Published online Apr 27, 2024. doi: 10.4240/wjgs.v16.i4.1184
Peer-review started: October 23, 2023
First decision: January 6, 2024
Revised: February 2, 2024
Accepted: March 6, 2024
Article in press: March 6, 2024
Published online: April 27, 2024
Processing time: 182 Days and 5.9 Hours
Splenic rupture associated with Behçet’s syndrome (BS) is extremely rare, and there is no consensus on its management. In this case report, a patient with BS-associated splenic rupture was successfully treated with splenic artery emboli
The patient was admitted for pain in the left upper abdominal quadrant. He was diagnosed with splenic rupture. Multiple oral and genital aphthous ulcers were observed, and acne scars were found on his back. He had a 2-year history of BS diagnosis, with symptoms of oral and genital ulcers. At that time, he was treated with oral corticosteroids for 1 month, but the symptoms did not alleviate. He underwent SAE to treat the rupture. On the first day after SAE, the patient re
SAE might be a good choice for BS-associated splenic rupture based on good sur
Core Tip: This study presents a case of splenic rupture associated with Behçet’s syndrome (BS). BS was confirmed using the International Criteria for Behçet’s Disease. The patient opted for splenic artery embolization (SAE) over splenectomy, resulting in successful hematoma control. The patient’s postoperative recovery was favorable, with no complications, suggesting the effectiveness of SAE in BS-associated splenic rupture management. These findings emphasize the significance of early BS diagnosis and the potential benefits of SAE in selected cases, contributing to the understanding and treatment of this rare but critical manifestation of BS.
- Citation: Zhu GZ, Ji DH. Successful splenic artery embolization in a patient with Behçet’s syndrome-associated splenic rupture: A case report. World J Gastrointest Surg 2024; 16(4): 1184-1188
- URL: https://www.wjgnet.com/1948-9366/full/v16/i4/1184.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i4.1184
Behçet’s syndrome (BS) is an autoimmune disease associated with numerous systemic manifestations, including skin, arthritis, ocular, and vascular lesions[1]. Vascular lesions are characterized by the involvement of vessels of all types (veins and arteries) and sizes. Arterial involvement develops in only 1%-7% of the patients with BS and is mainly observed in isolated cases. Thus, arterial involvement is significantly less frequent than venous involvement and is extremely rare in clinical practice. Nevertheless, it has a high mortality rate. Among patients with arterial involvement, arterial rupture (e.g., BS-associated splenic rupture) is the most common cause of death in patients with BS[2]. Since BS-associated splenic rupture is extremely rare, no consensus exists on its treatment.
A 58-year-old man presented to the emergency department in September 2021, complaining of pain in the abdominal upper left quadrant after a brief loss of consciousness during a bowel movement 24 h earlier.
After the admission examination, the patient consented to partial splenic artery embolization (SAE) to control sub
The patient had a 2-year history of hypertension and type 2 diabetes, both under control. He was diagnosed with BS 2 years ago with symptoms of oral and genital ulcers. At that time, he was treated with oral corticosteroids for 1 month, but the symptoms did not alleviate.
The personal history of the patient was with hypertension and type 2 diabetes. The family history was not specified.
