Published online Apr 27, 2024. doi: 10.4240/wjgs.v16.i4.1130
Peer-review started: November 14, 2023
First decision: January 5, 2024
Revised: January 23, 2024
Accepted: March 20, 2024
Article in press: March 20, 2024
Published online: April 27, 2024
Processing time: 160 Days and 9.1 Hours
Gallstone disease is one of the most common digestive disorders in the United States and leads to significant morbidity, mortality, and health care utilization.
To expand on earlier findings and investigate prepandemic rates and trends in the gallstone disease burden in the United States using national survey and claims databases.
The National Ambulatory Medical Care Survey, National Inpatient Sample, Na
Gallstone disease prevalence (claims-based, 2019) was 0.70% among commercial insurance enrollees, 1.03% among Medicaid beneficiaries, and 2.09% among Me
The gallstone disease burden in the United States is substantial and increasing, particularly among women, His
Core Tip: We used national survey and claims databases to investigate prepandemic rates and trends in the United States gallstone disease burden. Gallstone disease prevalence (claims-based, 2019) ranged from 0.70% to 2.09% and rose over a decade. Gallstone disease contributed to approximately 2.2 million ambulatory care visits, 1.2 million emergency department visits, 625000 hospital discharges, and 2000 deaths annually. Medical care was higher among women, Hispanics, and older adults and lower among Blacks. Ambulatory care and emergency department visit rates with gallstone disease rose while hospital discharge and mortality rates declined. Cholecystectomies performed included 605000 ambulatory laparoscopic, 280000 inpatient laparoscopic, and 49000 inpatient open procedures annually.
- Citation: Unalp-Arida A, Ruhl CE. Burden of gallstone disease in the United States population: Prepandemic rates and trends. World J Gastrointest Surg 2024; 16(4): 1130-1148
- URL: https://www.wjgnet.com/1948-9366/full/v16/i4/1130.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i4.1130
Gallstones (cholelithiasis) are concretions, usually composed of cholesterol or bilirubin, which develop in the gallbladder. Gallstones may form if bile contains excess cholesterol or bilirubin or insufficient bile salts. Most gallstones in the United States and western countries are cholesterol gallstones. Risk factors include older age, female sex, Native American and Hispanic ethnicity, overweight or obesity, diabetes, smoking, higher parity among women, rapid weight loss, and genetic factors. Non-Hispanic black race-ethnicity, greater alcohol consumption, increased serum cholesterol, and greater phy
Gallstones are common and lead to significant morbidity, mortality, and health care utilization in the United States and worldwide. More than 20 million people in the United States have ultrasound-detected gallbladder disease[1]. The pre
A more recent report on the burden of gastrointestinal, liver, and pancreatic disease in the United States found that cholelithiasis was the physician diagnosis for 863000 office visits and 327000 emergency department visits in the United States in 2016[9]. Cholelithiasis and cholecystitis was the 10th most common among all-listed digestive disease diagnoses from emergency department visits in 2018 with 1.5 million visits and the 5th most common among all-listed digestive disease diagnoses in United States hospitals in 2018 with 741000 admissions[9].
Current estimates of the gallstone disease burden in the United States are useful to all multidisciplinary clinicians, researchers, public health professionals, and policy makers for better planning. We used national survey and claims databases to expand on earlier findings and estimate current trends in the gallstone disease burden in the United States.
The National Ambulatory Medical Care Survey (NAMCS), Healthcare Cost and Utilization Project (HCUP) National Inpatient Sample (NIS), HCUP Nationwide Emergency Department Sample (NEDS), HCUP Nationwide Ambulatory Surgery Sample (NASS), Vital Statistics of the United States, Optum Clinformatics® Data Mart (CDM), and the Centers for Medicare and Medicaid Services (CMS) Medicare 5% Sample and Medicaid databases were used to estimate claims-based prevalence, medical care including cholecystectomy, mortality, and years of potential life lost prior to age 75 years with a primary or other gallstone diagnosis.
The NAMCS is conducted in the United States by the National Center for Health Statistics of the Centers for Disease Control and Prevention (CDC)[10]. It is an annual nationally representative sample survey of office-based outpatient visits to non-federal health care providers. It is a multistage stratified probability sample of geographically defined areas, physician practices within these areas, and patient visits within physician practices.
The HCUP NIS, NEDS, and NASS are maintained by the Agency for Healthcare Research and Quality. The NIS consists of a nationally representative sample of discharges from all participating non-federal hospitals collected annually[11]. It contains data from more than 7 million hospital stays each year (unweighted) and estimates more than 35 million hospitalizations nationally (weighted). Data collected include up to 15 diagnoses and 7 surgical procedures.
The HCUP NEDS consists of a nationally representative sample of hospital-owned emergency department visits from non-federal hospitals collected annually regardless of whether they result in admission[12]. It contains data from over 30 million emergency department visits each year (unweighted) and estimates approximately 145 million emergency de
The HCUP NASS consists of a nationally representative sample of major ambulatory surgery encounters performed in hospital-owned facilities[13]. It contains approximately 7.8 million ambulatory surgery encounters each year and appro
The Vital Statistics of the United States: Multiple Cause-of-Death Data are managed by CDC and include all deaths occurring within the United States collected annually[14]. An underlying cause and up to 20 contributing causes of death were derived from death certificates.
Optum’s CDM is comprised of administrative health care claims for members of large commercial health plans[15]. Administrative claims submitted by providers and pharmacies are verified, adjudicated, and de-identified before in
CMS created the Medicare 5% sample to be representative of the entire population of Medicare beneficiaries and it is housed in the CMS Chronic Conditions Data Warehouse[16]. Data are linked by a unique, unidentifiable beneficiary key.
The CMS Medicaid files include the entire population of Medicaid beneficiaries and are housed in the CMS Chronic Conditions Data Warehouse[6]. Data are linked by a unique, unidentifiable beneficiary key. Medicaid eligibility is based on income below a certain level that varies among states, so Medicaid beneficiaries represent a low-income population.
Gallstone disease morbidity was identified by an International Classification of Diseases (ICD), Ninth Revision, Clinical Modification (ICD-9-CM) code of 574 or an ICD, Tenth Revision, Clinical Modification (ICD-10-CM) code of K80, and gallstone disease mortality by an ICD, Tenth Revision (ICD-10) code of K80. The first-listed diagnosis was considered the primary diagnosis and all remaining diagnoses were considered secondary and included under ‘all-listed’. For national event-level data sources, diagnoses were counted only once under the all-listed category, irrespective of the number of actual diagnoses listed on a medical record or death certificate. In other words, if there was more than one gallstone disease diagnosis listed on a medical record or death certificate, only one diagnosis was counted for the ‘all-listed’ ca
Laparoscopic cholecystectomy was identified by a Current Procedural Terminology (CPT®) code of 47562, 47563 or 47564, an ICD-9 Procedure Coding System (PCS) code of 51.23 or 51.24, or an ICD-10-PCS code of 0FT44 or 0FB44. Open cholecystectomy was identified by a CPT® code of 47600, 47605, 47610, 47612 or 47620, an ICD-9-PCS code of 51.21 or 51.22, or an ICD-10-PCS code of 0FB40, 0FB43, or 0FT40.
