Published online Mar 27, 2025. doi: 10.4240/wjgs.v17.i3.99015
Revised: December 14, 2024
Accepted: January 7, 2025
Published online: March 27, 2025
Processing time: 228 Days and 2.2 Hours
Among all forms of heterotopic ossification, heterotopic mesenteric ossification (HMO) is rare, with fewer than 100 reported cases to date. Postoperative early small bowel obstruction caused by HMO is even rarer, presenting extremely high surgical risks, the potential for multiple surgeries, and a poor prognosis. There have been no reported cases of conservative treatment for resolving such early postoperative obstruction.
A 57-year-old male presented with severe postoperative small bowel obstruction shortly after undergoing open radical resection for transverse colon cancer. Laparotomy revealed extensive adhesions in the proximal jejunum and mesen
Hormone therapy may have a potential role in treating small bowel obstruction caused by early HMO after operative intervention.
Core Tip: In this case, we present a unique treatment approach for resolving early postoperative heterotopic ossification of mesentery-induced small bowel obstruction. There was difficulty dissecting the small bowel obstruction during the second surgery, thus we tried treatment with methylprednisolone, which gradually relieved the patient’s bowel obstruction, thereby providing a new and effective strategy for early postoperative heterotopic ossification of the mesentery-induced small bowel obstruction and hypothesizing that early postoperative heterotopic ossification of the mesentery is a specific postoperative inflammatory response.
- Citation: Chen JT, Li YP, Guo SQ, Huang JS, Wang YG. Nonsurgical treatment of postoperative intestinal obstruction caused by heterotopic ossification of the mesentery: A case report. World J Gastrointest Surg 2025; 17(3): 99015
- URL: https://www.wjgnet.com/1948-9366/full/v17/i3/99015.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i3.99015
Heterotopic ossification refers to the formation of bone tissue in soft tissue where there is normally no bone tissue, which is an unusual pathological state. Heterotopic ossification was first discovered by the German doctor Riedel in 1883 and is commonly found in the limbs, especially the elbow joint[1]. Heterotopic mesenteric ossification (HMO) is extremely rare. In 1983, Hansen et al[2] first reported HMO. However, to date, fewer than 100 cases have been reported. Here, we report the case of a patient with colorectal cancer who underwent radical resection and developed HMO within a short period of time, accompanied by severe intraabdominal obstruction. Despite our inability to resolve the obstruction during surgery, treatment with methylprednisolone gradually relieved the patient’s obstruction and prevented further progression of HMO.
A 57-year-old Han Chinese male underwent open radical surgery for transverse colon cancer. Postoperative abdominal distension progressively worsened, and severe abdominal pain developed on the 14th day after surgery, which was unbearable.
The patient underwent open radical resection for transverse colon cancer. On the fifth day after surgery, the patient experienced persistent abdominal distension and was unable to pass gas or stool. We employed non-operative managements, including nasogastric decompression, fluid resuscitation, and correction of electrolyte abnormalities. On the 13th postoperative day, the patient’s abdominal distension intensified. We suspected that intestinal obstruction might be due to stenosis at the anastomotic site. Colonoscopy revealed that the anastomotic site was unobstructed. Conse
The patient had a 15-year history of hypertension, which was controlled. He was diagnosed with cerebral hemorrhage in 2011 and underwent left inguinal hernia repair 8 years ago.
The patient denied any family history of malignant tumors.
Physical examination revealed abdominal distention, abnormal bowel sounds, tenderness in the abdomen, and no Blumberg’s sign.
Alkaline phosphatase activity was elevated, and other indicators were normal.
