Published online Jan 27, 2025. doi: 10.4240/wjgs.v17.i1.101623
Revised: November 4, 2024
Accepted: December 2, 2024
Published online: January 27, 2025
Processing time: 97 Days and 9.6 Hours
Jejunal diverticula (JD) are rare clinical conditions that are typically incidentally detected and asymptomatic. When acute complications arise, surgical exploration may be necessary for accurate diagnosis and appropriate treatment. In this report, we present a case of multiple JD complicated by gastrointestinal bleeding and review the pathogenesis, diagnosis, and treatment of JD to increase clinician awa
A 70-year-old male patient with multiple JD presented with repeated massive gastrointestinal bleeding. The patient did not respond to symptomatic conservative treatment. Additional diagnostic investigations, including digestive endo
Complications caused by JD are often difficult to diagnose, and surgical explora
Core Tip: Jejunal diverticula (JD) are rare clinical conditions that can lead to nonspecific symptoms, making diagnosis challenging. Gastrointestinal bleeding caused by JD is observed in 3%-8% of patients and may manifest as either fresh rectal bleeding or dark red bloody stools. In cases of complications, early diagnosis can be facilitated through the use of endoscopy and computed tomography scans, with surgical resection of the affected bowel being the most suitable treatment option. In this report, we present a case of multiple JD associated with recurrent gastrointestinal bleeding, and we discuss its pathogenesis, diagnosis, and treatment options.
- Citation: Li MY, Han Z, Wang H, Wang YY, Zhao ZR. Multiple jejunal diverticula with repeated gastrointestinal bleeding: A case report. World J Gastrointest Surg 2025; 17(1): 101623
- URL: https://www.wjgnet.com/1948-9366/full/v17/i1/101623.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i1.101623
Jejunal diverticula (JD) are rare clinical conditions that are typically incidentally detected and asymptomatic[1]. Unlike Meckel's diverticula, JD tend to be acquired pseudodiverticula and are more common in older patients, particularly those over 60 years of age, with a slight male predominance[2,3]. Owing to the lack of a true muscular wall, they are usually thin and fragile, making them more susceptible to serious complications such as hemorrhage, perforation, or inflammation than true diverticula[3,4]. Massive gastrointestinal bleeding from JD is exceedingly rare, and delayed diagnosis may result in a high mortality rate. Here, we present a male patient with multiple JD who experienced recurrent gas
A 70-year-old male with a one-day history of bloody stools presented at our center.
The patient experienced a significant amount of dark red bloody stools without an obvious cause, accompanied by abdominal distension, nausea, and vomiting the day prior. Additionally, he exhibited signs of hypovolemia, including panic, fatigue, and pallor. A comprehensive abdominal computed tomography (CT) scan revealed suspected blood accumulation in the rectal lumen, but no significant abnormalities were noted in the surrounding areas. He was subse
Prior to this episode, the patient was in good health and denied any history of gastrointestinal bleeding conditions or related medications.
No relevant personal or family history was recorded.
His vital signs were not stable, with a blood pressure of 12.7/7.1 kPa and a blood oxygen saturation of 98%. Upon examination, his abdomen appeared flat and soft, without any signs of swelling or tenderness.
The laboratory results revealed a low hemoglobin level (6.5 g/dL) and slightly increased white blood cell count (12.1 × 109/L). The rest of the routine blood and biochemical examinations revealed no obvious abnormalities.
When his condition stabilized, he underwent gastroscopy and colonoscopy, which did not reveal any active bleeding sites except for one colonic polyp and stagnant blood in the intestinal lumen. To further identify the cause and location of the bleeding, the patient underwent abdominal angiography, which again was negative.
