Published online Sep 27, 2024. doi: 10.4240/wjgs.v16.i9.2823
Revised: July 16, 2024
Accepted: August 5, 2024
Published online: September 27, 2024
Processing time: 211 Days and 22.8 Hours
Choledocholithiasis is a common clinical bile duct disease, laparoscopic choledocholithotomy is the main clinical treatment method for choledocholithiasis. However, the recurrence of postoperative stones is a big challenge for patients and doctors.
To explore the related risk factors of gallstone recurrence after laparoscopic choledocholithotomy, establish and evaluate a clinical prediction model.
A total of 254 patients who underwent laparoscopic choledocholithotomy in the First Affiliated Hospital of Ningbo University from December 2017 to December 2020 were selected as the research subjects. Clinical data of the patients were collected, and the recurrence of gallstones was recorded based on the postope
Postoperative stone recurrence rate was 10.23% (26 patients). Multivariate Logistic regression analysis showed that cholangitis, the diameter of the common bile duct, the diameter of the stone, number of stones, lithotripsy, preoperative total bilirubin, and T tube were risk factors associated with postoperative recurrence (P < 0.05). The clinical prediction model was ln (p/1-p) = -6.853 + 1.347 × cholangitis + 1.535 × choledochal diameter + 2.176 × stone diameter + 1.784 × stone number + 2.242 × lithotripsy + 0.021 × preoperative total bilirubin + 2.185 × T tube.
Cholangitis, the diameter of the common bile duct, the diameter of the stone, number of stones, lithotripsy, preoperative total bilirubin, and T tube are the associated risk factors for postoperative recurrence of gallstone. The prediction model in this study has a good prediction effect, which has a certain reference value for recurrence of gallstone after laparoscopic choledocholithotomy.
Core Tip: To explore the related risk factors of gallstone recurrence after laparoscopic choledocholithotomy, establish and evaluate a clinical prediction model. A total of 254 patients who underwent laparoscopic choledocholithotomy in the First Affiliated Hospital of Ningbo University from December 2017 to December 2020 were selected as the research subjects. Clinical data of the patients were collected, and the recurrence of gallstones was recorded based on the postoperative follow-up.
- Citation: Wu YJ. Establishment and evaluation of prediction model of recurrence after laparoscopic choledocholithotomy. World J Gastrointest Surg 2024; 16(9): 2823-2828
- URL: https://www.wjgnet.com/1948-9366/full/v16/i9/2823.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i9.2823
Choledocholithiasis can lead to serious complications such as acute cholangitis, biliary pancreatitis, and obstructive jaundice[1]. Presently, laparoscopic choledocholithotomy is the main treatment method of choledocholithiasis, with its characteristics less trauma to patients, fast recovery, and low postoperative infection rate. However, the probability of gallstone recurrence after laparoscopic choledocholithotomy is significantly high[2]. Currently, most researchers believe that the gallstones found within 6 months are residual stones, and the stones found after 6 months are recurrence stones after surgery[3]. According to reports, the probability of gallstone recurrence after choledocholithiasis is 5%-20%[4], Most recurrences occur within 2 years, and the recurrence of stone will result in a significant burden on the patient's body[5], emotions, and financially. However, there is no consensus on the influencing factors of gallstone recurrence after laparoscopic choledocholithotomy. This study analyzed the risk factors associated with the recurrence of gallstones after laparoscopic choledocholithotomy, established a clinical prediction model and discussed the predictive significance of the proposed.
A total of 254 patients (comprising 128 males and 126 females, aged 13 to 88 years) who underwent laparoscopic choledocholithotomy in the First Affiliated Hospital of Ningbo University from December 2017 to December 2020 were retrospectively enlisted as the study subjects.
Inclusion criteria: (1) The patient was diagnosed with choledocholithiasis via color ultrasound and magnetic resonance imaging examination, without a prior history of abdominal surgery; (2) Postoperative imaging examination showed no residual bile duct stones; and (3) The clinical data and follow-up data are complete.
Exclusion criteria: (1) Diagnosed with cancer before surgery; (2) Previous history of endoscopic choledocholithotomy; and (3) Preoperative imaging suggested complicated intrahepatic bile duct stones.
The gender, age, clinical manifestations, preoperative auxiliary examination, and other information were collected. All patients underwent laparoscopic choledocholithotomy + cholecystectomy. Subsequently, the patients were followed up 6 months after the operation, and there was no stone recurrence.
