Published online Feb 27, 2025. doi: 10.4240/wjgs.v17.i2.99826
Revised: November 4, 2024
Accepted: December 6, 2024
Published online: February 27, 2025
Processing time: 105 Days and 1.2 Hours
Surgery is the gold standard for gallstone treatment. Nevertheless, the compli
To examine the impact of perioperative comprehensive nursing on pain intensity, complication rates, and patient comfort in individuals undergoing gallstone sur
From February 2022 to February 2024, 195 patients who underwent gallstone surgery at Sanmen People’s Hospital were selected and divided into two groups: A control group receiving routine nursing care (95 patients) and a research group receiving perioperative comprehensive nursing (100 patients). Key postoperative recovery indicators, including time to first postoperative anal exhaust, oral food intake, and ambulation, were observed, along with pain intensity (measured by the numeric rating scale), complication rate (bleeding, incision infection, re
The research group showed significantly shorter times to first postoperative anal exhaust, oral intake, and ambulation. Moreover, numeric rating scale pain scores in the research group were markedly lower post-nursing, and the total complication rate was significantly reduced compared to the control group. Furthermore, comfort levels improved considerably in the research group, and World Health Organization Quality of Life-BREF scores across the physical, psychological, social, and environmental domains were significantly higher compared to the control group following nursing care.
Perioperative comprehensive nursing effectively enhances postoperative recovery in patients undergoing gallstone surgery, reducing pain, lowering complications, and improving patient comfort and quality of life, which deserves clinical application.
Core Tip: Gallstone surgery is the gold-standard treatment for gallstones; however, it may lead to complications and negatively impact patients’ health and quality of life. Perioperative care for patients undergoing gallstone surgery is essential to minimize postoperative complications as much as possible and enhance patient comfort and quality of life. In this study, comprehensive perioperative nursing was implemented for patients undergoing gallstone surgery and compared with routine care. Our results indicated that comprehensive perioperative nursing significantly promotes postoperative recovery, effectively alleviates pain, reduces overall complication rates, and improves patient comfort and quality of life, making it worthy of clinical promotion.
- Citation: Bao CY, Ding XK, Qi QF, Ye P, Fang ZJ. Effect of comprehensive perioperative nursing on pain intensity, complication rates, and comfort levels in patients undergoing gallstone surgery. World J Gastrointest Surg 2025; 17(2): 99826
- URL: https://www.wjgnet.com/1948-9366/full/v17/i2/99826.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i2.99826
Gallstones are common digestive system disorders, classified into cholesterol, pigment, and mixed stones, with cholesterol stones accounting for 90% of cases[1,2]. The risk of gallstones in adults ranges from 10% to 20%, and appro
Perioperative comprehensive nursing is a model that provides comprehensive care for patients at various stages-before, during, and after surgery, as well as post-discharge. This patient-centered approach develops customized nursing plans tailored to the patient’s needs and provides guidance on psychological support, disease awareness, health education, environmental adjustment, diet, pain management, and post-hospital care[8,9]. This model has shown clinical benefits for perioperative patients across various conditions. For example, its application in patients with esophageal cancer significantly reduces negative emotions and lowers medical costs, resulting in high satisfaction among patients and their families. In perioperative patients with brain tumors and epilepsy, it can reduce the risk of epilepsy recurrence, relieve pain and stress responses, and improve patient compliance and quality of life. Similarly, for patients with gynecological tumors, this approach effectively lowers the risk of gastrointestinal complications and promotes postoperative recovery[10-12]. Currently, few studies have examined the clinical effects of perioperative comprehensive nursing in patients undergoing gallstone surgery. This study aims to conduct a comprehensive evaluation focusing on pain intensity, complication rates, and patient comfort.
Inclusion criteria: All patients met the relevant diagnostic criteria for gallstones[13], satisfied the surgical indications, and had authentic and complete clinical data. Exclusion criteria: Patients with other severe gallbladder diseases, liver system disorders, serious infectious diseases, immune disorders, drug dependence, or malignancies were excluded. This retrospective study received approval from the ethics committee of Sanmen People’s Hospital. Through strict screening based on the above inclusion and exclusion criteria, 195 patients who underwent gallstone surgery in our hospital from February 2022 to February 2024 were selected and grouped according to the care they received: 95 patients receiving routine nursing were included in the control group, and 100 patients receiving perioperative comprehensive nursing were assigned to the research group.