On the basis of clinical evidence, it was preliminarily identified as unexplained gastrointestinal bleeding. After explora
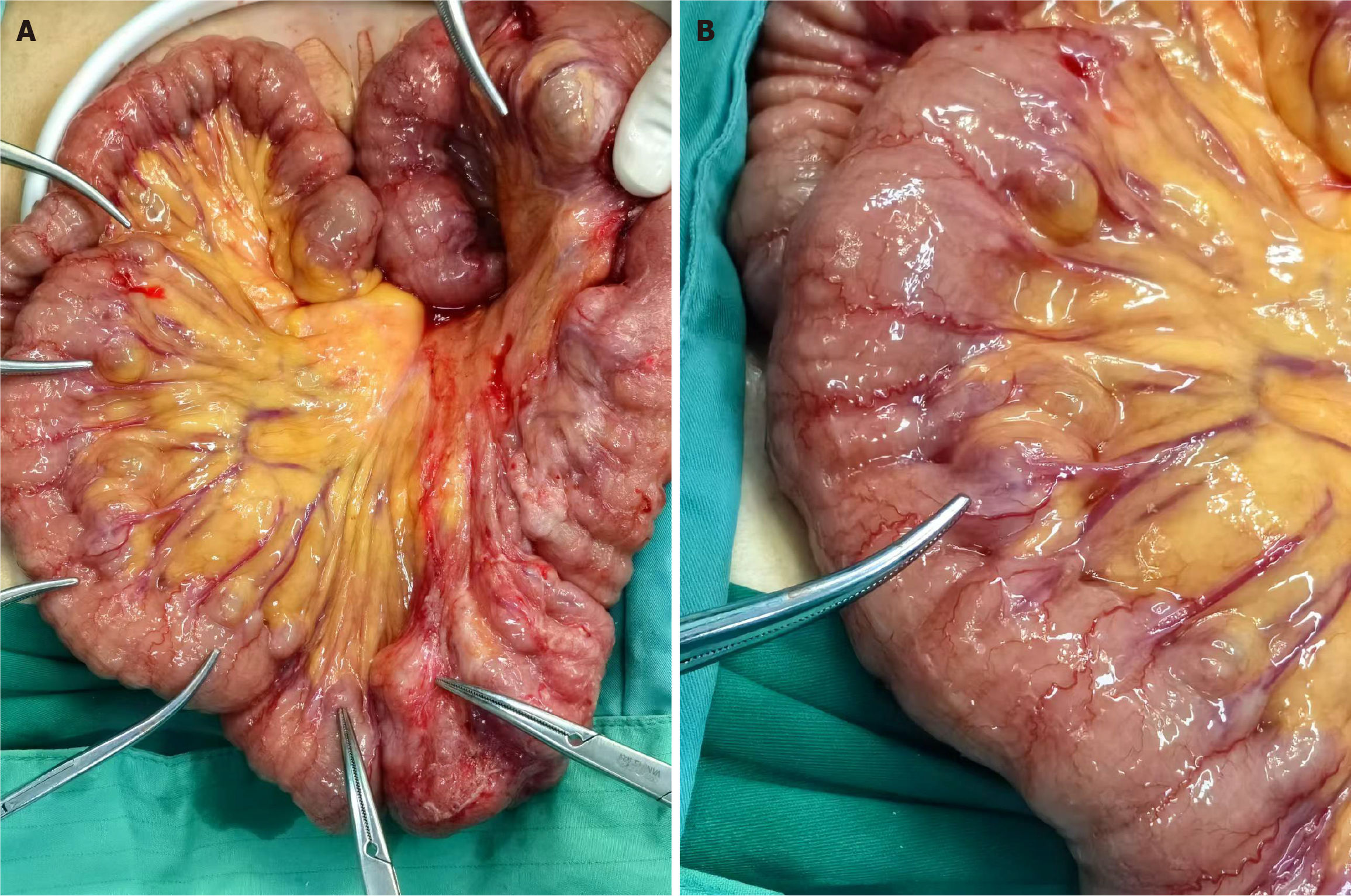
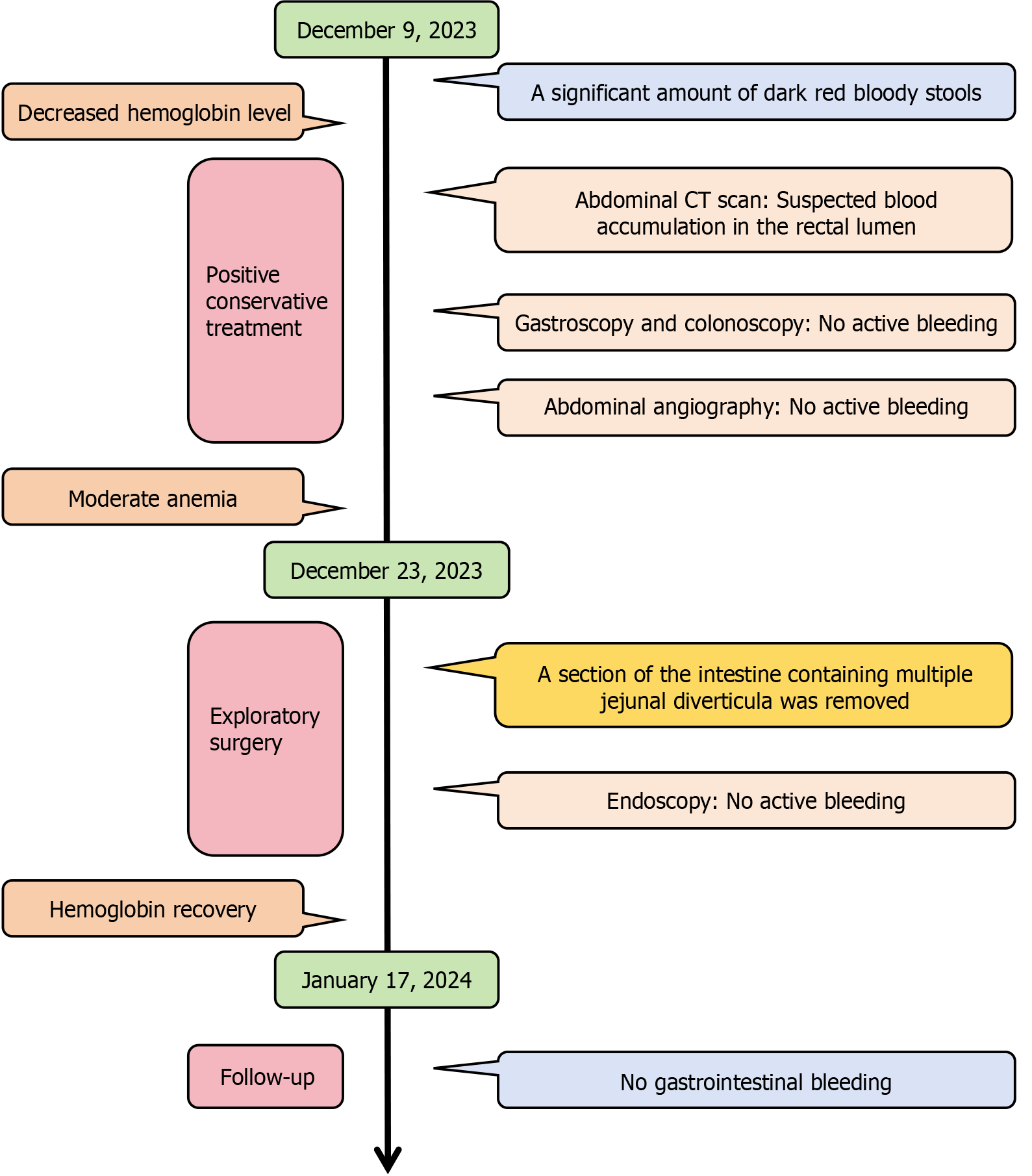
His condition recurred, and he remained in a state of moderate anemia. Positive conservative treatment such as blood transfusion and intravenous fluid replenishment had no obvious effect. Exploratory surgery was conducted, revealing multiple diverticula of the jejunum located 25-55 cm from the flexural ligament (Figure 1A). Additionally, the mesenteric rim vessels showed signs suggestive of hemangiomas (Figure 1B). To further rule out other potential causes of bleeding, an incision was made adjacent to the small bowel diverticulum, followed by another endoscopy to thoroughly examine the bowel both proximally and distally. No active bleeding was observed, with only stagnant blood residue visible in the ascending colon. Ultimately, approximately 55 cm of the proximal jejunum was resected, and an intestinal anastomosis was performed. The anatomical specimen revealed multiple diverticula-like structures characterized by a significantly thinned intestinal wall.
After the operation, the patient received symptomatic support treatment, and he was discharged from the hospital successfully. The final pathological examination of the resected specimen confirmed the presence of multiple JD with increased vascularization, bruising, and bleeding. Subsequent follow-up assessments indicated that the patient did not experience any further gastrointestinal bleeding (Figure 2), confirming that multiple JD were the source of the bleeding.
