Published online Mar 27, 2025. doi: 10.4240/wjgs.v17.i3.99784
Revised: December 25, 2024
Accepted: January 15, 2025
Published online: March 27, 2025
Processing time: 95 Days and 1.6 Hours
Currently, colonoscopy still needs continuous optimization and exploration of novel alternative approaches to enhance the experience of patients during co
To analyze the efficacy of water infusion combined with defoamers in colono
This study included 97 patients undergoing colonoscopy from January 2024 to June 2024. The participants were categorized into two groups, namely, the control group (n = 47), who underwent conventional colonoscopy, and the experimental group (n = 50), who received colonoscopy using water injection combined with defoamers. A comparative analysis was then conducted on the disease detection rate (colonic polyps, colonorrhagia, colonic ulcers, colonic mucosal lesions, and others), colonoscopy duration, abdominal pain [visual analog scale (VAS)], Boston bowel preparation scale (BBPS), self-rating anxiety scale (SAS), bowel preparation comfort, complications (intestinal perforation, bleeding, nausea and vomiting, abdominal pain, and abdominal distension), and patient satisfaction.
The experimental group demonstrated a significantly higher total disease detection rate, BBPS scores, and patient satisfaction compared with the control group. Further, the research group exhibited shorter colonoscopy duration, lower VAS and SAS scores and total complication rate, and better patient comfort and satisfaction.
These results indicate that the combination of water injection and defoamers exhibited an overall better therapeutic effect than conventional colonoscopy, mainly reflected in higher disease detection rate, faster examination ef
Core Tip: Continuous innovation and exploration of new alternative solutions for colonoscopy remain essential to improve patients’ colonoscopy experience. This study proposes the application of the water-infusion method combined with de
- Citation: Li J, Chen JP, Lai CH, Fu L, Ji Y. Efficacy of water infusion combined with defoamers in colonoscopy. World J Gastrointest Surg 2025; 17(3): 99784
- URL: https://www.wjgnet.com/1948-9366/full/v17/i3/99784.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i3.99784
Colonoscopy is intuitive and effective for the clinical assessment of colon polyps, colonorrhagia, colon ulcers, colonic mucosal lesions, and various other intestinal diseases[1,2]. This examination method utilizes a flexible colonoscope with an approximately 1-cm diameter to extend from the patient’s anus into the rectum and then the colon to observe any abnormalities in the colon[3]. Colonoscopy exhibits certain clinical advantages, but it is essentially an invasive procedure that inevitably brings discomfort and adverse experiences to patients[4,5]. Painless endoscopy minimizes patient dis
Conventional colonoscopy with the air insufflation method mainly involves intestinal cavity exposure through air insufflation and using the axial shortening technique to introduce the endoscope, followed by body position changes, abdominal compressions, and other ways to achieve colonoscopy[8,9]. However, this approach induces strong intestinal stimulation, causing discomfort due to colon expansion after inflation, as well as the possibility of subsequent looping that may hinder cecal insertion[10]. The present study proposed water injection combined with defoamers to improve the above situation, considering the currently limited research in this field. Unlike air insufflation, water injection is an intervention that reduces the air injection while taking advantage of the characteristics of the water to flow from the lower colon to the lower position, thereby decreasing the intestinal dilatation and the difficulty of endoscope passage by reducing the sigmoid colon curvature[11,12]. Further, this test is beneficial to reduce the risk of loop formation, greatly shortening the assessment duration and relieving discomfort, including abdominal distension and pain[13]. Defoamers improve visibility during colonoscopy and provide a clearer field of vision during the inspection, thereby minimizing undesirable disturbances (foam or mucus, etc.) in the patient’s body and helping to improve the examination efficiency[14,15]. The defoamers typically used in colonoscopy include simethicone, dimethicone, and dyclonine hydrochloride mucilagines in clinical practice. Notably, simethicone represents a compound of dimethicone and silicon dioxide, with a significantly better defoaming capacity than that of dimethicone. Moreover, it entails a lower usage cost when compared to dyclonine hydrochloride mucilagines[16]. Hence, the present study selected simethicone as the defoaming agent for the clinical analysis.
In this study, we proposed the use of water injection combined with defoamers in colonoscopy and compared it with conventional colonoscopy, to confirm its clinical advantages and provide more options for improving the medical experience of patients undergoing colonoscopy.
