Published online Sep 27, 2024. doi: 10.4240/wjgs.v16.i9.3041
Revised: June 6, 2024
Accepted: July 16, 2024
Published online: September 27, 2024
Processing time: 197 Days and 1.4 Hours
Currently, perioperative complications of classic Whipple surgery occur at a rate of approximately 40%. Common complications include delayed gastric emptying, pancreatic fistula, and bile leakage, whereas gastrojejunostomy (GJ) leakage is rare.
This case report will assess the management of a GJ leak in a 71-year-old male patient following the Whipple procedure. After surgery, the patient was trans
Current literature reports a GJ leakage rate of 0. 54% following Whipple surgery, with clinical findings lasting on average between 4-34 days. Surgery was the main form of therapy for this case, with a success rate of 84%, and percutaneous drai
Core Tip: Gastrojejunostomy leakage post-Whipple procedure, although rare, presents significant management challenges. This case highlights the successful endoscopic application of titanium clips to close leakage in a 71-year-old patient, marking a novel approach for treating such complications. Typically managed through surgery or percutaneous drainage with an 84% success rate, this report introduces endoscopy as a viable and less invasive option. Early intervention and adoption of such innovative techniques could potentially enhance recovery outcomes, emphasizing the importance of considering endoscopic treatment in similar clinical scenarios.
- Citation: Muhammedoğlu B, Ay OF. Endoscopic clipping of gastrojejunostomy leakage following Whipple procedure: A case report. World J Gastrointest Surg 2024; 16(9): 3041-3047
- URL: https://www.wjgnet.com/1948-9366/full/v16/i9/3041.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i9.3041
Whipple surgery pancreaticoduodenectomy (PD) is a major procedure used for both benign and malignant tumors in the periampullary region. It has a 5% mortality rate and up to 40% morbidity rate, even with advanced surgical methods and intensive care[1,2].
Whipple surgery can be performed using two techniques: Gastrojejunostomy (GJ) (classic PD) or duodenojejunostomy (DJ) and pylorus-preserving PD (PPPD)[3]. Anastomotic leakage occurs in approximately 10%-20% of pancreaticojejunostomy (PJ) cases and 3% of hepaticojejunostomy cases[4]. Anastomotic leakage of the GJ or DJ after PD is uncommon but can be severe and challenging to manage. The rate ranges from 0.54% to 1% in literature for GJ or DJ[5,6].
The rarity and complexity of GJ leakage after Whipple surgery necessitate enhanced clinical understanding. This report introduces an endoscopic solution for such a complication in a 71-year-old male, a novel approach in clinical practice. Through this case and literature review, we aimed to broaden the knowledge on management strategies and the potential of endoscopic repair in similar cases.
Approximately 500 mL of bile was drained from the incision site and drains of a patient who underwent an open Whipple operation for a pancreatic head tumor, starting on the postoperative seventh day.
The patient, whose American Society of Anesthesiologists physical status classification score was 3 and body mass index: 30.8, was taken to the open, classical Whipple operation. The operation time was 300 minutes, and the estimated blood loss was 150 mL. During the operation, the two erythrocyte suspensions and fresh frozen plasma were replaced. Postoperatively, the patient was transferred to the intensive care unit as intubated. Bleeding from the gastroenterostomy line was detected in the endoscopy performed after active hemorrhagic content was seen in the nasogastric tube on the first postoperative day. Bleeding was controlled using endoscopic adrenaline injection. The patient was extubated on the 2nd postoperative day and transferred to the clinic on the 4th postoperative day.
