Published online Feb 27, 2025. doi: 10.4240/wjgs.v17.i2.102105
Revised: November 11, 2024
Accepted: December 19, 2024
Published online: February 27, 2025
Processing time: 105 Days and 4.6 Hours
Pancreaticobiliary maljunction (PBM) is a rare congenital abnormality in pancreaticobiliary duct development. PBM is commonly found in children, and it often leads to acute pancreatitis and other diseases as a result of pancreaticobiliary reflux. Roux-en-Y choledochojejunostomy is a common surgical method for the treatment of PBM, but there are several associated complications that may occur after this operation.
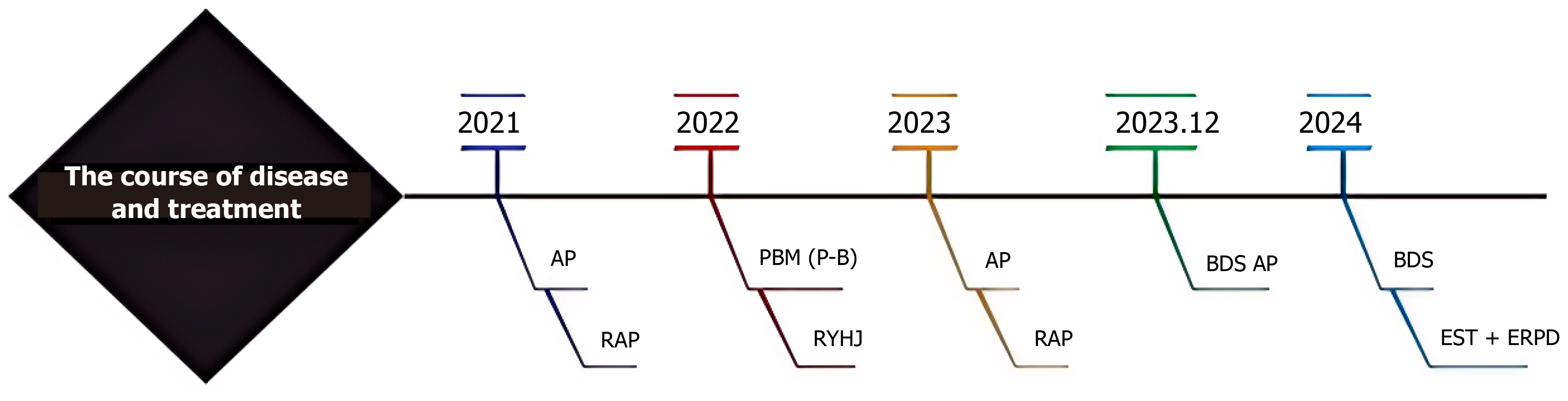
The patient, a 12-year-old female, was hospitalized nearly 20 times in 2021 for recurrent acute pancreatitis. In 2022, she was diagnosed with PBM and underwent laparoscopic common bile duct resection and Roux-en-Y choledochojejunostomy in a tertiary hospital. In the first year after surgery, the patient had more than 10 recurrent acute pancreatitis episodes. After undergoing abdominal computed tomography and other examinations, she was diagnosed with “residual bile duct stones and recurrent acute pancreatitis”. On January 30, 2024, the patient was admitted to our hospital due to recurrent upper abdominal pain and was cured through endoscopic retrograde cholangiopancreatography.
This article reports a case of a child with distal residual common bile duct stones and recurrent acute pancreatitis after Roux-en-Y choledochojejunostomy for PBM. The patient was cured through endoscopic retrograde cholangiopancreatography.
Core Tip: This paper reports a case of common bile duct stump stones and recurrent acute pancreatitis in a child after Roux-en-Y choledochojejunostomy was performed to treat pancreaticobiliary maljunction. She was cured through endoscopic retrograde cholangiopancreatography, and this successful case provides a valuable reference for the clinical treatment of postoperative gastrointestinal diseases in the future, and helps to reduce the incidence and mortality of patients.