The control group received conventional nursing care, including standard preoperative preparations, timely symptomatic treatments such as anti-infection measures and oxygen therapy after surgery, and perioperative therapeutic interventions. The research group received perioperative comprehensive nursing care, as follows.
Comprehensive preoperative nursing: Nurses gained an in-depth understanding of each patient’s condition through communication and provided tailored psychological support based on individual personality traits. Additionally, patients were educated on the procedures, including the principles, basic steps, and potential complications. Through this approach, most preoperative concerns and anxieties were alleviated, with assistance from family members, so patients could be in an optimal mental state before surgery.
Comprehensive intraoperative nursing: Operating room staff strictly adhered to aseptic protocols and assessed potential safety risks. Venous access was established, and patient privacy was protected. Nursing staff meticulously inspected surgical instruments to ensure functionality, assisted patients in achieving a comfortable posture, monitored vital signs, and adjusted room temperature and lighting during the operation. Additionally, attention was given to thermal insulation: The operating table was warmed, infusion liquids were prewarmed, and rinsing fluids were kept in a constant-temperature incubator. Given the frailty and brittle bones often associated with elderly patients, excessive traction was avoided. General anesthesia and endotracheal intubation were administered, with care taken to ensure the natural positioning of the arms to prevent tube kinking. During venipuncture, arms were not overlay abducted to avoid nerve damage. Furthermore, nurses closely monitored the procedures, assisted the surgeon by adjusting lighting and providing instruments, thereby ensuring smooth operations and minimizing surgical time.
Comprehensive postoperative care: Postoperatively, dietary intervention was customized based on the patient’s intestinal function and eating ability. For patients who could eat, palatable diets were prepared to increase protein intake and enhance their immunity, while those temporarily unable to eat were advised to begin eating 48 hours after surgery, with regular oral care to keep the mouth and lips moist. In addition, the type and degree of pain were evaluated in detail, and proactive pain management was conducted accordingly. Preemptive analgesia was administered to stabilize the patients’ moods, encouraging their active participation in treatment.
Comprehensive nursing after discharge: Discharge guidance was provided for patients to follow the doctor’s instructions, emphasizing taking choleretic drugs on time and doing moderate nonstrenuous physical activity. They were also advised to eat regularly, avoid irritating foods, and refrain from alcohol consumption. Moreover, patients were informed to have regular follow-ups.
Postoperative recovery: The time to first postoperative anal exhaust, oral food intake, and ambulation was recorded for both groups.
Pain intensity: Postoperative pain was assessed using the numeric rating scale[14], with scores ranging from 0 to 10. A score of 0 indicated no pain, 1-3 classified as mild pain (tolerable with pain only upon coughing or turning over), 4-6 indicated moderate pain (pain present when lying flat, turning over, or coughing, but able to sleep well), and 7-10 indicated severe pain (intense, unbearable pain preventing sleep).
Complication rate: Adverse events such as bleeding, incision infection, and recurrence were monitored and recorded for both groups, with the complication rate calculated.
Comfort: The visual analogue scale was used to assess comfort levels before and after surgery[15], with scores ranging from 0 to 10. Scores of 1-4, 5-7, and 8-10 indicated mild, moderate, and severe discomfort, respectively.