Because of potential short-term effects of the coronavirus disease 2019 (COVID-19) pandemic on gallstone disease healthcare utilization and mortality, statistics highlighted in the text are for 2019, while figures present trends through 2020.
Estimates for the total population and by age, sex, race, and Hispanic origin were calculated for each year of national data. Event counts are shown as number in thousands. For calculating United States population rates, annual population data were derived from the national population estimates program of the United States Census Bureau and the CDC. For all rate calculations, population estimates used as the denominator were mid-year population counts by age, sex, race, and Hispanic origin. Rates were age-adjusted by direct standardization using the year 2000 population estimates and are shown per 100000 population[17]. NAMCS, NIS, NEDS, and NASS data were weighted to generate national estimates. Ambulatory care visit (NAMCS) data points were 3-year averages to provide more stable estimates. Ambulatory care numbers and rates represent visits, not persons with a visit. Hospital numbers and rates represent discharges, not persons with an inpatient stay.
Enrollees/beneficiaries were considered gallstone disease patients if they had one or more claims with an ICD-9-CM or ICD-10-CM diagnostic code indicative of gallstone disease in any diagnostic code field. The claims-based prevalence was calculated as the percentage of privately insured enrollees/beneficiaries who qualified as gallstone disease patients in a given year. Estimates were reported overall and stratified by age, gender, race/ethnicity, and region.
Optum© CDM member eligibility files containing birth year, demographics, and eligibility period were linked to inpatient confinement (acute care hospital or skilled nursing facility stay), medical (health care professional services), medical diagnosis, and pharmacy claims files. Privately insured enrollees were included if they: (1) Had a single con
The CMS Medicare 5% sample study population/denominator consisted of beneficiaries who were 65 years or older as of January 1st of the year, resided in the 50 United States states or Washington DC, and were enrolled in fee-for-service Part A or Part B Medicare benefits or in the Medicare Advantage program (Part C/Health Maintenance Organization benefits) at any time during the year. The denominator file which contains demographic and enrollment data was linked by the beneficiary unique identifier to institutional (hospital inpatient stays, hospital outpatient services, skilled nursing facilities, home health agencies and hospice care organizations) or non-institutional (also called Part B; health care professionals, supplies, and services) medical claims files. Estimates from the 5% sample are multiplied by 20 to represent national estimates.
The CMS Medicaid study population/denominator consisted of beneficiaries who were 19 to 64 years as of January 1st of the year, resided in the 50 United States states or Washington DC, and were enrolled in Medicaid benefits at any time during the year. The denominator file which contains demographic and enrollment data was linked by the beneficiary unique identifier to institutional or non-institutional medical claims files. Medicaid eligibility is based on income below a certain level that varies among states, so Medicaid beneficiaries represent a low-income population.
Among 13.7 million commercial insurance enrollees, 96000 had a gallstone disease diagnosis resulting in a claims-based prevalence of 0.70% (2019). Claims-based prevalence was higher among 39.6 million Medicaid beneficiaries, of whom 408000 had a gallstone disease diagnosis for a claims-based prevalence of 1.03% (2019). Claims-based prevalence was highest among Medicare beneficiaries. Among 54.4 million Medicare beneficiaries, 1.1 million had a gallstone disease diagnosis resulting in a claims-based prevalence of 2.09% (2019). Prevalence increased with age among all three groups. Prevalence was higher among women compared with men among commercial insurance enrollees and Medicaid beneficiaries but was higher among male Medicare beneficiaries in recent years. Among commercial insurance enrollees, pre
