Published online Dec 27, 2024. doi: 10.4240/wjgs.v16.i12.3857
Revised: September 23, 2024
Accepted: October 15, 2024
Published online: December 27, 2024
Processing time: 247 Days and 17.9 Hours
Gastric mucosal heterotopia (GMH) is a rare, typically asymptomatic condition characterized by ectopic gastric mucosa in tissues outside the stomach. However, it can lead to severe complications, including small intestinal perforation. This case report highlights the unique clinical presentation of GMH-induced recurrent small intestinal perforations, which has been rarely documented. These findings emphasize the importance of considering GMH in patients with unexplained recurrent gastrointestinal perforations.
A 13-year-old female presented with acute abdominal pain. Her medical history included four prior surgeries for small intestinal perforations. Enhanced compu
GMH should be considered in cases of recurrent unexplained intestinal perforations.
Core Tip: This case report illuminates the rare but clinically significant phenomenon of recurrent small intestinal perforation caused by gastric mucosal heterotopia. This case was a challenging diagnostic journey that culminated in successful surgical management, demonstrating the critical need for high clinical suspicion and comprehensive diagnostic approaches in patients with unexplained recurrent intestinal perforations. It underscores the importance of considering gastric mucosal heterotopia as a potential etiology, which, although rare, necessitates tailored diagnostic and therapeutic strategies to prevent severe complications and improve patient outcomes, offering valuable insights into enhancing care for similar rare cases.
- Citation: Li ZW, Jiang TF, Yang CK, Xu ZJ, Zhu WB, Li E. Recurrent small intestinal perforation from gastric mucosal heterotopia: A case report. World J Gastrointest Surg 2024; 16(12): 3857-3861
- URL: https://www.wjgnet.com/1948-9366/full/v16/i12/3857.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i12.3857
Gastric mucosal heterotopia (GMH) represents an uncommon pathology characterized by the ectopic presence of gastric mucosa outside the stomach, predominantly in the esophagus but less frequently in the small intestine[1,2]. GMH pathogenesis is poorly understood, but one widely accepted hypothesis is the embryonic displacement of gastric mucosa[3]. Although GMH typically remains asymptomatic and is often an incidental finding during gastrointestinal examinations, it can lead to severe complications, including bleeding, intestinal obstruction, and perforation[4-7]. Incidences of GMH in the small intestine are rare but have been documented as putative causes of small intestinal perforation. Recurrent small intestinal perforation attributed to GMH is exceedingly rare and poses a diagnostic challenge. This case report presents a novel instance of recurrent small intestinal perforation resulting from GMH, aiming to enrich the understanding of this rare condition and its clinical implications.
A 13-year-old female presented to our emergency department on June 9, 2023 with acute abdominal pain which had persisted for 10 hours.
The patient reported severe abdominal pain localized to the central and right abdomen accompanied by mild nausea but no vomiting. She denied any changes in bowel habits, fever, or other associated symptoms.
The patient’s medical history included four previous surgical interventions for small intestinal perforations at various sites between August 2020 and February 2022. She had no documented history of Crohn’s disease, intestinal tuberculosis, Henoch-Schönlein purpura, or vasculitis.
There were no significant findings in the patient’s personal or family medical history, and no reports of hereditary gastrointestinal disorders.
Upon examination, the patient’s vital signs were as follows: Temperature of 36 °C; pulse of 79 beats per minute; respiratory rate of 20 breaths per minute; and blood pressure of 106/55 mmHg. The patient appeared in acute distress, was unable to lie flat, and presented with rapid breathing. The abdomen was flat, but the abdominal muscles were rigid, presenting a board-like abdomen. There was generalized tenderness across the entire abdomen, with marked tenderness and rebound tenderness in the upper abdomen.
The patient’s blood routine examination revealed an elevated white blood cell count [16.6 × 109/L; normal range: (4.1-11.0) × 109/L], indicating a likely infectious or inflammatory response. Neutrophil percentage was significantly increased (92.6%; normal range: 31%-70%), further supporting the presence of acute inflammation.
