Published online Aug 27, 2024. doi: 10.4240/wjgs.v16.i8.2640
Revised: July 10, 2024
Accepted: July 22, 2024
Published online: August 27, 2024
Processing time: 60 Days and 3.1 Hours
Intussusception occurs in children and progresses rapidly. If not treated in time, it may lead to secondary complications such as intestinal perforation, which affect the quality of life and health of children. Surgery is the most common clinical treatment and has a good effect. However, the postoperative prognosis of children with intussusception has a correlation with the postoperative rehabilitation method. Therefore, in this study, we explored the relationship between postopera
To explore the relationship between postoperative rehabilitation, gastrointestinal function, and inflammatory factor levels in children with intussusception.
The medical records of 18 children who were admitted to our hospital for intussusception surgery between October 2022 and May 2024 were retrospectively reviewed. The patients were divided into the routine nursing group (n = 6) and rehabilitation training group (n = 12) according to the postoperative rehabilitation method. The general data, gastrointestinal function, and inflammatory factor levels of the two groups were statistically analyzed. Pearson correlation analysis of gastrointestinal function, inflammatory factors, and postoperative rehabilitation was performed.
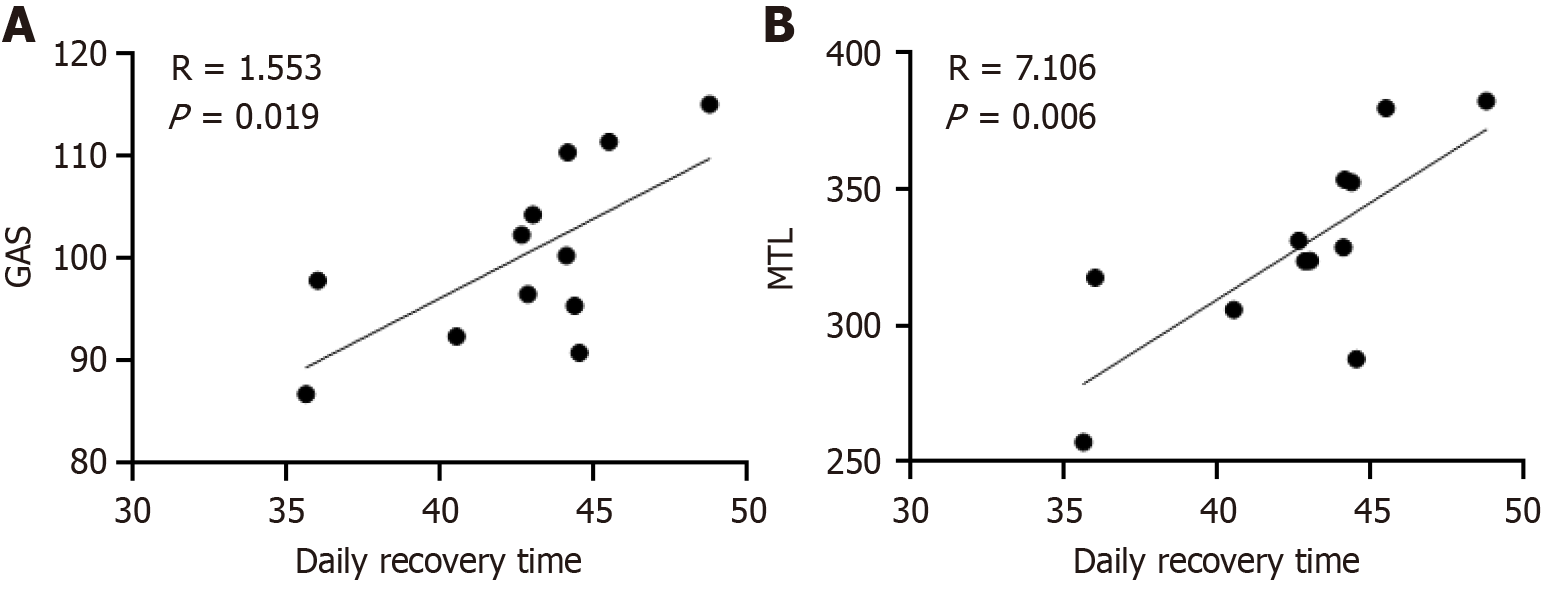
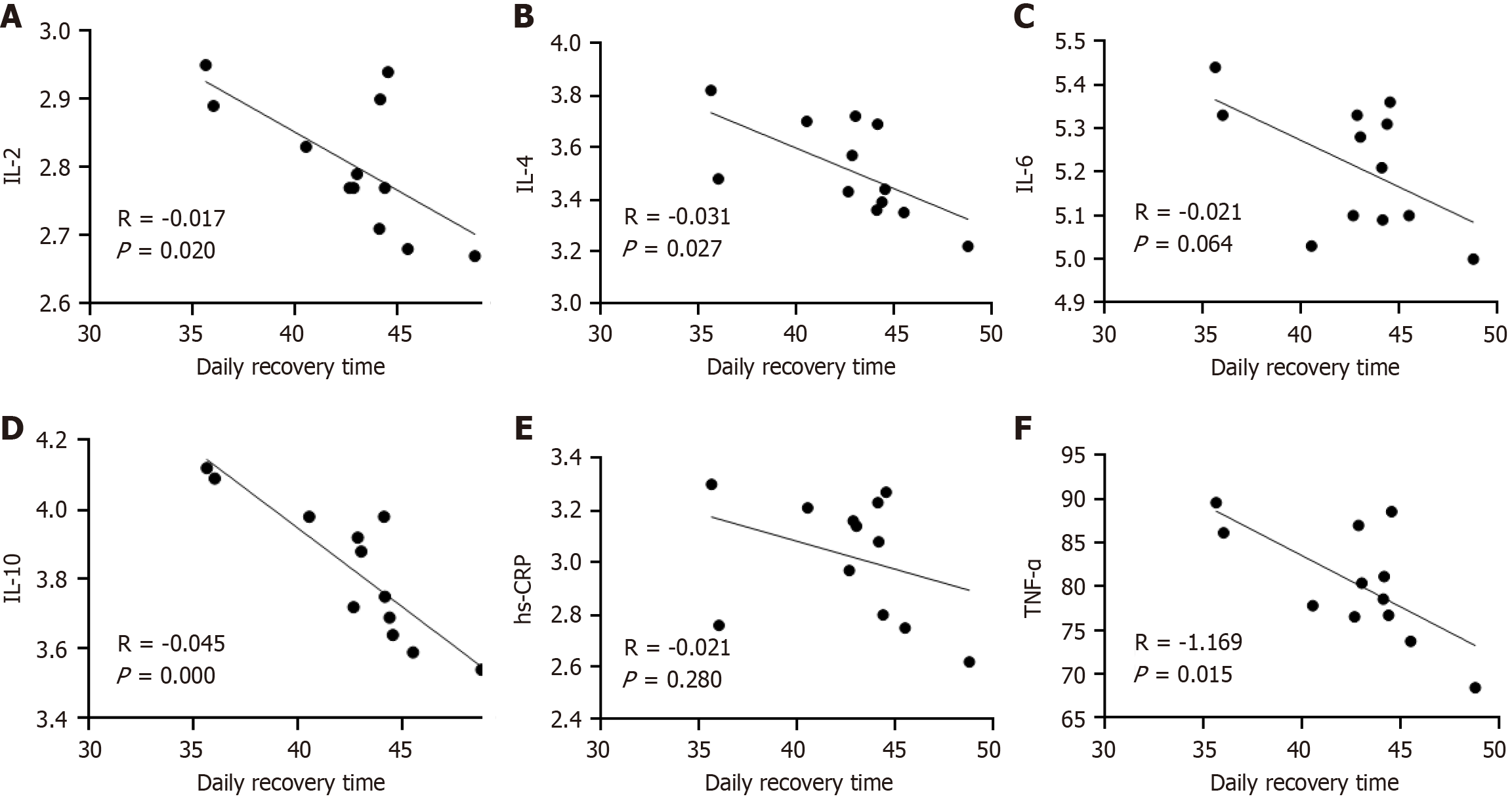
We found no significant intergroup differences in sex, age, or disease course (P > 0.05). The times to first defecation, bowel sound recovery, and anal exhaust were shorter and inflammatory factor levels were lower in the rehabilitation training group than in the routine nursing group (P < 0.05). Pearson correlation analysis showed that gastrin and motilin levels were positively correlated with postoperative rehabilitation (P < 0.05). Interleukin (IL)-2, IL-4, IL-6, IL-10, high-sensitivity C-reactive protein, and tumor necrosis factor-α levels were negatively correlated with postoperative rehabilitation (P < 0.05). Gastrointestinal function was positively correlated (P < 0.05), and levels of inflammatory factors were negatively correlated with postoperative recovery time (P < 0.05).
We found a positive correlation between gastrointestinal function and postoperative rehabilitation training, and a negative correlation between inflammatory factor levels and rehabilitation training in children with intussusception.
