Published online Mar 27, 2025. doi: 10.4240/wjgs.v17.i3.100185
Revised: December 12, 2024
Accepted: January 13, 2025
Published online: March 27, 2025
Processing time: 116 Days and 1.3 Hours
Thirst management in convalescent patients recovering from a digestive surgery performed under general anesthesia requires attention. A simple, practical, and safe method can effectively relieve thirst symptoms in such patients.
To evaluate the enhanced recovery after surgery (ERAS)-based evidence-based care (EBC) plus ice stimulation therapy for thirst management of convalescent patients following digestive surgery performed under general anesthesia.
A total of 191 patients convalescing after digestive surgery performed under general anesthesia between March 2020 and February 2023 and experiencing thirst were selected. In total, 89 patients and 102 patients in the control and research groups received routine care and ERAS-based EBC plus ice stimulation therapy, respectively. The following data were comparatively analyzed: (1) Thirst degree (thirst intensity numerical rating scale) and thirst distress (TD) degree (TD scale); (2) Oral mucosal wetness; (3) Unstimulated whole salivary flow rate (UWSFR); (4) Adverse reactions (palpitation, fatigue, chapped lips, and nausea and vomiting); and (5) Nursing satisfaction.
After nursing, thirst degree and distress were statistically lower in the research group than in the control group. Additionally, compared with the control group, the research group exhibited a lower degree of oral mucosal wetness, higher UWSFR, fewer adverse reactions, and more total nursing satisfaction.
ERAS-based EBC plus ice stimulation therapy can effectively alleviate thirst in convalescent patients recovering from a digestive surgery performed under general anesthesia. It can alleviate xerostomia symptoms, reduce adverse reactions, and improve patient comfort.
Core Tip: After a digestive surgery performed under general anesthesia, thirst management in patients during the recovery phase requires great attention because patients who underwent such surgical procedures typically require an extended duration to revert to feasible and normal water consumption. This study aims to analyze the application of evidence-based care (EBC), based on enhanced recovery after surgery (ERAS), in conjunction with ice stimulation therapy, to address thirst management in convalescent patients who underwent digestive surgery under general anesthesia. A comprehensive analysis was performed to investigate various factors including degree of thirst, degree of thirst distress, wetness of the oral mucosa, unstimulated whole salivary flow rate, adverse reactions, and nursing satisfaction. Reportedly, ERAS-based EBC plus ice stimulation therapy effectively alleviated thirst severity experienced by patients convalescing after a digestive surgery performed under general anesthesia, ameliorated xerostomia symptoms, diminished adverse reactions, and augmented patient comfort. Moreover, the study furnished valuable clinical evidence concerning the prophylaxis and thirst treatment after digestive surgery under general anesthesia.
- Citation: Chen L, Li BX, Gan QZ, Guo RG, Chen X, Shen X, Chen Y. Enhanced recovery after surgery-based evidence-based care plus ice stimulation for thirst management in convalescent patients following digestive surgery under general anesthesia. World J Gastrointest Surg 2025; 17(3): 100185
- URL: https://www.wjgnet.com/1948-9366/full/v17/i3/100185.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i3.100185
Thirst is a natural response to the body’s sense of need to replenish water content. After surgery under general anesthesia, several patients experience varying degrees of thirst, primarily caused by prolonged fasting and water prohibition before and after surgery, endotracheal intubation during surgery, and anesthetic drugs[1]. Water consum
Enhanced recovery after surgery (ERAS) combines multidisciplinary knowledge and multiple modes of care for accelerating patient recovery by optimizing several perioperative care measures that reduce the stress response of surgery[5]. To achieve this goal and enhance the effectiveness of nursing, evidence-based care (EBC) uses scientific methods and evidence-based questions to collect nursing evidence and formulated scientific preventive measures for ameliorating adverse events catered to patient-specific needs and clinical experiences[6]. Thirst is a common and an uncomfortable issue experienced by several intensive care unit (ICU)-treated patients. The common clinical practice of using oral swabs and ice water sprays effectively reduces thirst and xerostomia symptoms[7]. Ice stimulation therapy uses low temperatures generated by spraying ice water and ice gargling to stimulate specific receptors in the oropharynx, which are known as transient receptor potential melastatin 8 on cold sensory receptors. When rapidly activated, these receptors present on the oral mucosa upon stimulation by ice and open a transient receptor potential channel[8], enhancing patient comfort and satisfaction and remarkably reducing the degree of thirst experienced by the patients, ultimately reducing their thirst-induced distress[9]. Reportedly, perioperative thirst is an intense discomfort experienced by patients immediately after surgery and is associated with high morbidity; additionally, providing patients with ice stimulation (popsicles) as a part of perioperative care can effectively alleviate thirst intensity[10].