Quality of life: The World Health Organization Quality of Life-BREF (WHOQOL-BREF)[16] was used to evaluate patient’s quality of life. This scale contains 26 items, measuring four dimensions: Physiology, psychology, social re
This study utilized SPSS version 18.0 for statistical analysis. Categorial data were expressed as the number of cases with percentages [n (%)], while continuous data were presented as mean ± SEM. The χ2 test was used for comparing categorical data; an independent sample t-test was used for comparing continuous data between groups, and a paired t-test was used for comparisons before and after nursing within groups. A P value of less than 0.05 was considered statistically sig
The two patient cohorts did not show statistically significant differences in general characteristics such as sex, age, course of disease, history of alcoholism, smoking history, or family history of disease (P > 0.05) (Table 1).
| Indicators | Control group (n = 95) | Research group (n = 100) | χ2/t | P value |
| Sex (male/female) | 45/50 | 43/57 | 0.375 | 0.540 |
| Age (years old) | 49.03 ± 11.55 | 51.55 ± 12.95 | 1.431 | 0.154 |
| Course of disease (months) | 6.96 ± 1.92 | 7.20 ± 2.09 | 0.834 | 0.405 |
| History of alcoholism (Yes/No) | 22/73 | 24/76 | 0.019 | 0.890 |
| History of smoking (Yes/No) | 25/70 | 21/79 | 0.764 | 0.382 |
| Family disease history (Yes/No) | 9/86 | 7/93 | 0.396 | 0.529 |
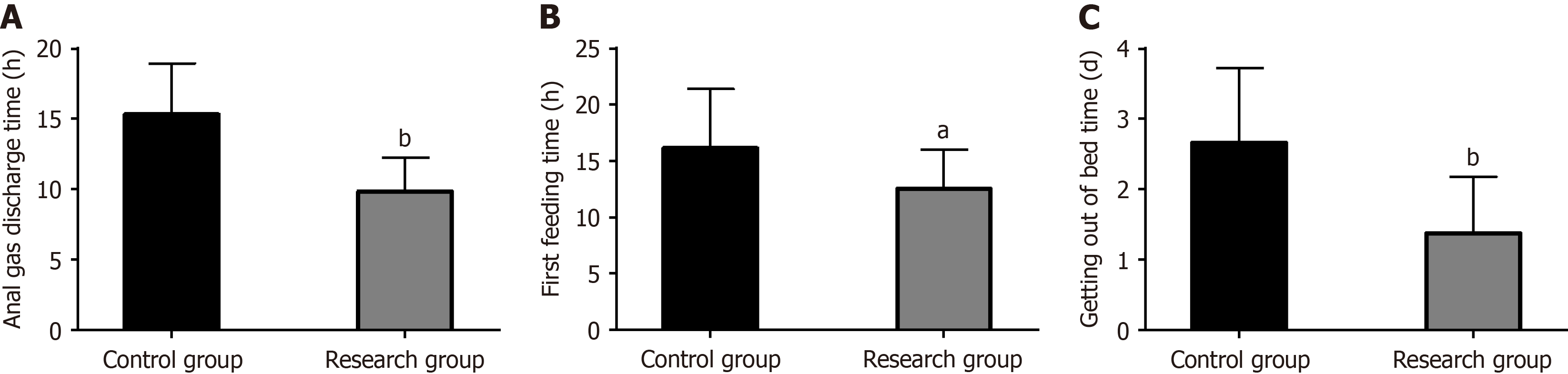
The research group exhibited significantly shorter times to first postoperative anal exhaust (9.85 ± 2.40 hours vs 15.33 ± 3.61 hours), oral food intake (12.51 ± 3.53 hours vs 16.13 ± 5.26 hours), and ambulation (1.38 ± 0.80 days vs 2.66 ± 1.06 days) compared to the control group (P < 0.05) (Figure 1 and Table 2).
| Indexes | Control group (n = 95) | Research group (n = 100) | t | P value |
| Time to first postoperative anal exhaust (hour) | 15.33 ± 3.61 | 9.85 ± 2.4 | 12.541 | < 0.001 |
| Time to first postoperative oral food intake (hour) | 16.13 ± 5.26 | 12.51 ± 3.53 | 5.669 | < 0.001 |
| Time to first postoperative ambulation (day) | 2.66 ± 1.06 | 1.38 ± 0.8 | 9.548 | < 0.001 |
Pain intensity, as assessed by the numeric rating scale, indicated that patients in the research group experienced significantly milder pain compared to the control group (P < 0.05) (Table 3).