Core Tip: In this study, we found that postoperative rehabilitation training in children with intussusception could accelerate the recovery of gastrointestinal function, elevate the levels of gastrin and migratory complex wave, and at the same time, significantly reduce the inflammatory factors, such as interleukin (IL)-2, IL-4, IL-6, IL-10, high-sensitivity C-reactive protein, and tumor necrosis factor-α. This study confirms that the rehabilitation training has a significant effect on the improvement of gastrointestinal function and the alleviation of inflammation, which is an important revelation in the clinical treatment.
- Citation: Wei XY, Huo HC, Li X, Sun SL, Zhang J. Relationship between postoperative rehabilitation style, gastrointestinal function, and inflammatory factor levels in children with intussusception. World J Gastrointest Surg 2024; 16(8): 2640-2648
- URL: https://www.wjgnet.com/1948-9366/full/v16/i8/2640.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i8.2640
Pediatric surgical diseases with purulent blood paroxysms develop rapidly and can induce complications, such as intestinal perforation, intestinal necrosis, and endotoxemia, if not treated in time. This can seriously affect the life and health of children[1]. Currently, the primary clinical operation is to treat children, which is better than[2]. Studies have shown that postoperative prognosis is not only related to the surgical procedure but also to the mode of postoperative rehabilitation to a certain extent[3]. Surgical trauma and the application of anesthetic drugs can cause gastrointestinal dysfunction and inflammatory reactions, such as indigestion, diarrhea, and constipation after surgery, which can delay recovery in children[4]. Therefore, understanding postoperative gastrointestinal function and inflammatory factor levels in children with intussusception is helpful in developing reasonable and effective rehabilitation methods and improving the recovery rate and quality of life of children. In this study, we aimed to explore the effects of different rehabilitation methods on gastrointestinal function and inflammatory factor levels in children, provide a scientific basis for clinicians to formulate individualized rehabilitation programs, improve the rehabilitation effect and quality of life of children with intussusception, reduce the incidence of complications, and provide new ideas and methods for the treatment of acute abdomen in children.