| Demographic characteristics | Number of enrollees | Number of enrollees with disease | Claims-based prevalence (%) | Ambulatory care visits | Emergency department visits | Inpatient stays | |||
| Number | Rate per 100000 | Number | Rate per 100000 | Number | Rate per 100000 | ||||
| Age (yr) | |||||||||
| 0 to 11 | 1151595 | 74 | 0.01 | 166 | 14 | 1 | 0 | 21 | 2 |
| 12 to 24 | 1513615 | 1746 | 0.12 | 3130 | 207 | 89 | 6 | 319 | 21 |
| 25 to 44 | 2751143 | 12191 | 0.44 | 21940 | 797 | 703 | 26 | 1884 | 68 |
| 45 to 54 | 1522133 | 9860 | 0.65 | 16064 | 1055 | 773 | 51 | 1944 | 128 |
| 55 to 64 | 1683723 | 13626 | 0.81 | 20042 | 1190 | 1966 | 117 | 3776 | 224 |
| 65 to 74 | 2676036 | 27435 | 1.03 | 34291 | 1281 | 8425 | 315 | 9121 | 341 |
| 75+ | 2448780 | 31352 | 1.28 | 34847 | 1423 | 11055 | 451 | 14610 | 597 |
| Sex | |||||||||
| Female | 7184225 | 57525 | 0.80 | 83108 | 1157 | 12915 | 180 | 16716 | 233 |
| Male | 6562800 | 38759 | 0.59 | 47372 | 722 | 10097 | 154 | 14959 | 228 |
| Race-ethnicity | |||||||||
| White | 8855438 | 61929 | 0.70 | 83162 | 939 | 15179 | 171 | 20686 | 234 |
| Black | 1279712 | 10245 | 0.80 | 12817 | 1002 | 2912 | 228 | 3663 | 286 |
| Hispanic | 1562580 | 13974 | 0.89 | 20433 | 1308 | 2832 | 181 | 4140 | 265 |
| Asian | 623622 | 3392 | 0.54 | 4986 | 800 | 542 | 87 | 928 | 149 |
| Unknown | 1425673 | 6744 | 0.47 | 9082 | 637 | 1547 | 109 | 2258 | 158 |
| Region | |||||||||
| Northeast | 1512196 | 11049 | 0.73 | 14288 | 945 | 2738 | 181 | 4146 | 274 |
| Midwest | 3262384 | 19830 | 0.61 | 26775 | 821 | 5077 | 156 | 6714 | 206 |
| South | 5749137 | 44952 | 0.78 | 60159 | 1046 | 10882 | 189 | 14558 | 253 |
| West | 3223308 | 20453 | 0.63 | 29258 | 908 | 4315 | 134 | 6257 | 194 |
| Total | 13747025 | 96284 | 0.70 | 130480 | 949 | 23012 | 167 | 31675 | 230 |
| Demographic characteristics | Number of enrollees | Number of enrollees with disease | Claims-based prevalence (%) | Ambulatory care visits | Emergency department visits | Inpatient Stays | |||
| Number | Rate per 100000 | Number | Rate per 100000 | Number | Rate per 100000 | ||||
| Age (yr) | |||||||||
| 65 to 69 | 20237900 | 308820 | 1.53 | 423580 | 2093 | 141260 | 698 | 61100 | 302 |
| 70 to 74 | 13266460 | 267640 | 2.02 | 352280 | 2655 | 132480 | 999 | 58240 | 439 |
| 75 to 79 | 9036280 | 222320 | 2.46 | 281200 | 3112 | 117780 | 1303 | 52500 | 581 |
| 80 to 84 | 5891120 | 167340 | 2.84 | 195480 | 3318 | 99660 | 1692 | 47100 | 800 |
| 85+ | 5976720 | 173720 | 2.91 | 173100 | 2896 | 126000 | 2108 | 58040 | 971 |
| Sex | |||||||||
| Female | 29919040 | 601540 | 2.01 | 798340 | 2668 | 320720 | 1072 | 142000 | 475 |
| Male | 24489440 | 538300 | 2.20 | 627300 | 2562 | 296460 | 1211 | 134980 | 551 |
| Race | |||||||||
| White | 41376760 | 861180 | 2.08 | 1062720 | 2568 | 459580 | 1111 | 206300 | 499 |
| Black | 4973980 | 95700 | 1.92 | 105460 | 2120 | 61140 | 1229 | 25640 | 515 |
| Other | 8057740 | 182960 | 2.27 | 257460 | 3195 | 96460 | 1197 | 45040 | 559 |
| Region | |||||||||
| Northeast | 9949240 | 216300 | 2.17 | 274340 | 2757 | 111840 | 1124 | 48920 | 492 |
| Midwest | 11818160 | 231920 | 1.96 | 279940 | 2369 | 130720 | 1106 | 57740 | 489 |
| South | 20410320 | 437300 | 2.14 | 550700 | 2698 | 233980 | 1146 | 109480 | 536 |
| West | 12230760 | 254320 | 2.08 | 320660 | 2622 | 140640 | 1150 | 60840 | 497 |
| Total | 54408480 | 1139840 | 2.09 | 1425640 | 2620 | 617180 | 1134 | 276980 | 509 |
| Demographic characteristics | Number of enrollees | Number of enrollees with disease | Claims-based prevalence (%) | Ambulatory care visits | Emergency department visits | Inpatient stays | |||
| Number | Rate per 100000 | Number | Rate per 100000 | Number | Rate per 100000 | ||||
| Age (yr) | |||||||||
| 19 to 34 | 18016135 | 138819 | 0.77 | 169416 | 940 | 100163 | 556 | 28456 | 158 |
| 35 to 44 | 8135908 | 80155 | 0.99 | 88679 | 1090 | 46780 | 575 | 15519 | 191 |