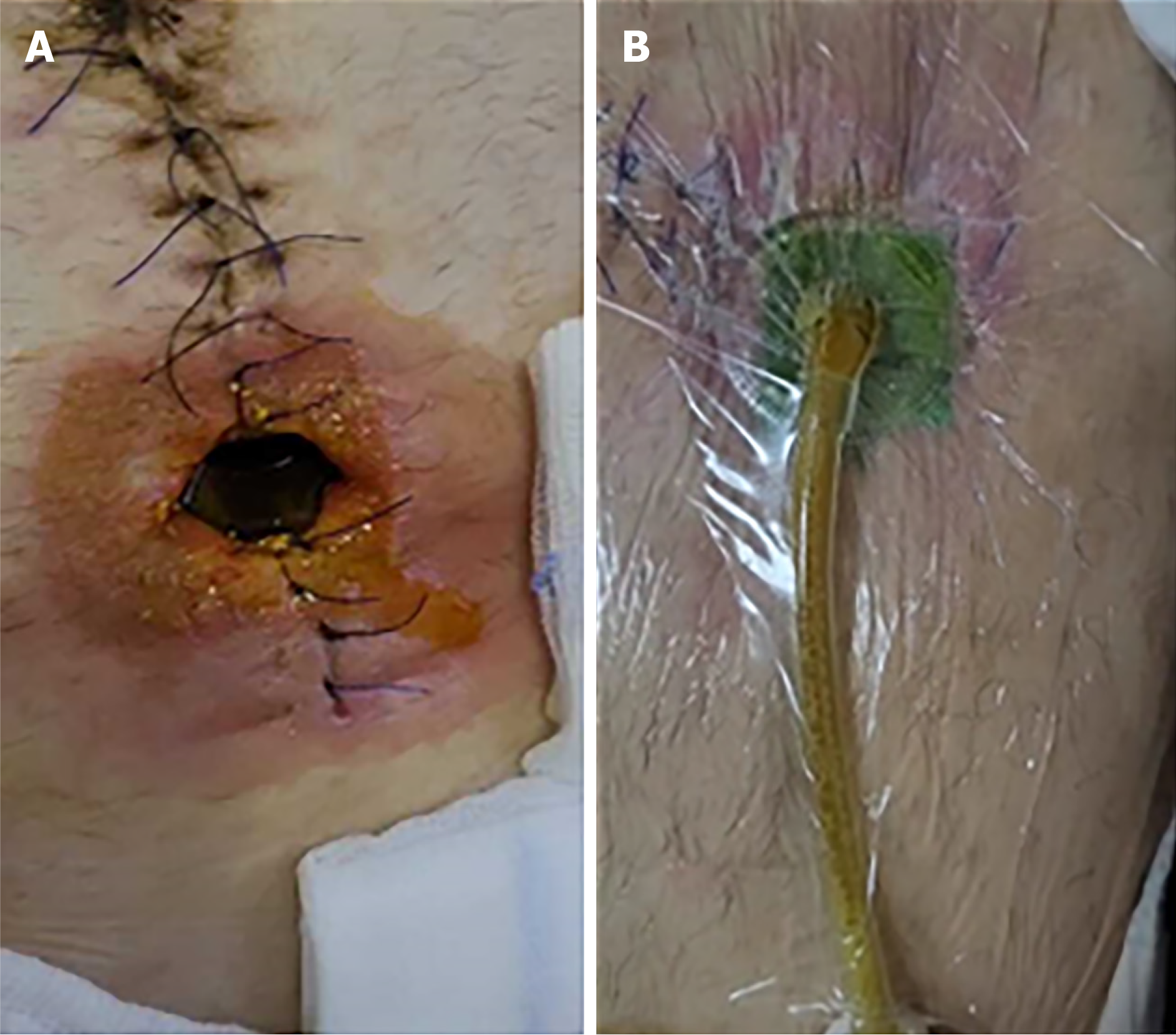
Vacuum closure treatment was applied to the patient, who was discharged from the incision site on the 7th posto
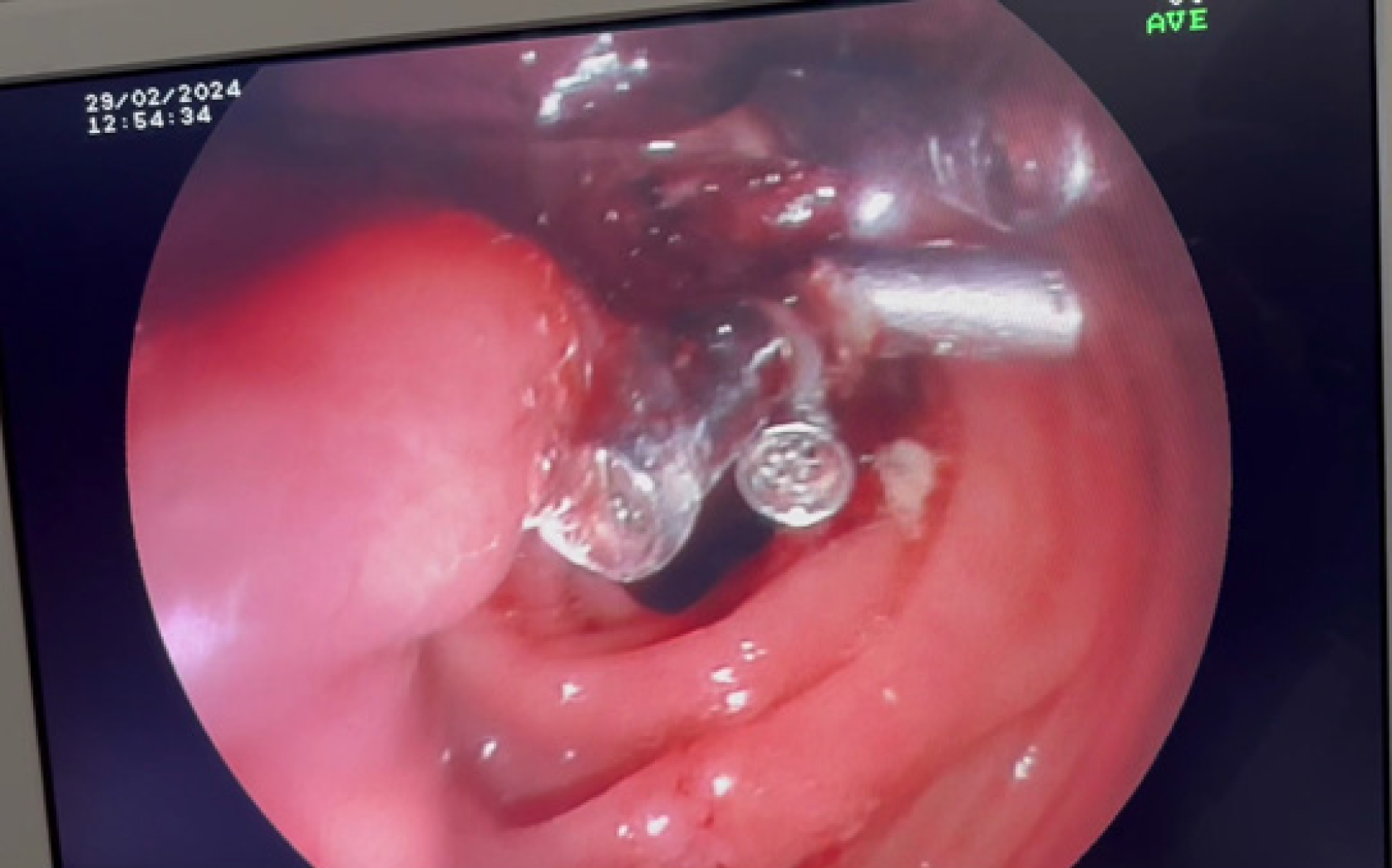
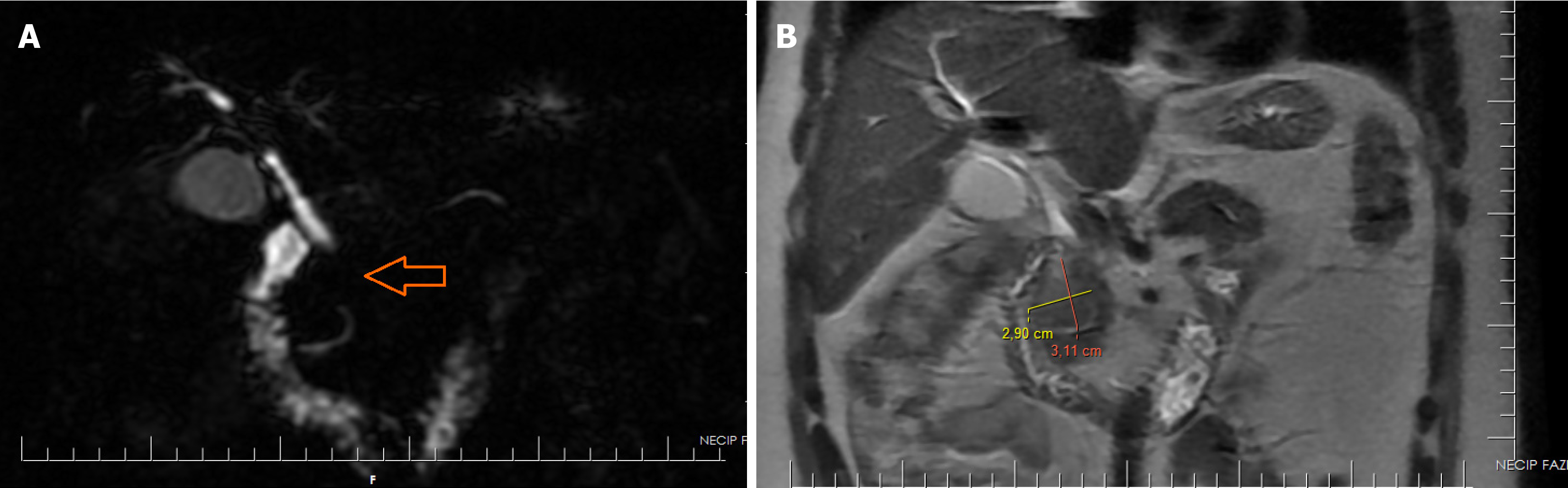
On the 21st postoperative day, the discharge was distinctly bilious, with a flow rate of 500 mL. A control endoscopy decision was made because the pancreatic stent was placed outside the parenchyma and there was significant fluid collection around the gastroenterostomy line on control CT (Figure 2). During examination, an opening of approximately 4 mm was observed in the gastroenterostomy line. The opening was closed using five titanium clips (Figure 3). At this point, we hypothesized that adrenaline injections might interfere with anastomotic blood supply, leading to fistula formation.
Approximately one month ago the patient presented with mechanical icterus (total bilirubin level 7 mg/dL) and un
The patient denied a family history of malignant tumors. The patient had a history of undergoing cholecystectomy and inguinal hernia repair.
On physical examination, the vital signs were as follows: Body temperature, 37.1 ℃; blood pressure, 123/77 mmHg; heart rate, 103 beats per min; respiratory rate, 21 breaths per min. During the abdominal examination, the incision remained intact, but there was an opening in the umbilicus for the vacuum-assisted dressing to get inside (Figure 5). There was a total of over 500 mL of bile from the drains and incision. No obvious signs of peritoneal irritation were noted. Patients can be mobilized and perform breathing exercises.
When endoscopic intervention was performed, white blood cell was 9.34 × 103 cells/uL, hemoglobin was 11.1 g/dL, and total bilirubin was 1.45 mg/dL. Liver and renal function tests were normal. There was no acidosis in arterial blood gas examination, respiratory parameters were normal.
Gastroscopy was performed for diagnostic purposes because of the presence of collection and minimal air density in the gastroenterostomy line, as shown in the CT scan. 4 mm fistula openings in the gastroenterostomy stapler line were closed using five titanium clips during the examination.