- Citation: Li JF, Xie MJ, Wei JX, Yang CN, Chen GW, Li LQ, Zhao YN, Liu LJ, Xie S. Common bile duct stump stones and recurrent acute pancreatitis after Roux-en-Y choledochojejunostomy in a child: A case report. World J Gastrointest Surg 2025; 17(2): 102105
- URL: https://www.wjgnet.com/1948-9366/full/v17/i2/102105.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i2.102105
Pancreaticobiliary maljunction (PBM) is a congenital abnormality in pancreaticobiliary duct development[1]. PBM is commonly found in children and often leads to acute pancreatitis and other diseases due to pancreaticobiliary reflux. Roux-en-Y choledochojejunostomy is a representative surgical method for the treatment of PBM that aims to separate pancreatic juice and bile, prevent cholestasis and pancreatic juice reflux, and address PBM-induced acute pancreatitis. However, the distal residual common bile duct, which is used as a drainage channel for pancreatic juice post-transection, can cause pancreatic juice accumulation and reflux, leading to complications, such as recurrent acute pancreatitis (RAP) and even the formation of common bile duct stones. Here we report the case of a child who was treated with distal residual common bile duct stones and RAP after Roux-en-Y choledochojejunostomy and was cured by endoscopic retrograde cholangiopancreatography (ERCP). This case report is presented along with a literature review on the topic.
The patient, a 12-year-old female, was admitted to the hospital because of recurrent upper abdominal pain that had persisted for more than 3 years.
The patient presented with recurrent upper abdominal pain.
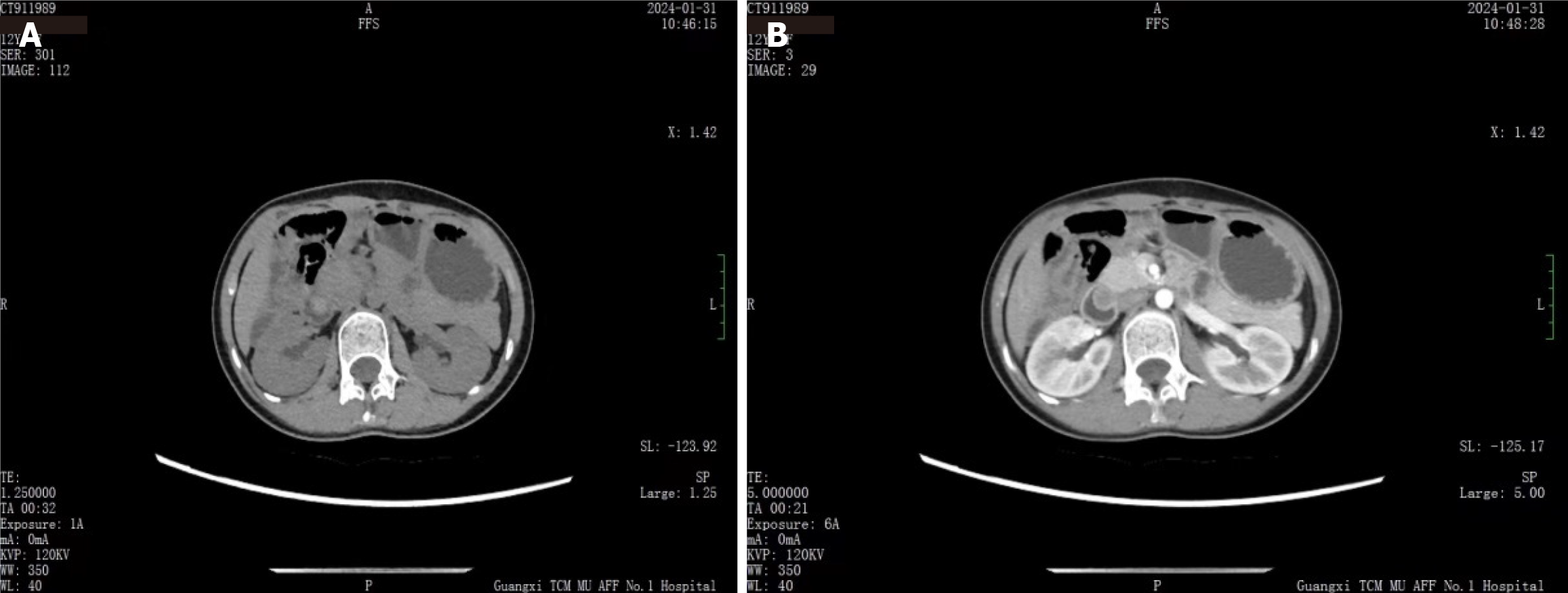