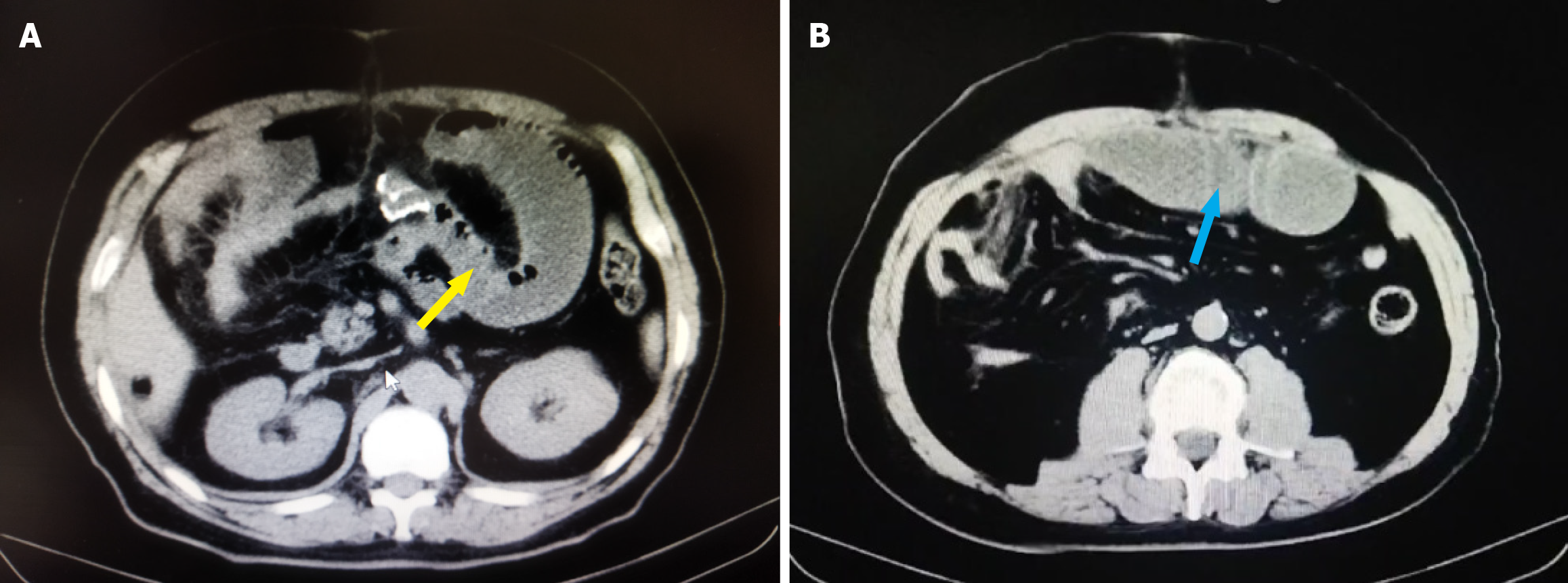
Colonoscopy revealed that the anastomosis was unobstructed without stenosis, but the mucosa of the proximal small intestine was markedly edematous, making it impossible for the colonoscope to pass through. A CT scan revealed dilation of the small bowel (Figure 1A and B), but no other abnormalities were observed.
The final diagnosis was intestinal obstruction.
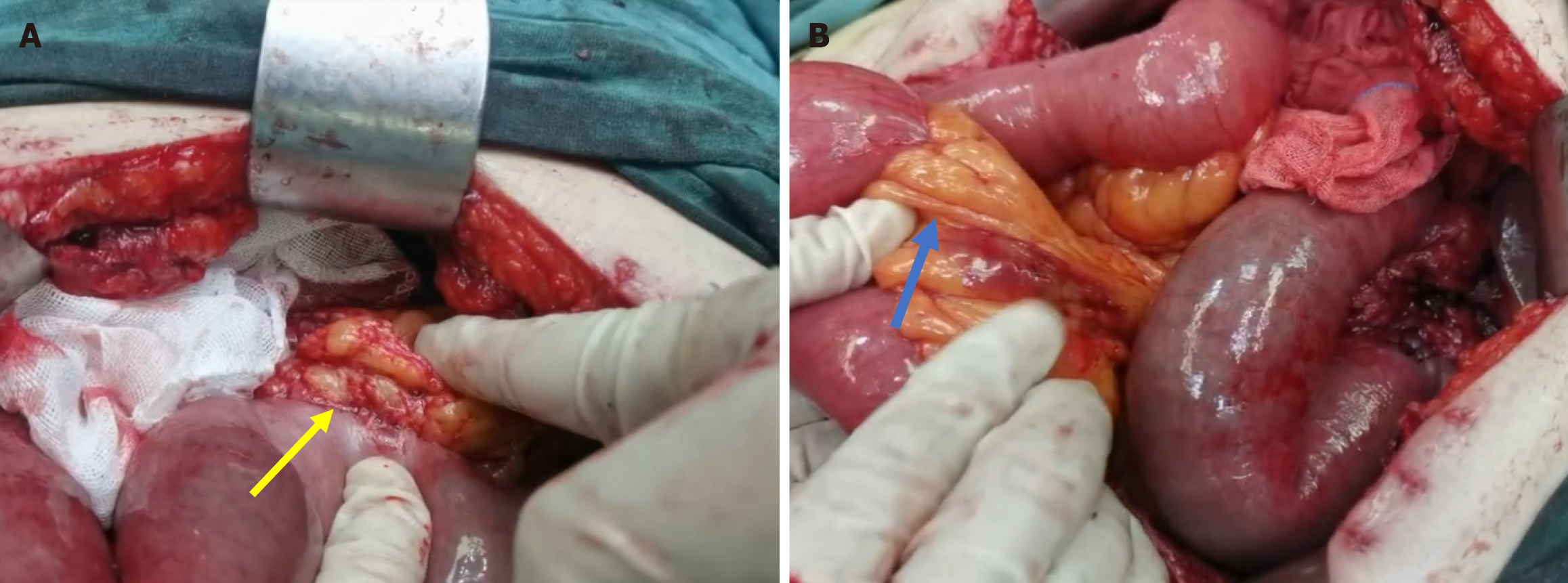
Laparotomy revealed segmental intestinal obstruction in multiple segments, with extensive and tight adhesions of the proximal jejunum and mesentery near the flexure of the ligament of Treitz, approximately 35 cm from the ligament. The original colonic flexure and the original site of the hepatic flexure were also extensively adhered (Figure 2A). The entire small intestine was adhered together like a cake, and the adhesion strength was significantly greater than that of normal abdominal adhesions 14 days after surgery. There was no free small intestine longer than 10 cm in the abdominal cavity, which prevented us from identifying the proximal and distal ends. Thus, enterostomy could not be performed. Attempts at blunt and sharp dissection failed to completely resolve the intestinal obstruction. Even if the surgeon avoided the use of energy-based cutting, carefully dissecting the patient with scissors can still easily damage the small intestine. Addi
Postoperative care included fasting, placement of an intestinal obstruction set, suppression of digestive fluid secretion with octreotide, and nutritional support. The intestinal obstruction set was difficult to place through the ligament of Treitz. Methylprednisolone was given for anti-inflammatory and symptomatic treatment for one week, with an initial dose of 40 mg per day followed by 40 mg twice a day for the next two days and then 40 mg per day until the seventh day, followed by discontinuation on the eighth day. The patient was monitored closely for complications such as stress ulcers and electrolyte imbalances.