This study included 191 patients who were convalescing after a digestive surgery performed under general anesthesia and comparatively analyzed the clinical effectiveness of ERAS-based EBC plus ice stimulation therapy for managing postoperative thirst in these patients and validating the clinical advantages of this combination therapy.
This retrospective study included 191 patients convalescing after a digestive surgery performed under general anesthesia between March 2020 and February 2023 and experienced thirst. The control and research groups included 89 cases and 102 cases of routine care and ERAS-based EBC plus ice stimulation therapy, respectively; both groups were clinically comparable regarding general information (P > 0.05).
Patients convalescing from digestive surgery performed under general anesthesia and experiencing thirst; who were > 18 years old, nonmechanically ventilated, and willing to accept the nursing method; with no history of audio-visual diseases.
However, patients with insufficient volume of jugular vein filling as indicated by ultrasound determination; oral diseases; history of clinically diagnosed xerostomia, diabetes insipidus, and other diseases causing abnormal fluid volume and thirst; unstable blood pressure, heart rate, and other vital signs and chronic diseases; and inability to cooperate with the investigation were excluded.
The control group received routine care interventions: Ward temperature (22 °C - 24 °C) and humidity (50%-60%) were maintained within the normal range. The members of the research team were provided with cotton swabs dipped in warm indoor water (maintained at 22 °C - 27 °C) to moisten the lips and mouths of the patients. Next, lip balm was applied to patients’ lips to prevent dryness. These care measures were serially performed seven times a day—three times in the morning and four times in the afternoon—with an interval of 1 hour between consecutive care sessions to ensure that the patients had sufficient time to relax. Moreover, to ensure that the patients could enjoy a peaceful lunch break, a 2-hour interval was arranged between the third and fourth nursing sessions. After each session, the used articles were promptly collected and disposed of owing to hygiene.
The research group received ERAS-based EBC plus ice stimulation therapy. Standard nursing protocol was followed, the room temperature and humidity were maintained at 22 °C - 24 °C and 50%-60%, respectively. A special elephant trunk-shaped spray nozzle (specification: (1) 30 mL; and (2) Material: Food-grade Pickering emulsion) connected to a spray bottle filled with ice sterilization water (0 °C - 6 °C) was used[11]. During the ice stimulation therapy, the spray nozzle was inserted deep into the patient’s mouth, and ice water was sprayed in the following order: (1) Upper jaw; (2) Left cheek; (3) Tongue surface; (4) Right cheek; and (5) Throat. Each area was sprayed three times to ensure sufficient moisture. After spraying ice water, lip balm was applied to the patients’ lips to keep them moisturized. While spraying iced water, the amount of liquid sprayed was controlled at approximately 0.1 mL, and the total amount of liquid in the entire spraying process was maintained at approximately 1.5 mL. During the nursing procedure, the patients’ vital signs were closely monitored to ensure their safety and comfort. Care measures were repeated seven times a day—thrice in the morning and four times in the evening. A 1-hour interval was maintained between consecutive sessions to ensure sufficient rest time. Similarly, to prevent disturbances during the patients’ lunch breaks, a 2-hour interval was arranged between the third and fourth operations. After each nursing operation, the used items were promptly disposed of to keep the environment clean and tidy.