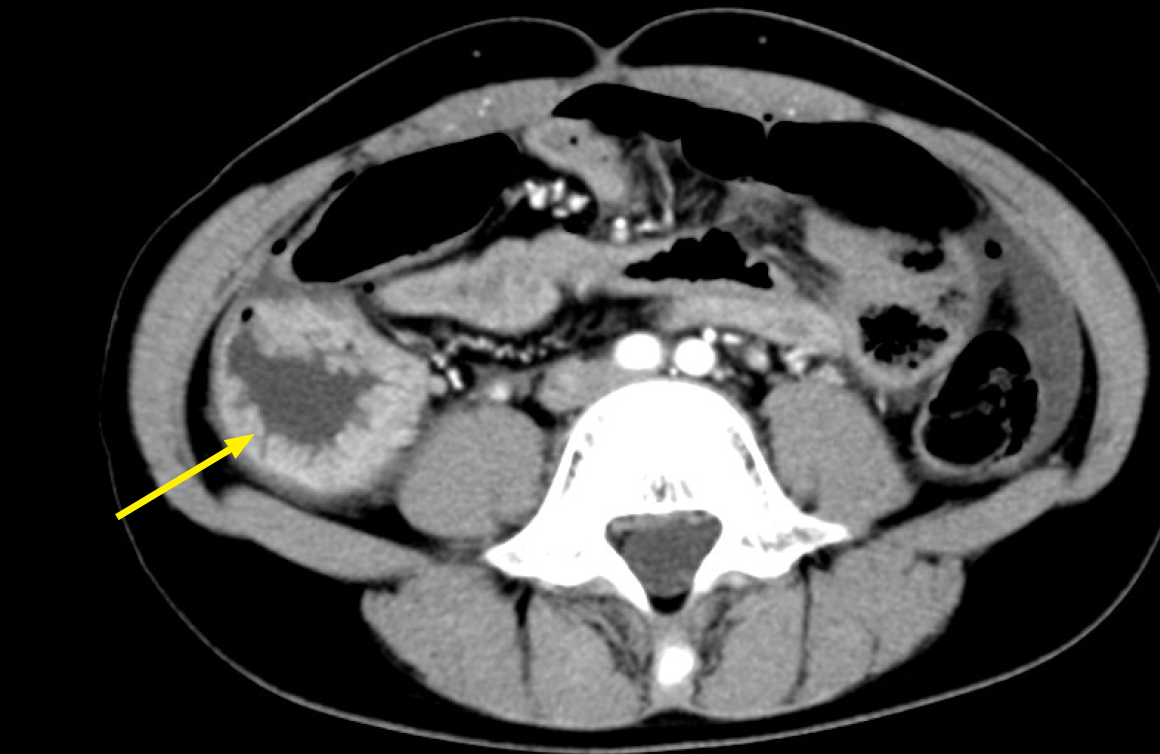
Enhanced abdominal computed tomography was performed upon admission and revealed localized thickening and dilation of the small bowel with evidence of perforation (Figure 1). These findings were consistent with small intestinal perforation, warranting emergency surgical intervention.
Given the urgent nature of the patient’s condition, no formal multidisciplinary expert consultation was conducted. Based on the clinical presentation and diagnostic findings, emergency surgery was performed promptly. Postoperative pathological evaluation confirmed the diagnosis of GMH, which was retrospectively discussed among the surgical and pathology teams.
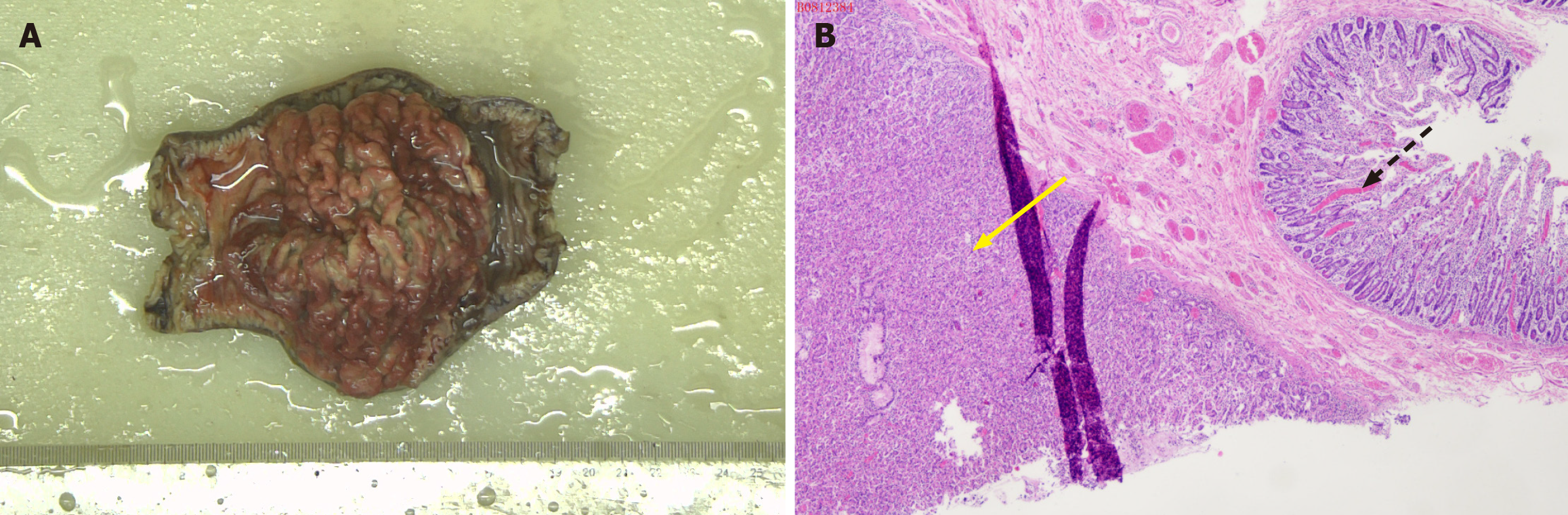
The final diagnosis was recurrent small intestinal perforation caused by GMH. Pathological examination of the resected intestinal tissue confirmed the presence of extensive GMH and localized ulceration and perforation (Figure 2). GMH was identified as the underlying cause of the patient’s recurrent perforations.
