Published online Nov 27, 2024. doi: 10.4240/wjgs.v16.i11.3559
Revised: August 24, 2024
Accepted: September 13, 2024
Published online: November 27, 2024
Processing time: 90 Days and 6.6 Hours
The effects of electrical stimulation on gastrointestinal function recovery after gynecological abdominal surgery was not clear.
To systematically evaluate the effects of electrical stimulation on gastrointestinal function recovery after gynecological abdominal surgery.
The Cochrane Library, Web of Science, PubMed, ProQuest, and the Chinese bio
Seven controlled trials, involving 520 patients, were included. The results of meta-analysis showed that electrical stimulation could shorten the recovery time of intestinal sound after gynecological abdominal surgery [odds ratio (OR): -5.11, 95%CI: -5.84 to -4.38, P < 0.00001] and improve the time of first anal exhaust (OR:
Electrical stimulation can shorten this reduces the length of time it takes for the patient to recover from bowel sounds and also affects the time to first anal voiding and defecation to some extent, thereby promoting gas
Core Tip: Electrical stimulation can shorten this reduces the length of time it takes for the patient to recover from bowel sounds and also affects the time to first anal voiding and defecation to some extent, thereby promoting gastrointestinal function recovery after gynecological abdominal surgery.
- Citation: Huang XX, Gu HF, Shen PH, Chu BL, Chen Y. Meta-analysis of electrical stimulation promoting recovery of gastrointestinal function after gynecological abdominal surgery. World J Gastrointest Surg 2024; 16(11): 3559-3567
- URL: https://www.wjgnet.com/1948-9366/full/v16/i11/3559.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i11.3559
Abdominal surgery is a common type of surgery used to treat gynecological diseases and is mainly used to treat pelvic organs[1]. After gynecological abdominal surgery, patients are prone to gastrointestinal dysfunction such as abdominal distension, abdominal pain, loss of appetite, and delay of exhaust and defecation time[2], which can increase the intestinal pressure, slow down the healing of surgical anastomoses, and even cause intestinal obstruction[3]. Simultaneously, it can lead to a rise in the patient’s diaphragm, inhibit the chest range of motion, cause dyspnea, and lead to deep venous thrombosis of the lower limbs[4]. All of these conditions negatively affect postoperative rehabilitation. At present, encouraging patients to get out of bed early after surgery, gastrointestinal decompression, and gastric motility drugs are often used in clinical practice to promote recovery of gastrointestinal function, but the effect is not ideal[5]. However, electrical stimulation can stimulate the local nerves and muscle tissue in the abdomen of patients, accelerate the recovery of postoperative gastrointestinal function[6], and effectively reduce postoperative complications. Therefore, this study searched domestic and foreign studies on the application of electrical stimulation to promote gastrointestinal function recovery in patients after gynecological abdominal surgery and analyzed its application effect to provide evidence-based medical data for gastrointestinal function recovery after clinical gynecological abdominal surgery.
Using the library's network resources to consult related studies, we attempted to understand the progress of domestic and foreign research. Sources: Cochrane Library, Web of Science, PubMed, ProQuest, and Chinese Biomedical Literature Databases Wanfang, Weipu, and CNKI. We used a combination of subject and free words to manually searched for relevant references, if necessary. Randomized controlled trials on the use of electrical stimulation to promote recovery of gastrointestinal function after gynecological abdominal surgery were collected from January 2010 to May 2024. Simultaneously, the references of the included studies were traced back to supplement the acquisition of relevant studies. The search was carried out by combining subject terms and keywords. The English search terms were: "Electrical sti
Inclusion criteria: (1) Type: Relevant trials published in China and abroad on the promotion of gastrointestinal function recovery after gynaecological abdominal surgery through electrical stimulation, in Chinese or English only; (2) Subjects: Patients who underwent gynecological abdominal surgery and showed abdominal distension, nausea, reduced bowel sounds, and stopped anal exhaust and defecation, which met the diagnostic criteria for postoperative gastrointestinal dysfunction in gastroenterology[7]. The two groups were consistent in terms of age, sex, disease course, and educational level; (3) Intervention measures: The control group received routine treatment after surgery (gastrointestinal decom
Exclusion criteria: (1) The content of the article was incomplete or cannot be extracted; (2) The literature types were review, meeting minutes, experience summary; (3) Experiments with animals as research objects; (4) Non-randomized controlled clinical research articles; (5) Non-Chinese and English literature; or (6) The literature did not set up a suitable control group or lacked the necessary outcome data.