| 45 to 54 | 6837507 | 86815 | 1.27 | 88868 | 1300 | 41658 | 609 | 16890 | 247 |
| 55 to 64 | 6606519 | 102452 | 1.55 | 96526 | 1461 | 39721 | 601 | 19125 | 289 |
| Sex | |||||||||
| Female | 23368766 | 286708 | 1.23 | 341646 | 1462 | 170220 | 728 | 54372 | 233 |
| Male | 16227303 | 121533 | 0.75 | 101843 | 628 | 58102 | 358 | 25618 | 158 |
| Race-ethnicity | |||||||||
| White | 16266919 | 173456 | 1.07 | 196304 | 1207 | 91310 | 561 | 30701 | 189 |
| Black | 7392713 | 62358 | 0.84 | 57154 | 773 | 37617 | 509 | 12727 | 172 |
| Hispanic | 6279192 | 84023 | 1.34 | 95940 | 1528 | 54029 | 860 | 19315 | 308 |
| Asian | 1800629 | 13259 | 0.74 | 16320 | 906 | 4911 | 273 | 2202 | 122 |
| American Indian/Alaska native | 571976 | 7821 | 1.37 | 8035 | 1405 | 4041 | 706 | 2050 | 358 |
| Hawaiian/Pacific Islander | 207441 | 2033 | 0.98 | 1940 | 935 | 1286 | 620 | 378 | 182 |
| Multiracial/unknown | 7077199 | 65291 | 0.92 | 67796 | 958 | 35128 | 496 | 12617 | 178 |
| Region | |||||||||
| Northeast | 8712132 | 82116 | 0.94 | 87273 | 1002 | 40923 | 470 | 17035 | 196 |
| Midwest | 7836180 | 80735 | 1.03 | 94764 | 1209 | 43962 | 561 | 13226 | 169 |
| South | 11095989 | 114258 | 1.03 | 115694 | 1043 | 64653 | 583 | 22782 | 205 |
| West | 11951768 | 131132 | 1.10 | 145758 | 1220 | 78784 | 659 | 26947 | 225 |
| Total | 39596069 | 408241 | 1.03 | 443489 | 1120 | 228322 | 577 | 79990 | 202 |
Gallstones contributed to 2.2 million ambulatory care visits (3-year average for 2014 to 2016), 1.2 million emergency department visits (2019), and 625000 hospital discharges (2019). Ambulatory care visit, emergency department visit, and hospital discharge rates were all higher among women compared with men. Ambulatory care visit rates and hospital discharge rates were highest among Hispanics. Ambulatory care visit rates were higher among Whites compared with Blacks, but hospital discharge rates were similar. Ambulatory care visit rates increased with age. Emergency department visit rates were highest among older adults and similar among middle aged and younger adults. Hospital discharge rates increased with age, especially among persons 65+ years. Hospital discharge rates underestimate the actual burden be
| Demographic characteristics | Ambulatory care visits (2015) | Emergency department visits (2019) | Hospital discharges (2019) | Mortality (2019) | ||||
| Number in thousands | Rate per 100000 | Number in thousands | Rate per 100000 | Number in thousands | Rate per 100000 | Number of deaths | Rate per 100000 | |
| Age (yr) | ||||||||
| 0 to 11 | 2 | 4 | 2 | 5 | 2 | 3 | 0 | 0 |
| 12 to 24 | 148 | 263 | 95 | 172 | 28 | 51 | 3 | 0 |
| 25 to 44 | 565 | 669 | 343 | 392 | 114 | 130 | 61 | 0.1 |
| 45 to 54 | 467 | 1084 | 170 | 417 | 75 | 185 | 66 | 0.2 |
| 55 to 64 | 414 | 1015 | 190 | 447 | 109 | 256 | 190 | 0.5 |
| 65 to 74 | 389 | 1415 | 179 | 570 | 126 | 399 | 307 | 1.0 |
| 75+ | 218 | 1080 | 221 | 977 | 171 | 759 | 1169 | 5.2 |
| Sex | ||||||||
| Female | 1466 | 870 | 756 | 426 | 356 | 186 | 959 | 0.4 |
| Male | 738 | 418 | 444 | 257 | 269 | 152 | 837 | 0.5 |
| Race | ||||||||
| White | 1901 | 691 | - | - | 508 | 169 | 1517 | 0.5 |
| African American | 172 | 380 | - | - | 74 | 166 | 154 | 0.4 |
| Other | 131 | 519 | - | - | 49 | 190 | 125 | 0.5 |
| Hispanic origin | ||||||||
| Hispanic | 600 | 1254 | - | - | 111 | 223 | 157 | 0.4 |
| Not Hispanic | 1604 | 554 | - | - | 521 | 159 | 1639 | 0.5 |
| Total | 2204 | 642 | 1200 | 339 | 625 | 168 | 1796 | 0.5 |
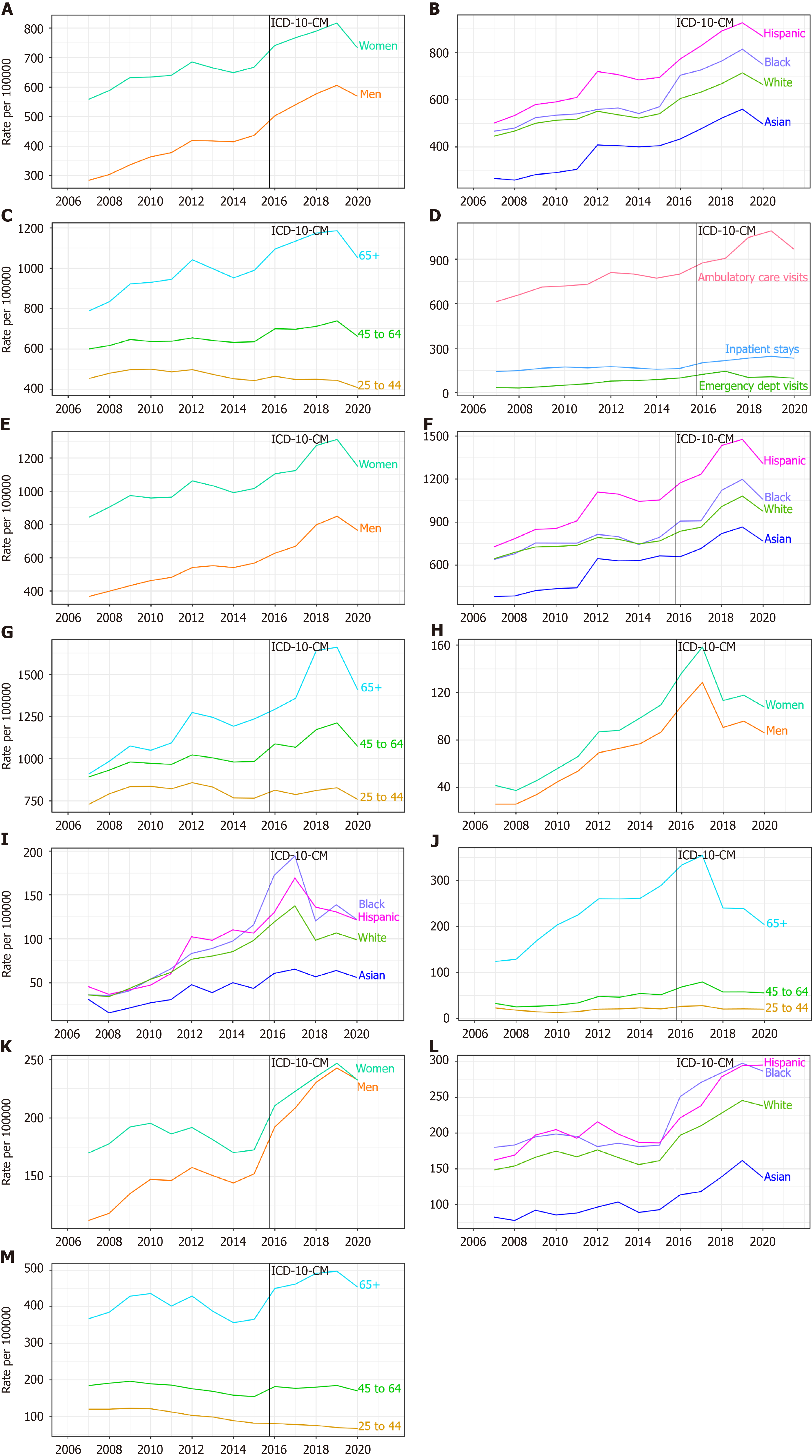
From 2005 to 2016, the ambulatory care visit rate (all-listed per 100000) increased by almost 50% overall (434 to 642) and among sex, racial-ethnic, and age groups. From 2006 to 2019, the emergency department visit rate (all-listed per 100000) increased by more than a third (248 to 339). A rise was seen in both women and men and among all age groups. In contrast, the hospital discharge rate (all-listed per 100000) decreased by 17% (203 to 168) from 2006 to 2019. A decline was seen among each sex, race, and ethnic group, but primarily among older adults (Table 4, Figure 3A-I).