The patient had been hospitalized nearly 20 times in 2021 due to RAP and was diagnosed with abnormal pancreaticobiliary junction in 2022. The patient underwent laparoscopic choledochectomy and Roux-en-Y anastomosis of the common hepatic duct and jejunum at a tertiary hospital. Nearly 1 year after the operation, the patient continued to experience RAP more than ten times. In December 2023, the patient experienced recurrent abdominal pain, and abdominal computed tomography (CT) at another hospital showed changes after cholecystectomy, stones in the ampullary region of the common bile duct, and unclear margins around the head of the pancreas.
The patient was born in Laibin, Guangxi Zhuang Autonomous Region, and had lived in Laibin for a long time. She had no history of living in epidemic areas, no history of contact with infected water and epidemic sources, no history of radiation or poison exposure, no drug exposure history, no smoking history, and no alcohol consumption history.
After admission, the patient’s initial vital signs were: Body temperature, 36 °C; pulse, 94 times/minute; breath, 20 times/minute; blood pressure, 94/59 mmHg; height, 148 cm; body weight, 36 kg; body mass index, 16.44; and body surface area, 1.21 m2.
After admission, the serum amylase and lipase levels were 155 U/L and 70.7 U/L (both by enzyme colorimetry), respectively, with normal liver function.
The abdominal CT examination showed changes after cholecystectomy, with stones in the ampullary region of the common bile duct (Figure 1).
The diagnosis of RAP was confirmed by the patient’s medical history and imaging data[2], and the symptoms were relieved through conservative treatments such as fluid replacement, anti-inflammatory therapy, and inhibition of pancreatic enzyme secretion.