Studies that met the research purpose and exclusion criteria were screened, the full text was read further after careful reading of the title, abstract and removal of studies that disagreed with this analysis, while studies with poor design or poor quality content were removed. Indicators such as authors of experiments, specific time of publication and sample size were extracted through Microsoft Excel. The final report had to be screened independently by 2 systematically trained researchers, verified by a third party, if necessary.
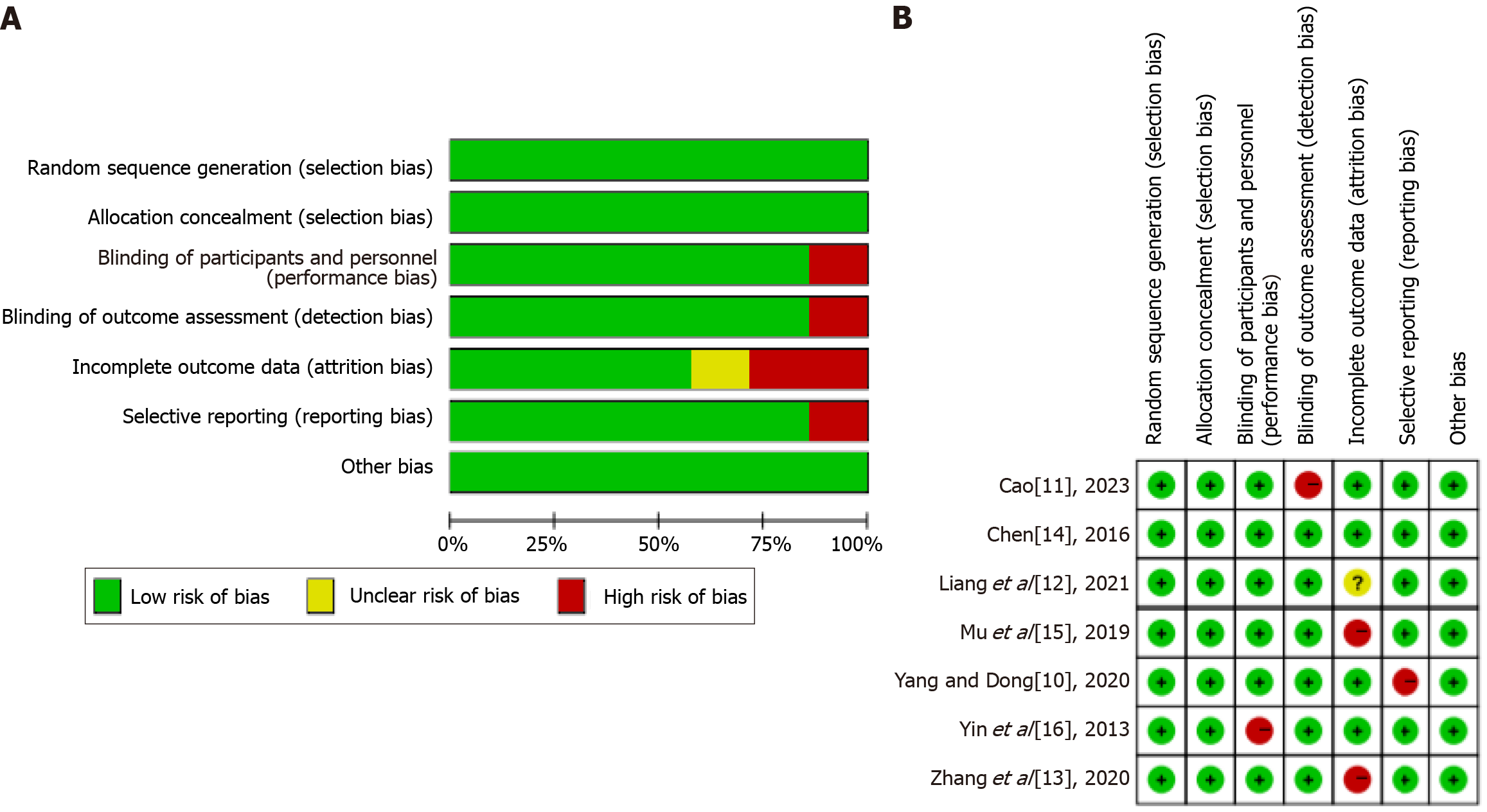
Two researchers independently reviewed the included literature based on the Cochrane Bias Risk Assessment Tool 5.1[8,9]. The specific bias trends in the included literature were assessed and detailed as high, and unclear, covering items such as: (1) Random allocation of; (2) Distribution scheme hiding; (3) Blind method for the subjects and the implementers of the treatment plan; (4) Blind method to measure the findings of the study; (5) Completeness of outcome data; (6) Purposeful reporting of final