Following the identification of excessive biliary drainage and suspected fistula, further diagnostic steps were initiated. Radiological and endoscopic examinations were conducted on the 21st postoperative day, which confirmed a fistula along the staple line. Gastroscopy revealed a 4 mm fistula within the gastroenterostomy line. Subsequent imaging, including a CT scan, highlighted the minimal air density near the site, indicating the presence of a fistula. This comprehensive diagnostic approach facilitated targeted intervention and guided successful closure of the fistula using titanium clips during endoscopy.
The final diagnosis for the patient was a post-Whipple GJ fistula. This diagnosis was established after the detection of biliary fluid leakage from the surgical site and confirmation of a fistula along the gastroenterostomy staple line through endoscopic examination.
On the initial day after the procedure, the patient's bile drainage decreased to less than 50 mL. No bile-like fluid was observed in the vacuum dressing applied through the incision. On the third day post-procedure, the patient resumed oral intake, and drains were removed.
The fistula was successfully managed using endoscopic treatment. The patient resumed oral intake the day after the procedure. The patient was in good general condition, with stable vital signs.
Labori et al[5] reported gastroenterostomy leakage rates of 0.74% following Whipple operation. Furthermore, PJ leakage was detected in 50% of the cases. Eighty-four percent of the cases were managed surgically, with a mortality rate of 15%. In the context of gastroenterostomy leaks, which are uncommon according to the literature, we did not observe a leak in the PJ and decided to perform endoscopic management.
Studies have highlighted that low preoperative hemoglobin levels and a history of radiotherapy are significant risk factors for gastroenterostomy leaks following the Whipple operation[7]. Preoperative blood urea nitrogen/creatinine ratio and perioperative blood transfusion were associated with gastroenterostomy leaks[6]. The preoperative hemoglobin level and renal function in our patient were within the normal ranges. Two units of erythrocyte suspension was trans
The emergence of symptoms after GJ varies between 4 and 34 days according to the literature. In terms of surgical technique, no statistical difference has been observed in the literature between GJ/DJ leaks in classic PD and PPPD[3]. Likewise, according to the literature, there is no statistically significant difference in the leakage rate in gastroenterostomies performed with a stapler or handsewn[8]. We think that the findings in our patient emerged on the 7th posto
In 84% of the cases, laparotomy was performed to manage gastroenterostomy leaks following Whipple. Percutaneous drains inserted by interventional radiologists have also been used as management techniques. Regarding endoscopic management, only one esophagectomy case involved the use of a stent as an advanced endoscopic technique[5,7,8]. There is only one report available on endoscopic treatment. An endoscopic stent was used to manage a post-Whipple DJ leak in a patient who had undergone esophagectomy[9]. In this context, we believe we are the first to report a case of managing a GJ leak following the Whipple procedure using the endoscopic clip method.
The endoscopic treatment of GJ leaks has also been documented in cases of bariatric surgery and gastrectomy for gastric cancer. The defect diameter for endoscopic treatment should be less than 2 cm, and the separation should be less than 70% of the lumen[10]. Options such as fibrin material spraying[11], endoscopic suturing[11], stenting[12], and endoscopic vacuum-assisted closure[13] are technically available. The efficacy of these techniques varies, and decisions should be based on clinical findings and experience.
This case report has several limitations. Firstly, it is based on a single patient, which limits the generalizability of the findings. The clinical outcomes observed may not be representative of a broader patient population undergoing similar procedures. Secondly, as a retrospective analysis, the study is subject to inherent biases and limitations related to data collection and analysis. The specific clinical environment and conditions under which the observations were made may also affect the results. Furthermore, the long-term efficacy and safety of the endoscopic clipping technique used in this case require further investigation through prospective studies involving a larger cohort of patients. Additionally, this case report does not include a comparative analysis with other treatment options, which makes it difficult to fully assess the advantages and disadvantages of the endoscopic approach. More extensive and comparative research is needed to better understand the potential benefits and limitations of this technique in the management of GJ leaks after Whipple procedure.
