Published online Nov 27, 2024. doi: 10.4240/wjgs.v16.i11.3578
Revised: August 27, 2024
Accepted: September 9, 2024
Published online: November 27, 2024
Processing time: 274 Days and 1.4 Hours
Asplenia-type heterotaxy syndrome (HS) is rare and refers to visceral malposition and dysmorphism. It is associated with a high infant mortality rate due to cardiac anomalies, and related digestive endoscopic interventions are poorly understood. With the improved long-term prognosis of these individuals after modern cardiac surgery, intra-abdominal anomalies have become increasingly significant.
Herein, we report successful endoscopic retrograde cholangiopancreatography (ERCP) in a 14-year-old male with asplenia-type HS that involved unique imaging findings and technical difficulties. His anatomic anomalies included complex congenital heart disease, midline liver placement, an absent spleen, a left-sided inferior vena cava, and dextroposition of the stomach and pancreas. He suffered from choledocholithiasis with obstructive jaundice, and the stone was successfully extracted with a basket following endoscopic papillary balloon dilation.
Although anatomic anomalies in HS increase the degree of technical difficulty when performing ERCP, they can be safely managed by experienced endosco
Core Tip: Endoscopic retrograde cholangiopancreatography (ERCP) can be challenging in cases of anatomical variations. Owing to its rarity, ERCP in patients with asplenia-type heterotaxy syndrome is poorly understood. Although anatomic anomalies lead to increased technical difficulties and risks when standard endoscopic procedures are performed, a thorough preoperative evaluation and the performance of the procedure by a skilled endoscopist in this case enabled the successful completion of the intended procedure, demonstrating that ERCP can be safely performed in patients with asplenia-type heterotaxy syndrome.
- Citation: Zhang YY, Ruan J, Fu Y. Therapeutic endoscopic retrograde cholangiopancreatography in a patient with asplenia-type heterotaxy syndrome: A case report. World J Gastrointest Surg 2024; 16(11): 3578-3583
- URL: https://www.wjgnet.com/1948-9366/full/v16/i11/3578.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i11.3578
Endoscopic retrograde cholangiopancreatography (ERCP) is widely used for diagnosing and treating pancreaticobiliary disease but can be challenging in cases of anatomical variations. Owing to its rarity, ERCP in patients with asplenia-type heterotaxy syndrome (HS) is poorly understood. It is very important for interventional endoscopists to recognize variations in intra-abdominal viscera. Herein, we report the first case, to our knowledge, of successful ERCP in a patient with asplenia-type HS, which involved unique imaging findings and technical difficulties. We present the following case according to the care reporting checklist.
A 14-year-old male was referred for persistent upper right quadrant abdominal pain, nausea, and jaundice for 4 days.
The symptoms started 4 days before presentation and included persistent upper right quadrant abdominal pain, nausea, and jaundice.
The patient underwent the Glenn procedure and pulmonary arterioplasty for complex congenital heart disease at ages 4 and 5 years, respectively. He took aspirin daily thereafter, with a current dosage of 100 mg/day. Usually, he could take care of himself and attend school but could not participate in sports activities.
The patient denied any remarkable family history.
He appeared emaciated with a dark complexion, jaundiced sclera, and cyanotic lips and nail bed. His resting pulse oxygen saturation was 75%, his blood pressure was 87/51 mmHg, and his pulse rate was 80 beats/minute. Physical examination revealed significant jaundice and right epigastric tenderness but Murphy’s sign was negative.
Laboratory studies revealed a total bilirubin level of 196.5 μmol/L (normal range: 3.4-20.5), a direct bilirubin level of 100.0 μmol/L (normal range: 0-6.8), an aspartate aminotransferase level of 128 U/L (normal range: 8-40), and an alanine aminotransferase level of 137 U/L (normal range: 5-40).