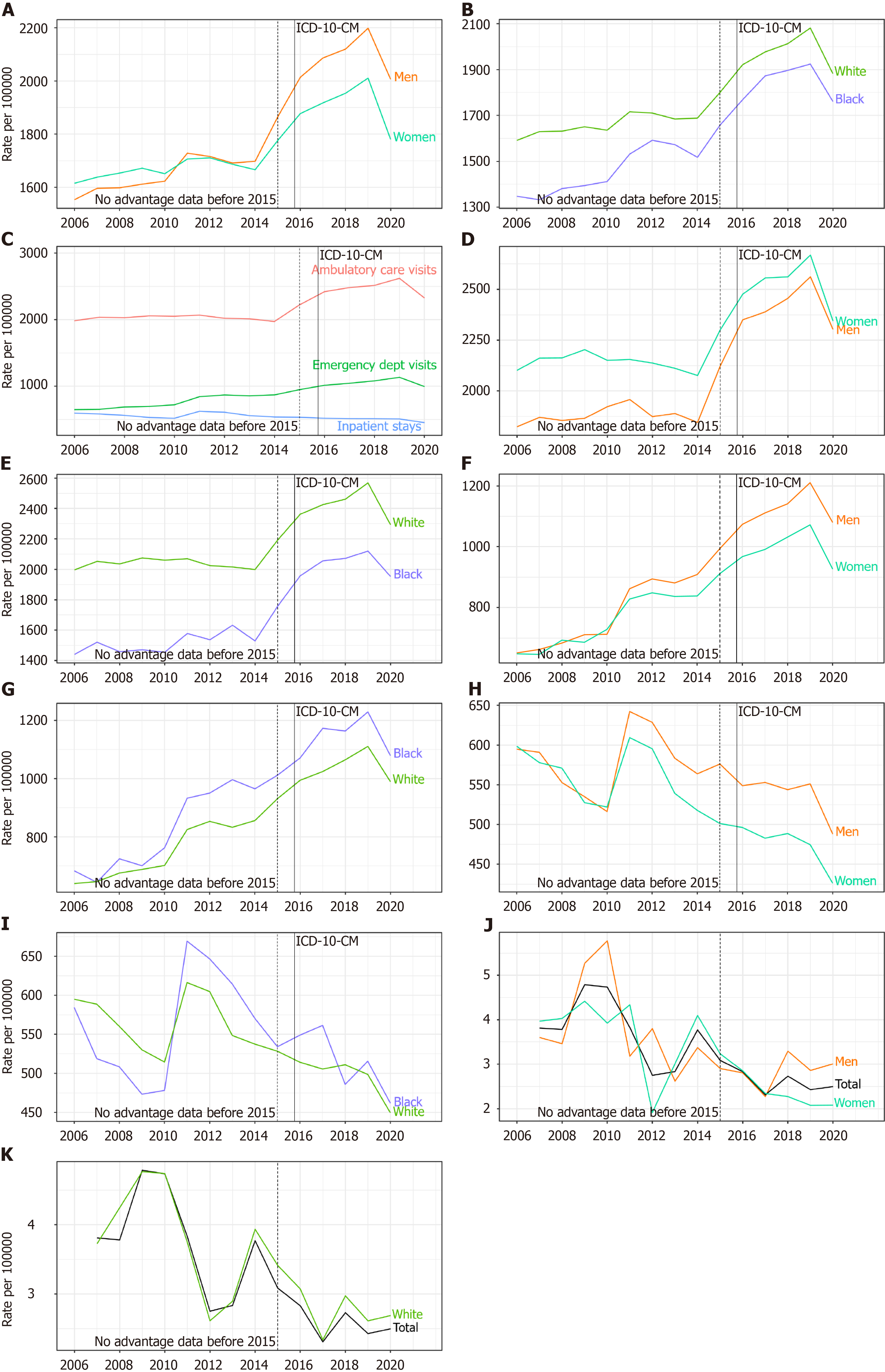
Among commercial insurance enrollees, rates (all-listed per 100000) were higher compared with national data for am
Among Medicare beneficiaries, rates (all-listed per 100000) were higher compared with national data for ambulatory care visits (2221 vs 642 in 2015), emergency department visits (1134 vs 339 in 2019) and hospitalizations (509 vs 168 in 2019). Ambulatory care visit rates were higher among women, but in contrast to national data that included persons of all ages, emergency department visit and hospitalization rates were higher among male compared with female Medicare beneficiaries. Ambulatory care visit rates were higher among Whites compared with Blacks, but in contrast to national data, hospitalization rates were generally higher among Black compared with White Medicare beneficiaries. Emergency de
Among Medicaid beneficiaries aged 19 to 64 years, rates (all-listed per 100000) were higher compared with national data for emergency department visits (577 vs 339 in 2019) and hospitalizations (202 vs 168 in 2019). Among Medicaid beneficiaries, health care utilization rates were highest among Hispanics and American Indians/Alaska natives, intermediate among Whites and Hawaiians/Pacific Islanders, and lowest among Blacks and Asians (Table 3).
Gallstones contributed to 2000 deaths in the United States (2019). Mortality rates were higher among men compared with women and much higher among persons 65+ years compared with younger adults. Rates were lower for Blacks compared with Whites and slightly lower for Hispanics compared with Whites after a steeper decline. From 2006 through 2019, the mortality rate (underlying or other cause per 100000) decreased by more than a quarter overall (0.63 to 0.45) and among each sex and racial-ethnic group, but primarily among adults 65+ years (Table 4, Figures 3J-L, 2J and K).
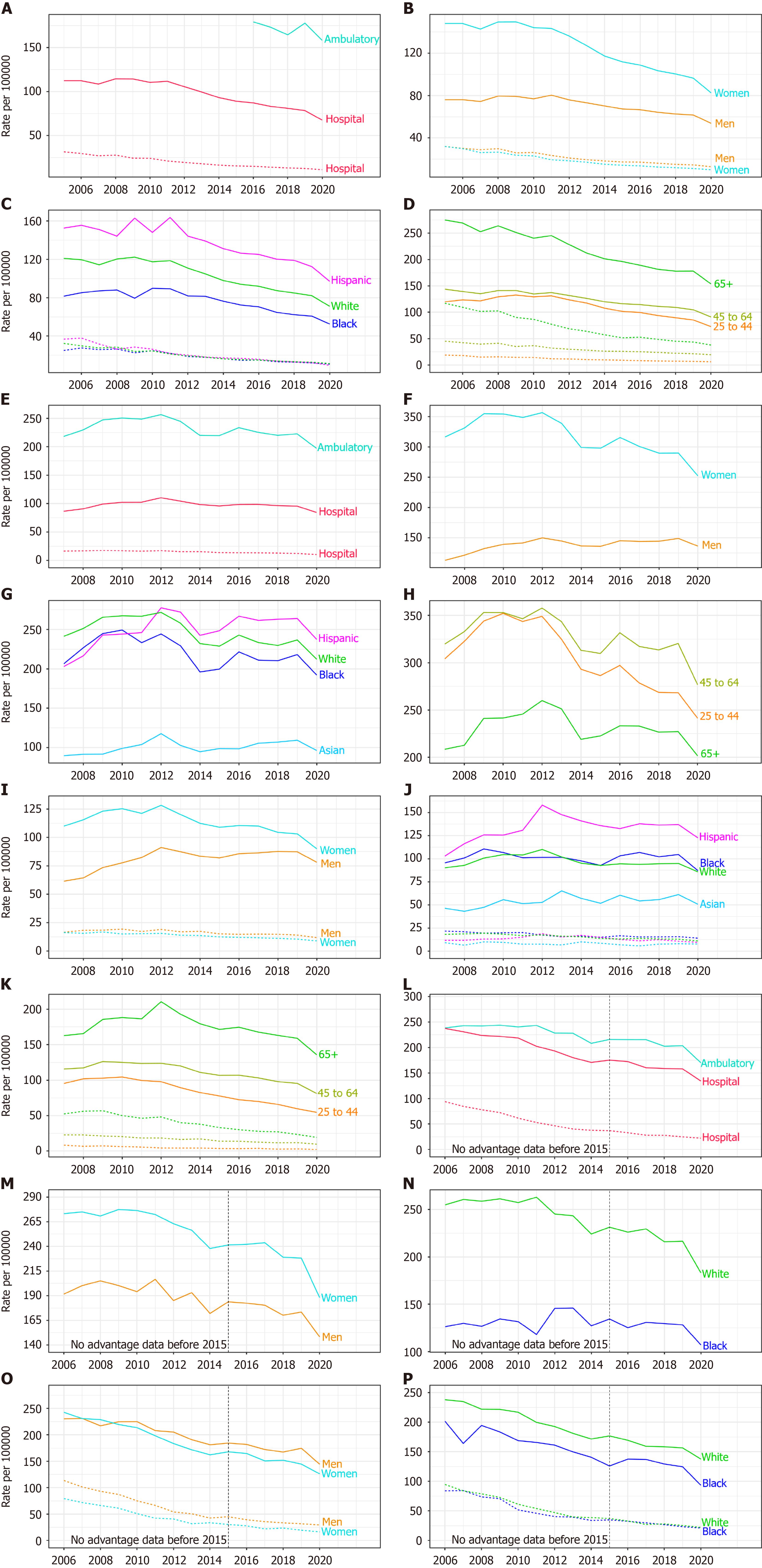
In 2019, cholecystectomies performed in the United States included 605000 ambulatory laparoscopic, 280000 inpatient laparoscopic, 49000 inpatient open, and 1000 ambulatory open procedures. Rates (per 100000) were highest for ambula
| Demographic characteristics | Ambulatory | Inpatient | ||||||
| Number in thousands1 | Rate per 1000001 | Number in thousands2 | Rate per 1000002 | Number in thousands1 | Rate per 1000001 | Number in thousands2 | Rate per 1000002 | |
| Age (yr) | ||||||||
| 0 to 11 | 720 | 2 | 0 | 0 | 615 | 1 | 395 | 1 |
| 12 to 24 | 57257 | 104 | 83 | 0.1 | 20435 | 37 | 1020 | 2 |
| 25 to 44 | 217271 | 248 | 365 | 0.4 | 74860 | 86 | 6005 | 7 |
| 45 to 54 | 109649 | 268 | 294 | 0.7 | 40125 | 98 | 6485 | 16 |
| 55 to 64 | 105287 | 248 | 301 | 0.7 | 47175 | 111 | 11440 | 27 |
| 65 to 74 | 78051 | 248 | 246 | 0.8 | 48685 | 155 | 13585 | 43 |
| 75+ | 37144 | 165 | 168 | 0.7 | 47655 | 211 | 9995 | 44 |
| Sex | ||||||||
| Female | 440796 | 260 | 872 | 0.5 | 172020 | 96 | 22265 | 11 |
| Male | 164542 | 96 | 584 | 0.3 | 107520 | 62 | 26660 | 15 |
| Race | ||||||||
| White | - | - | - | - | 232640 | 82 | 40298 | 13 |
| African American | - | - | - | - | 27545 | 61 | 5485 | 12 |
| Other | - | - | - | - | 21967 | 82 | 3626 | 14 |
| Hispanic origin | ||||||||
| Hispanic | - | - | - | - | 60436 | 112 | 5893 | 12 |
| Not Hispanic | - | - | - | - | 221716 | 72 | 43516 | 13 |
| Total | 605379 | 178 | 1456 | 0.4 | 279550 | 78 | 48925 | 13 |
Among commercial insurance enrollees, rates (per 100000 in 2019) were higher compared with national data for ambu
| Demographic characteristics | Ambulatory | Inpatient | ||||||
| Number in thousands1 | Rate per 1000001 | Number in thousands2 | Rate per 1000002 | Number in thousands1 | Rate per 1000001 | Number in thousands2 | Rate per 1000002 | |
| Age (yr) | ||||||||
| 0 to 24 | 1306 | 49 | 2 | 0.1 | 293 | 11 | 10 | 0 |
| 25 to 44 | 7383 | 268 | 22 | 0.8 | 1641 | 60 | 85 | 3 |
| 45 to 64 | 10270 | 320 | 62 | 1.9 | 3059 | 95 | 380 | 12 |
| 65+ | 11646 | 227 | 137 | 2.7 | 8147 | 159 | 1202 | 24 |