In this extraordinary case, we describe the first reported instance of managing a GJ leak following Whipple surgery via endoscopic clipping. This novel approach shows the potential of less invasive endoscopic techniques than traditional surgical interventions for such complications. Our experience emphasizes the importance of considering endoscopic methods in the management of post-Whipple anastomotic leaks, potentially offering a safer and more efficient alternative to conventional surgical repair. This case contributes significantly to the existing literature by suggesting a paradigm shift in the treatment strategy for GJ leaks after the Whipple procedure.
| 1. | Symeonidis D, Zacharoulis D, Kissa L, Samara AA, Petsa E, Tepetes K. From Classic Whipple to Pylorus Preserving Pancreaticoduodenectomy and Ultimately to Pylorus Resecting - Stomach Preserving Pancreaticoduodenectomy: A Review. Chirurgia (Bucur). 2023;118:335-347. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Emekli E, Gündoğdu E. Computed tomography evaluation of early post-operative complications of the Whipple procedure. Pol J Radiol. 2020;85:e104-e109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 3. | Hüttner FJ, Fitzmaurice C, Schwarzer G, Seiler CM, Antes G, Büchler MW, Diener MK. Pylorus-preserving pancreaticoduodenectomy (pp Whipple) versus pancreaticoduodenectomy (classic Whipple) for surgical treatment of periampullary and pancreatic carcinoma. Cochrane Database Syst Rev. 2016;2:CD006053. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 80] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 4. | Eshuis WJ, Tol JA, Nio CY, Busch OR, van Gulik TM, Gouma DJ. Leakage of the gastroenteric anastomosis after pancreatoduodenectomy. Surgery. 2014;156:75-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Labori KJ, Tholfsen T, Yaqub S, Lassen K, Kleive D, Waage A. Gastro- or Duodenojejunostomy Leaks After Pancreatoduodenectomy: Single Center Experience and Narrative Literature Review. J Gastrointest Surg. 2021;25:3130-3136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Winter JM, Cameron JL, Yeo CJ, Lillemoe KD, Campbell KA, Schulick RD. Duodenojejunostomy leaks after pancreaticoduodenectomy. J Gastrointest Surg. 2008;12:263-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Mazza M, Crippa S, Pecorelli N, Tamburino D, Partelli S, Castoldi R, Balzano G, Falconi M. Duodeno-jejunal or gastro-enteric leakage after pancreatic resection: a case-control study. Updates Surg. 2019;71:295-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Hajibandeh S, Hajibandeh S, Khan RMA, Malik S, Mansour M, Kausar A, Subar D. Stapled anastomosis versus hand-sewn anastomosis of gastro/duodenojejunostomy in pancreaticoduodenectomy: A systematic review and meta-analysis. Int J Surg. 2017;48:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Honig SE, Lundgren MP, Kowalski TE, Lavu H, Yeo CJ. Advanced Endoscopic Rescue of a Complication (Duodenojejunostomy Leak) After a Pylorus-Preserving Pancreaticoduodenectomy in a Post-Esophagectomy Patient with Pancreatic Adenocarcinoma: A Case Report and Review of the Literature. J Pancreat Cancer. 2020;6:5-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Jeong SH, Lee JK, Seo KW, Min JS. Treatment and Prevention of Postoperative Leakage after Gastrectomy for Gastric Cancer. J Clin Med. 2023;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 11. | Rábago LR, Ventosa N, Castro JL, Marco J, Herrera N, Gea F. Endoscopic treatment of postoperative fistulas resistant to conservative management using biological fibrin glue. Endoscopy. 2002;34:632-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 112] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 12. | Puli SR, Spofford IS, Thompson CC. Use of self-expandable stents in the treatment of bariatric surgery leaks: a systematic review and meta-analysis. Gastrointest Endosc. 2012;75:287-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 124] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 13. | Hwang JJ, Jeong YS, Park YS, Yoon H, Shin CM, Kim N, Lee DH. Comparison of Endoscopic Vacuum Therapy and Endoscopic Stent Implantation With Self-Expandable Metal Stent in Treating Postsurgical Gastroesophageal Leakage. Medicine (Baltimore). 2016;95:e3416. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 76] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/