This retrospective study included 97 patients undergoing colonoscopy in Nanhai Family Practice Hospital (Nanhai Guicheng Hospital) from January 2024 to June 2024. The participants were categorized into the control group (n = 47), who underwent conventional colonoscopy, and the experimental group (n = 50), who received colonoscopy with water injection and defoamers.
Inclusion criteria: All patients met the colonoscopy indications, with complete medical records and normal under
Exclusion criteria: Patients with a colorectal surgery history, digestive tract obstruction or perforation risk, active gastrointestinal bleeding, severe heart, lung, and kidney dysfunction, psychological illness, or mental disturbance, as well as pregnant women.
All participants were routinely placed in the left lateral decubitus position. Compound tetracaine gel was applied to the anus and the anterior part of the endoscope for local anesthesia and lubrication before the procedure. The same experienced endoscopist single-blindly performed all examinations. Both groups were assessed with ELUXEO 7000 electronic colonoscopy. The control group underwent a conventional colonoscopy, with conventional air as the injected gas. The experimental group underwent colonoscopy with water injection combined with defoamers. The defoamer, simethicone of 10 mL, was placed in a container and added to the warm water of 70 mL (approximately 40 °C) to prepare a unit of 80-mL solution after repeated stirring. The patient was instructed to administer it orally 20 minutes preoperatively. Posture rotation was then performed in the following order: (1) Supine position; (2) Left lateral position; (3) Prone position; and (4) Right lateral position, with each posture maintained for 5 minutes. Upper abdomen massage was then performed simultaneously. The endoscope special flushing pump was disinfected and placed in warm water controlled at 37 °C. The water injection end was then inserted into the biopsy hole of the endoscope, and a foot turn was utilized for water injection, which did not affect the colonoscopy procedure. The endoscope insertion method was the same as that of the conventional colonoscopy, adopting the method of “entering the endoscope along the cavity and shortening the longitudinal axis”. The difference was that the air insufflation pump was turned off, and the air insufflation was changed to a warm water (constant temperature: 37 °C) injection. The sewage was sucked out and clean warm water was injected to clear the vision field for easy endoscope insertion in case of residual sewage from the intestine that affected the visual field. The air retained in the intestine was sucked out at any time during the insertion to reduce bending and angularity, making the endoscope insertion easier.
The disease detection rate (colonic polyps, colonorrhagia, colonic ulcers, colonic mucosal lesions, and others), colo
Disease detection rate: This study recorded the detection rates of colonic polyps, colonorrhagia, colonic ulcers, colonic mucosal lesions, and other diseases.
Colonoscopy duration: The colonoscopy duration was observed and recorded in both groups.
Abdominal pain degree: The abdominal pain level of the participants before and after the intervention was evaluated with the VAS. The score, ranging from 0 point to 10 points, is positively correlated with the pain degree.
Bowel preparation effect: The bowel preparation effect was evaluated with the BBPS (total score: 9). A higher score indicates a better bowel preparation effect.
Psychological status: We utilized the SAS, a 20-item tool of subjective anxiety feelings scored based on the standard of 1, 2, 3, and 4, to assess patients’ psychological status. The score is proportional to the patient’s anxiety.
Bowel preparation comfort: The bowel preparation comfort level was compared with the VAS, with 0-4 points, 5-6 points, 7-8 points, and 9-10 points denoting mild, moderate, severe, and extremely severe discomfort, respectively.
Complications: The number of adverse events, including intestinal perforation, bleeding, nausea and vomiting, abdominal pain, and abdominal distension, were observed and recorded. Further, the total postoperative complication rate was calculated.
Patient satisfaction: Patient satisfaction was measured with the department’s self-made bowel preparation satisfaction scale (full score: 100 points) and compared between the two groups. The score was judged as very satisfied (≥ 80 points), relatively satisfied (60–79 points), and dissatisfied (≤ 60 points). A higher score indicates higher patient satisfaction.
The measurement data were statistically expressed as the mean ± SE of the mean. The one-sample Kolmogorov–Smirnov test for normality and Levene’s test were used to assess the normality and homoscedasticity of the measurement data, respectively. A two-independent sample t-test was implemented for each parameter if the data complied with a normal distribution. Conversely, the Mann–Whitney U test was used. Count data were presented as ratios (percentages), and the between-group comparisons were conducted with χ² tests. Data were analyzed with Statistical Package for the Social Sciences version 18.0, with the statistical difference level set at P-values of < 0.05.