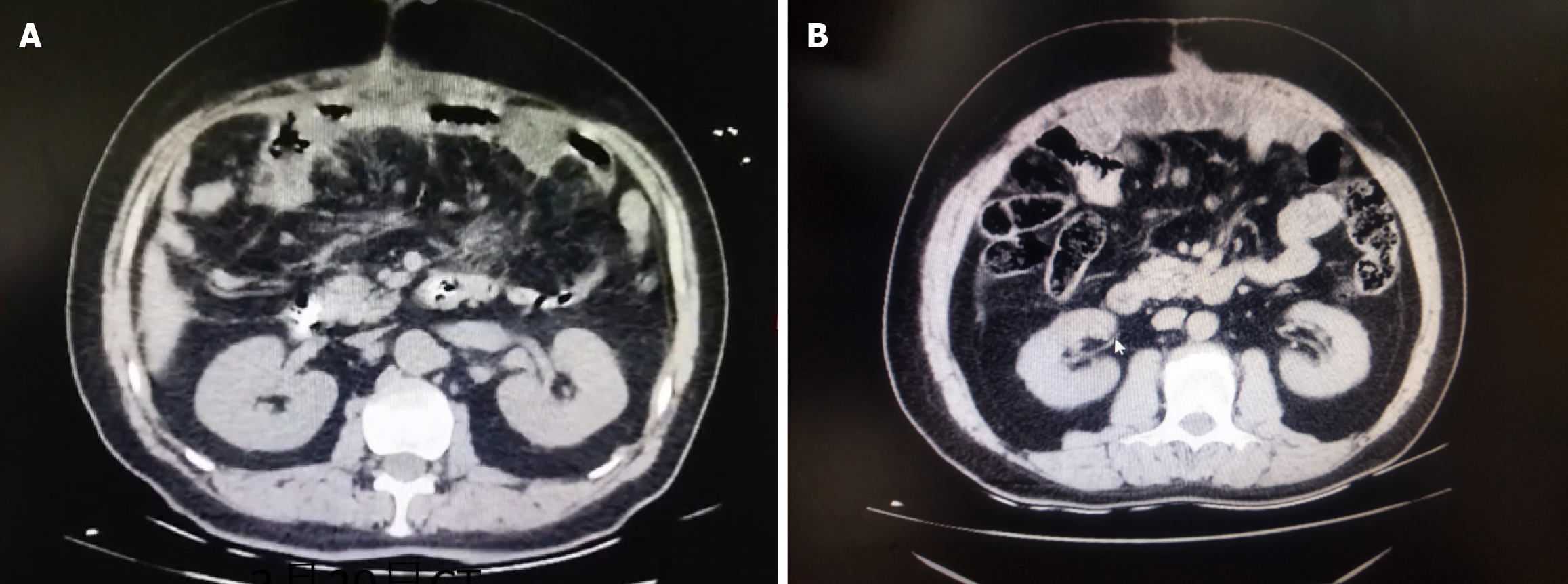
The intestinal obstruction gradually improved after one week of hormone therapy (Figure 4A), and the patient was discharged from the hospital on the 25th day after the second surgery. At the eight-month follow-up visit, the patient reported no discomfort. CT imaging revealed no significant abnormalities (Figure 4B).
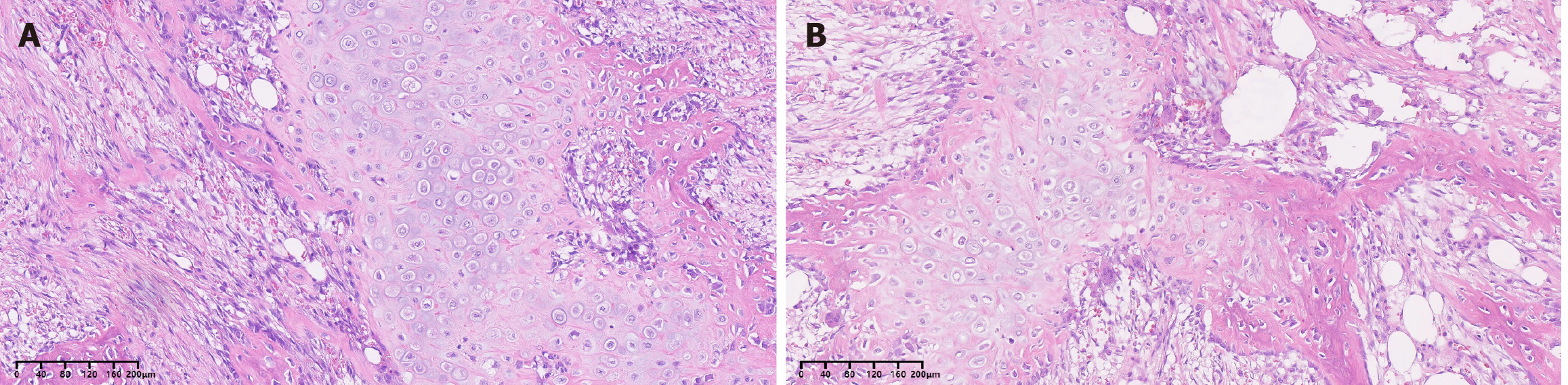
The occurrence of HMO is the result of specific signaling molecules in the peritoneal cavity that induce mesenchymal stem cell osteogenesis, and abdominal trauma and surgery seem to be the triggering factors for this process[3,4]. Another explanation is that trauma and surgery lead to the transplantation of bone tissue to the mesentery[5]. A review of the literature (Supplementary Table 1) revealed that most of the reported cases of HMO were found in males (57/64, 89.06%), with a median age of 51.5 years (range 21-88 years), and are closely related to a history of abdominal trauma and surgery (52/58, 89.66%). The remaining cases were spontaneous HMO[6]. HMO primarily occurs in the small intestinal mesentery (50/64, 78.13%), and the symptoms mainly manifest as small intestinal obstruction (32/58, 55.17%)[7] and enterocutaneous fistula (6/58, 10.34%)[8]. There are no specific laboratory findings associated with HMO, and only alkaline phosphatase may be elevated[9], which may be related to the increased activity of osteoblasts and the need for more case support. The unique feature of this case was the rapid formation of bone tissue, with bone formation occurring within 14 days, which may have been due to insufficient deposition of calcium salts, and the CT scan did not show a high-density image. Second, HMO is accompanied by a strong inflammatory reaction