| Indicators | Control group (n = 95) | Research group (n = 100) | χ2 | P value |
| Painless | 3 (3.16) | 18 (18.00) | 20.536 | < 0.001 |
| Mild pain | 21 (22.11) | 35 (35.00) | ||
| Moderate pain | 50 (52.63) | 38 (38.00) | ||
| Severe pain | 21 (22.11) | 9 (9.00) |
The incidence of complications, including bleeding, incision infection, and recurrence, was analyzed for both groups. The research group had a significantly lower overall complication rate than the control group (7.00% vs 21.05%; P < 0.05) (Table 4).
| Indicators | Control group (n = 95) | Research group (n = 100) | χ2 | P value |
| Hemorrhage | 8 (8.42) | 3 (3.00) | ||
| Incision infection | 7 (7.37) | 2 (2.00) | ||
| Recurrence | 5 (5.26) | 2 (2.00) | ||
| Total | 20 (21.05) | 7 (7.00) | 8.065 | 0.005 |
Patient comfort, assessed by the visual analogue scale, showed no significant difference between the two groups before surgery (P > 0.05). However, postoperatively, the research group showed significantly higher comfort levels than the control group (P < 0.05) (Table 5).
| Indicators | Control group (n = 95) | Research group (n = 100) | χ2 | P value |
| Before surgery | 0.500 | 0.779 | ||
| Slight discomfort | 16 (16.84) | 18 (18.00) | ||
| Moderate discomfort | 46 (48.42) | 52 (52.00) | ||
| Severe discomfort | 33 (34.74) | 30 (30.00) | ||
| After surgery | ||||
| Slight discomfort | 30 (31.58) | 48 (48.00) | ||
| Moderate discomfort | 44 (46.32) | 42 (42.00) | ||
| Severe discomfort | 21 (22.11) | 10 (10.00) | 7.981 | 0.019 |
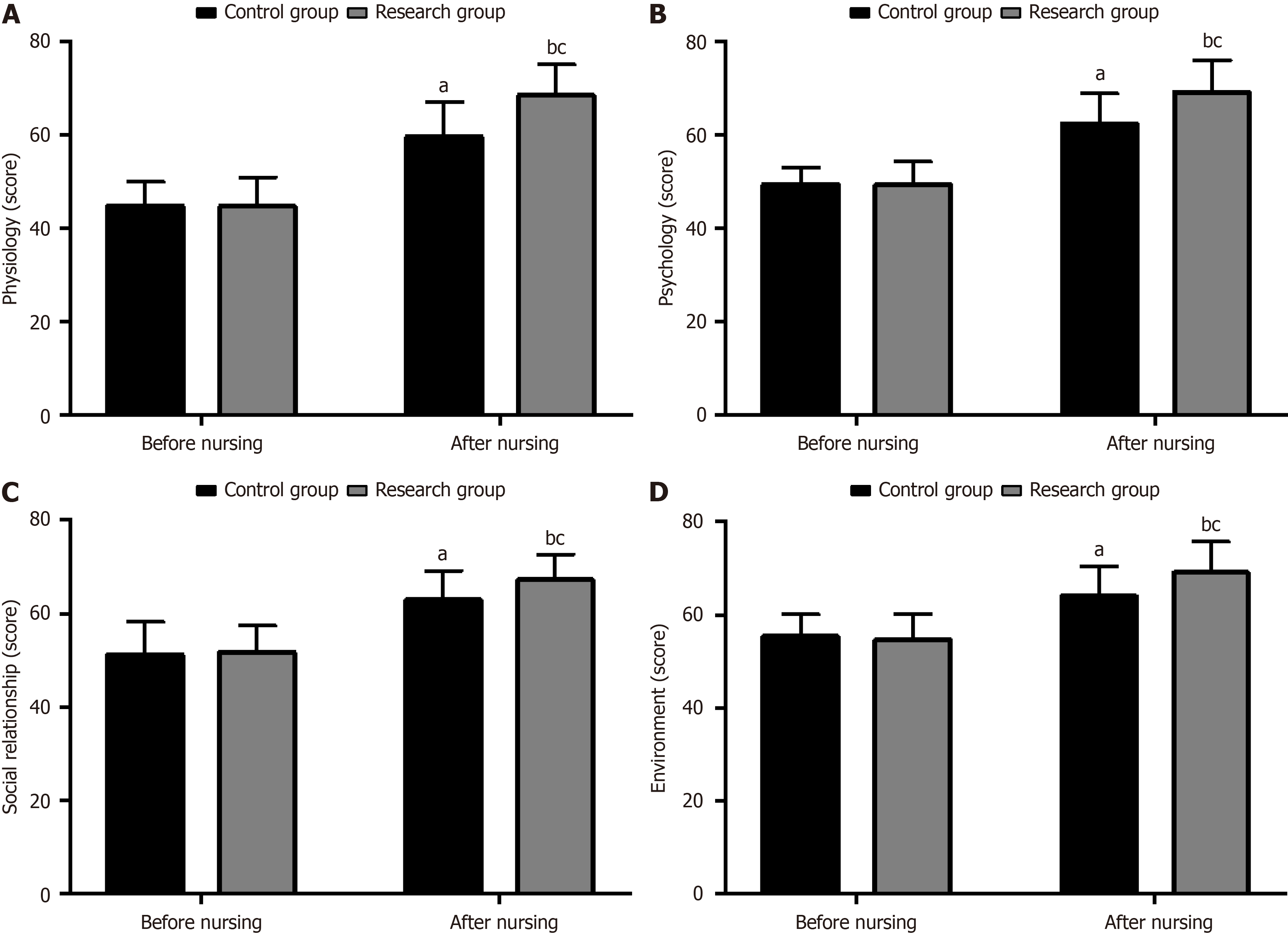
The WHOQOL-BREF scale was used to evaluate quality of life across four dimensions: Physiology, psychology, social relationships, and environment. No significant differences were observed between the groups before nursing (P > 0.05). In contrast, after nursing, scores in all dimensions significantly increased for both groups (P < 0.05), with the research group showing especially higher improvements (P < 0.05) (Figure 2 and Table 6).