Enrolled factors included: Age, gender, cholangitis, the diameter of the common bile duct, number of stones, the diameter of stone, preoperative total blood bilirubin, preoperative aspartate aminotransferase (AST), preoperative alanine aminotransferase (ALT), hepatitis B, duration of operation, lithotripsy, and indent T tube. All patients were followed up for 2 years.
The statistical analysis was performed using SPSS 22.0. χ² test was performed on the categorical variables and the t-test was performed on the continuous variables. Furthermore, the multivariate Logistic regression analysis was performed to identify statistically significant influencing factors. The priori value of was considered statistically significant. A clinical prediction model was established based on the outcome parameters, and the predictive value was evaluated using the receiver operating characteristic (ROC) curve.
The results showed that cholangitis, the diameter of the common bile duct, number of stones, the diameter of stones, lithotripsy, duration of the operation, preoperative total bilirubin, preoperative AST, and indwelling T tube was related to the recurrence of postoperative stone (P < 0.05). However, gender, age, hepatitis B, preoperative ALT were not associated with the recurrence of postoperative stone (See Table 1).
| Factors | Recurrence (n = 26) | No recurrence (n = 228) | χ²-value | P value |
| Gender | 0.758 | 0.384 | ||
| Male | 11 (42.31) | 117 (51.32) | ||
| Female | 15 (57.69) | 111 (48.68) | ||
| Age (years old) | 60.9 ± 13.7 | 59.1 ± 14.6 | -0.587 | 0.558 |
| Cholangitis | 25.612 | < 0.001 | ||
| Positive | 13 (50.00) | 27 (11.84) | ||
| Negative | 13 (50.00) | 201 (88.16) | ||
| The diameter of the common bile duct ≥ 15mm | 27.801 | < 0.001 | ||
| Positive | 19 (73.08) | 54 (23.68) | ||
| Negative | 7 (26.92) | 174 (76.32) | ||
| Number of stones ≥ 10 | 25.612 | < 0.001 | ||
| Positive | 13 (50.00) | 27 (11.84) | ||
| Negative | 13 (50.00) | 201 (88.16) | ||
| The diameter of stones ≥ 10mm | 15.301 | < 0.001 | ||
| Positive | 18 (69.23) | 70 (30.70) | ||
| Negative | 8 (30.77) | 158 (69.30) | ||
| Lithotripsy | 15.521 | < 0.001 | ||
| Positive | 5 (19.23) | 6 (2.63) | ||
| Negative | 21 (80.77) | 222 (97.37) | ||
| Hepatitis B | 0.997 | 0.318 | ||
| Positive | 5 (19.23) | 28 (12.28) | ||
| Negative | 21 (80.77) | 200 (87.72) | ||
| Duration of operation (min) | 225.88 ± 54.61 | 195.05 ± 50.39 | -2.931 | 0.004 |
| Preoperative total blood bilirubin (μmol/L) | 97.96 ± 50.76 | 49.16 ± 43.63 | -5.311 | < 0.001 |
| AST (U/L) | 155.96 ± 137.25 | 94.64 ± 103.91 | -2.751 | 0.006 |
| ALT (U/L) | 177.19 ± 135.09 | 142.04 ± 148.29 | -1.155 | 0.249 |
| T tube | 26.448 | < 0.001 | ||
| Positive | 22 (84.62) | 75 (32.89) | ||
| Negative | 4 (15.38) | 153 (67.11) |
The results showed that cholangitis, the diameter of the common bile duct, number of stones, the diameter of stone, lithotripsy, preoperative total bilirubin, and the indent T tube were independent risk factors associated with the recurrence of postoperative stone (P < 0.05), while the duration of operation and the preoperative AST had no relationship with the recurrence of postoperative stone (P > 0.05) (See Table 2).