results; and (7) Biased provenance regarding other. If the low risk was fully satisfied, it was deemed "Level A,” if partially satisfied, it was deemed "Level B,” and if not satisfied, it was deemed "level C.” All items that were "high risk bias" were eliminated.
Statistical analysis was performed using RevMan 5.3, and I2 was used to evaluate heterogeneity. When I2 was lower than 50% and P higher than 0.1 indicate too low or no heterogeneity, so meta-analysis was performed by fixed-effects model. However, when I2 ≥ 50% and P ≤ 0.1, the heterogeneity was high. In this case, meta-analyses were performed using a random-effects model, and bias was assessed using funnel plots.
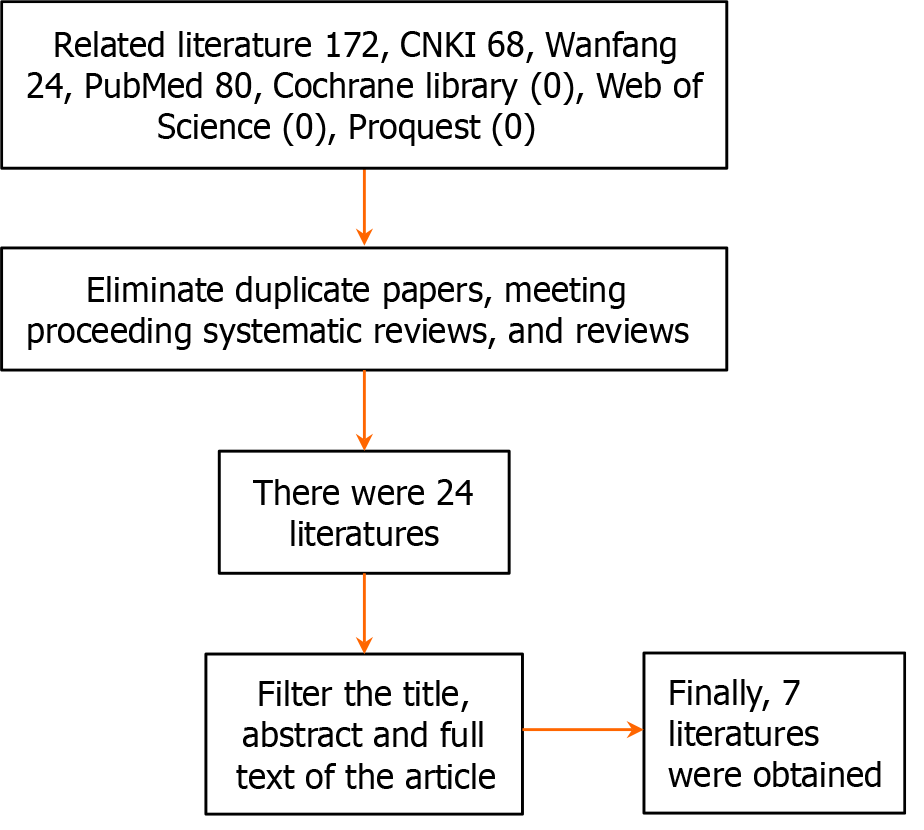
According to the above keywords, a total of 172 studies were obtained by searching various databases; 24 were obtained after all duplicated literature, meeting minutes, after removing the reviews and commentaries, and after the titles, abstracts and full text of the articles, the final seven articles were obtained. The search process is illustrated in Figure 1.