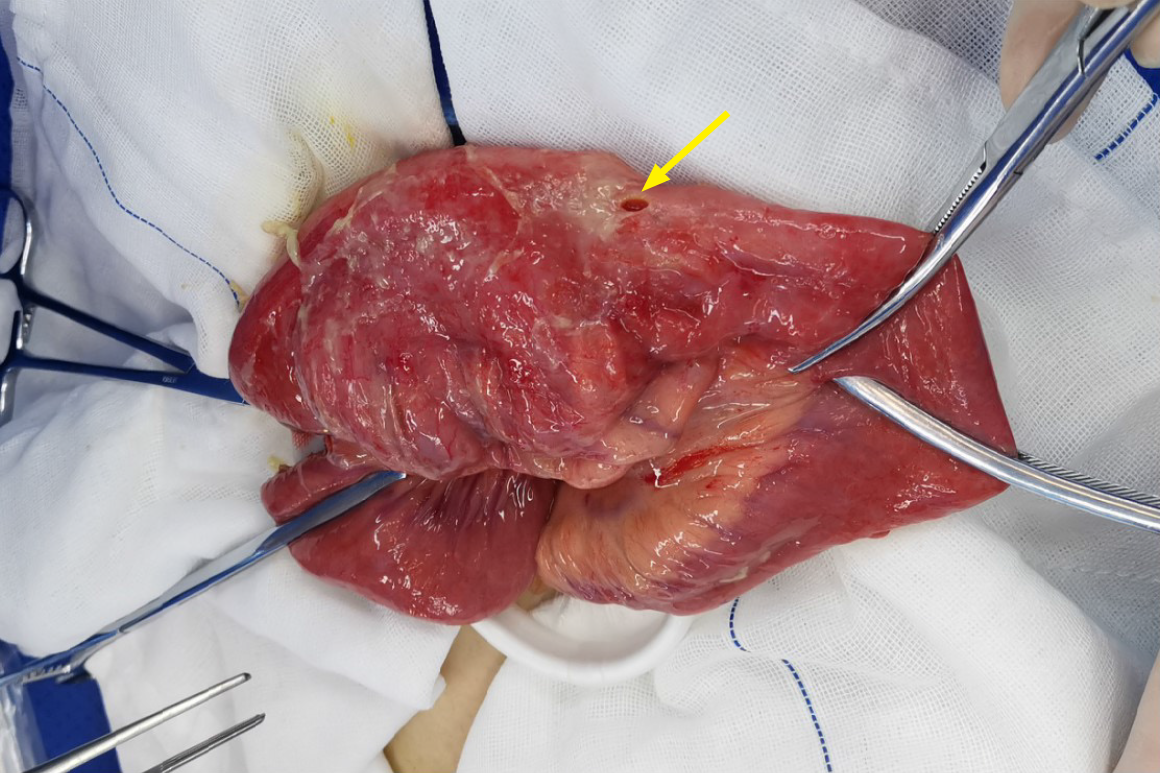
The patient underwent emergency laparoscopic exploration, which revealed significant dilation and a 0.5 cm jejunal perforation approximately 20 cm distal to the ligament of Treitz (Figure 3). A laparotomy was performed, and a 20 cm segment of the affected ileum was resected. The resected ends were then anastomosed using a 4-0 absorbable suture for end-to-end ileal closure. The abdomen was thoroughly irrigated, and the surgical site was inspected for additional perforations or abnormalities. The surgery concluded with drainage placement. Post-operative management included antibiotics and supportive care to prevent infection and promote healing.
