the above-mentioned aspects, indicating that multi-channel continuous nursing intervention significantly improves the treatment compliance of patients post-RGE. Fu et al[26] indicated that the application of targeted nursing intervention combined with psychological intervention in patients with GC undergoing chemotherapy improves patients’ mental well-being, promotes healthy behaviors, and enhances treatment compliance, which is similar to our observations. Subsequently, the assessment data on the General Self-Efficacy Scale revealed significantly higher scores of the Res than the Con in terms of positive attitude, self-stress relief, self-decision-making, and the total score postintervention, indicating that the use of multi-channel continuous nursing intervention for patients post-RGE significantly improved their self-efficacy. Yin et al[27] demonstrated that the deployment of a nursing intervention based on the Information-Knowledge-Attitude-Practice model among patients with GC catalyzes the construction of a comprehensive and accurate understanding of the disease and self-management concepts. This, in turn, significantly contributes to the augmentation of patients’ self-management capabilities, which supports the results of our investigation. After QoL assessment, the Res was advantageous over the Con in WHOQOL-BREF scores from the fields of physiology, psychology, social relations, and environment, indicating that multi-channel continuous nursing intervention significantly improves the QoL of patients post-RGE, similar to the research results of Zhang et al[28]. Liu et al[29] revealed that multi-channel continuous nursing intervention not only promoted the long-term functional recovery of elderly patients with hip fractures, relieved NEs, and reduced the risk of POCs, but also exerted a significant positive effect on improving patients’ QoL, which is congruent with our observations. Furthermore, many researchers have dedicated their efforts to the meticulous refinement of the multi-channel continuous nursing intervention experience. For instance, Calton et al[30] postulated that the integration of multi-channel continuous nursing intervention with telemedicine can confer survival advantages upon patients with cancer, including those with GC. This is particularly beneficial for individuals grappling with functional impairments, a high symptom burden, or those facing economic and geographical constraints. Zhang et al[31] introduced the proposition that the combination of multi-channel continuous nursing intervention with smart nursing wheelchairs not only results in a remarkable improvement in the operational efficiency of nursing personnel but also increases the overall quality and experience of nursing care, better meeting the daily needs of elderly patients or those with disabilities.
The possibility and potential advantages of integrating multi-channel extended care with other emerging nursing concepts or technologies are extremely significant and should not be underestimated in the slightest. This integration model not only opens up a new perspective for subsequent studies and expands more diverse research directions but also introduces new vitality to the innovative development of the nursing field. We plan to conduct in-depth research in this regard in the future, actively investigate the best practices of this integration, strive to achieve more significant breakthroughs in the nursing experience, and thus provide patients with higher-quality, more efficient, and personalized nursing services.
Conclusively, multi-channel continuous nursing intervention helps not only facilitate the postoperative rehabilitation of patients post-RGE, but also prevent POCs, relieve anxiety and depression, and improve treatment compliance, self-efficacy, and QoL, which provide effective measures and suggestions for treating patients with GC post-RGE.
| 1. | Han Z, Liu J, Zhang W, Kong Q, Wan M, Lin M, Lin B, Ding Y, Duan M, Li Y, Zuo X, Li Y. Cardia and non-cardia gastric cancer risk associated with Helicobacter pylori in East Asia and the West: A systematic review, meta-analysis, and estimation of population attributable fraction. Helicobacter. 2023;28:e12950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 2. | Yang L, Ying X, Liu S, Lyu G, Xu Z, Zhang X, Li H, Li Q, Wang N, Ji J. Gastric cancer: Epidemiology, risk factors and prevention strategies. Chin J Cancer Res. 2020;32:695-704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 159] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 3. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 68713] [Article Influence: 13742.6] [Reference Citation Analysis (201)] |
| 4. | Thrift AP, El-Serag HB. Burden of Gastric Cancer. Clin Gastroenterol Hepatol. 2020;18:534-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 432] [Cited by in RCA: 1080] [Article Influence: 180.0] [Reference Citation Analysis (7)] |
| 5. | Joshi SS, Badgwell BD. Current treatment and recent progress in gastric cancer. CA Cancer J Clin. 2021;71:264-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 382] [Cited by in RCA: 1194] [Article Influence: 238.8] [Reference Citation Analysis (9)] |
| 6. | Wang S, Xu L, Wang Q, Li J, Bai B, Li Z, Wu X, Yu P, Li X, Yin J. Postoperative complications and prognosis after radical gastrectomy for gastric cancer: a systematic review and meta-analysis of observational studies. World J Surg Oncol. 2019;17:52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 100] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 7. | Guo S, Shang MY, Dong Z, Zhang J, Wang Y, Zheng ZC, Zhao Y. A nomogram for predicting cancer-specific survival in different age groups for operable gastric cancer: a population-based study. Transl Cancer Res. 2020;9:2758-2768. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Rupp SK, Stengel A. Influencing Factors and Effects of Treatment on Quality of Life in Patients With Gastric Cancer-A Systematic Review. Front Psychiatry. 2021;12:656929. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 9. | Jacobsen PB, Lee M. Integrating Psychosocial Care Into Routine Cancer Care. Cancer Control. 