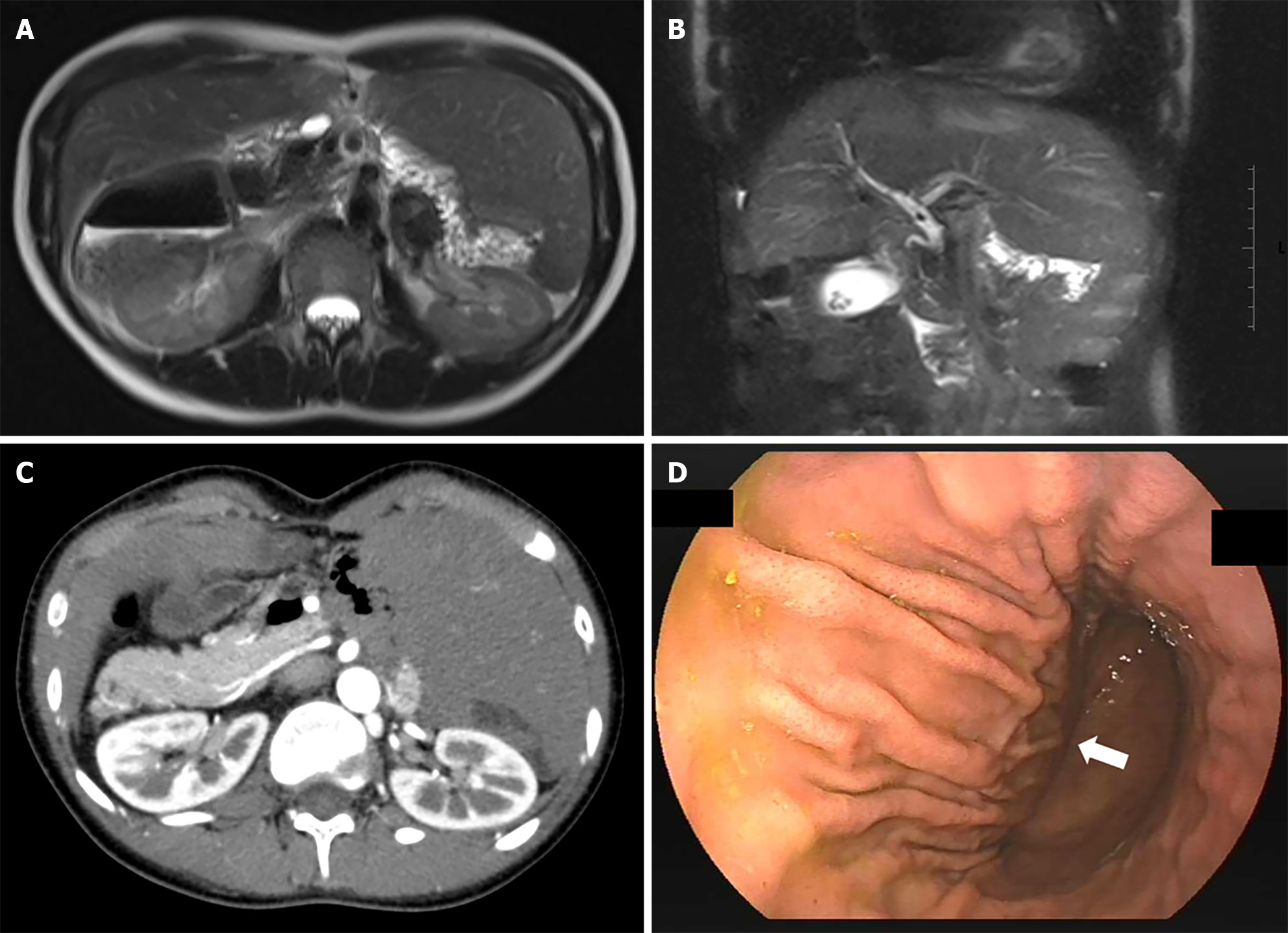
Echocardiography revealed a single ventricle, a functional single atrium, and postoperative changes, with an ejection fraction of 54%. Abdominal computed tomography and magnetic resonance imaging revealed an abnormal arrangement of the abdominal viscera, including dextroposition of the pancreas and stomach, absence of the spleen, left-sided inferior vena cava, and midline liver placement (Figure 1A and B). The absence of the spleen was further confirmed by abdominal ultrasound. Magnetic resonance cholangiopancreatography revealed a 6 mm stone in the common bile duct (CBD), with a slightly dilated upstream biliary tree and the presence of multiple gallstones (Figure 1C).
Combined with a history of persistent upper right quadrant abdominal pain, nausea, and jaundice, along with the physical examination and liver function test results, a diagnosis of choledocholithiasis compounded by obstructive jaundice was made. All anatomic variations, including cardiac anomalies, were consistent with asplenia-type HS. Therefore, the final diagnosis was choledocholithiasis with obstructive jaundice and asplenia-type HS.
