Published online Dec 27, 2024. doi: 10.4240/wjgs.v16.i12.3870
Revised: October 17, 2024
Accepted: October 23, 2024
Published online: December 27, 2024
Processing time: 99 Days and 4.2 Hours
Laparoscopic cholecystectomy is considered the gold standard for the treatment of patients with gallstones. However, bile duct injury is one of the most serious complications of this surgery, with an incidence rate of 0.3%-0.7%. Variations in anatomical structures are one of the main reasons for such injuries.
We report a 26-year-old male patient who presented with repeated upper abdominal pain for 1 year. Ultrasound examination and blood tests indicated gallstones accompanied by chronic cholecystitis. The patient underwent laparoscopic cholecystectomy. During the surgery, a communicating bile duct connec
Carefully manage communicating accessory bile ducts in cholecystectomy using cholangiography or meticulous separation, followed by ligation is effective.
Core Tip: This case report highlights the significance of recognizing and managing accessory hepatic duct injuries during laparoscopic cholecystectomy. Utilizing intraoperative cholangiography or indocyanine green fluorescence cholangiography can help identify biliary anomalies, while expert evaluation by a hepatobiliary surgeon is crucial. For confirmed communicating accessory hepatic ducts, total cholecystectomy with duct ligation offers an effective solution to prevent further complications.
- Citation: Zhao PJ, Ma Y, Yang JW. Laparoscopic cholecystectomy with communicating accessory hepatic duct injury and management: A case report. World J Gastrointest Surg 2024; 16(12): 3870-3874
- URL: https://www.wjgnet.com/1948-9366/full/v16/i12/3870.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i12.3870
Laparoscopic cholecystectomy is considered the gold standard for patients with gallstones. Bile duct injury is one of the most severe complications of cholecystectomy, with an incidence rate of 0.3%-0.7%[1,2]. One of the main causes of this injury is the variability in bile duct anatomy. Studies have shown that up to 47% of the population has anatomical variations in the biliary system[3].
The accessory hepatic duct is an anatomical variation of the biliary system, which is easily misidentified during surgery. Goor and Ebert defined communicating accessory hepatic ducts as those that communicate between major bile ducts but do not drain parts of the liver[4]. However, the actual prevalence rate is not clear. Correct identification and management of communicating accessory hepatic ducts during laparoscopic cholecystectomy is important. We share a case of communicating accessory hepatic duct injury and management during laparoscopic cholecystectomy.
We report a 26-year-old male patient who presented with recurrent upper abdominal pain for 1 year.
The patient experienced persistent abdominal distention pain in the upper abdomen a year ago after consuming fatty foods. The pain radiated to the right shoulder and was accompanied by nausea, but there were no symptoms of vomiting, fever, palpitations, shortness of breath, or chest pain. After taking ibuprofen, the symptoms were somewhat relieved. Since then, the abdominal pain has recurred multiple times. One month before admission, the abdominal pain worsened, and an ultrasound examination diagnosed “gallstones”. The patient used traditional Chinese medicine for treatment, but the abdominal pain continued to recur.
The patient denies any history of chronic diseases such as hypertension, heart disease, or diabetes, and reports no history of surgery, trauma, or blood transfusion. There is no known drug allergy history, and the patient denies any history of acute or chronic infectious diseases.
The patient’s place of origin is Dali. The patient does not have smoking or alcohol habits. Both parents are alive and have no history of chronic diseases. There is no family history of hereditary diseases.
At the time of consultation, his vital signs were normal. Physical examination revealed tenderness in the right upper abdomen, with no signs of peritonitis, and a negative Murphy’s sign.
Blood tests were normal, including white blood cells, transaminases, alkaline phosphatase, and bilirubin levels.
Ultrasound examination showed that the size of the gallbladder was normal, but the wall was irregular, with an echogenic mass of approximately 23 mm accompanied by a shadow.
Based on the examination results, the final diagnosis was gallbladder stones with chronic cholecystitis.