The medical records of 18 children with intussusception who were treated at our hospital between October 2022 and May 2024 were retrospectively analyzed. Patients were divided into a routine nursing group (n = 6) and a rehabilitation training group (n = 12) according to the postoperative rehabilitation method. The study was approved by the local ethics committee.
The inclusion criteria were as follows: (1) Met the diagnostic criteria of intussusception in pediatrics (8th edition)[5]; (2) Successful laparoscopic surgery; (3) Age 1–10 years; (4) Onset time < 3 days prior; (5) Availability of complete clinical data; (6) No malignant tumor or cardiovascular disease; and (7) No symptoms of acute or chronic infection before hospitalization.
The exclusion criteria were as follows: (1) Functional intestinal disease; (2) Congenital intestinal malformation; (3) Coagulation dysfunction; (4) Cognitive or speech disorder; (5) Severe intestinal strangulation or necrosis; and (6) Kidney or liver disease.
Routine nursing group: Postoperatively, the children in this group received routine nursing care, including limb massage before opening their eyes to promote blood circulation and relax their muscles. At the same time, according to the physician’s advice and specific conditions, ibuprofen (Anhui Huachen Pharmaceutical Co., Ltd., National Medicine Zhunzi; H34020169) was used to relieve pain. At 4 hours postoperatively, the children were encouraged to eat and drink a little water; for those without vomiting, nausea, or abdominal pain, enteral nutrition was administered within 1 day postoperatively to accelerate intestinal peristalsis and promote the recovery of gastrointestinal function, before being gradually transitioned to a conventional diet.
Rehabilitation training group: The children in this group received rehabilitation nursing care. In younger patients, the quadriceps femoris and ankle joints were rotated, flexed, and massaged regularly. Older children were instructed to exercise their fists, elbows, and shoulders three times a day for 15 minutes. The rehabilitation training plan was customized according to each patient’s specific situation, and the children were guided and assisted to complete the plan. Children were protected when they were active. Each child’s family members were trained in the program's implementation, taught its importance, and prevented from quitting the practice for fear of pain. During the rehabilitation process, we actively communicated with the children or their parents to provide encouragement, improve compliance and cooperation rates, and promote patient recovery. Both groups underwent a 5-day intervention.
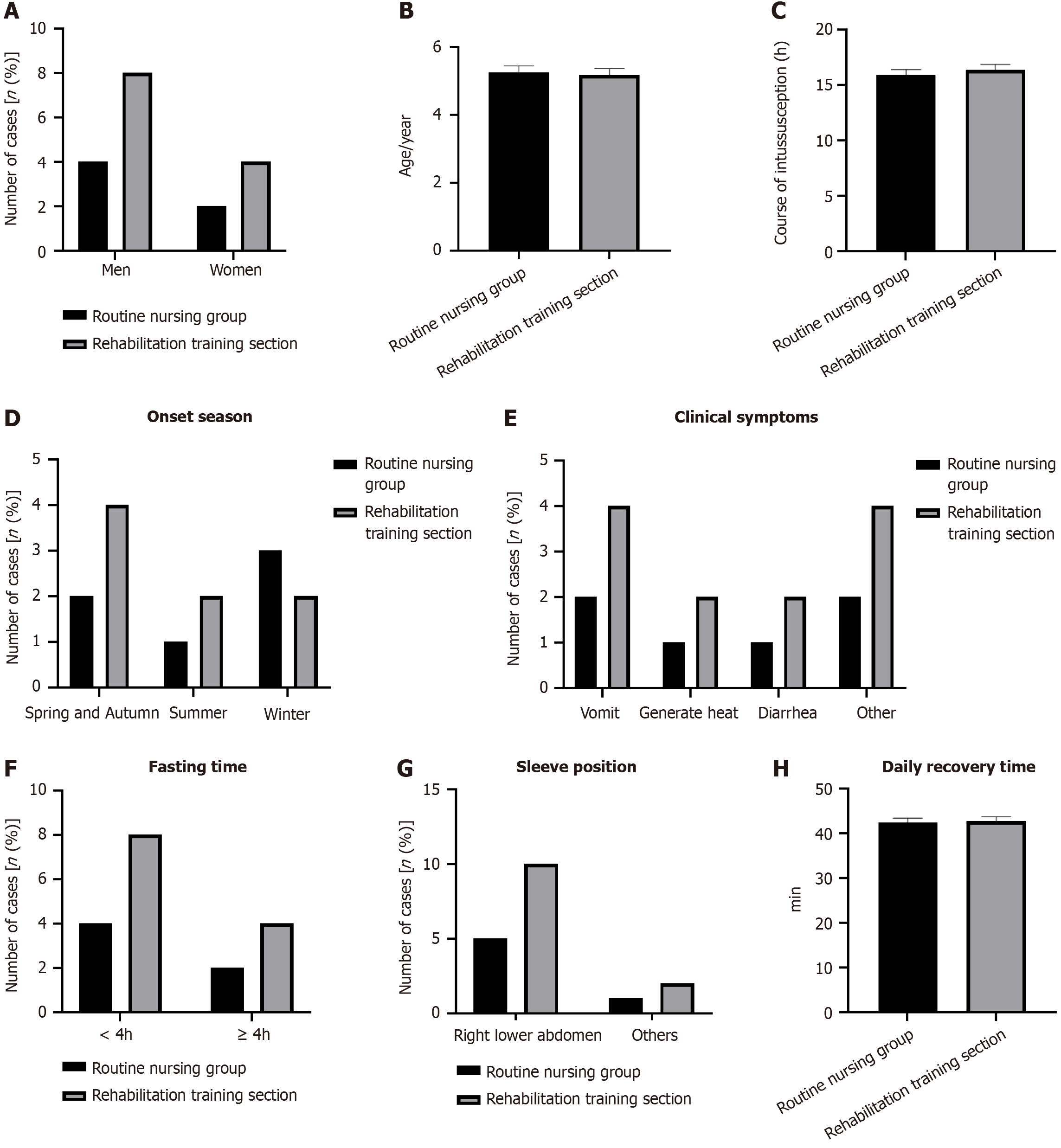
General data: The medical records of the two groups of children were analyzed, and general data, such as sex, age, intussusception course, onset season, clinical symptoms, fasting time, ferrule position, and daily rehabilitation training time, were collected.