ERCP was chosen as the initial treatment modality because of its minimally invasive nature and efficacy, and the lack of a need for general anesthesia. Preprocedure gastroduodenoscopy revealed a distorted gastric anatomy, with inversion of the greater and lesser curvatures (Figure 1D).
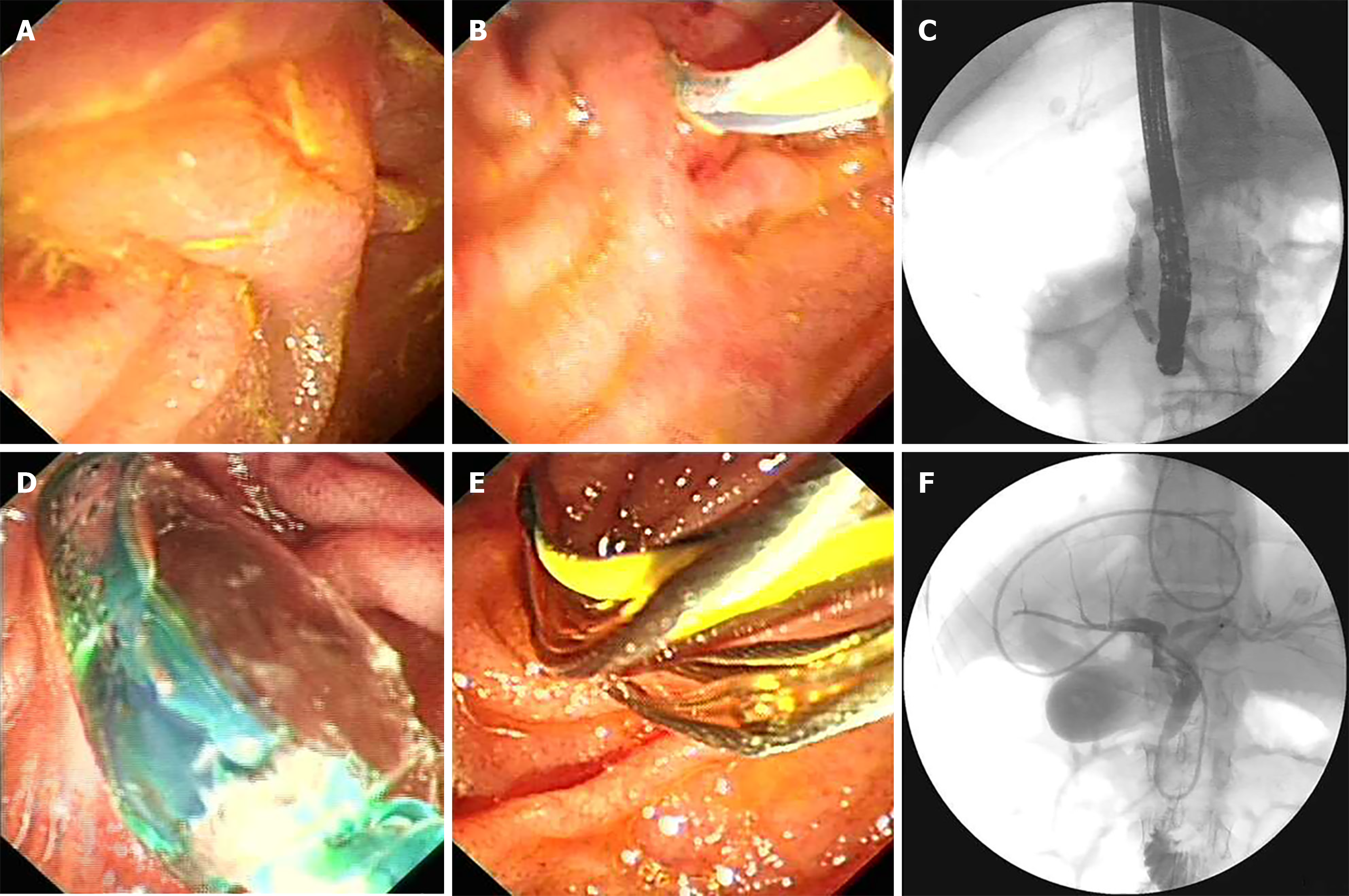
The patient remained fully conscious during the procedure under laryngopharyngeal topical anesthesia. He was in the prone position, and the endoscopist initiated intubation with a side-viewing endoscope on the right side of the patient, as usual. With careful rotation to locate the antrum, the endoscope was advanced into the duodenum. The papilla was oriented at the 11 o’clock position (Figure 2A). However, owing to the altered anatomy, the endoscope was tangential to the papilla and nearly parallel to the CBD, resembling a straight line. This positioning made maneuvering and controlling the endoscope challenging. With gentle handling and careful air volume control, we finally accessed the CBD via an ERCP cannula with a guidewire (Figure 2B). Cholangiography confirmed mild dilation of the CBD, with an impacted stone measuring 6 mm (Figure 2C).