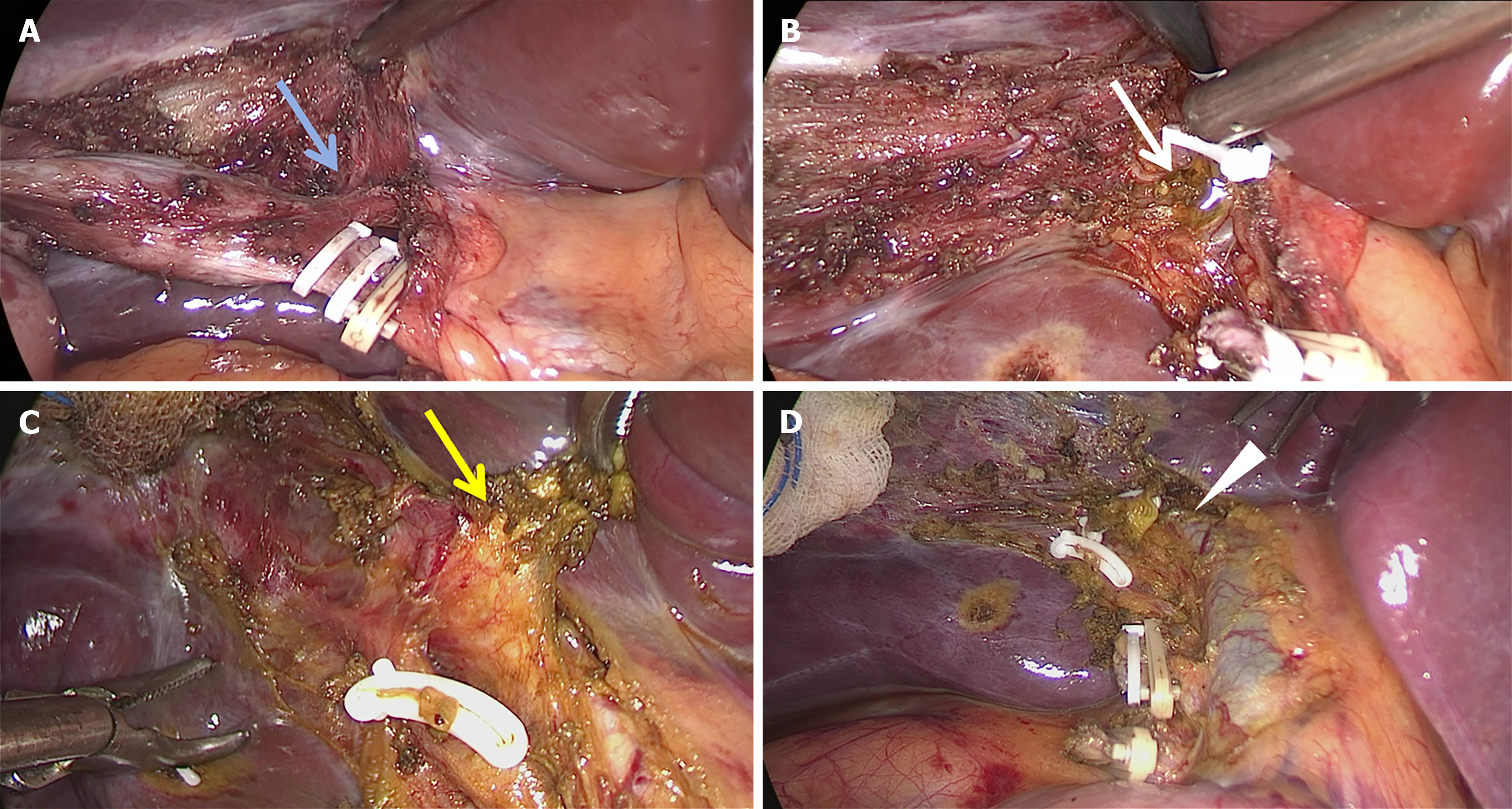
The patient was sent to the operating room. During the laparoscopic surgery, the cystic duct and the anterior branch of the cystic artery were separated. A duct connecting the gallbladder infundibulum and the right hepatic duct was found within the cystohepatic triangle. This duct was ruptured and bile leaked out during its separation. Careful separation during surgery confirmed this as a communicating accessory hepatic duct, and the stump was clamped. Postoperative exploration showed no bleeding or bile leakage from the stumps of the anterior branch of the cystic artery, the cystic duct, the posterior branch of the cystic artery, and the communicating accessory hepatic duct (Figure 1, Video).