in the abdominal cavity, with extensive adhesions forming between the small intestine, mesentery, and peritoneum. Finally, after hormonal therapy, there was gradual relief of the intestinal obstruction that could not be relieved by mechanical dissection, which is encouraging. The patient’s stool gradually transformed from a clay-colored consistency to a normal appearance (Supplementary Figure 1). Most gastrointestinal surgeons might not encounter such postoperative complications during their career. However, they should remain vigilant in preventing inflammatory intestinal obstruction caused by early postoperative HMO. Although only 7 cases of early postoperative HMO have been reported, they share common features: Rapid onset, extensive adhesions leading to difficulty in dissection, small intestinal obstructions, thick mesenteries, and hard fibrous osteoid tissue forming on the mesentery within 1 month after surgery. In such instances, there is a significantly elevated surgical risk owing to the inability to dissect inflammatory adhesions without causing damage to the small intestine. This increases the likelihood of multiple operations, reduces patient tolerance for such procedures, and leads to a poor prognosis. Only one of the seven patients recovered after intestinal adhesion dissection (Table 1)[10], and one patient recovered after the removal of 240 cm of the obstructed small intestine in addition to receiving nonsteroidal anti-inflammatory drug treatment[11]. Two patients died from postoperative complications resulting from multiple surgeries[12,13]. Moreover, three patients experienced recurrence following adhesiolysis or intestinal resection, necessitating multiple subsequent surgeries[2,14,15].
| Year | Age | Sex | Primary disease/operation | Clinical history | Onset | Site | Therapy | Outcome |
| 1983 | 55 | Male | Ulcerative colitis/surgery | SBO | 2 weeks | M | OP | Relapse |