Thirst degree and distress: The thirst intensity numerical rating scale (TINRS) was used to quantitatively evaluate thirst degree. TINRS is a straight line divided into 10 equal parts, each marked with a number ranging from 0 (no thirst) to 10 (extreme thirst) that represent different levels of thirst sensation. The patient was required to select a corresponding number representing their thirst level. A 10-point scoring system, the thirst distress (TD) scale was used for evaluating the degree of distress experienced by the patient because of thirst. A score of 0 indicates a lack of distress, whereas a score of 10 indicates a state of extreme discomfort experienced by the patient. The evaluator can directly question the patients regarding their thirst and distress, and based on the patients’ response and facial expressions, assign a score. A higher score indicated a greater distress.
Oral mucosal wetness: The wetness of the patients’ lips, tongue, and oral mucosa were examined to determine oral mucosal wetness, which was graded as follows: (1) 1 point, moist lips and mouth; (2) 2 points, dry lips but a moist mouth; (3) 3 points, dry lips and mouth; and (4) 4 points, peeling and chapped lips, in addition to dryness and paling of the mouth inside. This score reflects the degree of mouth moistness to assess possible thirst or other oral problems.
Unstimulated whole salivary flow rate: The cotton swab method was used to measure the unstimulated whole salivary flow rate (UWSFR) of patients. The specific operations were as follows: The saliva in the oral cavity was initially absorbed with cotton balls. Three preweighed dry cotton swabs were positioned in the patient’s mouth—one under the patient’s tongue and other two at the parotid glands on both sides. The patient was instructed to refrain from swallowing for 2 min, after which the cotton swabs were removed. The saliva on the patient’s tongue surface was again cleaned, and cotton swabs were reweighed. Their original weight was subtracted and the resulting weight was divided by 2 to get the patient’s UWSFR (in mg/minute).
Adverse reactions: The frequency of adverse reactions, such as palpitations, fatigue, chapped lips, and nausea and vomiting, was observed and recorded for evaluation.
Nursing satisfaction: A hospital-generated 100-point nursing satisfaction survey questionnaire was circulated among the patients to obtain feedback regarding nursing satisfaction. A score of ≥ 90 indicated “very satisfied”, 60-89 indicated “satisfied”, and < 60 indicated “dissatisfied”. Total satisfaction is the sum of very satisfied and satisfied as a percentage of the total number of cases.
Statistical Package for the Social Sciences 22.0 was used for all statistical analyses. The measurement and count data have been presented concerning the means ± SD and the number of cases (n) and percentage (%). Two independent samples, t-test and χ² test, were applied to the measurement and count data for identifying inter-group differences, with P < 0.05 as the statistical threshold.
The research and control groups matched with respect to age, weight, comorbidities, number of surgical procedures involved, and habitual water intake (P > 0.05) (Table 1).