Similar baseline data (e.g., sex, age, height, weight, disease course) were determined between the control and experimental groups (P > 0.05) (Table 1).
| Variables | Control group (n = 47) | Experimental group (n = 50) | χ2/t | P value |
| Sex | 0.227 | 0.634 | ||
| Male | 25 (53.19) | 29 (58.00) | ||
| Female | 22 (46.81) | 21 (42.00) | ||
| Age (years) | 49.26 ± 10.30 | 49.82 ± 12.24 | 0.243 | 0.809 |
| Height (cm) | 167.51 ± 9.27 | 168.28 ± 14.42 | 0.311 | 0.757 |
| Weight (kg) | 56.79 ± 10.94 | 61.76 ± 15.30 | 1.830 | 0.070 |
| Course of disease (months) | 6.55 ± 1.40 | 7.02 ± 1.48 | 1.604 | 0.112 |
The experimental group demonstrated a higher total detection rate of colonic polyps, colonorrhagia, colonic ulcers, colonic mucosal lesions, and other diseases than the control group (P < 0.05) (Table 2).
| Variables | Control group (n = 47) | Experimental group (n = 50) | χ2 | P value |
| Colon polyps | 12 (25.53) | 14 (28.00) | ||
| Colonorrhagia | 7 (14.89) | 9 (18.00) | ||
| Colonic ulcers | 5 (10.64) | 6 (12.00) | ||
| Colonic mucosal lesions | 2 (4.26) | 4 (8.00) | ||
| Others | 6 (12.77) | 11 (22.00) | ||
| Total | 32 (68.09) | 44 (88.00) | 5.665 | 0.017 |
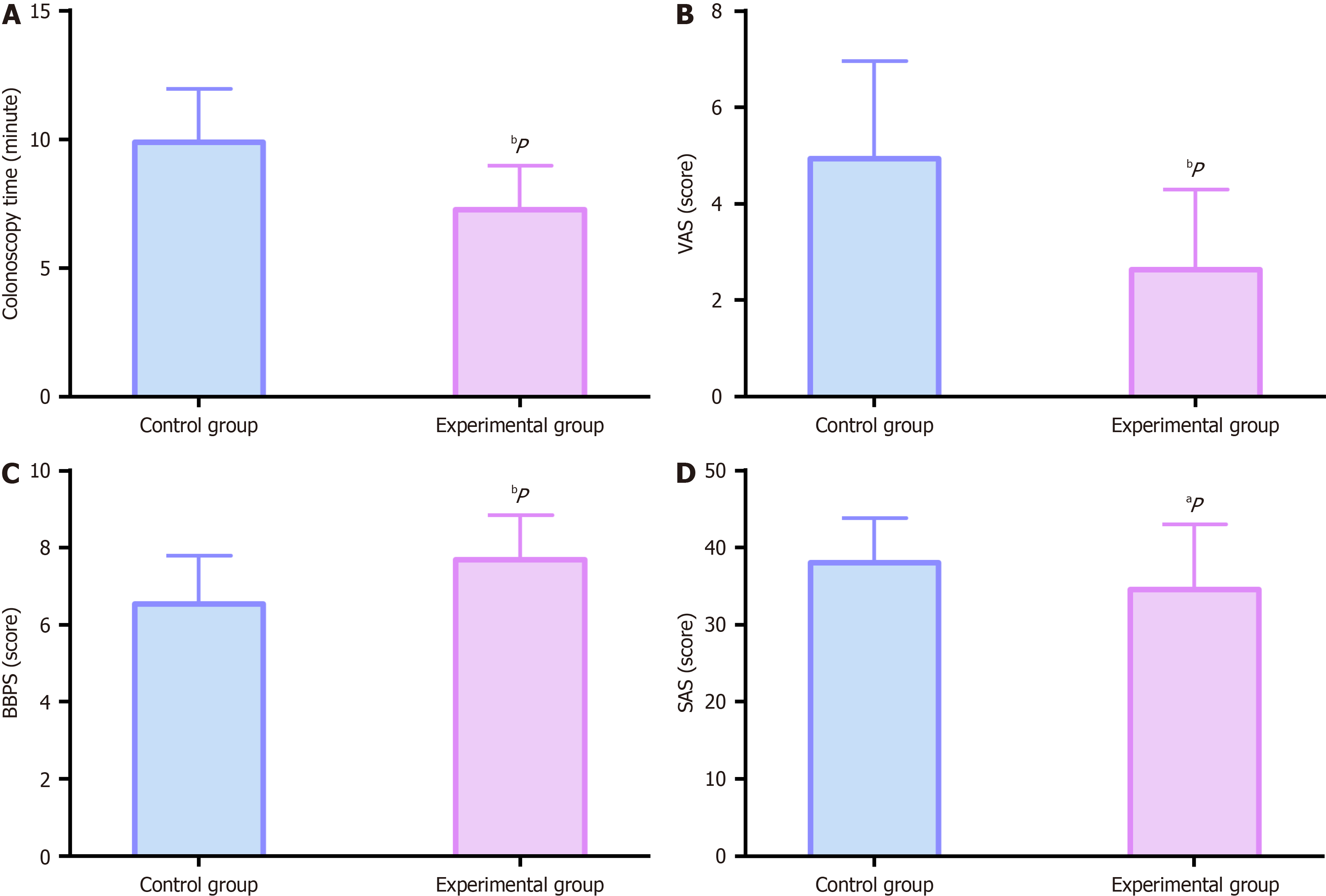
The experimental group demonstrated shorter colonoscopy duration, lower VAS and SAS scores, and higher BBPS scores than the control group (P < 0.05) (Figure 1).
Bowel preparation comfort was significantly better in the experimental group than in the control group (P < 0.05) (Table 3).
| Variables | Control group (n = 47) | Experimental group (n = 50) | χ2 | P value |
| Mild discomfort | 16 (34.04) | 35 (70.00) | 12.563 | < 0.001 |
| Moderate discomfort | 28 (59.57) | 15 (30.00) | 8.586 | 0.003 |
| Severe discomfort | 2 (4.26) | 0 (0.00) | 2.172 | 0.141 |
| Extremely severe discomfort | 1 (2.13) | 0 (0.00) | 1.075 | 0.300 |
The experimental group exhibited a lower overall incidence of intestinal perforation, bleeding, nausea and vomiting, abdominal pain, and abdominal distension than the control group (P < 0.05) (Table 4).
| Variables | Control group (n = 47) | Experimental group (n = 50) | χ2 | P value |
| Intestinal perforation | 2 (4.26) | 0 (0.00) | ||
| Bleeding | 1 (2.13) | 0 (0.00) | ||
| Nausea and vomiting | 2 (4.26) | 2 (4.00) | ||
| Abdominal pain | 2 (4.26) | 1 (2.00) | ||
| Abdominal distension | 2 (4.26) | 0 (0.00) | ||