Most JD are asymptomatic, difficult to identify and typically treated by observation when they are incidentally disco
The development of JD is commonly attributed to localized elevated intraluminal pressure and inherent weaknesses in the intestinal wall, which facilitate the penetration of mesenteric vessels through the intestinal wall[3,5]. Abnormal clumping of intestinal smooth muscle, resulting in uncoordinated movements and localized areas of high intestinal pressure, is believed to be a contributing factor[2,6]. However, JD typically manifest at the mesenteric margin, possibly due to the vulnerability of this area, where mesenteric vessels penetrate the intestinal wall[7]. Regardless, the end result is a sac-like protuberance of the mesenteric margin. Furthermore, peristalsis of the small intestine tends to fill these protruding pouches with liquid chyme, and if accompanied by a small caliber of the pouch, its contents remain difficult to empty even with normal peristalsis of the intestine[8]. The acquired diverticula lack a muscular wall and often exhibit paper-thin walls, as observed during surgical procedures. Alternatively, peripheral inflammation due to repeated irritation of the luminal contents of the bowel, as described above, can lead to edema and wall thickening[3].
JD typically remain silent until some acute and chronic complications arise[3,9]. Chronic complications such as abdo
Primary calculi in the small intestine are rare. Reduced bowel motility and long-term stasis of bowel contents are the most common triggers, and diverticula are a common cause[14]. Luminal stasis promotes bacterial overgrowth, resulting in bile salt dissociation, precipitate condensation, and, eventually, the formation of solid particles, namely, intestinal stones[15]. JD complicated by enterolithiasis can result in both acute and chronic small bowel obstruction, and surgical intervention can offer a definitive diagnosis and treatment[16]. The perforation of JD occurs in 2%-6% of cases[17]. Clinical diagnosis is challenging at this time because the symptoms resemble those of other causes of acute abdomen, such as peptic ulcer perforation and appendicitis[18]. In cases of acute complications, a thorough surgical examination of the bowel is imperative, even though identifying jejunal or ileal diverticula can be challenging, as they are often concealed within the mesenteric fat[4]. Successful outcomes can be achieved by resecting the affected bowel segment and performing an end-to-end anastomosis. To prevent the development of short bowel syndrome, large resections should be avoided during surgery, as the potential risks may outweigh the benefits[19].
Early diagnosis and prompt treatment can reduce morbidity and mortality[20]. However, rare complications often result in missed or delayed diagnosis, presenting a significant challenge for clinicians. CT angiography, a valuable diagnostic tool for acute gastrointestinal bleeding, can assist in identifying ongoing bleeding by revealing active contrast leakage into the intestine during the arterial phase[12]. Although our patient underwent a CT angiogram to locate the bleeding site, no significant findings were observed, likely due to the cessation of bleeding. While mesenteric vascular embolization has proven effective in treating colonic bleeding, its efficacy in treating small bowel bleeding is limited, possibly due to the narrower vasculature of the small bowel, leading to potential rebleeding even after successful initial treatment[21,22]. Capsule endoscopes can pass through the entire intestine and rely on the peristalsis of the intestine itself to provide images of the intestinal cavity in a nonsurgical manner, providing a new perspective for identifying the source of bleeding. Push colonoscopy can be used to examine a portion of the proximal jejunum to assist in diagnosing and treating angiodysplasia[23,24]. These endoscopic procedures may help identify gastrointestinal bleeding caused by the JD and provide further hemostatic treatment, to some extent avoiding surgery, although this was not done in our patient due to acute hemorrhage. Preoperative diagnosis of acute complications from JD is achieved in only 14% of cases, with surgical exploration sometimes being necessary to confirm the correct diagnosis[2].
In conclusion, diagnosing acute or chronic complications arising from JD is challenging. Timely surgical exploration may provide greater benefits to patients. The existing literature primarily consists of case reports, with relatively few retro
The authors thank the patient for his collaboration.