| Sex | ||||||||
| Female | 20830 | 290 | 111 | 1.5 | 7410 | 103 | 756 | 11 |
| Male | 9775 | 149 | 112 | 1.7 | 5730 | 87 | 921 | 14 |
| Race-ethnicity | ||||||||
| White | 20966 | 237 | 151 | 1.7 | 8406 | 95 | 1147 | 13 |
| Black | 2791 | 218 | 27 | 2.1 | 1339 | 105 | 201 | 16 |
| Hispanic | 4125 | 264 | 22 | 1.4 | 2140 | 137 | 168 | 11 |
| Asian | 680 | 109 | 7 | 1.1 | 382 | 61 | 50 | 8 |
| Unknown | 2043 | 143 | 16 | 1.1 | 873 | 61 | 111 | 8 |
| Region | ||||||||
| Northeast | 2383 | 158 | 22 | 1.5 | 1364 | 90 | 182 | 12 |
| Midwest | 7787 | 239 | 43 | 1.3 | 2697 | 83 | 413 | 13 |
| South | 14904 | 259 | 123 | 2.1 | 6277 | 109 | 775 | 14 |
| West | 5531 | 172 | 35 | 1.1 | 2802 | 87 | 307 | 10 |
| Total | 30605 | 223 | 223 | 1.6 | 13140 | 96 | 1677 | 12 |
Among Medicare beneficiaries, rates (per 100000 in 2019) were higher compared with national data for ambulatory laparoscopic (204 vs 178), inpatient laparoscopic (158 vs 78), and inpatient open (25 vs 13) cholecystectomies. Ambulatory laparoscopic cholecystectomy rates were higher among women, but in contrast to national data inpatient laparoscopic and open cholecystectomy rates were higher among male compared with female Medicare beneficiaries. Among Me
| Demographic characteristics | Ambulatory | Inpatient | ||||||
| Number in thousands1 | Rate per 1000001 | Number in thousands2 | Rate per 1000002 | Number in thousands1 | Rate per 1000001 | Number in thousands2 | Rate per 1000002 | |
| Age (yr) | ||||||||
| 65 to 69 | 44920 | 222 | 240 | 1.2 | 23360 | 115 | 4060 | 20 |
| 70 to 74 | 31080 | 234 | 300 | 2.3 | 21260 | 160 | 3380 | 26 |
| 75 to 79 | 19840 | 220 | - | - | 17720 | 196 | 2480 | 27 |
| 80 to 84 | 9640 | 164 | - | - | 12600 | 214 | 1840 | 31 |
| 75+ | 5280 | 88 | - | - | 11060 | 185 | 1760 | 29 |
| Sex | ||||||||
| Female | 68280 | 228 | 460 | 1.5 | 43220 | 145 | 5780 | 19 |
| Male | 42480 | 174 | 460 | 1.9 | 42780 | 175 | 7740 | 32 |
| Race | ||||||||
| White | 89580 | 217 | 740 | 1.8 | 64800 | 157 | 10480 | 25 |
| Black | 6380 | 128 | - | - | 6200 | 125 | 1160 | 23 |
| Other | 14800 | 184 | - | - | 15000 | 186 | 1880 | 23 |
| Region | ||||||||
| Northeast | 15480 | 156 | - | - | 12720 | 128 | 2480 | 25 |
| Midwest | 25100 | 212 | 280 | 2.4 | 17620 | 149 | 3020 | 26 |
| South | 49260 | 241 | 280 | 1.4 | 36280 | 178 | 5860 | 29 |
| West | 20920 | 171 | - | - | 19380 | 159 | 2160 | 18 |
| Total | 110760 | 204 | 920 | 1.7 | 86000 | 158 | 13520 | 25 |
Among Medicaid beneficiaries, rates (per 100000 in 2019) were higher compared with national data for ambulatory laparoscopic (261 vs 178) and inpatient laparoscopic (112 vs 78) cholecystectomies, but lower for inpatient open pro
| Demographic characteristics | Ambulatory | Inpatient | ||||||
| Number in thousands1 | Rate per 1000001 | Number in thousands2 | Rate per 1000002 | Number in thousands1 | Rate per 1000001 | Number in thousands2 | Rate per 1000002 | |
| Age (yr) | ||||||||
| 19 to 34 | 48231 | 268 | - | - | 19107 | 106 | 712 | 4.0 |
| 35 to 44 | 22854 | 281 | - | - | 9345 | 115 | 704 | 8.7 |
| 45 to 54 | 17784 | 260 | - | - | 8105 | 119 | 950 | 13.9 |
| 55 to 64 | 14468 | 219 | - | - | 7698 | 117 | 1235 | 18.7 |
| Sex | ||||||||
| Female | 84647 | 362 | - | - | 33167 | 142 | 1825 | 7.8 |
| Male | 18690 | 115 | - | - | 11088 | 68 | 1776 | 10.9 |
| Race-ethnicity | ||||||||
| White | 52396 | 322 | 252 | 1.5 | 17112 | 105 | 1690 | 10.4 |
| Black | 11598 | 157 | - | - | 6005 | 81 | 600 | 8.1 |
| Hispanic | 17567 | 280 | - | - | 11268 | 179 | 484 | 7.7 |
| Asian | 1892 | 105 | - | - | 1182 | 66 | - | - |
| American Indian/Alaska native | 2173 | 380 | - | - | 1038 | 182 | - | - |
| Hawaiian/Pacific Islander | 459 | 221 | - | - | 233 | 112 | - | - |
| Multiracial/unknown | 17252 | 244 | - | - | 7417 | 105 | 631 | 8.9 |
| Region | ||||||||
| Northeast | 17392 | 200 | - | - | 8986 | 103 | 617 | 7.1 |
| Midwest | 25378 | 324 | - | - | 7661 | 98 | 887 | 11.3 |