| Indicators | Control group (n = 95) | Research group (n = 100) | t | P value |
| Before surgery | ||||
| Physiology | 44.79 ± 5.13 | 44.70 ± 6.21 | 0.110 | 0.913 |
| Psychology | 49.38 ± 3.61 | 49.32 ± 4.94 | 0.096 | 0.923 |
| Social relationship | 51.22 ± 6.97 | 51.78 ± 5.65 | 0.618 | 0.538 |
| Environment | 55.34 ± 4.79 | 54.65 ± 5.54 | 0.928 | 0.354 |
| After surgery | ||||
| Physiology | 59.57 ± 7.37 | 68.42 ± 6.54 | 8.880 | < 0.001 |
| Psychology | 62.27 ± 6.51 | 69.12 ± 6.79 | 7.184 | < 0.001 |
| Social relationship | 62.92 ± 6.27 | 67.22 ± 5.45 | 5.118 | < 0.001 |
| Environment | 64.05 ± 6.33 | 69.13 ± 6.58 | 5.489 | < 0.001 |
Gallstones are etiologically associated with abnormally elevated levels of cholesterol or bilirubin in the biliary tract or bile in the gallbladder, with the risk increasing with age and a higher predilection among women[17,18]. Although gallstone surgery is the gold-standard treatment for patients with this condition, with proven efficacy, it inevitably causes varying degrees of bodily damage as an invasive procedure[19]. Therefore, high-quality nursing is needed to reduce surgery-related damage and facilitate the patient’s smooth recovery.
First, we observed that the time to first postoperative anal exhaust, oral food intake, and ambulation was markedly shortened in the research group compared to the control group. This finding suggests that perioperative comprehensive nursing is more conducive to promoting postoperative rehabilitation in patients undergoing gallstone surgery. This improvement may be attributed to the preoperative health education and emotional support that helped the patients achieve the optimal surgical state, the comfort care and meticulous surgical assistance provided during the operation that minimized the operation time, and the scientifically effective and customized dietary plan developed based on the patients’ intestinal function and eating conditions after the operation, all of which promoted the patients’ physical recovery[20,21].