| Indicators | Research group (n = 102) | Control group (n = 89) | χ²/t | P value |
| Age (years) | 48.51 ± 3.56 | 47.62 ± 3.44 | 1.751 | 0.082 |
| Weight (kg) | 58.59 ± 4.37 | 58.81 ± 5.62 | 0.304 | 0.762 |
| Sex | 1.998 | 0.158 | ||
| Male | 54 (52.94) | 38 (42.70) | ||
| Female | 48 (47.06) | 51 (57.30) | ||
| Comorbidities | 0.582 | 0.445 | ||
| Hypertension | 41 (40.20) | 31 (34.83) | ||
| Diabetes mellitus | 61 (59.80) | 58 (65.17) | ||
| Number of surgical procedures involved (item) | 1.163 | 0.281 | ||
| 1-2 | 64 (62.75) | 49 (55.06) | ||
| 3-4 | 38 (37.25) | 40 (44.94) | ||
| Habitual water intake (mL) | 2.060 | 0.560 | ||
| ≤ 500 | 22 (21.57) | 20 (22.47) | ||
| 501-1500 | 35 (34.31) | 23 (25.84) | ||
| 1501-2500 | 31 (30.39) | 29 (32.58) | ||
| ≥ 2501 | 14 (13.73) | 17 (19.10) |
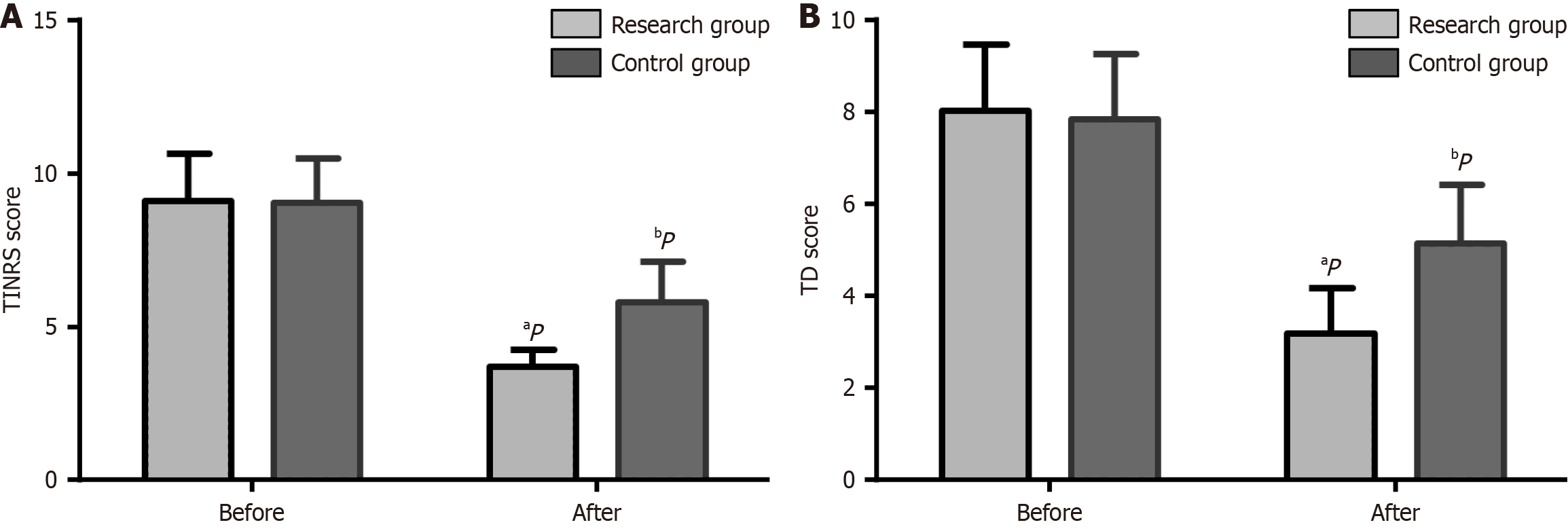
The research and control groups exhibited equivalent TINRS and TD scores before receiving care (P > 0.05) (Figure 1); The TINRS and TD scores of both groups decreased after nursing, with the scores of the research group being lower than the control group (P < 0.05).