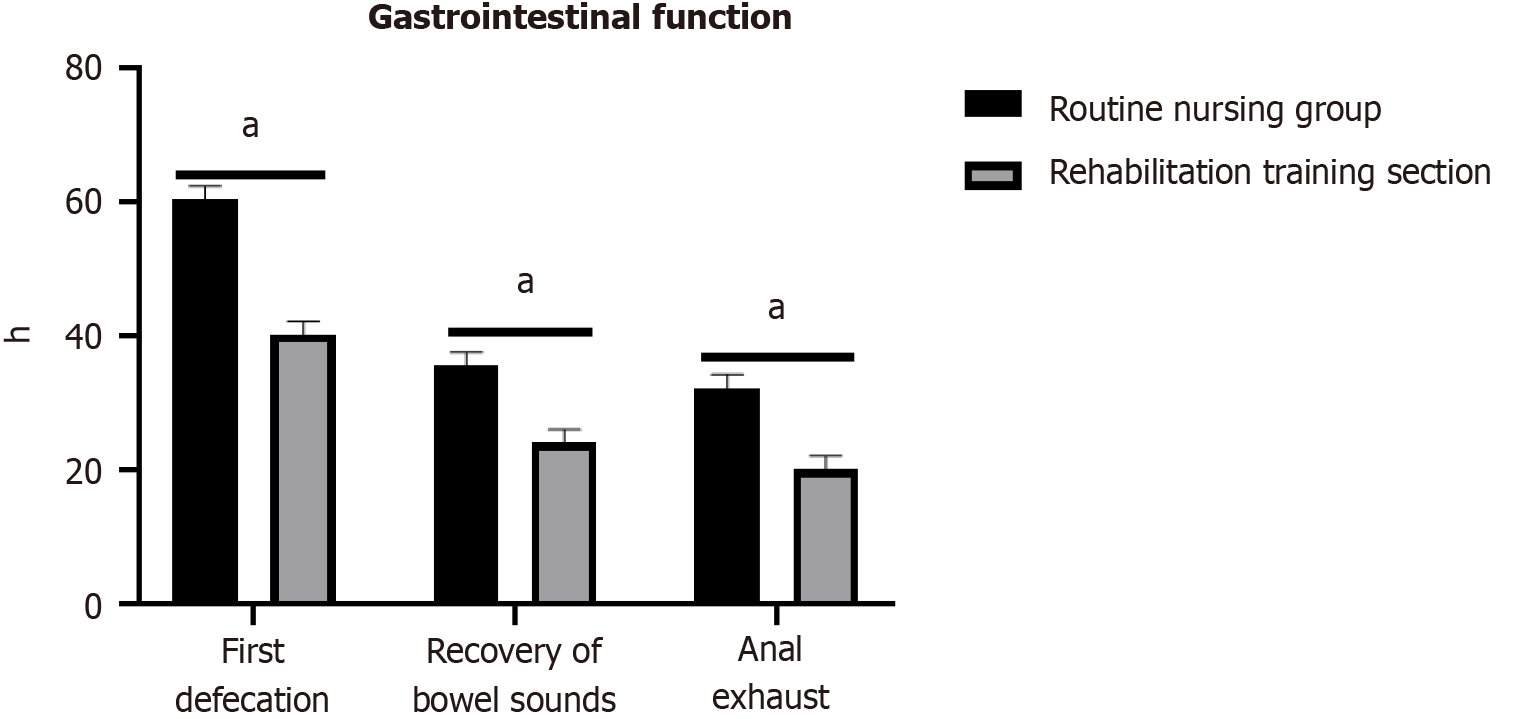
Recovery of gastrointestinal function: The gastrointestinal function indices of children after surgery, including the first defecation time, recovery time of bowel sounds, and anal exhaust time, were evaluated.