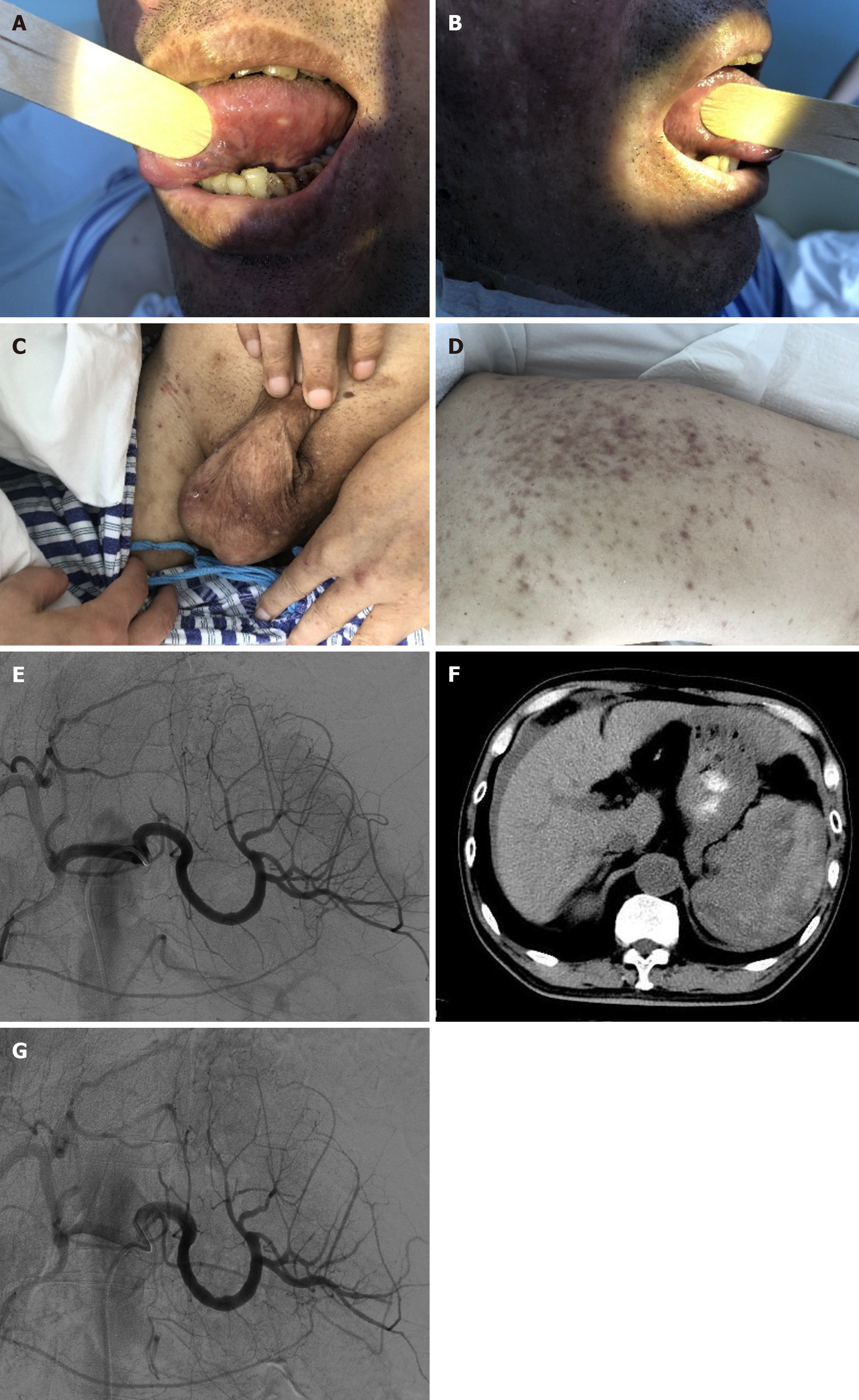
Multiple oral and genital aphthous ulcers were observed (Figure 1A-C). Acne scars were found on his back (Figure 1D). The patient denied any trauma or bouts of coughing.
The low hemoglobin levels (63 g/L) supported internal bleeding. The C-reactive protein levels were elevated at 49.4 mg/L, suggesting significant systemic and/or vascular inflammation. Five days after surgery, the patient’s hemoglobin levels were stable at 65 g/L without significant decline.
After admission, splenic arteriography did not show clear culprit blood vessels or lesions such as aneurysms or pseu
CT showed splenic rupture with a subcapsular hematoma of the spleen (Figure 1F).
A 5F short sheath was placed in the right femoral artery for reverse puncture. An RH catheter was placed for splenic arteriography. No clear signs of contrast agent exudation, aneurysms, or false aneurysms were found in the splenic artery trunk and branches. The embolization was performed using a microcatheter (Progreat; Terumo, Tokyo, Japan) that supplied 900-1200-µm microspheres (Embosphere; Merit Medical Systems, South Jordan, Utah, United States).