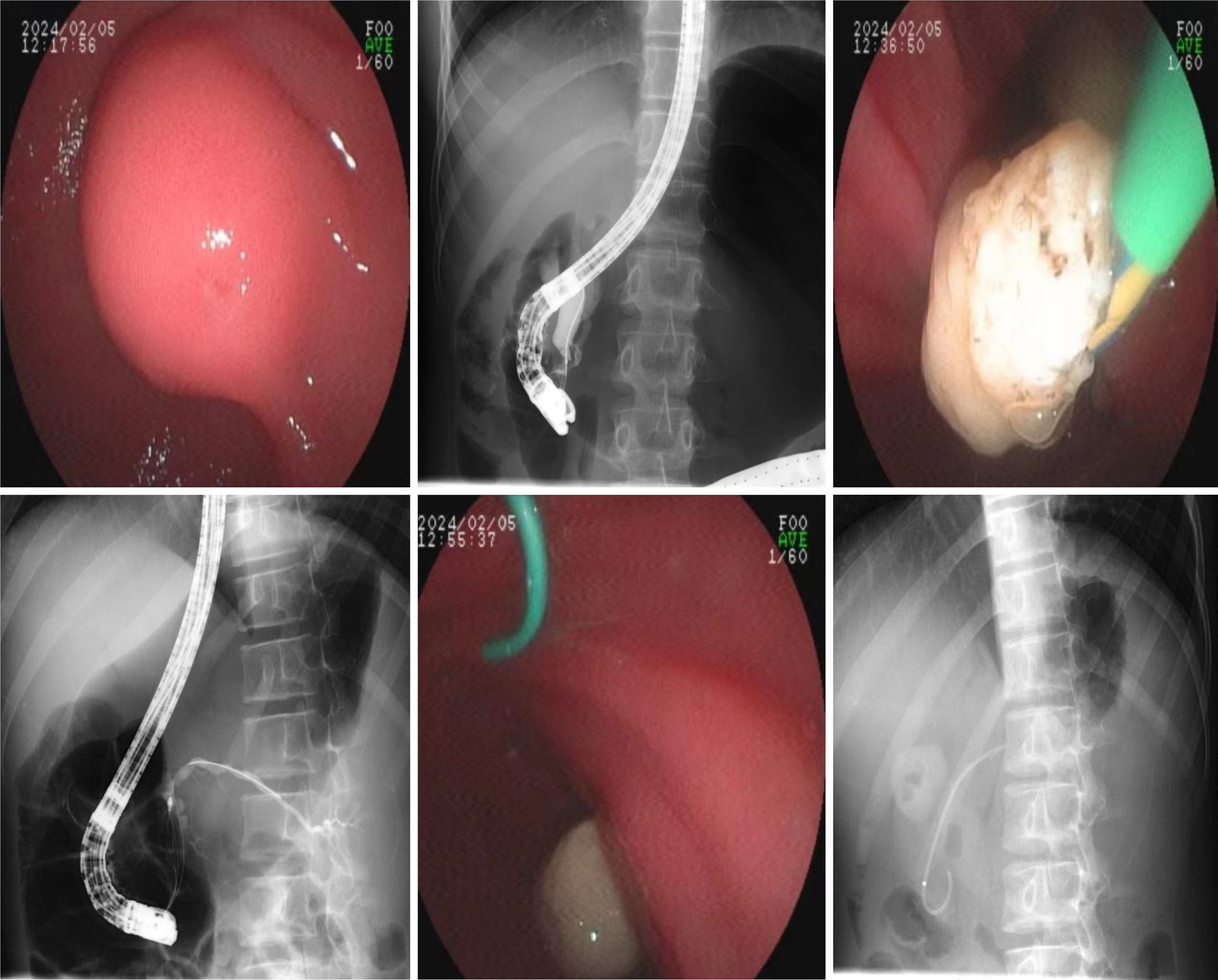
Based on the medical history and CT findings, the RAP was attributed to stones in the ampullary region of the common bile duct, which caused poor pancreatic juice removal. On February 5, 2024, ERCP was performed under duodenoscopy (Figure 2). The duodenal papilla appeared enlarged with a granular opening. The common bile duct stump was successfully intubated with a guide wire using a three-lumen smart knife, and no bile was observed after decompression. The common bile duct stump was shown by angiography, and a filling defect was found in the lower part of the common bile duct, measuring approximately 1.2 cm × 1.0 cm. The pancreatic duct was visualized with low confluence in the lower part of the common bile duct. After careful manipulation with a smart knife, the papilla was significantly dilated without bleeding. A stone basket was inserted to extract a white stone, approximately 1.2 cm × 1.0 cm in size, along with a large number of sediment stones. Subsequent basket angiography revealed no residual stones. The pancreatic duct was successfully reintubated, and a 5 French × 7 cm pancreatic duct stent was placed along the guide wire.
The patient experienced prompt relief from postoperative abdominal pain, resumed diet on day 3 after the operation, and was discharged on day 4 with no complications. The patient was followed up for 3 months postoperatively with no abdominal pain or recurrence of pancreatitis. On May 5, 2024, a follow-up abdominal CT scan was performed, and the pancreatic stent was removed. The patient’s condition has remained stable since the removal of the pancreatic stent. The patient’s medical history and treatment process are outlined (Figure 3).