| Total | 9 (19.15) | 3 (6.00) | 3.864 | 0.049 |
Higher patient satisfaction was identified in the experimental group compared with the control group (P < 0.05) (Table 5).
| Variables | Control group (n = 47) | Experimental group (n = 50) | χ2 | P value |
| Very satisfied | 17 (36.17) | 22 (44.00) | ||
| Satisfied | 19 (40.43) | 24 (48.00) | ||
| Dissatisfied | 11 (23.40) | 4 (8.00) | ||
| Overall satisfaction | 36 (76.60) | 46 (92.00) | 4.398 | 0.036 |
Colonoscopy, as the gold standard for diagnosing intestinal lesions, exhibits the advantages of easy operation and little effects on the gastrointestinal tract[17]. However, the efficiency and safety of colonoscopy depend on the bowel preparation degree to some extent[18]. Adequate bowel preparation not only helps to ensure smooth colonoscopy and shorten inspection time but also improves the high-quality detection rate and safety, thereby minimizing patient dis
In this study, we first assessed the disease detection rate and revealed that the experimental group demonstrated a higher overall detection rate for colon polyps, colonorrhagia, colon ulcers, colonic mucosal lesions, and other intestinal diseases, indicating that water injection combined with defoamers improved the disease detection rate in colonoscopy. Bai et al[21] revealed that the defoamer simethicone applied to colonoscopy significantly improved the adenoma detection rate, similar to our research results. Second, the experimental group exhibited a shorter colonoscopy duration, lower VAS and SAS scores, and higher BBPS scores, indicating that water injection combined with defoamers in colonoscopy is not only beneficial to improve colonoscopy efficiency, but also reduces abdominal pain, relieves patients’ anxiety, and improves bowel preparation. This may be because defoamers alter the surface tension of bubbles and promote bubble decomposition, causing a good bubble clearance in the intestine, which is conducive to improving the inspection ef
The above research results indicate that water injection combined with defoamers for patients undergoing colonoscopy demonstrates more clinical advantages compared with air insufflation, resulting in improved disease detection and examination efficiency, significantly reduced patient discomfort and anxiety, and markedly better bowel preparation effects and comfort, with a favorable safety profile and high popularity among patients.