Basic features of included studies: Seven studies published between 2013 and 2023 were included, and the case sources were all distributed in China. There were 520 patients with bronchiectasis, Control group (260), experimental group (260), where the minimum and maximum sample sizes were 40 and 120 respectively. Intervention measures: Of these, seven studies exist used electrical stimulation interventions, whereas the control group used routine nursing interventions. The data of all the study subjects are listed in Table 1[10-16].
| Ref. | Time of publication (year) | Sample size (control group/experimental group) | Packet mode | Intervention method | Outcome index | |
| Control group | Experimental group | |||||
| Yang and Dong[10] | 2020 | 25/25 | Randomized controlled trial | Routine nursing intervention | Electrical stimulation intervention | (2) |
| Cao[11] | 2023 | 60/60 | Randomized controlled trial | Routine nursing intervention | Routine nursing + electrical stimulation intervention | (1) (2) (3) |
| Liang et al[12] | 2021 | 40/40 | Non-randomized controlled trial | Routine nursing intervention | Electrical stimulation intervention | (1) (2) (3) |
| Zhang et al[13] | 2020 | 30/30 | Randomized controlled trial | Routine nursing intervention | Routine nursing + electrical stimulation intervention | (2) (3) |
| Chen[14] | 2016 | 20/20 | Randomized controlled trial | Routine nursing intervention | Routine nursing + electrical stimulation intervention | (1) (2) |
| Mu et al[15] | 2019 | 55/55 | Randomized controlled trial | Routine nursing intervention | Routine nursing + electrical stimulation intervention | (1) (2) (3) |
| Yin et al[16] | 2013 | 30/30 | Randomized controlled trial | Routine nursing intervention | Routine nursing + electrical stimulation intervention | (2) (3) |
Incorporating the results of research bias risk assessments: Random allocation was present in all included papers, of which six were randomised controls and one was a non-randomised control. There were no studies describing hidden allocation and blinded selectivity and other biased provenance. The results of the first anal exhaust time were mentioned in 7 studies, those of the first anal defecation time in 5, and those of bowel sound recovery time in 4. To assess the quality of the Cochrane Risk of Bias Assessment Tool (Figure 2).