In the study by Xu et al[22], the use of perioperative comprehensive care in patients with intracranial aneurysms significantly shortened the length of hospital stay and promoted recovery, which aligns with our findings. According to the report by Zhong et al[23], perioperative comprehensive nursing applied to patients with ruptured ectopic pregnancy not only improved treatment outcomes but also significantly accelerated patient recovery, supporting our findings.
The evaluation of pain intensity revealed notably milder pain in the research group compared to the control group, suggesting that perioperative comprehensive nursing can significantly reduce postoperative pain in patients undergoing gallstone surgery. This effect may be related to the professional postoperative pain management provided by the nursing team. Targeted intervention programs based on the types and degrees of patients’ pain can effectively relieve post
After evaluating complications, we observed that the incidence of total complications, such as bleeding, incision infection, and recurrence, was significantly lower in the research group than in the control group. This indicates that perioperative comprehensive care for patients undergoing gallstone surgery is beneficial in reducing the risk of complications. This may be attributed to the comprehensive nature of perioperative nursing, which provides thorough care services for patients before, during, and after the operation, as well as after discharge. From the patient’s perspective, all details in various aspects are meticulously implemented, and careful observation and care are provided. Similarly, Xu et al[26] reported that perioperative comprehensive nursing effectively reduced preoperative anxiety and postoperative complications in patients undergoing laparoscopic cholecystectomy.
Subsequently, the comfort assessment showed a significantly higher comfort level in the research group compared to the control group, indicating that perioperative comprehensive nursing for patients undergoing gallstone surgery has a significant effect on improving comfort. This improvement may be due to the provision of comprehensive perioperative nursing interventions. Before the operation, effective communication is employed to dispel patients’ doubts and negative emotions as much as possible. During the operation, meticulous and comprehensive care is provided regarding body position, temperature, lighting, and thermal insulation for both the body and infusion. Postoperatively, comprehensive care in terms of diet, oral hygiene, and pain management is provided, while after discharge, thorough guidance on medication, exercise, lifestyle, and diet is provided. Through these measures, the physical and mental comfort of patients is ensured to the greatest extent possible.
Toğaç and Yılmaz[27] indicated that perioperative comprehensive nursing for patients undergoing laparoscopic cholecystectomy effectively alleviated anxiety and significantly enhanced comfort, aligning with our research results. The evaluation of patients’ quality of life further demonstrated significantly higher WHOQOL-BREF scores in physiology, psychology, social relationships, and environment in the research group compared to prepare levels and the control group. This indicates that perioperative comprehensive nursing is effective in enhancing the quality of life for patients undergoing gallstone surgery.
To a certain extent, the improvement in patients’ quality of life observed in this study can be attributed to the effective facilitation of postoperative recovery, significant alleviation of pain, efficient reduction of complication rates, and successful enhancement of comfort. In the study by Wei et al[28], perioperative comprehensive nursing for patients undergoing gallstone surgery not only significantly shortened the time to first postoperative anal exhaust, bowel movement, and mobilization, as well as hospitalization time, but also reduced the incidence of postoperative complications and improved patients’ quality of life, consistent with our observations. In the report by Yu and Tang[29], perioperative comprehensive nursing for colorectal cancer patients effectively shortened the recovery time for the first exhaust, food intake, and bowel sounds, reduced the risk of postoperative complications, and significantly improved self-care ability and quality of life, similar to our research findings.
This study has several limitations that require further improvement. To begin with, as a single-center study, the sample size is relatively small. Subsequent multicenter studies with larger sample sizes are necessary to ensure the representativeness of the sample and the generalizability of the results. Second, there has been no in-depth investigation into the risk factors influencing patient comfort or the incidence of complications. Analyses in these areas should be included to further optimize nursing measures. Lastly, long-term follow-up has not been conducted. Incorporating a follow-up period of 3 to 5 years or even longer would be beneficial for understanding the long-term clinical benefits of comprehensive perioperative nursing. We will continuously improve the study in these areas.