Postoperatively, the patient recovered well without any complications. At the 10-month follow-up, the patient remained asymptomatic and no further episodes of perforation were reported, indicating significant improvement in her quality of life.
This exceptionally rare case describes a patient’s experience with four episodes of small intestinal perforation over the course of 18 months, ultimately culminating in a diagnosis of GMH in the small intestine. The rarity of GMH associated with recurrent small intestinal perforation underscores the novelty and clinical significance of this case. This case showcases two notable characteristics, namely the recurrence of perforations within a relatively short timeframe and the occurrence of each perforation at a unique site within the small intestine. These features differentiate this case from the relatively few reports on other GMH-related intestinal perforation cases, highlighting its exceptional nature.
The persistence of small intestinal perforations at multiple locations requires the consideration of GMH as a differential diagnosis. This case demonstrates the potential for GMH to cause recurrent perforations at disparate locations, urging clinicians to consider GMH diagnosis in similar clinical scenarios. Although the link between GMH and intestinal perforation remains speculative, it is plausible that the presence of ectopic gastric mucosa induced localized irritation and an inflammatory response, leading to perforation. This hypothesis is supported by the recurrence of perforations at different sites in this patient, suggesting a systemic predisposition rather than isolated incidents.
Timely and precise application of surgical intervention is critical to manage this type of case. Here, emergency laparoscopic surgery was essential in identifying and addressing the intestinal pathology, highlighting the efficacy of surgical management in resolving perforation-associated issues. This outcome underscores the importance of considering more proactive diagnostic approaches, including endoscopic or laparoscopic examinations with a pathological biopsy, in patients presenting with recurrent small intestinal perforation.
In summary, this case adds to our understanding of GMH as a potential cause of recurrent small intestinal perforation, emphasizing the need for clinical vigilance and comprehensive diagnostic strategies in managing similar cases. It reinforces the pivotal role of surgical intervention in such contexts and advocates for an increased awareness among clinicians regarding the potential for GMH to manifest in recurrent, site-variable intestinal perforations.
This report describes a unique case of recurrent small intestinal perforation caused by GMH, underscoring the critical need for thorough etiological assessment in cases with similar presentation. It reinforces the imperative for precise diagnostic and therapeutic interventions, coupled with diligent follow-up, in managing such rare occurrences. Ultimately, this case enhances our understanding of GMH, contributing to enhanced diagnostic accuracy, informed treatment approaches, and improved patient outcomes in the context of this rare pathology.
The authors would like to thank the medical and nursing staff of the Department of Gastrointestinal Surgery at Meizhou People’s Hospital for their support during the patient’s treatment and recovery. Special thanks to the pathology team for their assistance in diagnosing the case. The authors also express their gratitude to the patient and her family for their cooperation and consent to publish this case report.
| 1. | von Rahden BH, Stein HJ, Becker K, Liebermann-Meffert D, Siewert JR. Heterotopic gastric mucosa of the esophagus: literature-review and proposal of a clinicopathologic classification. Am J Gastroenterol. 2004;99:543-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 110] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 2. | Fang Y, Chen L, Chen DF, Ren WY, Shen CF, Xu Y, Xia YJ, Li JW, Wang P, Zhang AR, Shao SZ, Yu XN, Peng GY, Fang DC. Prevalence, histologic and clinical characteristics of heterotopic gastric mucosa in Chinese patients. World J Gastroenterol. 2014;20:17588-17594. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Feurle GE, Helmstaedter V, Buehring A, Bettendorf U, Eckardt VF. Distinct immunohistochemical findings in columnar epithelium of esophageal inlet patch and of Barrett's esophagus. Dig Dis Sci. 1990;35:86-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Sánchez-Pernaute A, Hernando F, Díez-Valladares L, González O, Pérez Aguirre E, Furió V, Remezal M, Torres A, Balibrea JL. Heterotopic gastric mucosa in the upper esophagus ("inlet patch"): a rare cause of esophageal perforation. Am J Gastroenterol. 1999;94:3047-3050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 40] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Ralbovsky A, Reyna T, Kabeer M, Nael A, Yang C. Not All that Strictures Is IBD: Gastric Heterotopia Leading to Perforation and Small Bowel Obstruction Mimicking IBD. JPGN Rep. 2022;3:e106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 6. | Briggs FL, Moore JP. Heterotopic gastric mucosa of the small bowel with perforated ulcer. Am Surg. 1979;45:413-417. [PubMed] |
| 7. | Isbister WH, Weedon D. Perforated jejunal ulcer and heterotopic gastric mucosa. Br J Surg. 1976;63:954-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/