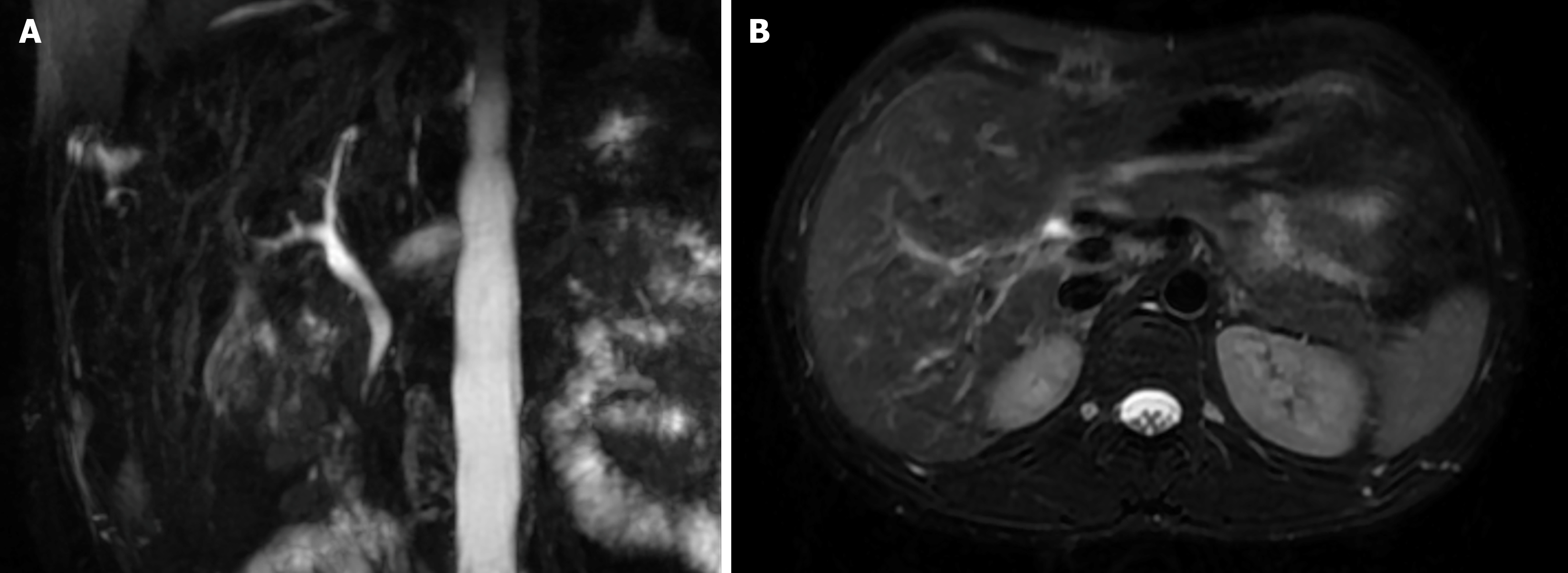
Postoperatively, the patient’s liver function showed no significant changes. He was discharged 3 days later. During the 2 weeks postoperative follow-up, magnetic resonance imaging and magnetic resonance cholangiopancreatography showed no signs of intrahepatic or extrahepatic bile duct stricture, and the patient was in good condition. The pathology report showed chronic cholecystitis with gallstones (Figure 2).
Accessory hepatic ducts are bile duct branches that drain bile from liver lobes, segments, or subsegments and connect directly with extrahepatic bile ducts, cystic ducts, or the gallbladder body. However, there is no consistent definition for them. 94% accessory hepatic ducts drain the right lobe of the liver, and only 6% drain the left lobe[5]. Hisatsugu and their colleagues divided accessory right hepatic ducts based on their convergence with the cystic duct into the following types: (1) Type I, cystic duct converges with the accessory right hepatic duct; (2) Type II, accessory right hepatic duct and cystic duct converge at the same location on the common bile duct; (3) Type III, accessory right hepatic duct drains into the common hepatic duct; (4) Type IV, accessory right hepatic duct drains into the distal common bile duct of the cystic duct; and (5) Type V, accessory right hepatic duct drains into the cystic duct[6].