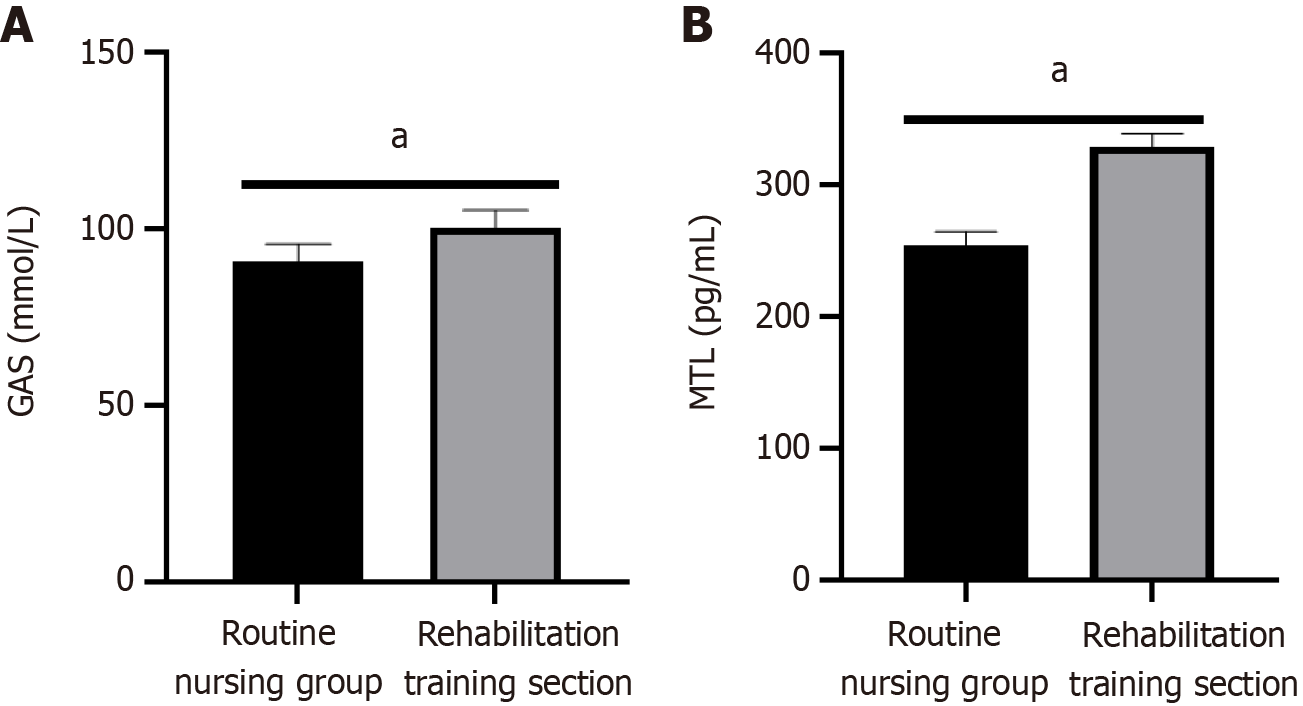
Gastrointestinal function: After 5 days of rehabilitation, 5 mL of fasting venous blood was collected from the children in the morning and centrifuged for 10 minutes (radius, 11 cm; rotation speed, 3000 rpm). The levels of gastrin (GAS) and motilin (MTL) were measured using radioimmunoassay.
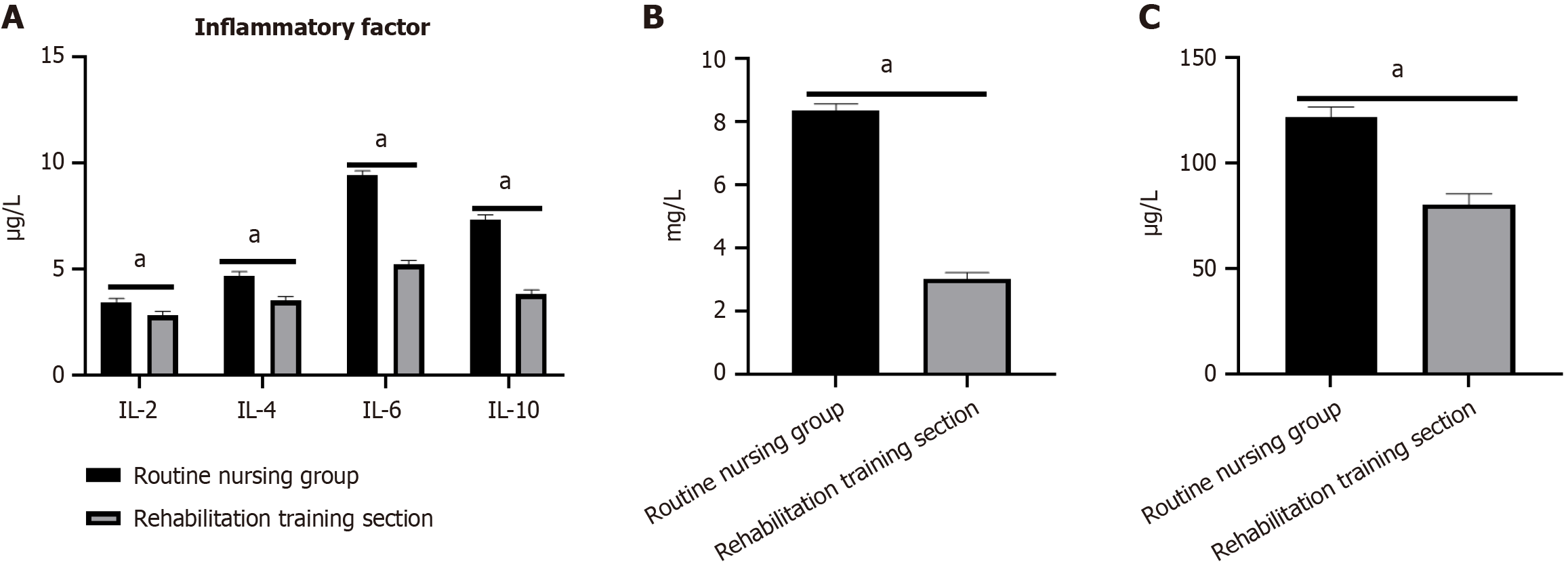
Inflammatory factors: After 5 days of rehabilitation, 8-10 mL of venous blood was taken from each child after fasting, and serum interleukin (IL)-2, IL-4, and tumor necrosis factor-α (TNF-α) were detected by enzyme-linked immunosorbent assay according to the manufacturer’s instructions (Wuhan Jilide Bio).