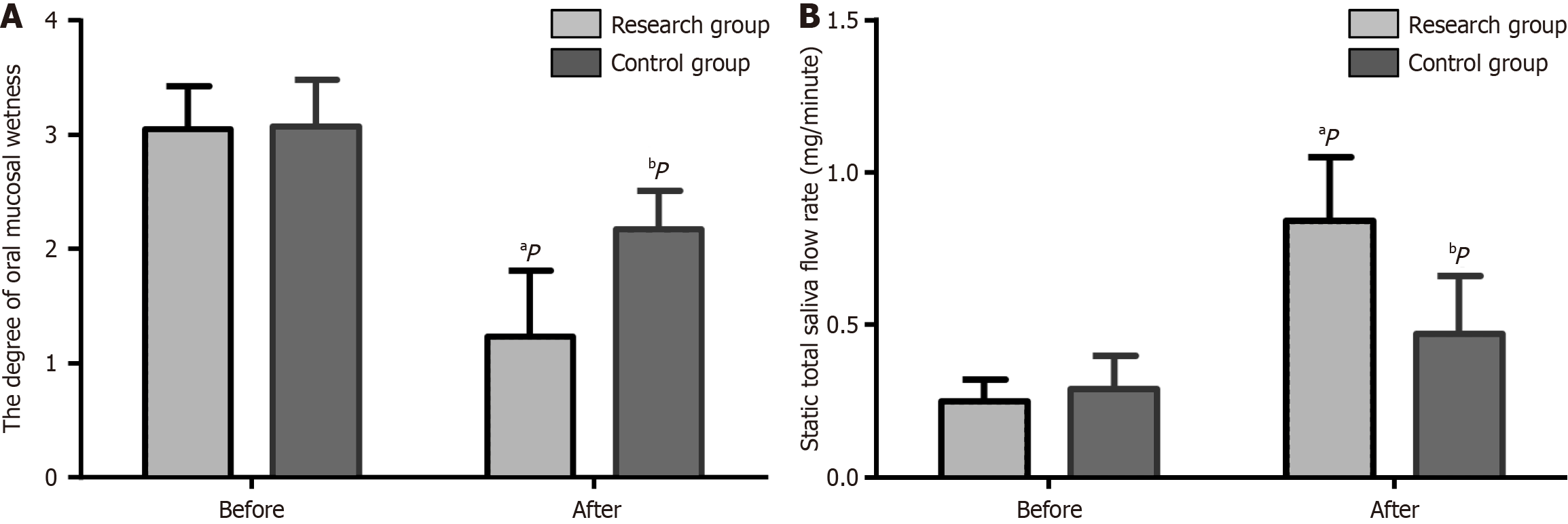
The oral mucosal wetness scores before care did not demonstrate any significant inter-group differences (P > 0.05). After receiving care, the oral mucosal wetness scores of both groups statistically decreased and were lower in the research group (P < 0.05) than the control group (Figure 2A).
Both groups had similar UWSFRs before receiving care (P > 0.05) (Figure 2B); the UWSFRs of both groups statistically increased after care and were higher in the research group than in the control group (P < 0.05).
An analysis of the number and percentage of cases of palpitations, fatigue, chapped lips, and nausea and vomiting in the two groups indicated that the total incidence of adverse reactions was lower in the research group (3.92%), compared with the control group (24.72%, P < 0.05) (Table 2).
| Indicators | Observation group (n = 102) | Control group (n = 89) | χ² | P value |
| Palpitations | 1 (0.98) | 3 (3.37) | ||
| Fatigue | 2 (1.96) | 6 (6.74) | ||
| Chapped lips | 0 (0.00) | 9 (10.11) | ||
| Nausea and vomiting | 1 (0.98) | 4 (4.49) | ||
| Total | 4 (3.92) | 22 (24.72) | 17.481 | < 0.001 |
The inter-group comparison revealed that the overall nursing satisfaction was higher in the research group (95.10%) than the control group (69.66%), with a statistical significance of P < 0.05 (Table 3).
| Indicators | Research group (n = 102) | Control group (n = 89) | χ² | P value |
| Very satisfied | 58 (56.86) | 19 (21.35) | ||
| Satisfied | 39 (38.24) | 43 (48.31) | ||
| Dissatisfied | 5 (4.90) | 27 (30.34) | ||
| Total satisfaction | 97 (95.10) | 62 (69.66) | 22.051 | < 0.001 |
Digestive surgeries are typically performed under general anesthesia for various surgical needs[12]. However, before receiving general anesthesia, patients fasted and abstained from ingesting any fluids pre-operatively and post-operatively, leading to prolonged inactivity of the digestive system and reduced secretion of digestive fluids and saliva[13,14]. Meanwhile, blood loss and cell dehydration during digestive surgeries can lead to hypovolemia, hemoconcentration, and increased plasma osmotic pressure, eventually leading to thirst[15]. Thirst causes discomfort in patients and enhances their stress responses, oxygen consumption, and metabolic burden, triggering negative emotions such as anxiety and irritability, affecting patient treatment and nursing compliance, and resulting in responses such as tube biting and unplanned extubations[16,17]. This study proposes ERAS-based EBC plus ice stimulation therapy and verifies its potential advantages in combating thirst experienced by patients undergoing digestive surgery under general anesthesia to provide useful clinical evidence for the prevention and treatment of thirst after surgeries conducted under general anesthesia.