Intraoperative cholangiography plays an important role in understanding biliary anatomy and can reduce the incidence of bile duct injuries during laparoscopic cholecystectomy[7]. However, the procedure is complex, extends operation time, and involves radiation exposure, so it is not routinely performed in many institutions. In recent years, numerous studies have shown that using fluorescent laparoscopy for indocyanine green fluorescence cholangiography can significantly reduce the risk of bile duct injury[8,9]. Simultaneously, if bile duct injury is detected during surgery, it should ideally be handled by an experienced hepatobiliary surgeon who performs careful separation and exploration to identify the type of injury and anatomical anomalies, avoiding thermal damage from electrocautery[10,11]. In this case, intraoperative exploration and postoperative magnetic resonance cholangiopancreatography showed no segmental intrahepatic bile duct dilation, confirming that the abnormal duct communicated with the right hepatic duct on one end and the gallbladder infundibulum on the other, suggesting it was a communicating accessory hepatic duct.
According to Kurahashi et al’s classification[12], an abnormal duct communicating with the cystic duct is classified as type A, which is considered high risk. Subtotal cholecystectomy can avoid bile duct injury but was not included in this study[12]. Goor and Ebert[13] classified communicating accessory hepatic ducts into four types: (1) F1, connecting the right hepatic duct and the common hepatic duct; (2) F2, connecting the right hepatic duct and the cystic duct; (3) F3, connecting the right hepatic duct and the gallbladder neck; and (4) F4, connecting the right and left hepatic ducts. In cholecystectomy, F2 and F3 types are mainly involved. Therefore, for patients with communicating accessory hepatic ducts found during laparoscopic cholecystectomy, total cholecystectomy combined with ligation of the communicating accessory hepatic duct is a viable option.
Our study indicates that if bile duct injury is found during laparoscopic cholecystectomy, an experienced hepatobiliary surgeon should carefully separate and explore the injury type and anatomical anomalies, and intraoperative cholangiography or indocyanine green fluorescence cholangiography should be performed when necessary. If confirmed as a communicating accessory hepatic duct, total cholecystectomy combined with ligation of the communicating accessory hepatic duct should be considered. In conclusion, we further validated the effectiveness of this research through a surgical video that we produced. This video not only offers a detailed demonstration of the key steps but also enhances the understanding of the communicating accessory hepatic duct ligation.
The authors express their gratitude to the medical, surgical, and radiology teams at the First Affiliated Hospital of Dali University for their expertise in managing this case. They also acknowledge the rehabilitation team for their role in facilitating the patient’s recovery. Special thanks are extended to the patient for consenting to share his case, which contributes to the advancement of medical knowledge.
| 1. | de'Angelis N, Catena F, Memeo R, Coccolini F, Martínez-Pérez A, Romeo OM, De Simone B, Di Saverio S, Brustia R, Rhaiem R, Piardi T, Conticchio M, Marchegiani F, Beghdadi N, Abu-Zidan FM, Alikhanov R, Allard MA, Allievi N, Amaddeo G, Ansaloni L, Andersson R, Andolfi E, Azfar M, Bala M, Benkabbou A, Ben-Ishay O, Bianchi G, Biffl WL, Brunetti F, Carra MC, Casanova D, Celentano V, Ceresoli M, Chiara O, Cimbanassi S, Bini R, Coimbra R, Luigi de'Angelis G, Decembrino F, De Palma A, de Reuver PR, Domingo C, Cotsoglou C, Ferrero A, Fraga GP, Gaiani F, Gheza F, Gurrado A, Harrison E, Henriquez A, Hofmeyr S, Iadarola R, Kashuk JL, Kianmanesh R, Kirkpatrick AW, Kluger Y, Landi F, Langella S, Lapointe R, Le Roy B, Luciani A, Machado F, Maggi U, Maier RV, Mefire AC, Hiramatsu K, Ordoñez C, Patrizi F, Planells M, Peitzman AB, Pekolj J, Perdigao F, Pereira BM, Pessaux P, Pisano M, Puyana JC, Rizoli S, Portigliotti L, Romito R, Sakakushev B, Sanei B, Scatton O, Serradilla-Martin M, Schneck AS, Sissoko ML, Sobhani I, Ten Broek RP, Testini M, Valinas R, Veloudis G, Vitali GC, Weber D, Zorcolo L, Giuliante F, Gavriilidis P, Fuks D, Sommacale D. 2020 WSES guidelines for the detection and management of bile duct injury during cholecystectomy. World J Emerg Surg. 2021;16:30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 139] [Cited by in RCA: 135] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 2. | Pesce A, Palmucci S, La Greca G, Puleo S. Iatrogenic bile duct injury: impact and management challenges. Clin Exp Gastroenterol. 