| B | SE | Wald | P value | Exp (B) | 95%CI | ||
| Cholangitis | 1.347 | 0.647 | 4.335 | 0.037 | 3.846 | 1.082 | 13.666 |
| The diameter of the common bile duct | 1.535 | 0.645 | 5.668 | 0.017 | 4.639 | 1.312 | 16.409 |
| Diameter of stones | 2.176 | 0.750 | 8.414 | 0.004 | 8.811 | 2.025 | 38.335 |
| The number of stone | 1.784 | 0.699 | 6.510 | 0.011 | 5.956 | 1.512 | 23.458 |
| Lithotripsy | 2.242 | 1.130 | 3.935 | 0.047 | 9.411 | 1.027 | 86.231 |
| Duration of operation | -0.009 | 0.007 | 1.475 | 0.224 | 0.991 | 0.977 | 1.006 |
| Preoperative total blood bilirubin | 0.021 | 0.007 | 10.239 | 0.001 | 1.022 | 1.008 | 1.035 |
| AST | 0.004 | 0.003 | 1.467 | 0.226 | 1.004 | 0.997 | 1.011 |
| T tube | 2.185 | 0.815 | 7.198 | 0.007 | 8.894 | 1.802 | 43.900 |
| Constant | -6.853 | 1.725 | 15.779 | 0.000 | 0.001 | ||
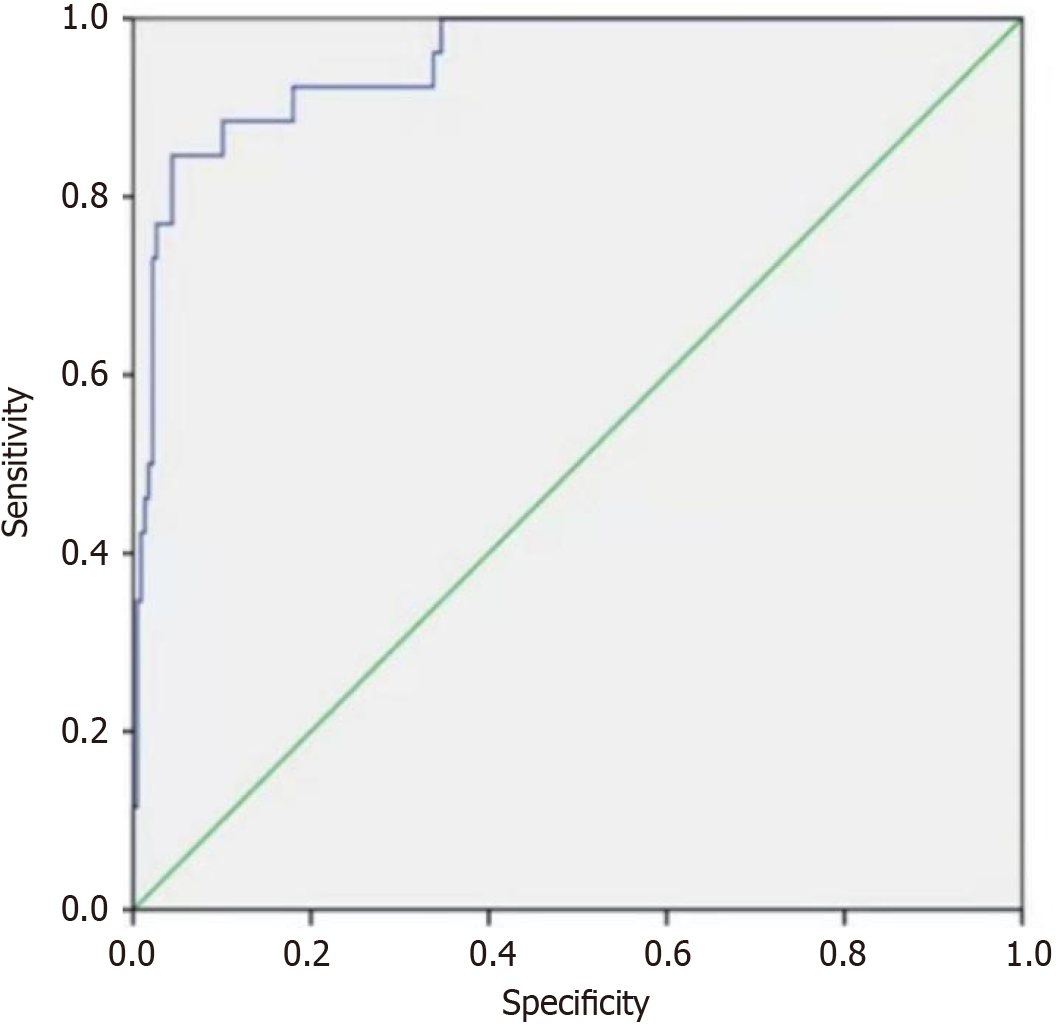
The regression model is established based on the regression coefficients and the constant term of the logistic regression analysis. The clinical prediction model was ln (p/1-p) = -6.853 + 1.347 × cholangitis + 1.535 × choledochal diameter + 2.176 × stone diameter + 1.784 × stone number + 2.242 × lithotripsy + 0.021 × preoperative total bilirubin + 2.185 × T tube. P is the probability of stone recurrence after laparoscopic choledocholithotomy. Patients with cholangitis means 1, without cholangitis means 0, the Diameter of common bile duct ≥ 15 mm means 0, the diameter of common bile duct ≤ 15 mm means 0. Diameter of stone ≥ 10mm means 1, the diameter of stone ≤ 10 mm means 0. The number of stones ≥ 10 means 1, less than or equal to 10 means 0. Patients use lithotripsy means 1, no lithotripsy means 0. Patient use T tube means 1, otherwise 0. The ROC curves are summarized based on the established models. The area under the ROC curve was 95.1%, the highest value of The Yorden finger is selected as the cut-off point. In this study, the cut-off point was selected as 0.802, with a sensitivity of 84.6% and specificity of 95.6%, thus showing a high predictive value for the recurrence of postoperative gallstones (See Figure 1).
