Published online Feb 27, 2024. doi: 10.4240/wjgs.v16.i2.596
Peer-review started: September 13, 2023
First decision: November 1, 2023
Revised: December 10, 2023
Accepted: January 22, 2024
Article in press: January 22, 2024
Published online: February 27, 2024
Processing time: 165 Days and 2.6 Hours
Hemolymphangioma of the jejunum is rare and lacks clinical specificity, and can manifest as gastrointestinal bleeding, abdominal pain, and intestinal obstruction. Computed tomography, magnetic resonance imaging, and other examinations show certain characteristics of the disease, but lack accuracy. Although capsule endoscopy and enteroscopy make up for this deficiency, the diagnosis also still re
A male patient was admitted to the hospital due to abdominal distension and abdominal pain, but a specific diagnosis by computed tomography examination was not obtained. Partial resection of the small intestine was performed by robotic surgery, and postoperative pathological biopsy confirmed the diagnosis of hemo
Robotic surgery is an effective way to treat hemolymphangioma through minima
Core Tip: Endoscopy and computed tomography are often used for the diagnosis of hemolymphangioma of the jejunum. Laparotomy is a traditional treatment for this tumor. Our study was the first to introduce robotic surgical techniques, bringing new possibilities for the treatment of this tumor. This procedure can reduce surgical trauma and pain and accelerate recovery. In addition, robotic surgery can also improve the accuracy of the procedure. The presented patient recovered quickly and had no serious complications. Our results indicate that robotic surgery for jejunal angiolangioma is feasible, and provides better treatment options for the patients.
- Citation: Li TN, Liu YH, Zhao J, Mu H, Cao L. Treatment of hemolymphangioma by robotic surgery: A case report. World J Gastrointest Surg 2024; 16(2): 596-600
- URL: https://www.wjgnet.com/1948-9366/full/v16/i2/596.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i2.596
Hemolymphangioma occurs in the transition area between the lymphatic system and the vascular system of the human body. The lesion site forms a cystic tumor composed of lymphatic vessels and blood vessels, commonly seen in the skin, soft tissues, and internal organs. The etiology of this disease is unknown, but is related to innate factors. In clinical pre
In our case, robotic surgery was applied for the first time. Under the concept of Enhanced Recovery after Surgery, we achieved a good combination of minimally invasive and radical resection.
A 47-year-old man visited another hospital due to abdominal pain for 2 d, and abdominal CT suggested a small intestine-occupying lesion. The patient was admitted to our hospital for further examination on November 23, 2022. The ab
A 47-year-old man visited another hospital due to abdominal pain for 2 d, and abdominal CT suggested a small intestine-occupying lesion. The patient was admitted to our hospital for further examination on November 23, 2022. The abdo
Mild tenderness in the upper abdomen, without rebound tenderness or muscular tension was revealed on physical exa
Routine blood parameters, biochemical functions, tumor markers, and blood gas findings were normal.
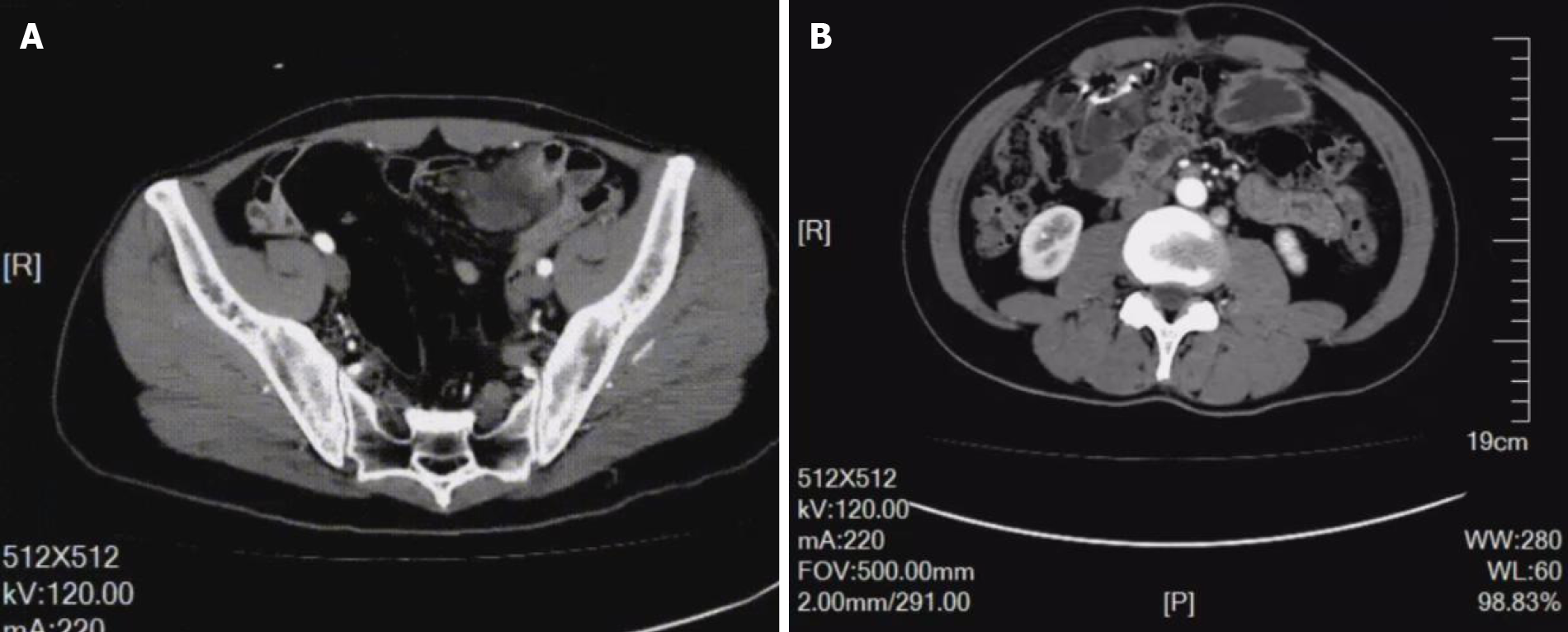
An enhanced CT scan showed significant localized annular enhancement in the left pelvic small bowel wall. The lumen was narrowed, and the outer wall of the small bowel was rough in texture. In addition, the adjacent mesentery was thickened with increased density, and slightly large lymph nodes were faintly visible inside the mesentery. No dilation of the proximal intestine was observed. Three-phase CT values were 52, 63, and 67 HU, respectively (Figure 1A; Video 1).
