Published online Mar 27, 2025. doi: 10.4240/wjgs.v17.i3.102190
Revised: December 23, 2024
Accepted: January 8, 2025
Published online: March 27, 2025
Processing time: 123 Days and 23.7 Hours
Bile leakage is a common complication following laparoscopic common bile duct exploration (LCBDE) with primary duct closure (PDC). Identifying and analyzing the risk factors associated with bile leakage is crucial for improving surgical outcomes.
To explore the value analysis of common risk factors for bile leakage after LCBDE and PDC, with a focus on strict adherence to indications.
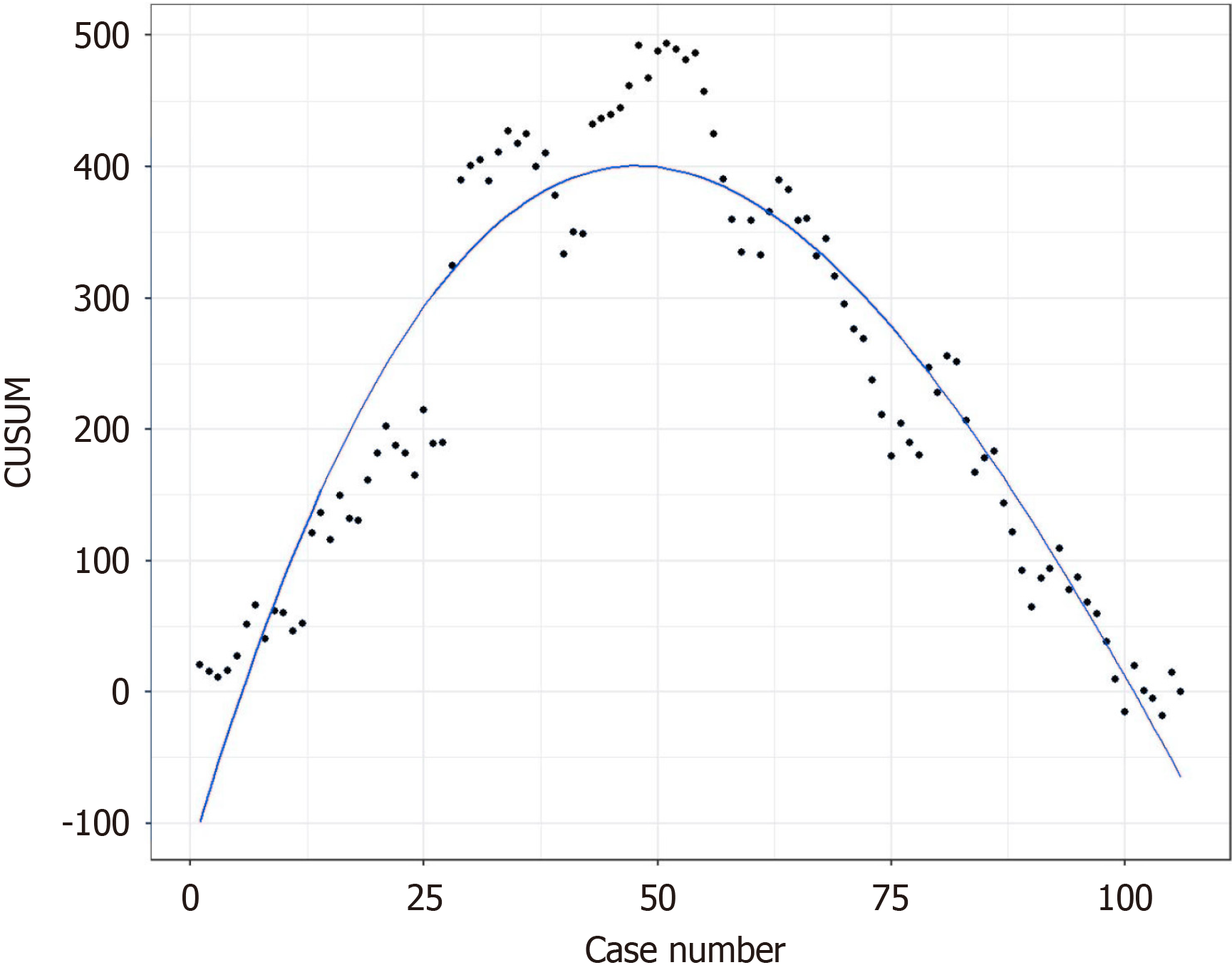
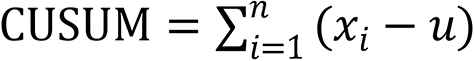
Clinical data of 106 cases undergoing LCBDE + PDC in the Hepatobiliary and Pancreatic Surgery Department (Division 1) of Chuzhou First People’s Hospital from April 2019 to March 2024 were collected. Retrospective and multiple factor regression analysis were conducted on common risk factors for bile leakage. The change in surgical time was analyzed using the cumulative summation (CUSUM) method, and the minimum number of cases required to complete the learning curve for PDC was obtained based on the proposed fitting curve by identifying the CUSUM maximum value.