Endoscopic papillary balloon dilatation (EPBD) was performed (Figure 2D), followed by successful stone extraction with a basket (Figure 2E). Postoperative cholangiography through the nanobiliary drainage tube confirmed that there were no residual stones (Figure 2F). Serendipitously, the tube mirrored the coronal shape of the inverted stomach. The procedure duration was 53 minutes, with no desaturation episodes.
The postoperative course was uneventful. The patient recovered well, with improvements in both clinical and biochemical parameters.
ERCP is widely used to diagnose and treat pancreaticobiliary disease but can be challenging in cases of anatomical anomalies.
Situs anomalies can be classified into three categories: situs solitus, situs inversus, and situs ambiguous. Situs solitus refers to a normal position of the thoracic and abdominal viscera. Situs inversus is characterized by the mirrored arrangement of the viscera, either totalis or partialis. Situs ambiguous refers to an abnormal organ arrangement that is not a partial or complete mirror image but rather in varying positions[1]. Situs ambiguous, more precisely currently defined as HS, is divided into two subtypes, namely, asplenia-type HS and polysplenia-type HS, depending on the presence or absence of the spleen and the number of splenules[1,2]. HS is rare, occurring in approximately 1 in 10000 total births[3].
Classic findings in HS include cardiac malpositioning, septal defects, bilateral bilobed or trilobed lungs, midline liver placement, intestinal malrotation, and abnormal spleen development[4]. The specific characteristics of asplenia-type HS were summarized from 11 cases: congenital heart disease (11 cases, mainly involving the common atrioventricular canal), midline liver placement (10 cases), dextroposition of the stomach (7 cases), and left-sided inferior vena cava (9 cases)[1]. Our patient exhibited all these features. Moreover, asplenia-type HS is associated with more severe congenital heart disease and higher morbidity and mortality than polysplenia-type HS is[1,5]. Death occurs in the first year of life in up to 80% of cases, mainly due to severe cardiac anomalies[1,5].
In summary, asplenia-type HS is rare and associated with a high infant mortality rate, and related digestive endoscopic interventions are rarely performed and poorly understood. Few reports of ERCP in HS patients exist, and those that exist all involve cases of polysplenia-type HS without cardiac anomalies[6-8]. We report the first successful performance of ERCP in a patient with asplenia-type HS involving unique endoscopic and imaging findings and technical difficulties.
Despite the risks associated with ERCP, it was pursued as the first treatment modality given his complex clinical presentation. Owing to the complex, variable clinical manifestations in patients with HS, techniques for situs inversus patients, such as 180° endoscope rotation, mirror imaging, and positional adjustment of the patient and/or endoscopist could not be applied indiscriminately[9,10].
The patient was fully conscious and received laryngopharyngeal topical anesthesia throughout the procedure, as the risk of subjecting his fragile body to general anesthesia was too high. Given that the patient had normal placement of the duodenum and biliary tract, we placed him in the prone position, and the endoscopist initiated intubation on his right side in the usual fashion.
With respect to the difficulty of achieving cannulation due to altered anatomy, after failing with the sphincterotome, we accessed the CBD via a wire-led ERCP cannula, which, compared with the sphincterotome, has a slightly softer tip and a subtly different cannulating axis direction. The use of a rotatable sphincterotome to accommodate anatomical anomalies was reported in a patient with situs inversus[11]. When options such as a rotatable sphincterotome are not available, a wire-led cannula may be a worthwhile alternative.