SPSS 26.0 statistical software was used for data processing and analysis. Normally distributed measurement data were expressed as mean ± SD, and intergroup comparisons were made using the t-test. Counting data were expressed as examples (n) or rates (%), and data were compared using the χ2 test. The Pearson correlation coefficient was used to analyze the relationships among gastrointestinal function, inflammatory factor levels, rehabilitation mode, and rehabilitation time. The significance level was α = 0.05.
We found no statistically significant intergroup differences in general data, including sex, age, disease course, and onset season (P > 0.05; Supplementary Table 1 and Figure 1).
The times to first defecation, bowel sound recovery, and anal exhaust in the rehabilitation training group were shorter than those in the routine nursing group (P < 0.05; Supplementary Table 2 and Figure 2).
Gastrointestinal function was significantly higher in the rehabilitation training group than in the routine nursing group (P < 0.05; Supplementary Table 3 and Figure 3).
The levels of inflammatory factors were significantly lower in the rehabilitation training group than in the routine nursing group (P < 0.05; Supplementary Table 4 and Figure 4).
Pearson correlation analysis was used to analyze the relationships among gastrointestinal function, inflammatory factors, and postoperative rehabilitation in children with intussusception and it was found that GAS, MTL, and postoperative rehabilitation training were significantly positively correlated (P < 0.05). IL-2, IL-4, IL-6, IL-10, high-sensitivity C-reactive protein (hs-CRP), and TNF-α were significantly negatively correlated with postoperative rehabilitation training (P < 0.05; Table 1).
| Index | Pearson correlation | P value (bilateral) | Deviation | Standard error | 95%CI | |
| Lower limit | Upper limit | |||||
| GAS | 0.490 | 0.039 | -0.014 | 0.160 | 0.115 | 0.740 |
| MTL | 0.714 | 0.001 | 0.000 | 0.107 | 0.453 | 0.881 |
| IL-2 | -0.782 | 0.000 | -0.006 | 0.105 | -0.972 | -0.564 |
| IL-4 | -0.871 | 0.000 | -0.016 | 0.043 | -0.964 | -0.798 |
| IL-6 | -0.971 | 0.000 | -0.003 | 0.015 | -0.997 | -0.943 |
| IL-10 | -0.979 | 0.000 | -0.003 | 0.008 | -0.995 | -0.965 |
| hs-CRP | -0.981 | 0.000 | -0.002 | 0.007 | -0.996 | -0.970 |
| TNF-α | -0.921 | 0.000 | -0.003 | 0.028 | -0.974 | -0.867 |
Pearson correlation analysis found that gastrointestinal function was positively correlated with postoperative rehabilitation time (P < 0.05), whereas the inflammatory factors IL-2, IL-4, IL-10, and TNF-α were negatively correlated with postoperative rehabilitation time (P < 0.05). No significant correlation was noted between IL-6 and hs-CRP levels and postoperative recovery time (P > 0.05; Figures 5 and 6).
Intussusception is a surgical disease in children that can be caused by dietary changes, infection, and other factors[6]. In recent years, with continuous progress in medical technology, laparoscopy has become widely used for the treatment of intussusception. Laparoscopy provides a safe environment for reduction, significantly reduces fear and discomfort in children, and can achieve a greater reduction than traditional nonsurgical treatment[7]. However, as an invasive method, laparoscopic intussusception reduction can easily cause trauma, complications, and delayed disease recovery[8]. Therefore, postoperative rehabilitation is important for improving patient prognosis. Some studies have found obvious differences in the hospital stay and gastrointestinal function of postoperative patients among different rehabilitation methods[9]. Therefore, in this study, we aimed to analyze the effects of different postoperative rehabilitation methods on gastrointestinal function and inflammatory factors in children with intussusception to improve the postoperative rehabilitation effect.
Comparison of the general data, gastrointestinal recovery time, gastrointestinal function, and inflammatory factor levels between study groups revealed that the recovery time of the gastrointestinal tract was shorter in the rehabilitation training group than in the routine nursing group. Meanwhile, Pearson correlation analysis revealed that gastrointestinal function was positively correlated with postoperative recovery time, while levels of the inflammatory factors IL-2, IL-4, IL-10, and TNF-α were negatively correlated with postoperative recovery time (P < 0.05).