| 1. | Sánchez-Peralta LF, Bote-Curiel L, Picón A, Sánchez-Margallo FM, Pagador JB. Deep learning to find colorectal polyps in colonoscopy: A systematic literature review. Artif Intell Med. 2020;108:101923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 65] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 2. | Hong SM, Baek DH. A Review of Colonoscopy in Intestinal Diseases. Diagnostics (Basel). 2023;13:1262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 3. | Muthukuru S, Alomari M, Bisen R, Parikh MP, Al Momani L, Talal Sarmini M, Lopez R, Muthukuru S, Thota PN, Sanaka MR. Quality of Colonoscopy: A Comparison Between Gastroenterologists and Nongastroenterologists. Dis Colon Rectum. 2020;63:980-987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Veldhuijzen G, Klaassen NJM, Van Wezel RJA, Drenth JPH, Van Esch AA. Virtual reality distraction for patients to relieve pain and discomfort during colonoscopy. Endosc Int Open. 2020;8:E959-E966. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 5. | Hayman CV, Vyas D. Screening colonoscopy: The present and the future. World J Gastroenterol. 2021;27:233-239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (3)] |
| 6. | Lakhoo K, Almario CV, Khalil C, Spiegel BMR. Prevalence and Characteristics of Abdominal Pain in the United States. Clin Gastroenterol Hepatol. 2021;19:1864-1872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 7. | Yan L, Wang X, Chen Z, Wu N, Li H, Yang B. Safety and efficacy of remimazolam tosilate combined with low-dose fentanyl for procedural sedation in obese patients undergoing gastroscopy: study protocol for a single-centre, double-blind, randomised controlled trial. BMJ Open. 2023;13:e079095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 8. | Rogers AC, Van De Hoef D, Sahebally SM, Winter DC. A meta-analysis of carbon dioxide versus room air insufflation on patient comfort and key performance indicators at colonoscopy. Int J Colorectal Dis. 2020;35:455-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Guacho JAL, Moura DTH, Ribeiro IB, Moura BFBH, Gallegos MMM, McCarty T, Toma RK, Moura EGH. Insufflation of Carbon Dioxide versus Air During Colonoscopy Among Pediatric Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Clin Endosc. 2021;54:242-249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 10. | Choy MC, Matharoo M, Thomas-Gibson S. Diagnostic ileocolonoscopy: getting the basics right. Frontline Gastroenterol. 2020;11:484-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Aziz M, Sharma S, Fatima R, Lee-Smith W, Sodeman T, Nawras A, Adler DG. How to increase proximal adenoma detection rate: a meta-analysis comparing water exchange, water immersion and air/CO(2) insufflation methods for colonoscopy. Ann Gastroenterol. 2020;33:178-186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Jiao TX, Hu Y, Guo SB. Clinical value of sigmoid colon water exchange colonoscopy: a prospective randomized clinical trial. Sci Rep. 2023;13:13704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 13. | Ma L, Yan J, Shen J, Sang J, Xu H. Comparison of application value between conventional air insufflation and water infusion in colonoscopy. Int J Clin Exp Pathol. 2020;13:2333-2341. [PubMed] |
| 14. | Roy A, Goenka MK. Simethicone and N-acetyl cysteine in improving mucosal visibility: Towards a "clearer view" during endoscopy. Indian J Gastroenterol. 2024;43:863-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 15. | Nabi Z, Vamsi M, Goud R, Sayyed M, Basha J, Reddy PM, Reddy R, Reddy P, Manchu C, Darisetty S, Gupta R, Tandan M, Rao GV, Reddy DN. Pre-medication with simethicone and N-acetyl cysteine for improving mucosal visibility during upper gastrointestinal endoscopy: A randomized controlled trial. Indian J Gastroenterol. 