2019;12:121-128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 78] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 3. | Munie S, Nasser H, Go PH, Rosso K, Woodward A. Case report of a duplicated cystic duct: A unique challenge for the laparoscopic surgeon. Int J Surg Case Rep. 2019;56:78-81. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Wang W, Huang H, He K, Wang L, Su S, Zhang Z, Wang P, Guo B, Ren X, Li O. Detection of the communicating accessory bile duct in laparoscopic resection of residual gallbladder by the combination of the indocyanine green fluorescence cholangiography and the intraoperative cholangiography: A case report. Photodiagnosis Photodyn Ther. 2023;42:103587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 5. | Uchiyama K, Tani M, Kawai M, Ueno M, Hama T, Yamaue H. Preoperative evaluation of the extrahepatic bile duct structure for laparoscopic cholecystectomy. Surg Endosc. 2006;20:1119-1123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 6. | Kurata M, Honda G, Okuda Y, Kobayashi S, Sakamoto K, Iwasaki S, Chiba K, Tabata T, Kuruma S, Kamisawa T. Preoperative detection and handling of aberrant right posterior sectoral hepatic duct during laparoscopic cholecystectomy. J Hepatobiliary Pancreat Sci. 2015;22:558-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Brunt LM, Deziel DJ, Telem DA, Strasberg SM, Aggarwal R, Asbun H, Bonjer J, McDonald M, Alseidi A, Ujiki M, Riall TS, Hammill C, Moulton CA, Pucher PH, Parks RW, Ansari MT, Connor S, Dirks RC, Anderson B, Altieri MS, Tsamalaidze L, Stefanidis D; and the Prevention of Bile Duct Injury Consensus Work Group. Safe Cholecystectomy Multi-society Practice Guideline and State of the Art Consensus Conference on Prevention of Bile Duct Injury During Cholecystectomy. Ann Surg. 2020;272:3-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 171] [Article Influence: 28.5] [Reference Citation Analysis (0)] |
| 8. | Hou YK, Liu WK, Gao YB, Tian XD, Yang YM. Enhanced fluorescence cholangiography with indocyanine green: A methodology for reducing the potential hazard of bile duct injury during laparoscopic cholecystectomy. Hepatobiliary Pancreat Dis Int. 2024;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Ankersmit M, van Dam DA, van Rijswijk AS, van den Heuvel B, Tuynman JB, Meijerink WJHJ. Fluorescent Imaging With Indocyanine Green During Laparoscopic Cholecystectomy in Patients at Increased Risk of Bile Duct Injury. Surg Innov. 2017;24:245-252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 10. | Julian D, Martín S, Martín P, Rodrigo SC, Guillermo A, Oscar M, Juan P. Role of laparoscopy in the immediate, intermediate, and long-term management of iatrogenic bile duct injuries during laparoscopic cholecystectomy. Langenbecks Arch Surg. 2022;407:663-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 11. | Zidan MHE, Seif-Eldeen M, Ghazal AA, Refaie M. Post-cholecystectomy bile duct injuries: a retrospective cohort study. BMC Surg. 2024;24:8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 13] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 12. | Kurahashi S, Komatsu S, Matsumura T, Fukami Y, Arikawa T, Saito T, Osawa T, Uchino T, Kato S, Suzuki K, Toda Y, Kaneko K, Sano T. A novel classification of aberrant right hepatic ducts ensures a critical view of safety in laparoscopic cholecystectomy. Surg Endosc. 2020;34:2904-2910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (1)] |
| 13. | Goor DA, Ebert PA. Anomalies of the biliary tree. Report of a repair of an accessory bile duct and review of the literature. Arch Surg. 1972;104:302-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 99] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/