Pathological examination revealed a jejunal hemolymphangioma, and immunohistochemical staining was positive for both D2-40 and CD32.
Robot-assisted laparoscopic partial small bowel resection and lymph node dissection were performed under general anesthesia. During laparoscopic exploration, no significant ascites was found within the abdominal cavity, while the greater omentum was adhered to the right abdomen. Following release of the adhesion, the small bowel wall, approximately 250 cm away from Treitz ligament and 70 cm away from the ileocecum, was found to be thickened with a hard texture and a diameter of approximately 3 cm. There was no serosal invasion or obvious adhesion to surrounding tissues. Multiple enlarged lymph nodes were found within the small intestinal mesentery. Further exploration showed no sig
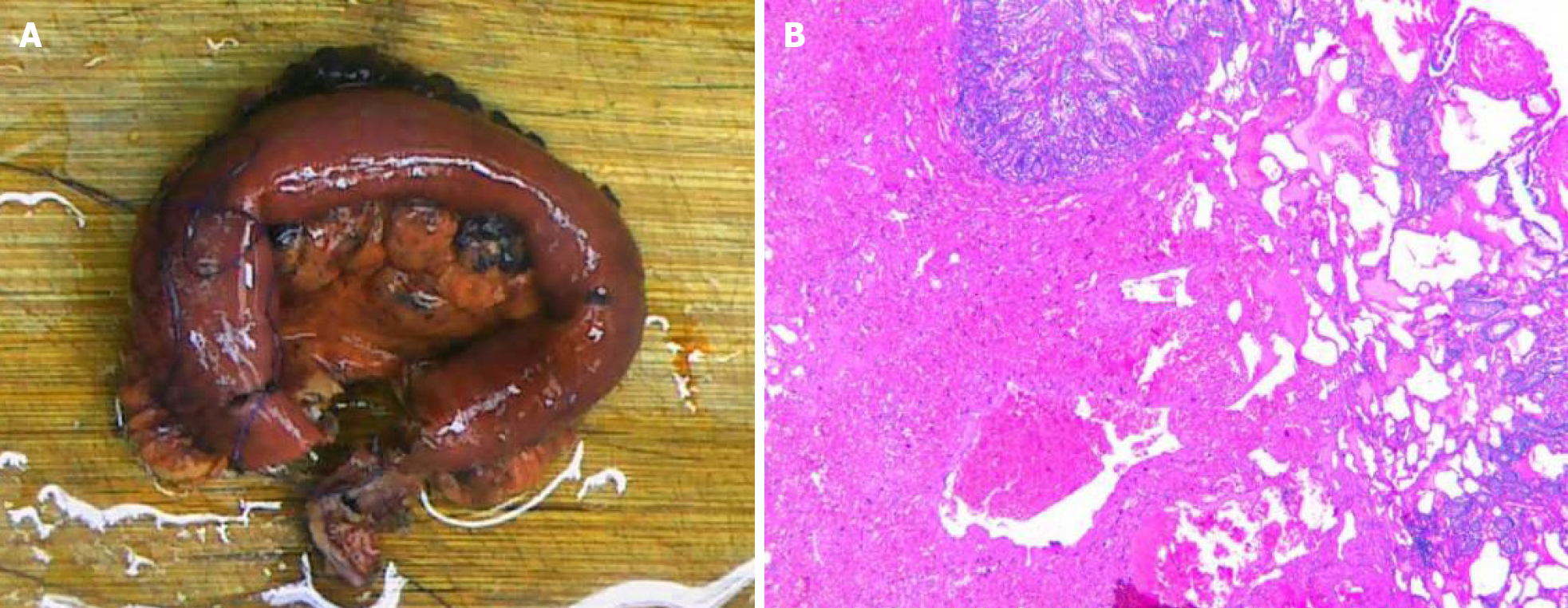
The patient underwent repeat abdominal enhanced CT which showed unobstructed anastomotic healing and no signs of intra-abdominal tumor recurrence 3 mo after surgery (Figure 1B; Video 2). The resected segments of the small intestine and mesentery were sent for pathological examination. Gross pathological evaluation revealed a 15-cm long lesion (perimeter: 4-5 cm) with a rough mucosal bulge (1.5 cm × 1.5 cm) 7 cm away from one cut end. The corresponding small intestinal serosal layer formed a 6 cm × 4 cm × 4 cm mass, which had a grey-red soft cut surface with outflow of dark red liquid. Hematoxylin and eosin staining showed cystic-like dilated blood and lymph vessels of varying sizes. The blood vessels were dilated into blood sinuses filled with red blood cells, while the lymph vessels containing lymphocytes were filled with eosinophilic proteins. These blood and lymph vessels showed a dopant distribution (Figure 2). Immunohistochemistry showed cluster of differentiation 34 (CD34) (focal +), CD31 (+), D2-40 (+), and Ki67 (dispersed +). Pathology suggested partial small intestinal hemolymphangioma invading the full-thickness bowel wall and mesentery. Both cut ends of the small bowel developed submucosal vascular proliferation accompanied by vascular dilation and congestion, and one peri-intestinal lymph node showed reactive hyperplasia. The patient had an excellent postoperative outcome without complications.
Hematolymphangioma is a benign tumor originating from the mesenchymal-embryonic tissues, and is a type of low-flow vascular malformation instead of a true neoplasm[1]. Primary hematolymphangioma is the result of developmental ab
Hematolymphangioma has varying clinical presentations, sizes and locations. The symptoms vary due to complications such as mass enlargement or bleeding, infection, perforation, torsion and rupture. In general, hematolymphangioma is rare in clinical practice, which may be due to the low incidence and lack of clinical presentations. In the current case, abdominal pain was the main symptom, and may have been a result of the space-occupying tumor. Gastrointestinal hematolymphangioma is diagnosed based on CT and endoscopic findings. CT is a very useful radiologic tool for diagnosis[2]. On CT images, hematolymphangioma presents with dilation of veins and lymphatic capillaries although with normal stromal tissue and vasculature. Malformed and dilated venous vessels usually present with th