| 2000 | 25 | Male | Fire-gun injury/surgery | SBO | 2 weeks | M | OP | Relapse |
| 2005 | 74 | Male | Intestinal obstruction/surgery | SBO | 10 days | M, O | OP | Death |
| 2010 | 50 | Male | Morbid obesity/surgery | Fistula/SBO | 12 days | M, O | OP | Relapse |
| 2011 | 39 | Male | Cancer/surgery | SBO | 2 weeks | O | OP | Recovery |
| 2014 | 88 | Male | Abdominal aortic aneurysm/surgery | SBO | 2 weeks | M | OP + NSAIDs | Recovery |
| 2018 | 72 | Male | Cancer/surgery | SBO | SW | M | OP | Death |
Ectopic ossification may represent a nonspecific inflammatory response. Methylprednisolone has been shown to inhibit inflammation resulting from both infectious and noninfectious factors by preventing inflammatory mediators from reacting and inhibiting complement involvement in the inflammatory response while also mitigating tissue damage repair following inflammation. In the advanced stage of inflammation, it can also suppress the vitality of fibroblasts, decrease the soluble collagen components in tissues, and minimize adhesion and scar formation. Although there are no documented successful cases thus far, hormonal therapy has emerged as an option that should potentially be pursued. Without such intervention, patients may face imminent mortality due to the inability to sustain parenteral nutrition or progressive energy failure. Fortunately, we successfully treated these inflammatory bowel obstructions with methylprednisolone, avoiding the risk of multiple surgeries, preserving the patient’s entire small intestine, and saving the patient’s life. The patient has been discharged from the hospital for more than eight months, and follow-up examinations revealed that the patient is in excellent health. Surgeons should consider this approach as a final attempt when confronted with similar challenges subsequent to unsuccessful surgical intervention (Video 1).