By optimizing nursing procedures and controlling stress reactions, ERAS helps patients undergoing digestive surgeries under general anesthesia recover quickly and safely[18]. Herein, the evidence-based medicine was used as basis to ensure that nursing measures were scientifically validated, thereby improving nursing efficacy[19]. Moreover, EBC uses a rigorous and logical methodology, enabling us to accrue diverse information and evidence, accurately identify problems, and propose practical and effective solutions[20,21]. Thirst is a painful sensation experienced by patients following digestive surgery under general anesthesia. The timely resolution of thirst-related physiological problems is a concrete manifestation of effective nursing[22]. The use of cotton swabs dipped in water can alleviate thirst and distress; however, the effect is not ideal. Because the lips are not protected by the stratum corneum, moisturizing cotton swabs can dry the oral lip surface and even cause peeling. Therefore, the long-term thirst cannot be resolved by this method[23]. This study has been adopted the ERAS-based EBC plus ice stimulation therapy for the research group, which effectively alleviated the thirst degree and distress compared with routine care used for the control group after nursing, and indicates that the ice water spray used in this combination therapy can moisten the entire mouth by reaching the patient’s throat. Ma et al[11] reported that ice water spray was more effective as a topical intervention for moistening the lips than a cotton swab dipped in water. Ice water spray can transform liquid into a fine water mist that quickly and evenly covers all mouth corners through the nozzle. The mist forms a protective film that, apart from effectively moisturizing the oral mucosa, reduces the dry peeling of the lips and stimulates the throat to produce more saliva, further alleviating xerostomia symptoms and thirst. Reportedly, providing ice water stimulation interventions to adult patients with postoperative thirst can effectively alleviate the moistness of the oral mucosa and be instrumental in relieving thirst[24]. This might partially explain the efficacy of nursing interventions plus ice stimulation therapy in reducing postoperative thirst following digestive surgery under general anesthesia. Next, compared with the control group, the degree of the oral mucosal wetness after nursing was significantly lower in the research group, indicating that ERAS-based EBC plus ice stimulation therapy can ensure a significant moisturizing effect on the patient’s oral cavity by effectively moisturizing the entire oral mucosa and forming a protective film on its surface. Moreover, the UWSFR was higher in the research group after nursing than the control group, indicating that the ERAS-based EBC plus ice stimulation therapy effectively promotes salivary gland secretion and significantly improves the UWSFR in the oral cavity. This reduces the dryness of the patients’ mouth and effectively alleviates thirst symptoms. Further, this favorably enhances the patients’ oral health and digestive function, which can be attributed to the UWSFR augmentation that serves to diminishes the risk of oral infections. The enhanced saliva can effectively fulfill the cleansing functions and safeguarding of the oral cavity. Moreover, it enhances food digestion and facilitates the digestive process[25,26]. This also corroborates with Tsai et al’s findings, stating that oral stimulation with ice cubes or ice products can effectively relieve postoperative thirst[27]. In addition, this study demonstrated an evidently lower incidence of adverse reactions in the research group than in the control group, indicating that the ERAS-based EBC plus ice stimulation therapy can reduce the incidence of adverse reactions caused by thirst following digestive surgery. In addition, the application of ice-cold water spray in accordance with the symptom management mode for patients admitted to ICUs effectively alleviates postoperative thirst intensity, improves oral comfort, shortens nursing time, and improves patients’ satisfaction with nursing[28]. Herein, the research group expressed significantly higher overall nursing satisfaction compared with the control group, indicating that ERAS-based EBC plus ice stimulation therapy can effectively alleviate postoperative thirst and discomfort, maintain oral comfort and psychological satisfaction, and contribute to the emotional stability and physical and mental pleasure of patients, creating a positive impression regarding the nursing work.