A multicenter, retrospective study indicated that the efficiency and complication rates of EPBD are equivalent to those of endoscopic sphincterotomy (EST) plus balloon dilation for stone removal, but the former is associated with a lower bleeding risk when used to remove small CBD stones (≤ 10 mm)[12]. Anatomical alterations makes controlling and maneuvering the endoscope difficult, increasing the degree of risk associated with EST. Therefore, considering the daily use of aspirin for the postoperative management of complex congenital heart disease and the presence of a small CBD stone (6 mm) in the patient and aiming to reduce the associated risk and protect the papillary sphincter, we chose EPBD instead of EST.
HS with complex congenital heart disease poses challenges. Recent studies have shown satisfactory outcomes with surgical management. With the improved long-term prognosis achieved with modern cardiac surgery, intra-abdominal anomalies increasingly affect the long-term outcomes[13]. It is believed that future discussions will increasingly focus on managing abdominal diseases related to these cases. It is crucial to reveal variations with imaging modalities and to be aware of them before initiating an invasive intervention to prevent complications.
Asplenia-type HS is rare and is associated with a high infant mortality rate, and endoscopic strategies in patients with this condition are poorly understood. Our case demonstrates that CBD stone removal can be safely performed by EPBD, even in a case complicated with cardiac anomalies. Given the complex manifestations and technical difficulties, thorough preoperative evaluations are crucial.
| 1. | Applegate KE, Goske MJ, Pierce G, Murphy D. Situs revisited: imaging of the heterotaxy syndrome. Radiographics. 1999;19:837-852; discussion 853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 181] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 2. | Bartram U, Wirbelauer J, Speer CP. Heterotaxy syndrome -- asplenia and polysplenia as indicators of visceral malposition and complex congenital heart disease. Biol Neonate. 2005;88:278-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 73] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Lin AE, Ticho BS, Houde K, Westgate MN, Holmes LB. Heterotaxy: associated conditions and hospital-based prevalence in newborns. Genet Med. 2000;2:157-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 119] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 4. | Pauvels LSP, Langer FW, Dos Santos D, Haygert CJP. Heterotaxy syndrome. Radiol Bras. 2018;51:344-345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Hashmi A, Abu-Sulaiman R, McCrindle BW, Smallhorn JF, Williams WG, Freedom RM. Management and outcomes of right atrial isomerism: a 26-year experience. J Am Coll Cardiol. 1998;31:1120-1126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 146] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 6. | de la Serna-Higuera C, Perez-Miranda M, Flores-Cruz G, Gil-Simón P, Caro-Patón A. Endoscopic retrograde cholangiopancreatography in situs inversus partialis. Endoscopy. 2010;42 Suppl 2:E98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Meyer J, Rossetti A, Scheffler M, Morel P, Majno P. Ampullectomy for an unexpected ampullary hamartoma in a heterotaxic patient. Int J Surg Case Rep. 2013;4:544-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Byun JR, Jahng JH, Song JC, Yu JS, Lee DK. Supine position endoscopic retrograde cholangiopancreatography in a patient with situs ambiguous with polysplenia. Dig Endosc. 2010;22:322-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Rocha M, Dias AM, Coimbra J. A Challenging Abdominal Pain. Gastroenterology. 2020;158:e11-e13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Naser J, Sarmini MT, Vozzo C, Saleh MA, Chahal P. ERCP and EUS technique in situs inversus totalis: preparing for a left-sided plot twist. VideoGIE. 2022;7:367-370. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 11. | Emmanuel J, Sriram N, Muthukaruppan R. Endoscopic retrograde cholangiopancreatography in a patient with complete situs inversus viscerum: A case report and literature review. DEN Open. 2022;2:e17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 12. | Ye Q, Zhang J, Ou X, Zhou X, Zhu C, Li W, Yao J, Zhang G. Efficacy and safety of three endoscopic techniques for small common bile duct stones (≤ 10 mm): a multicenter, retrospective, cohort study with propensity score matching. Surg Endosc. 2023;37:1863-1869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Kharel S, Koirala DP, Shrestha S, Sedai H, Shrestha BM, Homagain S, Kandel S. Heterotaxy syndrome with complex congenital heart disease, facial palsy, and asplenia: A rare newborn finding. Clin Case Rep. 2021;9:e04573. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/