| South | 33066 | 298 | 237 | 2.1 | 11824 | 107 | 1133 | 10.2 |
| West | 27501 | 230 | - | - | 15784 | 132 | 964 | 8.1 |
| Total | 103337 | 261 | 521 | 1.3 | 44255 | 112 | 3601 | 9.1 |
In this report, we expanded on earlier findings and investigated current trends in the gallstone disease burden in the United States using national survey and claims databases[18]. We found that the gallstone disease burden in the United States is substantial and increasing, particularly among women, Hispanics, and older adults. The prevalence of gallstone disease has increased, especially among older adults, based on claims diagnoses among both commercial insurance and Medicare enrollees. This is consistent with our previous findings using data from the National Health and Nutrition Examination Survey of a doubling of the gallstone disease prevalence in the United States population over the past three decades, possibly because of the worsening of metabolic risk factors and growth of laparoscopic cholecystectomy[4]. In the current report, prevalence was higher among older adults, women, American Indians/Alaska natives and Hispanics, and lower among Blacks (except among commercial insurance enrollees) and Asians, consistent with known risk factors. Among the three claims data sources used in the current analysis, prevalence was highest among Medicare beneficiaries (2.09%) as expected given that older age is a risk factor for gallstone disease. Prevalence was higher among Medicaid beneficiaries compared with commercial insurance enrollees (1.03% vs 0.70%). This may be because Medicaid beneficiaries represent a lower income group compared with persons with commercial insurance and gallstone disease was associated with lower socioeconomic status in the United States[4].
The mortality rate associated with gallstone disease is low, but the economic burden on the health care system is high. Because cholecystectomy is one of the most common procedures in the United States, gallstone disease and other biliary tract diseases are the most expensive digestive condition. According to a recent report, biliary tract diseases accounted for the highest health care expenditure ($16.9 billion) out of 23 digestive conditions that resulted in a total expenditure of $119.6 billion in 2018[9]. Gallstone disease mortality has continued to decline in recent years resulting in an approximately 80% lower mortality rate over the past four decades, primarily due to a decrease among older adults[6]. Although gallstone disease is more common among women and women had higher medical care rates, the mortality rate was higher among men. Sex differences in gallbladder disease severity may be a factor. Men were found more likely to pre
In contrast to mortality, rates of both ambulatory care visits to physicians’ offices and emergency department visits with gallstone disease increased since the mid-2000s. Hospital discharge rates declined beginning in the early 1990s due to the shift to outpatient laparoscopic cholecystectomy, then stabilized between 2000 and 2011, after which they again decreased[5]. The decline in recent years was primarily among older adults (Figure 3H) and may be the result of two decades of widespread use of laparoscopic cholecystectomy. Hospital discharge rates underestimate the actual burden because most hospitalizations with gallstones were for cholecystectomy and a high proportion of cholecystectomies were performed laparoscopically without an overnight stay, and therefore, were not included in hospitalization statistics. In contrast to national hospitalization data, among commercial insurance enrollees hospitalization rates increased. Blacks had lower ambulatory care visit and mortality rates, but similar hospital discharge rates compared with whites. Blacks may be in lower socioeconomic groups and have less access to care. They may also receive care in later stages of gallstone disease that may require inpatient hospitalization.