As a gastrointestinal hormone, GAS is secreted by G cells in the gastric antrum and duodenum, promoting gastric acid secretion and gastric antrum contraction, and directly affecting gastrointestinal secretion and motor function[10,11]. Min et al[12] found that patients who underwent rehabilitation training after laparoscopic surgery showed high GAS and MTL levels and improved gastrointestinal peristalsis. At the same time, Hsieh et al[13] found that rehabilitation training after laparoscopic surgery improved patients’ gastrointestinal function and the corresponding index level. These studies suggest that the postoperative rehabilitation style used in children with intussusception influences their gastrointestinal function. However, this study showed that the GAS and MTL levels in the rehabilitation training group were higher than those in the routine nursing group, and Pearson correlation analysis showed that GAS and MTL levels were positively correlated with postoperative rehabilitation training (P < 0.05). Postoperative rehabilitation training can regulate the hypothalamus-pituitary-adrenal axis and the autonomic nervous system, inhibit sympathetic nerve excitability, improve parasympathetic nerve excitability, and stimulate the gastrointestinal tract contraction and reflexes, thus improving local blood circulation and enhancing gastrointestinal peristalsis, shortening the retention time of food in the stomach, reducing the burden on the stomach, and stimulating GAS and MTL secretion. Simultaneously, rehabilitation training can improve cardiopulmonary function, enhance endurance, reduce stress and anxiety, indirectly promote gastrointestinal function recovery, and improve GAS and MTL levels in children[14,15].
As a key mechanism leading to gastrointestinal dysfunction, inflammatory reactions can affect patients’ postoperative rehabilitation[16]. Thyregod et al[17] showed that exercise rehabilitation has a controlling effect on the inflammatory response in patients. Simultaneously, Kaasgaard et al[18] found that early rehabilitation training can improve the inflammatory state and alleviate the clinical symptoms of patients with chronic obstructive pulmonary disease. These studies suggest that the postoperative rehabilitation style used in children with intussusception influences their gastrointestinal function. However, we also found that the levels of IL-2, IL-4, IL-6, IL-10, hs-CRP, and TNF-α were higher in the rehabilitation training group than in the routine nursing group. Moreover, the Pearson correlation analysis found that inflammatory factor levels were negatively correlated with postoperative rehabilitation training (P < 0.05). This is because rehabilitation training accelerates the blood circulation and metabolism of the children, promotes the accumulation of white blood cells and other immune cells in the blood, helps discharge waste and toxins from the body, promotes the regression of inflammatory reactions, and reduces the secretion of inflammatory factors. Simultaneously, exercises of the elbow and shoulder joints improved the range of motion, enhanced endurance, and reduced the inflammatory reactions caused by joint stiffness or sports injuries. Moreover, rehabilitation training reduces the stress response in children and the secretion of stress hormones such as cortisol, thus reducing the levels of inflammatory factors[19,20]. However, this study was limited by its small sample size and the relatively homogeneous source of study participants; therefore, targeted research in later stages is needed to ensure the authenticity and objectivity of our results.
In summary, gastrointestinal function was better and inflammatory factor levels were lower among children with intussusception who underwent postoperative rehabilitation training compared to routine nursing care. Gastrointestinal function and postoperative rehabilitation training were positively correlated, whereas inflammatory factor levels and postoperative rehabilitation training were negatively correlated.
| 1. | Mu J. Clinical characteristics and risk factors of IgA vasculitis with intussusception and intestinal perforation. J Paediatr Child Health. 2024;60:5-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Li N, Bao Q, Yuan J, Zhou X, Feng J, Zhang W. Open transumbilical intussusception reduction in children: A prospective study. J Pediatr Surg. 2021;56:597-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (1)] |
| 3. | Jamshidi M, Rahimi B, Gilani N. Laparoscopic and open surgery methods in managing surgical intussusceptions: A randomized clinical trial of postoperative complications. Asian J Endosc Surg. 2022;15:56-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Dai L, Gao L, Tao L, Hadinegoro SR, Erkin M, Ying Z, He P, Girsang RT, Vergara H, Akram J, Satari HI, Khaliq T, Sughra U, Celi AP, Li F, Li Y, Jiang Z, Dalimova D, Tuychiev J, Turdikulova S, Ikram A, Flores Lastra N, Ding F, Suhardono M, Fadlyana E, Yan J, Hu Z, Li C, Abdurakhmonov IY, Gao GF; ZF2001 Global Trial Group. Efficacy and Safety of the RBD-Dimer-Based Covid-19 Vaccine ZF2001 in Adults. N Engl J Med. 2022;386:2097-2111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 215] [Cited by in RCA: 198] [Article Influence: 49.5] [Reference Citation Analysis (0)] |