Multifactor logistic regression analysis showed that fibrinous inflammation and direct bilirubin/indirect bilirubin were significant independent high-risk factors for postoperative bile leakage (P < 0.05). The time to drain removal and length of hospital stay in cases without bile leakage were significantly shorter than in cases with bile leakage (P < 0.05), with statistical significance. The CUSUM method indicated that a minimum of 51 cases were required for the surgeon to complete the learning curve (P = 0.023).
With a good assessment of duodenal papilla sphincter function, unobstructed bile-pancreatic duct convergence, exact stone clearance, and sufficient surgical experience to complete the learning curve, PDC remains the preferred method for bile duct closure and is worthy of clinical promotion.
Core Tip: This study identifies key risk factors for bile leakage following laparoscopic common bile duct exploration and primary duct closure (PDC). Through retrospective analysis and logistic regression, fibrinous exudation and direct bilirubin/indirect bilirubin were found to be significant independent risk factors. The cumulative summation method demonstrated that a minimum of 51 cases is required for surgeons to master the PDC technique effectively. Proper assessment of duodenal papilla function, ensuring bile duct patency, and achieving surgical proficiency are essential for minimizing complications. Adhering to these guidelines may optimize patient outcomes and promote PDC as a preferred method in clinical practice.
- Citation: Yang QS, Zhang M, Ma CS, Teng D, Li A, Dong JD, Wang XF, Liu FB. Analysis of risk factors for bile leakage after laparoscopic exploration and primary suture of common bile duct. World J Gastrointest Surg 2025; 17(3): 102190
- URL: https://www.wjgnet.com/1948-9366/full/v17/i3/102190.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i3.102190
Laparoscopic common bile duct exploration (LCBDE) as a mature surgical method for treating intrahepatic and extrahepatic bile duct stones has undergone more than a century of development[1-4]. With the continuous advancement of medical technology, especially the use of high-definition laparoscopy, high-definition cholangioscopy, and stone frag
This study aims to explore how, under strict control of surgical indications, analyzing known risk factors for bile leakage after PDC can further optimize surgical strategies and reduce the incidence of complications. The research will summarize and analyze factors that may lead to bile leakage after PDC, including but not limited to patient age, bile duct diameter, severity of cholangitis, bile duct injury during surgery, and postoperative bile duct pressure. The role of multidisciplinary team collaboration, including surgeons, anesthesiologists, nursing teams, and radiologists, is in
A total of 106 cases were included in this study, consisting of patients who underwent LCBDE + PDC for liver ex
Inclusion criteria: (1) Patients with common bile duct dilation or suspected common bile duct lesions with negative exploration results; (2) Patients who have had their common bile duct stones removed completely and the end of the common bile duct is unobstructed; (3) Patients with gallbladder stones, common bile duct stones, and distal obstruction or stenosis of the common bile duct all effectively treated during surgery; (4) After completing the first stage suture surgery, observe the absence of sustained obvious bile leakage at the incision site of the common bile duct; and (5) Those who have successfully retained nasobiliary drainage before or during surgery.
Exclusion criteria: (1) Residual stones in the extrahepatic bile duct and stenosis at the end of the common bile duct that were not treated or treated satisfactorily during surgery; (2) Intrahepatic bile duct stones combined with intrahepatic bile duct stenosis; (3) Long term, reliable, and unobstructed external drainage of the bile duct is required due to the primary disease; (4) Elderly patients with biliary and pancreatic duct diseases; and (5) Combine patients with severe cardio
Complete cholecystectomy according to standard laparoscopic common operating procedures; Fully expose the common bile duct (free descending duodenal bulb if necessary), use low-power electrocoagulation (30 W) to occlude the serosal vascular network of the anterior wall of the bile duct, and make a sharp longitudinal incision of about 0.6 cm of the anterior wall of the common bile duct (depending on the size of the stone); Complete cholangioscopy for stone removal, clear infectious fibrous exudate, fully evaluate the function and patency of the duodenal papilla, and ensure accurate stone removal; Adopt intermittent/continuous suture of bile duct incision (suture selection: 4-0 Vicryl suture); Take out the specimen, rinse the surgical area, observe and rule out bile leakage, and then place a drainage tube at the lesser omentum hole to fix it by pulling out a trocar 5 mm below the right rib margin. Under direct visualization, remove each trocar and suture the incision layer by layer. Postoperative management includes monitoring the abdominal drainage tube: Closely observe the volume and nature of bile drainage. If bile is continuously drained for 3 days postoperatively or the single-day drainage volume is ≥ 100 mL, bile leakage may be indicated. For patients without a drainage tube, monitor for signs of peritoneal irritation. If necessary, perform abdominal puncture to check for bile. Suspected bile leakage can be confirmed via intraoperative cholangiography. Prompt control of infections secondary to bile leakage is crucial to avoid contraindications for surgical treatment. Provide appropriate nutritional support to aid recovery. Criteria for determining bile leakage typically include: Continuous bile drainage from the abdominal tube for 3 days post-surgery or single-day drainage volume ≥ 100 mL. For those without a drainage tube, signs of peritoneal irritation, bile extracted via abdominal puncture, or intra-abdominal bile found during reoperation. Detection of contrast agent accumulation outside the biliary system through intraoperative cholangiography or postoperative imaging (e.g., computed tomography, magnetic resonance imaging) suggests bile leakage. Symptoms like fever, abdominal pain, and tenderness, along with laboratory findings (e.g., elevated white blood cell count), support the diagnosis of bile leakage.