Overall, perioperative comprehensive nursing offers significant clinical advantages for patients undergoing gallstone surgery. These benefits primarily include accelerated postoperative rehabilitation, effective relief of postoperative pain, a reduced risk of total complications such as bleeding, incision infection, and recurrence, as well as significantly improved comfort and quality of life. Our findings provide additional options and clinical evidence for optimizing the management of patients undergoing gallstone surgery.
| 1. | Song Y, Ma Y, Xie FC, Jin C, Yang XB, Yang X, Long JY, Wang DX, Sang XT, Li LM, Zhao HT, Ning Y. Age, gender, geographic and clinical differences for gallstones in China: a nationwide study. Ann Transl Med. 2022;10:735. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 2. | Taylor DR, Crowther RS, Cozart JC, Sharrock P, Wu J, Soloway RD. Calcium carbonate in cholesterol gallstones: polymorphism, distribution, and hypotheses about pathogenesis. Hepatology. 1995;22:488-496. [PubMed] |
| 3. | Everhart JE, Ruhl CE. Burden of digestive diseases in the United States Part III: Liver, biliary tract, and pancreas. Gastroenterology. 2009;136:1134-1144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 511] [Cited by in RCA: 606] [Article Influence: 35.6] [Reference Citation Analysis (0)] |
| 4. | Sun H, Warren J, Yip J, Ji Y, Hao S, Han W, Ding Y. Factors Influencing Gallstone Formation: A Review of the Literature. Biomolecules. 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 114] [Article Influence: 28.5] [Reference Citation Analysis (0)] |
| 5. | Tanaka H, Imasato M, Yamazaki Y, Matsumoto K, Kunimoto K, Delpierre J, Meyer K, Zerial M, Kitamura N, Watanabe M, Tamura A, Tsukita S. Claudin-3 regulates bile canalicular paracellular barrier and cholesterol gallstone core formation in mice. J Hepatol. 2018;69:1308-1316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 6. | Stokes CS, Lammert F. Excess Body Weight and Gallstone Disease. Visc Med. 2021;37:254-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Jiang T, Zhang H, Yin X, Cai Z, Zhao Z, Mu M, Liu B, Shen C, Zhang B, Yin Y. The necessity and safety of simultaneous cholecystectomy during gastric surgery for patients with asymptomatic cholelithiasis. Expert Rev Gastroenterol Hepatol. 2023;17:1053-1060. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Partridge JSL, Ryan J, Dhesi JK; CPOC-BGS perioperative frailty guideline group. New guidelines for the perioperative care of people living with frailty undergoing elective and emergency surgery-a commentary. Age Ageing. 2022;51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 27] [Reference Citation Analysis (0)] |
| 9. | Harrison TG, Ronksley PE, James MT, Brindle ME, Ruzycki SM, Graham MM, McRae AD, Zarnke KB, McCaughey D, Ball CG, Dixon E, Hemmelgarn BR. The Perioperative Surgical Home, Enhanced Recovery After Surgery and how integration of these models may improve care for medically complex patients. Can J Surg. 2021;64:E381-E390. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Zhang XD, Zhao QY, Fang Y, Chen GX, Zhang HF, Zhang WX, Yang XP. Perioperative comprehensive supportive care interventions for chinese patients with esophageal carcinoma: a prospective study. Asian Pac J Cancer Prev. 2013;14:7359-7366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 11. | Jiang S, Li C, Hu S, Li Y, Wang Z, Bu Y. To Analyze the Application Value of Perioperative Nursing Care in Patients with Resected Brain Tumor Accompanied with Epileptic Symptoms under Cortical Electrocorticography Monitoring. J Healthc Eng. 2022;2022:4012304. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Spitz D, Chaves GV, Peres WAF. Impact of perioperative care on the post-operative recovery of women undergoing surgery for gynaecological tumours. Eur J Cancer Care (Engl). 2017;26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | European Association for the Study of the Liver (EASL). EASL Clinical Practice Guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 2016;65:146-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 444] [Cited by in RCA: 372] [Article Influence: 37.2] [Reference Citation Analysis (2)] |