PBM is caused by the confluence of the pancreatic and bile ducts in the duodenal wall in advance, forming a long common channel. Therefore, the sphincter of Oddi (SO) cannot control the confluence of the pancreaticobiliary ducts, leading to the reflux, mixture, and accumulation of pancreatic juice and bile, resulting in biliopancreatic duct-related diseases[1]. PBM is more common in girls aged younger than 10 years, with an incidence rate in the East of approximately 1/1000, which is higher than that in the West[3]. The underlying mechanism of PBM has not been fully elucidated, but its occurrence may be related to abnormal embryonic development, including ventral pancreatic dysplasia and stagnation of pancreaticobiliary junction migration into the duodenal wall[1]. PBM can be divided into two types: Biliary dilatation and non-dilation of the bile duct. The clinical manifestations of biliary dilatation-type PBM include recurrent abdominal pain, intermittent jaundice, and abdominal mass, which are often complicated with RAP, cholangitis, and common bile duct stones, while the clinical manifestations of non-dilation of the bile duct are relatively hidden and are generally found in adulthood[4]. PBM can be divided into three types according to the anatomy, namely the angle of the junction of the pancreatic duct and the bile duct[5]: (1) The common bile duct converges at a right angle to the pancreatic duct (B-P type); (2) The main pancreatic duct converges at an acute angle to the common bile duct (P-B type); and (3) The pancreaticobiliary junction neither belongs to B-P nor P-B, namely the complex type.
PBM can be diagnosed by imaging examinations such as magnetic resonance cholangiopancreatography, intraoperative cholangiography, percutaneous transhepatic cholangiography, endoscopic ultrasonography, multi-slice spiral CT, multi-slice spiral CT multi-plane three-dimensional reconstruction, intravenous infusion CT cholangiography, ERCP, or by surgery, autopsy, or other anatomical examinations[6]. As PBM is a risk factor for cholangiocarcinoma, early surgical or endoscopic treatment is recommended upon diagnosis to prevent the development of biliary tumors, regardless of the presence of clinical symptoms. Surgical treatment includes cholecystectomy, extrahepatic cholangioectomy, and Roux-en-Y reconstruction of the hepatic duct-jejunum[4]. Endoscopic treatments include ERCP common bile duct stone removal, pancreatic duct stone removal, pancreaticobiliary stent placement, and pancreaticobiliary dilatation[7].
In this report, the patient was a female who was younger than 10 years at the time of onset and experienced recurrent abdominal pain. Because the SO could not control confluence of the pancreaticobiliary ducts, the pancreatic juice and bile mixed and refluxed into the pancreatic duct, and the patient had experienced acute pancreatitis nearly 20 times within 1 year before the diagnosis of PBM. At the same time, ERCP revealed that the main pancreatic duct converged at an acute angle at the lower segment of the common bile duct, and the common bile duct opened separately at the duodenal papilla, confirming the type P-B defect. After the diagnosis of PBM, Roux-en-Y choledochojejunostomy was performed.
As a representative surgical method for the treatment of PBM, Roux-en-Y choledochojejunostomy advocates that the resection range should be up to the confluence of the left and right hepatic ducts and down to the common channel of the common bile duct. This procedure can achieve the separation of pancreatic juice and bile, prevent cholestasis and pancreatic juice reflux, and prevent the occurrence of PBM-induced acute pancreatitis. RAP after Roux-en-Y choledochojejunostomy is rarely reported. In this case, the patient had acute pancreatitis nearly 20 times due to PBM and underwent Roux-en-Y choledochojejunostomy. However, within 1 year after the operation, the patient still had more than ten acute pancreatitis attacks. CT examination showed ampullary calculi in the common bile duct, but no ERCP or surgical treatment was performed. ERCP revealed a large number of stones in the residual bile duct, which obstructed the outflow tract of pancreatic juice and led to RAP. However, the mechanism underlying common bile duct stump stones remains unclear. Some scholars believe that the blind loop syndrome of common bile duct stumps caused by SO dysfunction is related. Jiang et al[8] have even coined the term pancreatic common bile duct stones, positing that the primary cause may be attributed to pancreaticobiliary reflux triggered by pancreatic duct anomalies.