Choledocholithiasis is a common clinical bile duct disease, which is often accompanied by serious complications. Currently, laparoscopic choledocholithotomy is the main clinical treatment method for choledocholithiasis. However, the recurrence of postoperative stones is a big challenge for patients and doctors. The stone recurrence probability of 254 patients selected in this study within 2 years was 10.23%. The recurrence of stone often requires a second surgical treatment, which often results in severe pain and economic burden to the patients.
Stone recurrence after Choledocholithiasis is often the result of many factors. Findings from this study showed that cholangitis, the diameter of the common bile duct, number of stones, the diameter of stone, lithotripsy, preoperative total bilirubin, and T-tube were the risk factors for the recurrence of postoperative stone. The influence of cholangitis on the recurrence of stones may be that long-term cholangitis will lead to the fibrosis of the bile duct wall, which will result in the reduction of the bile flow rate and lead to cholestasis, and the subsequent formation of gallstones. Also, cholangitis leads to the weakening of the bile duct to secrete and absorb bile, some bacteria can produce β- Glucuronidase, which can decompose bilirubin diglucuronate, and convert the conjugated bilirubin into free bilirubin, which combines with calcium ions to form stones[2,6]. Some scholars believe that the diameter of the common bile duct ≥ 15 mm is closely related to the recurrence of gallstones after Choledocholithiasis[7], the influence of the diameter of the common bile duct ≥ 15 mm on the recurrence of postoperative stone may be that the long-term dilation of the common bile duct damages the smooth muscles of the bile duct, thus reducing the motor function of the bile duct, and the dilation of the bile duct diameter will reduce the flow rate of the bile, which leads to the recurrence of stones. Furthermore, Ohashi et al[8] believed that it was difficult for patients with the dilation of the bile duct to show tiny stone fragments in postoperative cholangiography, thus causing residual stones. Most scholars believe that patients with ≥ 10 number of stones are more likely to relapse after operation[9]. The effect of the number of stones on the recurrence may be that patients with more stones are more likely to form cholesterol crystals in their bile, hence, they are more likely to have a postoperative recurrence of stones. A large number of stones results in the long time stimulation of the bile duct wall, which also leads to chronic inflammation and fibrosis of the bile duct, and the subsequent formation of stones. This study also showed that stone size is closely related to recurrence of postoperative stone, large stones often need lithotriptic treatment, and long-term compression of large stones on the common bile duct will lead to the dilation of the bile duct and chronic cholangitis[10]. Lithotripsy often leads to the formation of stone fragments and the fragments can adhere to the bile duct wall, thus becoming the core component of recurrent stones[7,11]. Furthermore, lithotripsy leads to duodenal papilledema and bile duct injury, resulting in the poor drainage of the bile duct, and frequent stone removal operations will also damage the inner wall of the bile duct, resulting in bile duct infection. The study shows that preoperative total bilirubin has a significant impact on postoperative recurrence, and there is no specific study on it at present. A high level of total bilirubin may have an impact on the recovery of the liver and the common bile duct, which leads to stone recurrence. Besides, some scholars believe that patients with preoperative jaundice are often accompanied by congenital anatomic abnormalities, which leads to the recurrence of stones[12-14]. The long-term compression and stimulation of the T tube on the common bile duct results in the deformation of the normal structure of the bile duct mucosa and causes the occurrence of chronic cholangitis. The long-term indwelling of the T tube will lead to water and electrolyte disorder in the body, which affects postoperative recovery[15,16].