| 5. | Epstein LH, Wilfley DE, Kilanowski C, Quattrin T, Cook SR, Eneli IU, Geller N, Lew D, Wallendorf M, Dore P, Paluch RA, Schechtman KB. Family-Based Behavioral Treatment for Childhood Obesity Implemented in Pediatric Primary Care: A Randomized Clinical Trial. JAMA. 2023;329:1947-1956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 41] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 6. | Bebia Z, Reyes O, Jeanfreau R, Kantele A, De Leon RG, Sánchez MG, Banooni P, Gardener GJ, Rasero JLB, Pardilla MBE, Langley JM, Di Leo CM, Botelho-Nevers E, Buttery J, Laurichesse H, Madhi SA, García AM, Stanley T, Barjat T, Griffith R, Castrejón-Alba MM, de Heusch M, Dieussaert I, Hercor M, Lese P, Qian H, Tullio AN, Henry O. Safety and Immunogenicity of an Investigational Respiratory Syncytial Virus Vaccine (RSVPreF3) in Mothers and Their Infants: A Phase 2 Randomized Trial. J Infect Dis. 2023;228:299-310. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 40] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 7. | Xia S, Du J, Su J, Liu Y, Huang L, Yu Q, Xie Z, Gao J, Xu B, Gao X, Guo T, Liu Y, Zhou X, Yang H. Efficacy, immunogenicity and safety of a trivalent live human-lamb reassortant rotavirus vaccine (LLR3) in healthy Chinese infants: A randomized, double-blind, placebo-controlled trial. Vaccine. 2020;38:7393-7400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 8. | Wu Z, Li Q, Liu Y, Lv H, Mo Z, Li F, Yu Q, Jin F, Chen W, Zhang Y, Huang T, Hu X, Xia W, Gao J, Zhou H, Bai X, Liu Y, Liang Z, Jiang Z, Chen Y, Zhang J, Du J, Yang B, Xing B, Xing Y, Dong B, Yang Q, Shi C, Yan T, Ruan B, Shi H, Fan X, Feng D, Lv W, Zhang D, Kong X, Zhou L, Que D, Chen H, Chen Z, Guo X, Zhou W, Wu C, Zhou Q, Liu Y, Qiao J, Wang Y, Li X, Duan K, Zhao Y, Xu G, Yang X. Efficacy, safety and immunogenicity of hexavalent rotavirus vaccine in Chinese infants. Virol Sin. 2022;37:724-730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 9. | Thiem VD, Anh DD, Ha VH, Hien ND, Huong NT, Nga NT, Thang TC, McNeal MM, Meyer N, Pham HL, Huong NM, Gompana G, Cassels F, Tang Y, Flores J, Rathi N. Safety and immunogenicity of two formulations of rotavirus vaccine in Vietnamese infants. Vaccine. 2021;39:4463-4470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Chilengi R, Mwila-Kazimbaya K, Chirwa M, Sukwa N, Chipeta C, Velu RM, Katanekwa N, Babji S, Kang G, McNeal MM, Meyer N, Gompana G, Hazra S, Tang Y, Flores J, Bhat N, Rathi N. Immunogenicity and safety of two monovalent rotavirus vaccines, ROTAVAC® and ROTAVAC 5D® in Zambian infants. Vaccine. 2021;39:3633-3640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 11. | Tan E, Hoare K, Riley J, Fernando K, Haskell L, McKinlay CJ, Dalziel SR, Braithwaite I. Panic or peace - prioritising infant welfare when medicating feverish infants: a grounded theory study of adherence in a paediatric clinical trial. BMC Pediatr. 2022;22:195. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 12. | Min J, An KY, Park H, Cho W, Jung HJ, Chu SH, Cho M, Yang SY, Jeon JY, Kim NK. Postoperative inpatient exercise facilitates recovery after laparoscopic surgery in colorectal cancer patients: a randomized controlled trial. BMC Gastroenterol. 2023;23:127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 13. | Hsieh HF, Huang IC, Liu Y, Chen WL, Lee YW, Hsu HT. The Effects of Biofeedback Training and Smartphone-Delivered Biofeedback Training on Resilience, Occupational Stress, and Depressive Symptoms among Abused Psychiatric Nurses. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Nambi G, Abdelbasset WK, Alqahtani BA, Alrawaili SM, Abodonya AM, Saleh AK. Isokinetic back training is more effective than core stabilization training on pain intensity and sports performances in football players with chronic low back pain: A randomized controlled trial. Medicine (Baltimore). 2020;99:e20418. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Lopresti AL, Smith SJ, Rea A, Michel S. Efficacy of a curcumin extract (Curcugen™) on gastrointestinal symptoms and intestinal microbiota in adults with self-reported digestive complaints: a randomised, double-blind, placebo-controlled study. BMC Complement Med Ther. 2021;21:40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 16. | Tamakoshi K, Maeda M, Nakamura S, Murohashi N. Very Early Exercise Rehabilitation After Intracerebral Hemorrhage Promotes Inflammation in the Brain. Neurorehabil Neural Repair. 2021;35:501-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Thyregod M, Løkke A, Skou ST, Larsen J, Bodtger U. Changes in systemic inflammation after pulmonary rehabilitation in patients with COPD and severe physical inactivity - an exploratory study. Chron Respir Dis. 2022;19:14799731221112439. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 18. | Kaasgaard M, Rasmussen DB, Andreasson KH, Hilberg O, Løkke A, Vuust P, Bodtger U. Use of Singing for Lung Health as an alternative training modality within pulmonary rehabilitation for COPD: a randomised controlled trial. Eur Respir J. 2022;59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 19. | Wang Y, Yang SL, Luo SX, Tong H, Fang Q, Guo YZ. [Effects of virtual reality in phase I cardiac rehabilitation training for elderly coronary heart disease patients after percutaneous coronary intervention]. Sheng Li Xue Bao. 2023;75:953-961. [PubMed] |
| 20. | Laurindo LF, Santos AROD, Carvalho ACA, Bechara MD, Guiguer EL, Goulart RA, Vargas Sinatora R, Araújo AC, Barbalho SM. Phytochemicals and Regulation of NF-kB in Inflammatory Bowel Diseases: An Overview of In Vitro and In Vivo Effects. Metabolites. 2023;13:96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 101] [Reference Citation Analysis (0)] |