The ERAS-based EBC plus ice stimulation therapy can effectively alleviate thirst in convalescent patients following digestive surgery under general anesthesia, thereby alleviating xerostomia symptoms, reducing adverse reactions, and enhancing patient satisfaction.
| 1. | Sobot Novakovic S, Cuk S, Svraka D, Milosevic D. Patient Satisfaction With General Anesthesia Compared to Spinal Anesthesia for Cesarean Section: A Multicenter Observational Study. Cureus. 2023;15:e42666. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Brady M, Kinn S, Stuart P. Preoperative fasting for adults to prevent perioperative complications. Cochrane Database Syst Rev. 2003;CD004423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 221] [Article Influence: 9.6] [Reference Citation Analysis (1)] |
| 3. | Marsman M, Kappen TH, Vernooij LM, van der Hout EC, van Waes JA, van Klei WA. Association of a Liberal Fasting Policy of Clear Fluids Before Surgery With Fasting Duration and Patient Well-being and Safety. JAMA Surg. 2023;158:254-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 49] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 4. | Yin X, Zeng X, Wang T, Dong B, Wu M, Jia A, Ye L. Early versus delayed postoperative oral hydration in children following general anesthesia: a prospective randomized trial. BMC Anesthesiol. 2020;20:174. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Coopmans L, Amaya Aliaga J, Metsemakers WJ, Sermon A, Misselyn D, Nijs S, Hoekstra H. Accelerated Rehabilitation in Non-operative Management of Acute Achilles Tendon Ruptures: A Systematic Review and Meta-analysis. J Foot Ankle Surg. 2022;61:157-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Crawford CL, Rondinelli J, Zuniga S, Valdez RM, Cullen L, Hanrahan K, Titler MG. Testing of the Nursing Evidence-Based Practice Survey. Worldviews Evid Based Nurs. 2020;17:118-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Puntillo K, Arai SR, Cooper BA, Stotts NA, Nelson JE. A randomized clinical trial of an intervention to relieve thirst and dry mouth in intensive care unit patients. Intensive Care Med. 2014;40:1295-1302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 96] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 8. | van Belzen L, Postma EM, Boesveldt S. How to quench your thirst. The effect of water-based products varying in temperature and texture, flavour, and sugar content on thirst. Physiol Behav. 2017;180:45-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Nakaya TG, Conchon MF, Garcia AKA, Uchôa ET, Fonseca LF. Effects of the ice popsicle on vasopressin, osmolality, thirst intensity, and thirst discomfort. Rev Gaucha Enferm. 2021;42:e20190449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 10. | Conchon MF, Fonseca LF. Efficacy of an Ice Popsicle on Thirst Management in the Immediate Postoperative Period: A Randomized Clinical Trial. J Perianesth Nurs. 2018;33:153-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 11. | Ma F, He H, Xu B, Zhou J, Pu K. Effect of sterile ice water versus menthol spray on thirst symptoms of fasted children in the intensive care unit: A prospective cohort study. Medicine (Baltimore). 2023;102:e33315. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 12. | Bazurro S, Ball L, Pelosi P. Perioperative management of obese patient. Curr Opin Crit Care. 2018;24:560-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 60] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 13. | Malbrain MLNG, Langer T, Annane D, Gattinoni L, Elbers P, Hahn RG, De Laet I, Minini A, Wong A, Ince C, Muckart D, Mythen M, Caironi P, Van Regenmortel N. Intravenous fluid therapy in the perioperative and critical care setting: Executive summary of the International Fluid Academy (IFA). Ann Intensive Care. 2020;10:64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 194] [Cited by in RCA: 180] [Article Influence: 30.0] [Reference Citation Analysis (1)] |