Monitor postoperative drainage volume (mL/day) to determine the presence of bile leakage, surgical time, postoperative extubation time, postoperative discharge time, and total hospitalization costs. All cases were followed up routinely for 6-12 months after surgery, and no fluid accumulation, bile duct stenosis, stone recurrence.
Apply the cumulative summation (CUSUM) method to analyze the changes in surgical time. Representing the actual surgical time of each patient and the average surgical time of the same group of patients. Calculate the deviation between the actual surgical time value and the average surgical time value for each patient, and obtain CUSUM by summing multiple times. The calculation formula for this study is as follows: Sort the samples in the order of surgery and edit the serial numbers. Draw a scatter plot with CUSUM value as the vertical axis and number of cases as the horizontal axis, and then perform curve fitting. The fitting coefficient was used to determine the degree of fitting, and linear, quadratic, and cubic fitting were performed separately. The closer the value is to 1, the better the fitted curve.
This article uses SPSS 27.0 and R 4.3.2 to process and analyze the data. Continuous data is represented in the form of mean ± SD, while categorical data is represented in the form of frequency (percentage). Single factor logistic regression was used to analyze the risk factors for bile leakage, and multiple factor logistic regression was used to analyze the independent risk factors for bile leakage. The differences were statistically significant with P < 0.05 in the entire study. The rank sum test is used to analyze whether postoperative bile leakage has a significant impact on extubation time, discharge time, and total hospitalization costs. Construct a learning curve using CUSUM and fit it.
A single factor logistic regression model was established with total bilirubin, straight to straight ratio, history of diabetes, operation time, number of cases of surgery, history of hypertension, suture mode, incidence, common bile duct stones (single, multiple, discharged stones, fibrinous exudation, microstones), gallstones (microstones, multiple), grass to propylene ratio, albumin, white blood cell, total bile acid, hemoglobin, γ-glutamyl transpeptidase, C-reactive protein, common bile duct diameter, carbohydrate antigen 199, alkaline phosphatase, and other factors as independent variables, and whether bile leakage occurred after surgery as dependent variables (Tables 1 and 2). From the above results, it can be concluded that common bile duct stones (fibrinous exudation), total bilirubin, and direct bilirubin/indirect bilirubin ratio (direct to indirect ratio) have a significant impact on whether bile leakage occurs after surgery (P < 0.05), and are risk factors for postoperative bile leakage.
| Characteristic | Overall | No bile leakage occurs | Gallbladder leakage occurs | |
| Gallstones-multiple | No | 90 (84.91) | 78 (100) | 12 (100) |
| Yes | 16 (15.09) | 16 (0) | 0 (0) | |
| Gallstones-micro stones | No | 78 (73.58) | 69 (75) | 9 (75) |
| Yes | 28 (26.42) | 25 (25) | 3 (25) | |
| Gallstones-post laparoscopic common surgery | No | 93 (87.74) | 86 (58.33) | 7 (58.33) |
| Yes | 13 (12.26) | 8 (41.67) | 5 (41.67) | |
| Common bile duct stones-single | No | 67 (63.21) | 60 (58.33) | 7 (58.33) |
| Yes | 39 (36.79) | 34 (41.67) | 5 (41.67) | |
| Common bile duct stones | No | 52 (49.06) | 47 (41.67) | 5 (41.67) |
| Yes | 54 (50.94) | 47 (58.33) | 7 (58.33) | |
| Common bile duct stones-micro stones | No | 37 (34.91) | 34 (36.17) | 3 (25) |
| Yes | 69 (65.09) | 60 (63.83) | 9 (75) | |