Under normal physiological conditions, the tonic contraction of SO can maintain the tightness of the biliary tract and pancreatic duct, preventing intestinal bile (pancreatic) reflux and bacterial retrogression. Time-varying contraction can not only assist in maintaining the base pressure of SO and regulating the pressure of the common bile and pancreatic ducts but can also discharge small stones, tissue fragments, and bacteria in the biliopancreatic outflow tract through continuous contraction and relaxation, thus maintaining the patency and relative sterility of the biliopancreatic outflow tract. However, for the child with PBM, due to premature convergence of the main pancreatic duct and the common bile duct outside the duodenal wall, an overlong common channel limits the ability of SO to control the patency of the bile and pancreatic ducts. This phenomenon results in elevated pressure in both ducts, leading to inadequate discharge of pancreatic juice and bile, causing reflux into the pancreatic duct and triggering acute pancreatitis. Therefore, the patient had experienced repeated acute pancreatitis nearly 20 times before being diagnosed with PBM.
However, the patient still experienced more than 10 acute pancreatitis episodes after Roux-en-Y choledochojejunostomy. From our point of view, although bile diversion after choledochojejunostomy avoids bile reflux, it still cannot solve the problem of an overlong common channel, and there is still high pressure of the pancreatic juice outflow, forcing the pancreatic juice to reflux into the pancreatic duct and repeatedly inducing acute pancreatitis. At the same time, due to the child’s P-B-type pancreas divisum, the pancreatic juice converges from the main pancreatic duct to the common bile duct and then converges to the common channel through the common bile duct sphincter. As the bile is diverse after choledochojejunostomy, the lack of direct bile stimulation of the common bile duct sphincter may lead to impairment of the contractile function of the common bile duct sphincter, affecting the discharge of pancreatic juice, resulting in localized accumulation in the common bile duct stump and finally in the formation of stones. This localized accumulation and stone formation can obstruct pancreatic juice discharge, increase pancreatic duct pressure, cause acute pancreatitis, and create a vicious cycle. Therefore, the patient still experienced RAP after Roux-en-Y choledochojejunostomy, leading to the formation of common bile duct stump stones. In the long term, malignant transformation of the common bile duct stump may occur, even in patients with residual common bile duct cancer[1].
Regarding stones and RAP in the common bile duct stump after Roux-en-Y choledochojejunostomy, we believe that the key to treatment is to remove the duodenal papilla obstruction as soon as possible, clear the stones that remain in the common bile duct stump, and keep the pancreatic duct drainage unobstructed. In this case, the child underwent endoscopic sphincterotomy (EST) and biliary sphincterotomy under ERCP, with a pancreatic duct stent placed for direct drainage of the pancreatic duct and duodenum. With micro-reconstruction of the abnormal confluence of the pancreatic and bile ducts under ERCP, the pressure of the common channel was reduced, pancreatic juice drainage was promoted, pancreatic juice reflux and local accumulation were prevented, and the formation of common bile duct stones was avoided. The short-term effect was satisfactory, but the long-term efficacy requires further evaluation. In this case, pancreatic duct stent drainage was temporary. Whether acute pancreatitis and distal residual common bile duct stones recur after removal of the pancreatic duct stent, or even residual common bile duct malignant transformation, remains a long-term issue that requires close attention. However, some literature reports[7,9,10] that EST may be suitable for the treatment of some PBM. Preventing the development of “reflux-inflammation-atypical hyperplasia-carcinogenesis” can not only avoid the induction of biliary tumors but also relieve the complications of pancreatic duct stones, acute pancreatitis, and other diseases. Therefore, it is also promising that EST can improve long-term treatment efficacy in such cases. As a result, long-term follow-up, close monitoring, and regular evaluation are needed after surgery. If the abovementioned situation occurs, ERCP is needed to re-place the pancreatic stent and replace it regularly. Surgical treatment, such as pancreatic-intestinal anastomosis, may also be considered.