| 1. | Amodu LI, Boyd BA, Smirnov V. Jejunal Diverticulosis Causing Small Intestinal Volvulus and Closed Loop Obstruction. Am J Case Rep. 2024;25:e943376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 2. | Liu CY, Chang WH, Lin SC, Chu CH, Wang TE, Shih SC. Analysis of clinical manifestations of symptomatic acquired jejunoileal diverticular disease. World J Gastroenterol. 2005;11:5557-5560. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 38] [Cited by in RCA: 45] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Baskin RH Jr, Mayo CW. Jejunal diverticulosis; a clinical study of 87 cases. Surg Clin North Am. 1952;1185-1196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 49] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Shackelford RT, Marcus WY. Jejunal diverticula--a cause of gastro-intestinal hemorrhage: a report of three cases and review of the literature. Ann Surg. 1960;151:930-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Kawamura S, Nishijima M, Yamamoto T, Sakai KI, Hirai H, Imano M, Kato M, Ohyanagi H. Massive bleeding from multiple jejunal diverticula associated with an angiodysplasia: report of a case. Surg Today. 2000;30:750-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Krishnamurthy S, Kelly MM, Rohrmann CA, Schuffler MD. Jejunal diverticulosis. A heterogenous disorder caused by a variety of abnormalities of smooth muscle or myenteric plexus. Gastroenterology. 1983;85:538-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 125] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 7. | Gómez-Carrillo D, Núñez-Rocha RE, Perdomo CF, Fajardo R. Elucidating jejunal diverticulosis: Diagnostic and treatment insights from a perforated case study. Int J Surg Case Rep. 2024;119:109726. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Cooke WT, Cox EV, Fone DJ, Meynell MJ, Gaddie R. The clinical and metabolic significance of jejunal diverticula. Gut. 1963;4:115-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 97] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Wilcox RD, Shatney CH. Surgical implications of jejunal diverticula. South Med J. 1988;81:1386-1391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 67] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Rodriguez HE, Ziauddin MF, Quiros ED, Brown AM, Podbielski FJ. Jejunal diverticulosis and gastrointestinal bleeding. J Clin Gastroenterol. 2001;33:412-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Longo WE, Vernava AM 3rd. Clinical implications of jejunoileal diverticular disease. Dis Colon Rectum. 1992;35:381-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 94] [Article Influence: 2.8] [Reference Citation Analysis (1)] |
| 12. | Yaqub S, Evensen BV, Kjellevold K. Massive rectal bleeding from acquired jejunal diverticula. World J Emerg Surg. 2011;6:17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Kamaruddin NT, Tan JH, Teh JZ. Hidden cause of intestinal bleeding from jejunal diverticulum revealed on enteroscopy and treated successfully with segmental resection. ANZ J Surg. 2022;92:1932-1934. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Abtar HK, Mneimneh M, Hammoud MM, Zaaroura A, Papas YS. Primarily Proximal Jejunal Stone Causing Enterolith Ileus in a Patient without Evidence of Cholecystoenteric Fistula or Jejunal Diverticulosis. Case Rep Surg. 2016;2016:8390724. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Karveli E, Barlow C, Grant C, Conroy S, Papamichail M. Primary Jejunal Enterolith Causing Small Bowel Obstruction Without Any Underlying Bowel Abnormality. Cureus. 2022;14:e28743. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 16. | Chugay P, Choi J, Dong XD. Jejunal diverticular disease complicated by enteroliths: Report of two different presentations. World J Gastrointest Surg. 2010;2:26-29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 17. | Abdelhalim D, Kania T, Heldreth A, Champion N, Mukherjee I. Operative Management of Perforated Jejunal Diverticulitis. Cureus. 2022;14:e21330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 18. | Koli D, Vats M, Upreti HV. Perforated isolated jejunal diverticula: a rare cause of acute abdomen. Clin J Gastroenterol. 2020;13:728-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Novak JS, Tobias J, Barkin JS. Nonsurgical management of acute jejunal diverticulitis: a review. Am J Gastroenterol. 1997;92:1929-1931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | de Bree E, Grammatikakis J, Christodoulakis M, Tsiftsis D. The clinical significance of acquired jejunoileal diverticula. Am J Gastroenterol. 1998;93:2523-2528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 57] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 21. | Tan KK, Liu JZ, Ho CK. Emergency surgery for jejunal diverticulosis: our experience and review of literature. ANZ J Surg. 2011;81:358-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 22. | Tan KK, Wong D, Sim R. Superselective embolization for lower gastrointestinal hemorrhage: an institutional review over 7 years. World J Surg. 2008;32:2707-2715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 74] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 23. | Jackson CS, Kesavan C, Das A, Imbertson E, Strong RM. Endocuff-assisted push enteroscopy increases the detection of proximal small-bowel gastrointestinal angiodysplasias. Indian J Gastroenterol. 2022;41:300-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Mylonaki M, Fritscher-Ravens A, Swain P. Wireless capsule endoscopy: a comparison with push enteroscopy in patients with gastroscopy and colonoscopy negative gastrointestinal bleeding. Gut. 2003;52:1122-1126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 342] [Cited by in RCA: 316] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/