| Common bile duct stones-cellulose | No | 72 (67.92) | 69 (73.40) | 3 (25) |
| Yes | 34 (32.08) | 25 (26.60) | 9 (75) | |
| Common bile duct stones | No | 103 (97.17) | 91 (100) | 12 (100) |
| Yes | 3 (2.83) | 3 (0) | 0 (0) | |
| CBD | 5-6 | 7 (6.6) | 6 (8.33) | 1 (8.33) |
| 6-7 | 17 (16.04) | 15 (16.67) | 2 (16.67) | |
| 7-8 | 16 (15.09) | 15 (8.33) | 1 (8.33) | |
| 8-9 | 18 (16.98) | 15 (25) | 3 (25) | |
| > 9 | 48 (45.28) | 43 (41.67) | 5 (41.67) | |
| Factors, mean ± SD | ||||
| WBC | 7.35 ± 3.36 | 7.57 ± 3.39 | 5.64 ± 2.56 | |
| HB | 132.1 ± 16.42 | 132.23 ± 17.15 | 131.08 ± 9.23 | |
| CRP | 22.42 ± 46.68 | 23.91 ± 48.38 | 10.76 ± 29.06 | |
| CA199 | 99.06 ± 361.33 | 72.21 ± 283.09 | 233.27 ± 628.95 | |
| Total bilirubin | 41.33 ± 36.58 | 43.91 ± 37.93 | 21.13 ± 10.4 | |
| Directly increase the proportion | 2.64 ± 3.06 | 19.48 ± 21.73 | 7.04 ± 6.6 | |
| Indirect increase ratio | 1.52 ± 1.13 | 24.43 ± 17.75 | 14.09 ± 4.93 | |
| Straight to straight ratio | 0.82 ± 0.45 | 0.87 ± 0.44 | 0.45 ± 0.28 | |
| Albumin | 43.48 ± 5.09 | 1.6 ± 1.18 | 0.93 ± 0.32 | |
| ALT/AST | 0.76 ± 0.52 | 0.94 ± 0.98 | 0.36 ± 0.07 | |
| GGT | 308.09 ± 289.23 | 43.52 ± 5.19 | 43.16 ± 4.39 | |
| ALP | 166.2 ± 133.37 | 223.04 ± 241.17 | 73.29 ± 90.76 | |
| TBA | 33.2 ± 54.3 | 130.9 ± 161.17 | 41.76 ± 39.36 | |
| Operative time | 89.42 ± 28.76 | 0.75 ± 0.53 | 0.77 ± 0.4 | |
| Factors | Coefficient | Z value | P value |
| Incidence | -0.9614 | -1.5464 | 0.1220 |
| History of diabetes | 1.5041 | 1.6209 | 0.1050 |
| History of hypertension | 1.1436 | 1.8248 | 0.0680 |
| Gallstones-multiple | -16.6943 | -0.0102 | 0.9918 |
| Gallstones-micro stones | -0.0834 | -0.1180 | 0.9060 |
| Common bile duct stones-single | 0.2315 | 0.3712 | 0.7105 |
| Common bile duct stones | 0.3365 | 0.5420 | 0.5878 |
| Common bile duct stones-micro stones | 0.5306 | 0.7576 | 0.4487 |
| Common bile duct stones-cellulose | 2.1138 | 2.9930 | 0.0028 |
| Common bile duct stones | -14.5401 | -0.0105 | 0.9916 |
| CBD | -0.2231 | -0.1695 | 0.8654 |
| WBC | -0.2557 | -1.8175 | 0.0691 |
| HB | -0.0043 | -0.2297 | 0.8183 |
| CRP | -0.0105 | -0.8830 | 0.3772 |
| CA199 | 0.0009 | 1.1705 | 0.2418 |
| Total bilirubin | -0.0506 | -2.0312 | 0.0422 |
| Direct/indirect bilirubin | -7.0321 | -2.8225 | 0.0048 |
| Albumin | 0.0000 | 0.0000 | 1.0000 |
| ALT/AST | 0.0731 | 0.1259 | 0.8998 |
| GGT | 0.0000 | 0.0000 | 1.0000 |
| ALP | -0.0065 | -1.3364 | 0.1814 |
| TBA | -0.0024 | -0.3707 | 0.7109 |
| Operative time | 0.0157 | 1.7035 | 0.0885 |
| Suture method | 0.3221 | 0.4915 | 0.6231 |
Perform multiple logistic regression analysis using factors that have a significant impact on single factor logistic regression as independent variables, as shown in Table 3. The above results indicate that common bile duct stones (cellulose) and the ratio of direct bilirubin/indirect bilirubin are independent risk factors for postoperative bile leakage (P < 0.05).
| Factor | Partial regression coefficient | Error | Z value | P value | OR | 95%CI |
| Common bile duct stones-cellulose | 1.97008 | 0.77372 | 2.546 | 0.0109 | 7.171 | 1.705-38.400 |
| Total bilirubin | -0.03732 | 0.02841 | -1.314 | 0.189 | 0.963 | 0.903-1.010 |
| Direct/indirect bilirubin | -5.60348 | 2.43206 | -2.304 | 0.0212 | 0.004 | 0.000-0.154 |
The rank sum test was used to examine whether bile leakage had a significant impact on extubation time, discharge time, and total hospitalization costs. The results are as follows (Table 4). The above results show that patients who did not experience bile leakage after surgery had significantly shorter extubation time and discharge time compared to patients who experienced bile leakage after surgery, with P < 0.05 and statistical significance.