| 14. | González C, Garcia-Hernando G, Jensen EW, Vallverdú-Ferrer M. Assessing rheoencephalography dynamics through analysis of the interactions among brain and cardiac networks during general anesthesia. Front Netw Physiol. 2022;2:912733. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Kjeldsen CL, Hansen MS, Jensen K, Holm A, Haahr A, Dreyer P. Patients' experience of thirst while being conscious and mechanically ventilated in the intensive care unit. Nurs Crit Care. 2018;23:75-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 55] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 16. | Seyhan Ak E, Türkmen A, Sinmaz T, Biçer ÖS. Evaluation of Thirst in the Early Postoperative Period in Patients Undergoing Orthopedic Surgery. J Perianesth Nurs. 2023;38:448-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 17. | Wu C, Liu Y, Yang L, Tang Y, Zhou L, Wang X. Thirst Relief Effect of 0.75% Citric Acid Spray During the Anesthesia Recovery Period: A Randomized Controlled Trial. J Perianesth Nurs. 2021;36:642-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Xie J, Xia J, Ji Q, Wei HX, Li Y. [Application of the concept of accelerated rehabilitation surgery in the perioperative period of robot-assisted laparoscopic radical prostatectomy]. Zhonghua Nan Ke Xue. 2023;29:736-740. [PubMed] |
| 19. | Lv H, Yang N. Clinical effect of application of nursing concept of rehabilitation surgery for improvement of quality of postoperative recovery in orthopedics. J Orthop Surg Res. 2021;16:471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Cheng L, Feng S, Hu Y. Evidence-based nursing implementation in Mainland China: A scoping review. Nurs Outlook. 2017;65:27-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 21. | Zhao J, Liu X, Zhang W, Xing Y, Cho SW, Hao Y. Evidence-based nursing outputs and hot spot analysis of the last 5 years in mainland China: Results of a bibliometric analysis. Int J Nurs Pract. 2018;24:e12628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Yang HL, Liu FC, Tsay PK, Chou AH, Lin CC, Yu HP, Jao HC, Liu HE. Use of Transcutaneous Electrical Nerve Stimulation to Alleviate Thirst After Surgery: A Randomized Controlled Trial. J Perianesth Nurs. 2023;38:291-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 23. | Aroni P, Fonseca LF, Ciol MA, Margatho AS, Galvão CM. The use of mentholated popsicle to reduce thirst during preoperative fasting: A randomised controlled trial. J Clin Nurs. 2020;29:840-851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 24. | Silva TTMD, Dantas JKDS, Araújo SCM, Silva SO, Dantas DV, Dantas RAN. Strategies for thirst management in postoperative adult patients: a scoping review. Rev Bras Enferm. 2022;75:e20220154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 25. | Uchida H, Ovitt CE. Novel impacts of saliva with regard to oral health. J Prosthet Dent. 2022;127:383-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 42] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 26. | Shang YF, Shen YY, Zhang MC, Lv MC, Wang TY, Chen XQ, Lin J. Progress in salivary glands: Endocrine glands with immune functions. Front Endocrinol (Lausanne). 2023;14:1061235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 27] [Reference Citation Analysis (0)] |
| 27. | Tsai HY, Chao A, Hsiao WL. The effectiveness of cold oral stimuli in quenching postoperative thirst: A systematic review and meta-analysis. Intensive Crit Care Nurs. 2023;75:103359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 25] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 28. | Lian R, Zhou S, Guo Y, Liang H, Lin J, Li D, Wu W, Rao Y, Shao D, Zheng P, Yang X. The effect of ice-cold water spray following the model for symptom management on postoperative thirst in patients admitted to intensive care unit: A randomized controlled study. Intensive Crit Care Nurs. 2024;81:103571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 20] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/