2024;43:986-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 16. | Zhu Y, Li J, Gao J, Bai D, Yu Z, Jin S, Chen J, Li S, Jiang P, Ge Z, Liu M, Sun C, Su Y, Zhang Y, Zhang Y. Effect of simethicone for the management of early abdominal distension after laparoscopic cholecystectomy: a multicenter retrospective propensity score matching study. BMC Surg. 2024;24:170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 17. | Sharma P, Burke CA, Johnson DA, Cash BD. The importance of colonoscopy bowel preparation for the detection of colorectal lesions and colorectal cancer prevention. Endosc Int Open. 2020;8:E673-E683. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 57] [Article Influence: 9.5] [Reference Citation Analysis (1)] |
| 18. | Millien VO, Mansour NM. Bowel Preparation for Colonoscopy in 2020: A Look at the Past, Present, and Future. Curr Gastroenterol Rep. 2020;22:28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 83] [Article Influence: 13.8] [Reference Citation Analysis (2)] |
| 19. | Latos W, Aebisher D, Latos M, Krupka-Olek M, Dynarowicz K, Chodurek E, Cieślar G, Kawczyk-Krupka A. Colonoscopy: Preparation and Potential Complications. Diagnostics (Basel). 2022;12:747. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 20. | Hammami A, Elloumi H, Bouali R, Elloumi H. Clinical practice standards for colonoscopy. Tunis Med. 2021;99:952-960. [PubMed] |
| 21. | Bai Y, Fang J, Zhao SB, Wang D, Li YQ, Shi RH, Sun ZQ, Sun MJ, Ji F, Si JM, Li ZS. Impact of preprocedure simethicone on adenoma detection rate during colonoscopy: a multicenter, endoscopist-blinded randomized controlled trial. Endoscopy. 2018;50:128-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Jung W, Oh GM, Kim JH, Choi YJ, Son MY, Jung K, Kim SE, Moon W, Park MI, Park SJ. When should patients take simethicone orally before colonoscopy for avoiding bubbles: A single-blind, randomized controlled study. Medicine (Baltimore). 2023;102:e33728. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 23. | Chen S, Guo LL, Zhong L, Shen L, Zeng Q, Lai L, Tang S. Preparation of small bowel capsule endoscopy (SBCE) with simethicone: A meta-analysis. Clin Res Hepatol Gastroenterol. 2022;46:102029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 24. | Wu L, Cao Y, Liao C, Huang J, Gao F. Systematic review and meta-analysis of randomized controlled trials of Simethicone for gastrointestinal endoscopic visibility. Scand J Gastroenterol. 2011;46:227-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 98] [Article Influence: 6.5] [Reference Citation Analysis (4)] |
| 25. | Cadoni S, Ishaq S, Hassan C, Falt P, Fuccio L, Siau K, Leung JW, Anderson J, Binmoeller KF, Radaelli F, Rutter MD, Sugimoto S, Muhammad H, Bhandari P, Draganov PV, de Groen P, Wang AY, Yen AW, Hamerski C, Thorlacius H, Neumann H, Ramirez F, Mulder CJJ, Albéniz E, Amato A, Arai M, Bak A, Barret M, Bayupurnama P, Cheung R, Ching HL, Cohen H, Dolwani S, Friedland S, Harada H, Hsieh YH, Hayee B, Kuwai T, Lorenzo-Zúñiga V, Liggi M, Mizukami T, Mura D, Nylander D, Olafsson S, Paggi S, Pan Y, Parra-Blanco A, Ransford R, Rodriguez-Sanchez J, Senturk H, Suzuki N, Tseng CW, Uchima H, Uedo N, Leung FW. Water-assisted colonoscopy: an international modified Delphi review on definitions and practice recommendations. Gastrointest Endosc. 2021;93:1411-1420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 26. | Zhang S, Zheng D, Wang J, Wu J, Lei P, Luo Q, Wang L, Zhang B, Wang H, Cui Y, Chen M. Simethicone improves bowel cleansing with low-volume polyethylene glycol: a multicenter randomized trial. Endoscopy. 2018;50:412-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 27. | Moolla M, Dang JT, Shaw A, Dang TNT, Tian C, Karmali S, Sultanian R. Simethicone decreases bloating and improves bowel preparation effectiveness: a systematic review and meta-analysis. Surg Endosc. 2019;33:3899-3909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/