| Factors | No bile leakage occurs | Gallbladder leakage occurs | Z value | P value |
| Pull out time | 3.61 ± 1.25 | 5.33 ± 2.81 | -2.627 | 0.009 |
| Discharge time | 5.77 ± 1.44 | 8.67 ± 6.49 | -2.105 | 0.035 |
| Total hospitalization expenses | 15913.7 ± 3246.7 | 17249.28 ± 4344.86 | -0.648 | 0.517 |
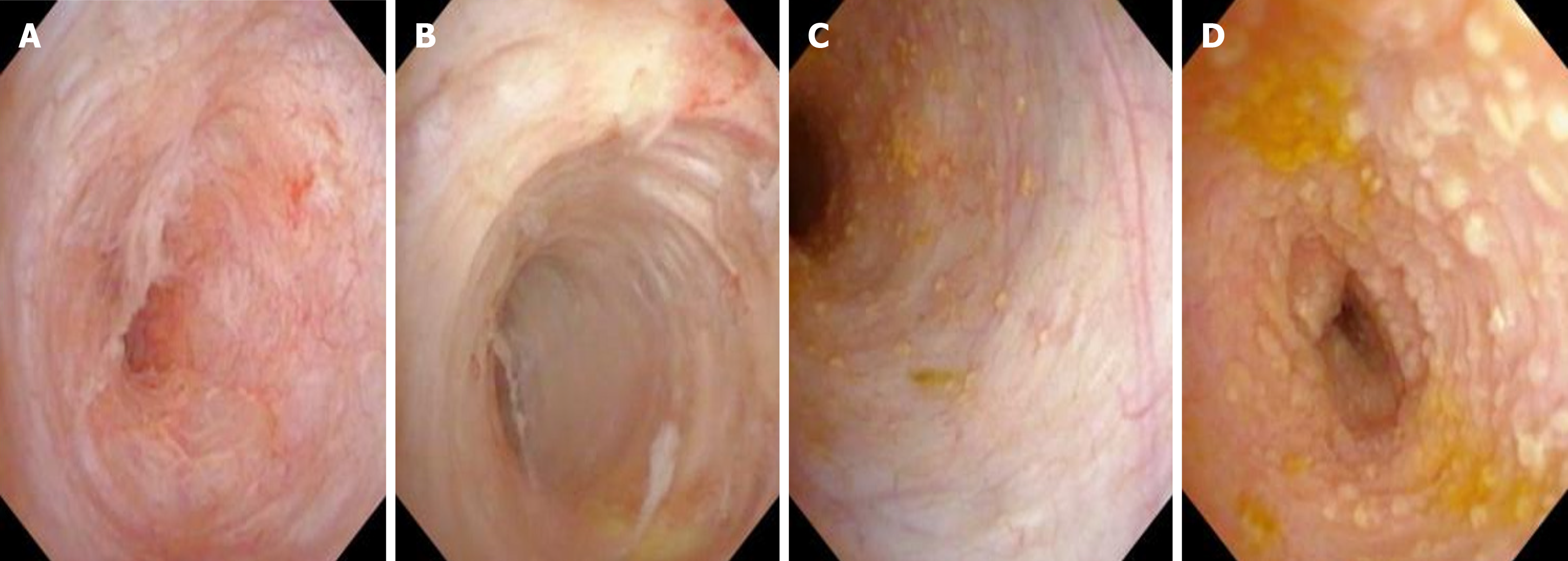
Obtain three fitting curves: Based on the proposed fitting curve, find the case number 51 with the maximum CUSUM value, which is the minimum number of surgeries required to cross the learning curve. The curve can be divided into two stages of surgical maturity, namely the stage of technical improvement and the stage of proficiency, based on the maximum value of CUSUM, which is 51. Using two groups as independent variables and postoperative bile leakage as the dependent variable, the logistic regression model shows that the surgical maturity stage significantly affects the occurrence of postoperative bile leakage (P = 0.023, Figure 1). The schematic diagram of gallbladder inflammation is shown in Figure 2 below.
 .
.
The comprehensive evaluation of the duodenal papilla function of the duodenal papilla includes the sphincter of Oddi (SO) [mainly involving the contraction and relaxation function of the bile duct sphincter and the ampulla sphincter, as well as the smooth flow of the bile and pancreatic ducts, and diseases leading to So dysfunction (SOD)] mainly include: Fibrosis or chronic inflammation-induced Oddi sphincter stenosis: This is one cause of SOD, where fibrosis or chronic inflammation of the sphincter leads to narrowing, affecting the normal flow of bile and pancreatic juices. Congenital sphincter hypertrophy, and neuromuscular or hormonal factors causing intermittent spasmodic dysfunction: These causes involve congenital issues or abnormal neurohormonal regulation, leading to functional abnormalities of the Oddi sphincter. Post-cholecystectomy dysfunction: After gallbladder removal, the Oddi sphincter may experience dysfunction due to the loss of the gallbladder’s regulatory effect on bile duct pressure, leading to bile excretion disorders and SOD. Oddi sphincter dysfunction refers to a series of clinical syndromes caused by structural or functional abnormalities of the bile duct and/or pancreatic duct sphincter[10-12]. Low pressure in the bile duct and smooth flow in the bile and pancreatic duct junction are necessary prerequisites for effective healing of the bile duct first-phase incision and reducing bile leakage. For different levels of patency at the distal end of the laparoscopic common bile duct[13], laparoscopic duodenal papilla step by step dilatable catheter dilatation or laparoscopic duodenal papilla balloon dilatation is adopted. When necessary, laparoscopic endoscopic nasobiliary drainage or laparoscopic common bile duct stent is performed to ensure the patency of the duodenal papilla and maintain low pressure in the bile duct.