Angiography was performed immediately after CT and during SAE and showed reduced swelling laterally to the spleen (Figure 1G). Abdominal CT showed no hematoma hyperplasia. A follow-up CT examination 3 months later showed that the splenic hematoma had formed a stable cystic effusion, suggesting that the patient had a good prognosis after SAE.
The most commonly used surgical treatment for splenic rupture is splenectomy or partial splenectomy[3,4]. To date, there is only a single reported case of BS-associated splenic rupture with splenic artery aneurysm[5], in which the patient was treated with splenectomy, but the patient’s follow-up was not mentioned. Furthermore, complications such as secondary infection can occur after splenectomy because the spleen is the largest peripheral immune organ in humans, participating in the body’s immune response through the production of lymphocytes and monocytes. Hence, splenectomy will likely cause immune system malfunction, resulting in a weakened immune system.
Therefore, spleen preservation is important in maintaining proper immune and hormonal functions, especially in patients with BS. In this manner, SAE is safer for immune function than splenectomy[6]. Still, SAE can carry a risk of hemorrhage, reintervention, and conversion to splenectomy, but no such complications were observed in the patient reported here. It suggests that good surgical practice and material selection might be important factors in preventing adverse reactions. The take-home message of this case is that SAE might be a valuable treatment option for BS-associated splenic rupture, as suggested previously in non-BS cases[7,8].
It must be highlighted that there was no absolute proof that BS caused the splenic rupture in the case reported here. Still, splenic rupture was possibly caused by BS since all other possible causes of splenic rupture (e.g., trauma and bouts of coughing) were excluded, but no pathological evidence supports it. On the other hand, splenic rupture has been reported in BS[5].
A patient with BS-associated splenic rupture was successfully treated with SAE. The postoperative prognosis was good. Although further clinical practice and more cases are needed to confirm the findings, it is suggested that good surgical practices, proper use of surgical materials, and standard medical therapy of SAE might be feasible for treating BS-associated splenic rupture.
| 1. | Emmi G, Bettiol A, Silvestri E, Di Scala G, Becatti M, Fiorillo C, Prisco D. Vascular Behçet's syndrome: an update. Intern Emerg Med. 2019;14:645-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 113] [Article Influence: 16.1] [Reference Citation Analysis (1)] |
| 2. | Chen J, Yao X. A Contemporary Review of Behcet's Syndrome. Clin Rev Allergy Immunol. 2021;61:363-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 3. | Dronamraju SS, Gaidhane SA, Mahalaqqa KN, Gaidhane AM, Andhale AG, Quazi ZS. Splenic Artery Embolization in Subcapsular Splenic Hematoma Secondary to Dengue Hemorrhagic Fever. J Glob Infect Dis. 2021;13:145-147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 4. | Sebastian B, Singhal S, Madhurkar R, Alex A, Uthappa M. Role of splenic artery embolization in gastric variceal hemorrhage due to sinistral portal hypertension. J Clin Interv Radiol. 2019;3:27-36. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Dolar E, Uslusoy H, Kiyici M, Gurel S, Nak SG, Gulten M, Zorluoglu A, Saricaoglu H, Memik F. Rupture of the splenic arterial aneurysm due to Behcet's disease. Rheumatology (Oxford). 2005;44:1327-1328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Tominaga GT, Simon FJ Jr, Dandan IS, Schaffer KB, Kraus JF, Kan M, Carlson SR, Moreland S 3rd, Nelson T, Schultz P, Eastman AB. Immunologic function after splenic embolization, is there a difference? J Trauma. 2009;67:289-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Miller ZA. Splenic artery embolization for atraumatic splenic rupture. J Card Surg. 2020;35:3642-3644. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Ahuja C, Farsad K, Chadha M. An Overview of Splenic Embolization. AJR Am J Roentgenol. 2015;205:720-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 77] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Immunology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Liu P, China; Shonaka T, Japan S-Editor: Zhang H L-Editor: A P-Editor: Xu ZH