In conclusion, early HMO may be accompanied by severe intra-abdominal inflammatory reactions, leading to intestinal obstruction. Our therapeutic approach provides a new treatment possibility for intestinal obstruction caused by early postoperative HMO, but more clinical cases are still needed for confirmation.
We appreciate the cooperation of the patient and his family during the treatment.
| 1. | Balboni TA, Gobezie R, Mamon HJ. Heterotopic ossification: Pathophysiology, clinical features, and the role of radiotherapy for prophylaxis. Int J Radiat Oncol Biol Phys. 2006;65:1289-1299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 213] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 2. | Hansen O, Sim F, Marton PF, Grüner OP. Heterotopic ossification of the intestinal mesentery. Report of a case following intraabdominal surgery. Pathol Res Pract. 1983;176:125-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Patel RM, Weiss SW, Folpe AL. Heterotopic mesenteric ossification: a distinctive pseudosarcoma commonly associated with intestinal obstruction. Am J Surg Pathol. 2006;30:119-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 34] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Gouëllo JP, Auvray L, Bouix A, Vazelle F, Guinard N, Hermes D. Early post-traumatic heterotopic mesenteric ossification: report of a case. Intensive Care Med. 2006;32:950-951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Koolen PG, Schreinemacher MH, Peppelenbosch AG. Heterotopic ossifications in midline abdominal scars: a critical review of the literature. Eur J Vasc Endovasc Surg. 2010;40:155-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Bovo G, Romano F, Perego E, Franciosi C, Buffa R, Uggeri F. Heterotopic mesenteric ossification ("intraabdominal myositis ossificans''): a case report. Int J Surg Pathol. 2004;12:407-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Fadare O, Bifulco C, Carter D, Parkash V. Cartilaginous differentiation in peritoneal tissues: a report of two cases and a review of the literature. Mod Pathol. 2002;15:777-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Torgersen Z, Osmolak A, Bikhchandani J, Forse AR. Ectopic bone in the abdominal cavity: a surgical nightmare. J Gastrointest Surg. 2013;17:1708-1711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Althaqafi RMM, Assiri SA, Aloufi RA, Althobaiti F, Althobaiti B, Al Adwani M. A case report and literature review of heterotopic mesenteric ossification. Int J Surg Case Rep. 2021;82:105905. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 10. | Shi X, Zhang W, Nabieu PF, Zhao W, Fu C. Early postoperative heterotopic omental ossification: report of a case. Surg Today. 2011;41:137-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Honjo H, Kumagai Y, Ishiguro T, Imaizumi H, Ono T, Suzuki O, Ito T, Haga N, Kuwabara K, Sobajima J, Kumamoto K, Ishibashi K, Baba H, Sato O, Ishida H, Kuwano H. Heterotopic mesenteric ossification after a ruptured abdominal aortic aneurism: case report with a review of literatures. Int Surg. 2014;99:479-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Androulaki A, Chatzoulis G, Kalahanis N, Lazaris AC. Heterotopic mesenteric ossification: a rare reactive process. J Gastroenterol Hepatol. 2005;20:664-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Amalfitano M, Fyfe B, Thomas SV, Egan KP, Xu M, Smith AG, Kaplan FS, Shore EM, Pignolo RJ. A case report of mesenteric heterotopic ossification: Histopathologic and genetic findings. Bone. 2018;109:56-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Marucci G, Spitale LS, Piccinni DJ. [Heterotopic mesenteric ossification. Description of a case]. Pathologica. 2000;92:331-334. [PubMed] |
| 15. | Yushuva A, Nagda P, Suzuki K, Llaguna OH, Avgerinos D, Goodman E. Heterotopic mesenteric ossification following gastric bypass surgery: case series and review of literature. Obes Surg. 2010;20:1312-1315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/