In this study, cases that did not undergo first-phase incision were mostly those in whom effective stone clearance could not be guaranteed, the conditions for bile duct wall closure were inadequate (such as significant needle hole leakage requiring multiple needle-point sutures but still unsatisfactory), severe bile duct inflammation requiring extended biliary decompression to increase perioperative safety and smooth recovery, a patient population unable to tolerate secondary surgery due to complications such as bile leakage, and the presence of factors such as liver hilum tumor that may lead to short-term extrinsic bile duct obstruction preventing the intraoperative placement of initial stents, advising against first-phase incision to prevent serious complications such as bile leakage and secondary surgeries, especially in elderly patients with relative contraindications.
Assessing the diameter of the common bile duct during surgery may be limited by factors such as differences in surgeons, inflammation of surrounding bile duct tissues preventing full visualization, and lack of effective measuring tools. Clinically, preoperative evaluations of the inner diameter of the common bile duct through methods such as color Doppler ultrasound, computed tomography, magnetic resonance cholangiopancreatography are more objective. However, the timing and methods of measurements using these various techniques differ, leading to significant va
For patients with common bile duct dilation greater than 8 cm, numerous clinical studies have confirmed that first-phase incision is safe and effective[14-16]. Given the lack of muscle layer in the extrahepatic bile ducts (primarily referring to the common bile duct), for patients with significant dilation (distinct from bile duct dilation), bile stasis, stone recurrence, and other long-term complications merit further clinical research. Animal experiments have shown that longitudinal incision of the bile duct does not lead to scar healing[17]. For individuals with a normal bile duct diameter that does not dilate due to sustained increase in bile duct pressure, it can be assumed that the SO function can maintain a good state of low pressure in the bile duct. This provides a theoretical basis for populations with smaller bile duct diameters. This study suggests that for patients with a common bile duct diameter < 8 mm, PDC can be safely performed without increasing the risk of long-term complications related to bile duct stricture.
Fibrinous inflammation often occurs on the mucous and serous membranes, referring to inflammatory exudate containing a large amount of fibrin protein. When there is biliary tract infection, the exuded fibrin, neutrophils, and necrotic mucosal tissues (the exuded fibrin coagulates) form a thin yellowish, elastic membrane covering the bile duct mucosa, known as pseudomembranous inflammation, which is often easily peeled off[18-21]. The substantial exudation of fibrinogen indicates severe vascular wall damage. In this study, the analysis of fibrinous exudate in the bile characteristic of acute biliary infection as a variable using single-factor and multi-factor regression analysis revealed that it is an independent risk factor for bile leakage postoperatively. In clinical practice, using basket retrieval for rotational removal, flushing of the bile duct is essential to ensure complete removal of intraluminal fibrinous covering, promoting smooth bile drainage and reducing the pressure buildup from bile stasis. Although the presence of fibrinous exudate in the common bile duct is an independent risk factor, the postoperative complication score for bile leakage (Clavien-Dindo classification) is grade 1, resolving with conservative observation. However, special attention is warranted for elderly patients, those with poor duodenal papillary function and patency, emphasizing cautious use of PDC.
Common suture techniques in clinical practice mainly include interrupted and continuous sutures; interrupted sutures are slower, have multiple knots, and are less effective in knotting outside the lumen, leading to slightly inferior hemostatic effects. The advantages of continuous sutures are less time-consuming, all knots are positioned outside the lumen, providing good hemostasis, yet disadvantages include a higher risk of tearing the thin and fragile bile duct wall, difficulty stitching into the biliary duct embedded in liver tissue, loose tying may result in bile leakage, while tight tension can lead to stricture at the anastomosis of tiny bile ducts.
Bile leakage post-PDC is often attributed to factors such as loose suture threads, minor leaks at the incision ends, or suture thread rupture at needle holes in thin-walled and narrow-bore bile ducts; increasingly, studies are optimizing the suture techniques for biliary ducts post-PDC, such as barbed suture (knotless) continuous sutures, layered sutures, full-thickness continuous eversion sutures, dual-needle bidirectional continuous sutures, and fibrin sealant coating[22-26]. Each suture technique has its advantages and disadvantages, balancing safety and trauma considerations, effectively reducing bile leak volume, and ease of adoption. These novel suture techniques have shown excellent clinical outcomes, worthy of further in-depth research in clinical practice.