| 14. | Sjölund BM, Mamhidir AG, Engström M. Pain prevalence among residents living in nursing homes and its association with quality of life and well-being. Scand J Caring Sci. 2021;35:1332-1341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Bielewicz J, Daniluk B, Kamieniak P. VAS and NRS, Same or Different? Pain Res Manag. 2022;2022:5337483. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 67] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 16. | Goes M, Lopes M, Marôco J, Oliveira H, Fonseca C. Psychometric properties of the WHOQOL-BREF(PT) in a sample of elderly citizens. Health Qual Life Outcomes. 2021;19:146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 17. | Lammert F, Gurusamy K, Ko CW, Miquel JF, Méndez-Sánchez N, Portincasa P, van Erpecum KJ, van Laarhoven CJ, Wang DQ. Gallstones. Nat Rev Dis Primers. 2016;2:16024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 590] [Cited by in RCA: 578] [Article Influence: 57.8] [Reference Citation Analysis (1)] |
| 18. | Völzke H, Baumeister SE, Alte D, Hoffmann W, Schwahn C, Simon P, John U, Lerch MM. Independent risk factors for gallstone formation in a region with high cholelithiasis prevalence. Digestion. 2005;71:97-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 152] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 19. | Latenstein CSS, Hannink G, van der Bilt JDW, Donkervoort SC, Eijsbouts QAJ, Heisterkamp J, Nieuwenhuijs VB, Schreinemakers JMJ, Wiering B, Boermeester MA, Drenth JPH, van Laarhoven CJHM, Dijkgraaf MGW, de Reuver PR; SECURE trial collaborators. A Clinical Decision Tool for Selection of Patients With Symptomatic Cholelithiasis for Cholecystectomy Based on Reduction of Pain and a Pain-Free State Following Surgery. JAMA Surg. 2021;156:e213706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Salazar Maya ÁM. Nursing Care during the Perioperative within the Surgical Context. Invest Educ Enferm. 2022;40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Akduran F, Karaca A, Eroglu SA. Effects of the supportive care needs of patients with cancer on their comfort levels. Int J Palliat Nurs. 2024;30:295-306. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Xu Y, Wang RY, Zhao YH. Effects of perioperative comprehensive nursing based on risk prevention for patients with intracranial aneurysm. Int J Clin Pract. 2021;75:e13761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 23. | Zhong L, Zhao Y, Zhu H. Randomized trial of the application value of comprehensive nursing intervention in the perioperative period of ruptured bleeding of ectopic pregnancy. Ann Palliat Med. 2021;10:4593-4600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 24. | Shellito AD, Dworsky JQ, Kirkland PJ, Rosenthal RA, Sarkisian CA, Ko CY, Russell MM. Perioperative Pain Management Issues Unique to Older Adults Undergoing Surgery: A Narrative Review. Ann Surg Open. 2021;2:e072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 25. | Gu YX, Wang XY, Chen Y, Shao JX, Ni SX, Zhang XM, Shao SY, Zhang Y, Hu WJ, Ma YY, Liu MY, Yu H. Optimizing surgical outcomes for elderly gallstone patients with a high body mass index using enhanced recovery after surgery protocol. World J Gastrointest Surg. 2023;15:2191-2200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (1)] |
| 26. | Xu Y, Wang H, Yang M. Preoperative nursing visit reduces preoperative anxiety and postoperative complications in patients with laparoscopic cholecystectomy: A randomized clinical trial protocol. Medicine (Baltimore). 2020;99:e22314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Toğaç HK, Yılmaz E. Effects of preoperative individualized audiovisual education on anxiety and comfort in patients undergoing laparoscopic cholecystectomy: randomised controlled study. Patient Educ Couns. 2021;104:603-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 28. | Wei L, Hong Q, Lin X, Chen Y, Yang F, Li F, Chen Y. Effect of comprehensive high-quality nursing care on postoperative complications, degree of pain, and nursing satisfaction in gallstone patients during perioperative period. Am J Transl Res. 2021;13:2678-2685. [PubMed] |
| 29. | Yu S, Tang Y. Effects of comprehensive care on psychological emotions, postoperative rehabilitation and complications of colorectal cancer patients after colostomy. Am J Transl Res. 2021;13:6889-6896. [PubMed] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/