All the associated risk factors are included in the clinical predictive model, which is given as: ln (P/1-P) = -6.853 + 1.347 × cholangitis + 1.535 × choledochal diameter + 2.176 × stone diameter + 1.784 × stone number + 2.242 × lithotripsy + 0.021 × preoperative total bilirubin + 2.185 × T tube. P is the probability of recurrence after laparoscopic choledocholithotomy. The area under the ROC curve was 95.1%. And the sensitivity and specificity were 84.6% and 95.6% respectively. Conclusively, the predictive model in this study has a good prediction effect and has a certain reference significance for the prediction of stone recurrence after laparoscopic choledocholithotomy. Future studies should involve larger sample sizes with the inclusion of more influencing factors, also, the follow-up time should be increased, and the postoperative condition of the subjects should be continuously monitored to improve the predictive ability of the proposed model.
| 1. | Park SY, Hong TH, Lee SK, Park IY, Kim TH, Kim SG. Recurrence of common bile duct stones following laparoscopic common bile duct exploration: a multicenter study. J Hepatobiliary Pancreat Sci. 2019;26:578-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 2. | Liu J, Wei XJ, Yang ZL, Liao XY, Wu LH, Zheng YP, Zheng JH, Hu YQ, Zheng XL. Risk factors of common bile duct stones recurrence and nomogram for predicting recurrence after endoscopic retrograde cholangiopancreatography: a dual-center retrospective cohort study. Eur Rev Med Pharmacol Sci. 2023;27:2504-2513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 3. | Wu Y, Xu CJ, Xu SF. Advances in Risk Factors for Recurrence of Common Bile Duct Stones. Int J Med Sci. 2021;18:1067-1074. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 56] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 4. | Toyoizumi H, Imazu H, Ikeda K, Mori N, Kanazawa K, Chiba M, Ang TL, Tajiri H. A novel second-generation multibending backward-oblique viewing duodenoscope in ERCP. Minim Invasive Ther Allied Technol. 2015;24:101-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Cai JS, Qiang S, Bao-Bing Y. Advances of recurrent risk factors and management of choledocholithiasis. Scand J Gastroenterol. 2017;52:34-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 6. | Zhou B, Hu J, Zhong Y. Surgical treatments for patients with recurrent bile duct stones and Oddis sphincter laxity. Intractable Rare Dis Res. 2017;6:172-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Sugiyama M, Atomi Y. Risk factors predictive of late complications after endoscopic sphincterotomy for bile duct stones: long-term (more than 10 years) follow-up study. Am J Gastroenterol. 2002;97:2763-2767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 100] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 8. | Ohashi A, Tamada K, Wada S, Hatanaka H, Tomiyama T, Tano S, Nakazawa K, Sugano K. Risk factors for recurrent bile duct stones after endoscopic papillary balloon dilation: long-term follow-up study. Dig Endosc. 2009;21:73-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Li L, Wang J, Tong CC, He CY. Risk factors of recurrent choledocholithiasis following therapeutic endoscopic retrograde cholangiopancreatography. Hepatobiliary Pancreat Dis Int. 2023;22:282-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 10. | Raijman I. Intracorporeal lithotripsy in the management of biliary stone disease. Semin Laparosc Surg. 2000;7:295-301. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Jones T, Al Musawi J, Navaratne L, Martinez-Isla A. Holmium laser lithotripsy improves the rate of successful transcystic laparoscopic common bile duct exploration. Langenbecks Arch Surg. 2019;404:985-992. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 12. | Coucke EM, Akbar H, Kahloon A, Lopez PP. Biliary Obstruction. 2022 Nov 26. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 13. | Deng F, Zhou M, Liu PP, Hong JB, Li GH, Zhou XJ, Chen YX. Causes associated with recurrent choledocholithiasis following therapeutic endoscopic retrograde cholangiopancreatography: A large sample sized retrospective study. World J Clin Cases. 2019;7:1028-1037. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 14. | Li S, Su B, Chen P, Hao J. Risk factors for recurrence of common bile duct stones after endoscopic biliary sphincterotomy. J Int Med Res. 2018;46:2595-2605. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Kim DI, Kim MH, Lee SK, Seo DW, Choi WB, Lee SS, Park HJ, Joo YH, Yoo KS, Kim HJ, Min YI. Risk factors for recurrence of primary bile duct stones after endoscopic biliary sphincterotomy. Gastrointest Endosc. 2001;54:42-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 90] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 16. | Geng ZM, Yao YM, Liu QG, Niu XJ, Liu XG. Mechanism of benign biliary stricture: a morphological and immunohistochemical study. World J Gastroenterol. 2005;11:293-295. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 29] [Cited by in RCA: 31] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/