Combining previous explorations, the author’s team has recently utilized the “continuous double-layer U-stitching technique,” achieving good clinical results. This technique can effectively prevent repeated pulling on the “first knot” and the suture segments (avoiding suture damage), reduce bile duct wall cutting (needle hole leaks), maintain consistent tension throughout (avoiding loose suture segments), promote tight and organized suture segments through a terminal “tissue knot,” effectively utilize peritoneal layer coverage to protect the biliary duct suture area, and reduce the impact of increased bile duct pressure on incision tension.
Jaundice resulting from elevated bilirubin levels can be roughly categorized as hepatocellular or obstructive; jaundice caused by biliary tract stones is primarily due to direct bilirubin elevation. Single-factor logistic regression analysis in this study indicates that the total bilirubin range for individuals without bile leakage is 43.91 ± 37.93 μmol/L, while the range for those with bile leakage is 21.13 ± 10.4 μmol/L, with a P value of 0.0422; the direct bilirubin ratio range for individuals without bile leakage is 0.87 ± 0.44, while that for individuals with bile leakage is 0.45 ± 0.28, with a P value of 0.0048, both being risk factors for postoperative bile leakage. Multi-factor logistic regression analysis demonstrates that the direct bilirubin ratio is an independent risk factor for bile leakage occurrence. This ratio is often overlooked in clinical practice, especially when the total bilirubin level is normal or mildly elevated, increasing the risk of bile leakage, emphasizing the need for further research and attention in clinical practice.
In the evaluation of duodenal papillary sphincter function, patency of the common bile duct and pancreatic duct, and successful completion of the learning curve for stone clearance, PDC remains the preferred method for biliary duct closure. The surgical strategy for common bile duct stones in the era of endoscopy needs further exploration and research in order to optimize management, improve patient outcomes, and minimize risks.
| 1. | Bosley ME, Cambronero GE, Sanin GD, Wood EC, Neff LP, Santos BF, Sudan R. Moving the needle for laparoscopic common bile duct exploration: defining obstacles for the path forward. Surg Endosc. 2024;38:6753-6761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Huang J, Chen H, Hu W, Liu J, Wei H, Tang X, Ran L, Fu X, Fang L. The feasibility and safety of laparoscopic transcystic common bile duct exploration after prior gastrectomy. Medicine (Baltimore). 2024;103:e38906. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Ramser B, Coleoglou Centeno A, Ferre A, Thomas S, Brooke M, Pieracci F, Morton A. Laparoscopic common bile duct exploration is an effective, safe, and less-costly method of treating choledocholithiasis. Surg Endosc. 2024;38:6076-6082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 4. | Wood EC, Gomez MK, Rauh JL, Saxena J, Conner J, Stettler GR, Westcott C, Nunn AM, Neff LP, Bosley ME. A Novel Taxonomy of Intraoperative Cholangiograms in Suspected Choledocholithiasis: A Tool for Advancing Laparoscopic Common Bile Duct Exploration Outcomes Research. Am Surg. 2025;91:7-11. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Podda M, Ielpo B. Invited Commentary to "Safety and Feasibility of Primary Closure Following Laparoscopic Common Bile Duct Exploration for Treatment of Choledocholithiasis" by Lunjian Xiang et al. World J Surg. 2023;47:1031-1032. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Xiang L, Li J, Liu D, Yan L, Zeng H, Liu Y. Correction: Safety and Feasibility of Primary Closure Following Laparoscopic Common Bile Duct Exploration for Treatment of Choledocholithiasis. World J Surg. 2023;47:1033. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Zhuang L, Li Y, Zhang L, Xu X, Sun D, Xi D, Lu Y. A comparison of the therapeutic outcomes between primary duct closure and T-tube drainage after laparoscopic common bile duct exploration: a single-centre retrospective study. Wideochir Inne Tech Maloinwazyjne. 2023;18:108-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 8. | Jiang Y, Lu J, Li W, Zhang J, Li L. Primary closure after laparoscopic common bile duct exploration is safe and feasible for patients with non-severe acute cholangitis. Langenbecks Arch Surg. 2022;407:1553-1560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 9. | Jiang Y, Zhang J, Li W, Li L. Primary closure versus T-tube drainage after laparoscopic common bile duct exploration in patients with non-severe acute cholangitis. Updates Surg. 2022;74:899-906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 10. | Feng Y, Zhang J, Jiao C, Zhu H, Cheng W, Xu S, Xiao B, Ni J, Chen X. Manometric Measurement of the Sphincter of Oddi in Patients with Common Bile Duct Stones: A Consecutive Study of the Han Population of China. Gastroenterol Res Pract. 2017;2017:9031438. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 11. | Liang T, Su W, Zhang Q, Li G, Gao S, Lou J, Zhang Y, Ma T, Bai X. Roles of Sphincter of Oddi Laxity in Bile Duct Microenvironment in Patients with Cholangiolithiasis: From the Perspective of the Microbiome and Metabolome. J Am Coll Surg. 2016;222:269-280.e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Muraki T, Memis B, Reid MD, Uehara T, Ito T, Hasebe O, Okaniwa S, Horigome N, Hisa T, Mittal P, Freedman A, Maithel S, Sarmiento JM, Krasinskas A, Koshiol J, Adsay V. Reflux-Associated Cholecystopathy: Analysis of 76 Gallbladders From Patients With Supra-Oddi Union of the Pancreatic Duct and Common Bile Duct (Pancreatobiliary Maljunction) Elucidates a Specific Diagnostic Pattern of Mucosal Hyperplasia as a Prelude to Carcinoma. Am J Surg Pathol. 2017;41:1167-1177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Masoni L, Mari FS, Pietropaolo V, Onorato M, Meucci M, Brescia A. Laparoscopic treatment for unsuspected common bile duct stones by transcystic sphincter of Oddi pneumatic balloon dilation and pressure-washing technique. World J Surg. 2013;37:1258-1262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Kouchi K, Takenouchi A, Matsuoka A, Yabe K, Yoshizawa H, Nakata C, Fujishiro J, Sugiyama H. Case Series of Endoscopic Papillary Balloon Dilation for Children with Common Bile Duct Stones and a Review of the Literature. J Clin Med. 2024;13:2251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 15. | Raza Z, Altayar O, Mahmoud T, Abusaleh R, Ghazi R, Early D, Kushnir VM, Lang G, Sloan I, Hollander T, Rajan E, Storm AC, Abu Dayyeh BK, Chandrasekhara V, Das KK. Clinical predictors of significant findings on EUS for the evaluation of incidental common bile duct dilation. Gastrointest Endosc. 2024;100:670-678.e1. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Wang ZX, Liu FL, Li L. Comparing percutaneous transhepatic papillary balloon dilation with endoscopic retrograde cholangiopancreatography in elderly patients for common bile duct stones: a 3-year retrospective study. Abdom Radiol (NY). 2024;49:2706-2713. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Tikhonova NB, Milovanov AP, Aleksankina VV, Fokina TV, Boltovskaya MN, Aleksankin AP, Artem'eva KA. Analysis of Healing of Rat Uterine Wall After Full-Thickness Surgical Incision. Bull Exp Biol Med. 2021;172:100-104. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Kobayashi M, Takai S, Sakurai K, Ehama Y. Impact of Different Treatments for Disseminated Intravascular Coagulation on Patients with or without Biliary Drainage for Severe Biliary Tract Infection. Open Access Emerg Med. 2023;15:437-445. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 19. | Lim KPK, Lee AJL, Jiang X, Teng TZJ, Shelat VG. The link between Helicobacter pylori infection and gallbladder and biliary tract diseases: A review. Ann Hepatobiliary Pancreat Surg. 2023;27:241-250. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 20. | Sharad N, Srivastava S, Ningombam A, Malhotra R, Mathur P. E. hirae Causing Biliary Tract Infection in a Patient with Cholangiocarcinoma: A Case Report. Infect Disord Drug Targets. 2023;23:e100523216757. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 21. | Zhang H, Cong Y, Cao L, Xue K, Qi P, Mao Q, Xie C, Meng Y, Cao B. Variability of bile bacterial profiles and drug resistance in patients with choledocholithiasis combined with biliary tract infection: a retrospective study. Gastroenterol Rep (Oxf). 2024;12:goae010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 22. | Fu Y, Wang S, Tan L, Liu Y. Celiac Axis Stenosis as an Independent Risk Factor for Bile Leakage in Laparoscopic Pancreaticoduodenectomy: A Retrospective Study. J Laparoendosc Adv Surg Tech A. 2024;34:682-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 23. | Kuraoka N, Ujihara T, Sakai S. Troubleshooting bile leakage after endoscopic ultrasound-guided hepaticogastrostomy with fully covered self-expandable metal stent deployment. J Hepatobiliary Pancreat Sci. 2024;31:e51-e52. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 24. | Matsubara S, Suda K, Nagoshi S. Immediate puncture of a dislocated partially covered self-expandable metal stent in endoscopic ultrasound-guided hepaticogastrostomy for prevention of bile leakage. Dig Endosc. 2024;36:1286-1287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 25. | Muranushi R, Harimoto N, Seki T, Hagiwara K, Hoshino K, Ishii N, Tsukagoshi M, Igarashi T, Watanabe A, Araki K, Shirabe K. Early drain removal after hepatectomy based on bile leakage prediction using drainage fluid volume and direct bilirubin level. Hepatol Res. 2024;54:1070-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 26. | Wu G, Li WY, Gong YX, Lin F, Sun C. Impact of open hepatectomy on postoperative bile leakage in patients with biliary tract cancer. World J Gastrointest Surg. 2024;16:67-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/