Most cholecystectomies are now performed laparoscopically in an ambulatory setting. Ambulatory laparoscopic cho
The data used in this report have limitations. For national data sources, ambulatory care numbers and rates represent visits, not persons with a visit and hospital numbers and rates represent discharges, not persons with an inpatient stay. National health care data do not include care in federal facilities and NEDS and NASS include only hospital-owned emergency departments and ambulatory surgery facilities, respectively; therefore, rates based on the United States po
The limitations are offset by the following strengths. NAMCS data were obtained from provider records. HCUP data sources are the largest all-payer inpatient, emergency department, and ambulatory surgery databases in the United States. National health care and Medicare data were weighted to provide national estimates, and mortality data include all deaths occurring in the United States. CDM, Medicare, and Medicaid data are person-level and claim-based pre
Because of potential short-term effects of the COVID-19 pandemic on gallstone disease healthcare utilization and mortality, we calculated trends using rates for 2019, while figures present data through 2020. Between 2019 and 2020, there were generally small decreases in medical care use with gallstone disease and increases in gallstone disease mor
The burden of gallstone disease in the United States is considerable and rising. Although the gallstone disease mortality rate has decreased over the past four decades leading to a low case fatality rate, medical care devoted to gallstone disease is significant. Cholecystectomy is one of the most common digestive disease surgical procedures. Gallstone disease prevalence (claims based), ambulatory care visit, and emergency department visit rates are increasing, and the app
The authors thank Bryan Sayer, MHS, for statistical analysis and Helen Corns, MPH, for statistical programming and figure creation. The work was supported by a contract from the National Institute of Diabetes and Digestive and Kidney Diseases, No. 75N94022F00050.
| 1. | Everhart JE, Khare M, Hill M, Maurer KR. Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology. 1999;117:632-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 549] [Cited by in RCA: 546] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 2. | Ruhl CE, Everhart JE. Gallstone disease is associated with increased mortality in the United States. Gastroenterology. 2011;140:508-516. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 151] [Cited by in RCA: 140] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 3. | Unalp-Arida A, Der JS, Ruhl CE. Longitudinal Study of Comorbidities and Clinical Outcomes in Persons with Gallstone Disease Using Electronic Health Records. J Gastrointest Surg. 2023;27:2843-2856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Unalp-Arida A, Ruhl CE. Increasing gallstone disease prevalence and associations with gallbladder and biliary tract mortality in the US. Hepatology. 2023;77:1882-1895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 87] [Article Influence: 29.0] [Reference Citation Analysis (0)] |
| 5. | Everhart JE, Ruhl CE. Burden of digestive diseases in the United States Part III: Liver, biliary tract, and pancreas. Gastroenterology. 2009;136:1134-1144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 511] [Cited by in RCA: 606] [Article Influence: 35.6] [Reference Citation Analysis (0)] |
| 6. | Everhart JE. Gallstones. In: Everhart JE, editor. Digestive diseases in the United States: epidemiology and impact. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Washington, DC: US Government Printing Office, 1994; NIH Publication No. 94–1447: 647–690. |
| 7. | Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Report. 2009;1-25. [PubMed] |
| 8. | National Institute of Diabetes and Digestive and Kidney Diseases. NIDDK Strategic Plan for Research. [cited 13 March 2024]. Available from: https://www.niddk.nih.gov/about-niddk/strategic-plans-reports/niddk-strategic-plan-for-research. |
| 9. | Peery AF, Crockett SD, Murphy CC, Jensen ET, Kim HP, Egberg MD, Lund JL, Moon AM, Pate V, Barnes EL, Schlusser CL, Baron TH, Shaheen NJ, Sandler RS. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2021. Gastroenterology. 2022;162:621-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 583] [Article Influence: 145.8] [Reference Citation Analysis (1)] |
| 10. | Centers for Disease Control and Prevention. National Center for Health Statistics. [cited 13 March 2024]. Available from: https://www.cdc.gov/nchs/ahcd/index.htm. |
| 11. | Agency for Healthcare Research and Quality. [cited 13 March 2024]. Available from: https://www.hcup-us.ahrq.gov/nisoverview.jsp#whats. |
| 12. | Agency for Healthcare Research and Quality. [cited 13 March 2024]. Available from: https://www.hcup-us.ahrq.gov/nedsoverview.jsp. |
| 13. | Agency for Healthcare Research and Quality. [cited 13 March 2024]. Available from: https://www.hcup-us.ahrq.gov/nassoverview.jsp. |
| 14. | National Bureau of Economic Research. Mortality Data - Vital Statistics NCHS Multiple Cause of Death Data. [cited 13 March 2024]. Available from: https://www.nber.org/research/data/mortality-data-vital-statistics-nchs-multiple-cause-death-data. |
| 15. | OPTUM®. Clinformatics® Data Mart Database. [cited 13 March 2024]. Available from: https://www.optum.com/content/dam/optum/resources/productSheets/Clinformatics_for_Data_Mart.pdf. |
| 16. | Chronic Conditions Data Warehouse. Centers for Medicare & Medicaid Services. [cited 13 March 2024]. Available from: https://www2.ccwdata.org/web/guest/home/. |
| 17. | Anderson RN, Rosenberg HM. Age standardization of death rates: implementation of the year 2000 standard. Natl Vital Stat Rep. 1998;47:1-16, 20. [PubMed] |
| 18. | Unalp-Arida A, Ruhl CE. The Burden of Digestive Diseases in the United States Population. medRxiv. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Bailey KS, Marsh W, Daughtery L, Hobbs G, Borgstrom D. Sex Disparities in the Presentation of Gallbladder Disease. Am Surg. 2022;88:201-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 20. | Fenelon A, Chinn JJ, Anderson RN. A comprehensive analysis of the mortality experience of hispanic subgroups in the United States: Variation by age, country of origin, and nativity. SSM Popul Health. 2017;3:245-254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 21. | Janeway MG, Sanchez SE, Rosen AK, Patts G, Allee LC, Lasser KE, Dechert TA. Disparities in Utilization of Ambulatory Cholecystectomy: Results From Three States. J Surg Res. 2021;266:373-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Research Data Assistance Center. Getting Started with CMS Data. [cited 13 March 2024]. Available from: https://resdac.org/getting-started-cms-data. |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ker CG, Taiwan; Qiao T, China; Reshetnyak VI, Russia; Yang LY, China S-Editor: Wang JJ L-Editor: A P-Editor: Xu ZH