2015;22:442-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Yao J, He W, Chen H, Qi Y. Nursing effect of continuous nursing intervention based on "Internet Plus" on patients with severe adrenal tumor. Medicine (Baltimore). 2023;102:e33187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 11. | Colson S, Schwingrouber J, Evans C, Roman C, Bourriquen M, Lucas G, Mellinas M, Brunet P, Cermolacce M, Chinot O, Mayen S, Berbis P. The creation and implementation of advanced practice nursing in France: Experiences from the field. Int Nurs Rev. 2021;68:412-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 12. | Luo L, Wang F, Wang L, Zhang J, Liu X, Wang W. Clinical Efficacy and Psychological Impact of Omaha-Based Continuing Care for Prostate Cancer Patients. Comput Math Methods Med. 2022;2022:8735363. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 13. | Fan L, He Y, Li Y, Li X, Liu D, Wang R. Efficacy and safety of traditional Chinese medicine nursing intervention in postoperative patients after gastrectomy. Oncol Lett. 2023;26:537. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 14. | Deng YH, Yang YM, Ruan J, Mu L, Wang SQ. Effects of nursing care in fast-track surgery on postoperative pain, psychological state, and patient satisfaction with nursing for glioma. World J Clin Cases. 2021;9:5435-5441. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Parker M, Kazemi F, Ahmed AK, Kuo CC, Nair SK, Rincon-Torroella J, Jackson C, Gallia G, Bettegowda C, Weingart J, Brem H, Mukherjee D. Exploring the impact of primary care utilization and health information exchange upon treatment patterns and clinical outcomes of glioblastoma patients. J Neurooncol. 2024;168:345-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 16. | Huang DD, Cai HY, Chen XY, Dong WX, Wangchuk D, Yan JY, Chen XL, Dong QT. Value of Sarcopenia defined by the new EWGSOP2 consensus for the prediction of Postoperative Complications and Long-term Survival after Radical Gastrectomy for Gastric Cancer: A comparison with four common nutritional screening tools. J Cancer. 2020;11:5852-5860. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 17. | Huang H, Guo Z, Li W, Zhang M, Li Y. A comparative study of using linear anastomosis with circular anastomosis in digestive tract reconstruction after laparoscopic radical total gastrectomy: A retrospective study. Medicine (Baltimore). 2023;102:e34588. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Lee MK. Decisional balance, self-leadership, self-efficacy, planning, and stages of change in adopting exercise behaviors in patients with stomach cancer: A cross-sectional study. Eur J Oncol Nurs. 2022;56:102086. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 19. | Soroceanu RP, Timofte DV, Danila R, Timofeiov S, Livadariu R, Miler AA, Ciuntu BM, Drugus D, Checherita LE, Drochioi IC, Ciofu ML, Azoicai D. The Impact of Bariatric Surgery on Quality of Life in Patients with Obesity. J Clin Med. 2023;12:4225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 20. | Nomura E. Postoperative functional evaluation of gastrectomy for gastric cancer. Chin J Cancer Res. 2022;34:567-574. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 21. | Yuan P, Wu Z, Li Z, Bu Z, Wu A, Wu X, Zhang L, Shi J, Ji J. Impact of postoperative major complications on long-term survival after radical resection of gastric cancer. BMC Cancer. 2019;19:833. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 22. | Hu J, Wang LL, Li Y. Effects of high-quality nursing intervention on negative emotions, postoperative complications and gastrointestinal function in patients with gastric cancer surgery. Am J Transl Res. 2022;14:1652-1662. [PubMed] |
| 23. | Porter LS, Keefe FJ, Baucom DH, Hurwitz H, Moser B, Patterson E, Kim HJ. Partner-assisted emotional disclosure for patients with gastrointestinal cancer: results from a randomized controlled trial. Cancer. 2009;115:4326-4338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 111] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 24. | Allum W, Lordick F, Alsina M, Andritsch E, Ba-Ssalamah A, Beishon M, Braga M, Caballero C, Carneiro F, Cassinello F, Dekker JW, Delgado-Bolton R, Haustermans K, Henning G, Hutter B, Lövey J, Netíková IŠ, Obermannová R, Oberst S, Rostoft S, Saarto T, Seufferlein T, Sheth S, Wynter-Blyth V, Costa A, Naredi P. ECCO essential requirements for quality cancer care: Oesophageal and gastric cancer. Crit Rev Oncol Hematol. 2018;122:179-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 25. | Rui A, Xu Q, Yang X. Effect of multidisciplinary cooperative continuous nursing on the depression, anxiety and quality of life in gastric cancer patients. Am J Transl Res. 2021;13:3316-3322. [PubMed] |
| 26. | Fu Y, Li Y, Guo R, Gao Q. Effect of Targeted Nursing Combined with Psychological Intervention on Chemotherapy for Gastric Carcinoma and its Influence on Patient Compliance. Altern Ther Health Med. 2024;AT9577. [PubMed] |
| 27. | Yin L, Zhang W, Liu L, Guo L, Guo M, He X, Zhu L. Application of nursing intervention based on the IKAP model in self-management of patients with gastric cancer. Am J Transl Res. 2022;14:6389-6398. [PubMed] |
| 28. | Zhang X, Yang L, Hou L, Liu J, Zhu H, Zhang J. Effect of a psychological nursing intervention on quality of life and cognitive function in patients with gastric carcinoma: A randomised controlled trial. Eur J Cancer Care (Engl). 2020;29:e13292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 29. | Liu J, Zhao Q, Wang J, Zhang J, Jiang J, Wang H. The effect of continuing care on postoperative life quality and long-term functional recovery in elderly patients with hip fracture. Am J Transl Res. 2021;13:5512-5518. [PubMed] |
| 30. | Calton BA, Nouri S, Davila C, Kotwal A, Zapata C, Bischoff KE. Strategies to Make Telemedicine a Friend, Not a Foe, in the Provision of Accessible and Equitable Cancer Care. Cancers (Basel). 2023;15:5121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 31. | Zhang Z, Xu P, Wu C, Yu H. Smart Nursing Wheelchairs: A New Trend in Assisted Care and the Future of Multifunctional Integration. Biomimetics (Basel). 2024;9:492. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/