In this report, it is found that RAP in children with PBM is easily ignored clinically. Relevant imaging examinations should be promptly improved, and ERCP should be performed when necessary to prevent missed diagnoses and misdiagnoses. Once PBM is diagnosed, clinicians should comprehensively consider multiple factors based on the different conditions of the children and choose appropriate treatment methods. Children with PBM are at risk of recurrence of RAP and formation of common bile duct stump stones after bilioenteric Roux-en-Y anastomosis. For the diagnosis and treatment of postoperative common bile duct stump stones and RAP, early ERCP examination is important to prevent delayed diagnosis and treatment. At the same time, there are still hidden risks of recurrence, infection, and carcinogenesis of RAP and common bile duct stump stones after ERCP. Long-term follow-up and review are still needed, and endoscopic and surgical interventional treatment should be performed again when necessary.
The authors would like to convey their heartfelt appreciation to the researchers who generously shared the data we utilized.
| 1. | Kamisawa T, Kaneko K, Itoi T, Ando H. Pancreaticobiliary maljunction and congenital biliary dilatation. Lancet Gastroenterol Hepatol. 2017;2:610-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 91] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 2. | Khurana V, Ganguly I. Recurrent acute pancreatitis. JOP. 2014;15:413-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 3. | Ono A, Arizono S, Isoda H, Togashi K. Imaging of Pancreaticobiliary Maljunction. Radiographics. 2020;40:378-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 4. | Ishibashi H, Shimada M, Kamisawa T, Fujii H, Hamada Y, Kubota M, Urushihara N, Endo I, Nio M, Taguchi T, Ando H; Japanese Study Group on Congenital Biliary Dilatation (JSCBD). Japanese clinical practice guidelines for congenital biliary dilatation. J Hepatobiliary Pancreat Sci. 2017;24:1-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 104] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 5. | Komi N, Tamura T, Miyoshi Y, Kunitomo K, Udaka H, Takehara H. Nationwide survey of cases of choledochal cyst. Analysis of coexistent anomalies, complications and surgical treatment in 645 cases. Surg Gastroenterol. 1984;3:69-73. [PubMed] |
| 6. | Kamisawa T, Ando H, Hamada Y, Fujii H, Koshinaga T, Urushihara N, Itoi T, Shimada H; Japanese Study Group on Pancreaticobiliary Maljunction. Diagnostic criteria for pancreaticobiliary maljunction 2013. J Hepatobiliary Pancreat Sci. 2014;21:159-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 93] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 7. | Jin Z, Bie LK, Tang YP, Ge L, Shen SS, Xu B, Li T, Gong B. Endoscopic therapy for patients with pancreaticobiliary maljunction: a follow-up study. Oncotarget. 2017;8:44860-44869. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Jiang YH, Zhang AH, Zhou SJ. Pancreatogenic choledocholithiasis in common bile duct stump after Roux-en-Y hepaticojejunostomy: A case report. Medicine (Baltimore). 2017;96:e8789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Zeng JQ, Deng ZH, Yang KH, Zhang TA, Wang WY, Ji JM, Hu YB, Xu CD, Gong B. Endoscopic retrograde cholangiopancreatography in children with symptomatic pancreaticobiliary maljunction: A retrospective multicenter study. World J Gastroenterol. 2019;25:6107-6115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (1)] |
| 10. | Yang YL. Clinical thinking and diagnosis and treatment strategies of biliopancreatic junction diseases. Waike Lilun Yu Shijian. 2015;20:102-107. [DOI] [Full Text] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/