Robotic surgery has the following advantages over traditional laparoscopic surgery[5]. (1) Higher accuracy: the robotic arm of the surgical system can more accurately replicate the doctor's surgical movements, and can filter out human tre
Generally, en bloc resection can provide the best results with a lower rate of recurrence; however, careful follow-up is required. Moreover, the rate of recurrence varies with the complexity, anatomical location and adequacy of resection. According to the literature, 10%-27% of lesions undergoing en bloc resection recur, whereas the rate could be up to 50%-100% in lesions undergoing partial resection. Compared to surgery, non-surgical treatments including cryotherapy, laser therapy, radiotherapy and localized injection of sclerosing agents are inferior[7].
Here, we report a male patient with a hematolymphangioma in the small intestine. Hematolymphangioma lacks typical clinical symptoms, and specific imaging examinations such as CT and magnetic resonance imaging are useful for con
| 1. | Xiao NJ, Ning SB, Li T, Li BR, Sun T. Small intestinal hemolymphangioma treated with enteroscopic injection sclerotherapy: A case report and review of literature. World J Gastroenterol. 2020;26:1540-1545. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Pan X, Dong Y, Yuan T, Yan Y, Tong D. Two cases of hemolymphangioma in the thoracic spinal canal and spinal epidural space on MRI: The first report in the literature. Medicine (Baltimore). 2017;96:e9524. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Kosmidis I, Vlachou M, Koutroufinis A, Filiopoulos K. Hemolymphangioma of the lower extremities in children: two case reports. J Orthop Surg Res. 2010;5:56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Fan Z, Li Y, Yan K, Wu W, Yin S, Yang W, Xing B, Li X, Zhang X. Application of contrast-enhanced ultrasound in the diagnosis of solid pancreatic lesions--a comparison of conventional ultrasound and contrast-enhanced CT. Eur J Radiol. 2013;82:1385-1390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Ye SP, Zhu WQ, Huang ZX, Liu DN, Wen XQ, Li TY. Role of minimally invasive techniques in gastrointestinal surgery: Current status and future perspectives. World J Gastrointest Surg. 2021;13:941-952. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Lim KT. Current surgical management of duodenal gastrointestinal stromal tumors. World J Gastrointest Surg. 2021;13:1166-1179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Takagi K, Umeda Y, Yoshida R, Fuji T, Yasui K, Yagi T, Fujiwara T. Innovative suture technique for robotic hepaticojejunostomy: double-layer interrupted sutures. Langenbecks Arch Surg. 2023;408:284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Demirli Atici S, Turkey; Kou G, China S-Editor: Qu XL L-Editor: Filipodia P-Editor: Qu XL