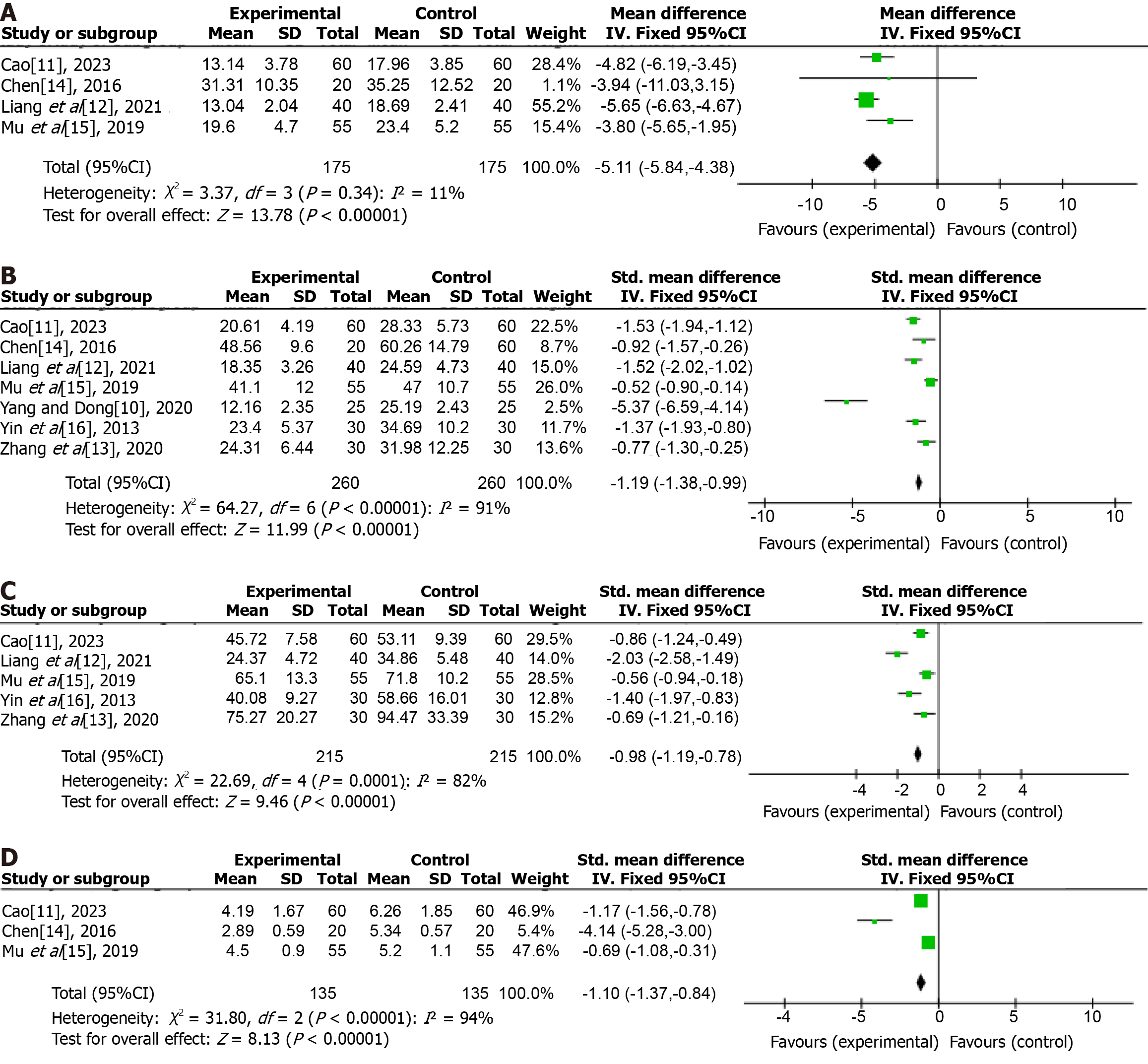
Bowel sound recovery time after electrical stimulation: Four studies reported the first intestinal sound recovery time after electrical stimulation. Heterogeneity between the 2 groups was (P = 0.34, I2 = 11%), with no heterogeneity. Meta-analysis showed that in terms of bowel sound recovery, the experimental group's recovery time was significantly better than that of the control group, and the difference was meaningful [odds ratio (OR): -5.11, 95%CI: -5.84 to -4.38, P < 0.00001; Figure 3A).
Time of first anal exhaust after electrical stimulation: Seven studies reported the time of the first anal exhaust after electrical stimulation. The heterogeneity between the experimental group and the control group showed that P < 0.00001, I2 = 91%, and there was heterogeneity. Meta-analysis showed that after electrical stimulation, the patients in the experimental group had their first anal defecation earlier compared to the control group, and the difference was significant (OR: -1.19, 95%CI: -1.38 to -0.99, P < 0.00001; Figure 3B).
Five studies reported the time of the first anal bowel movement after electrical stimulation. Heterogeneity between the experimental and control groups was P = 0.00001 and I2 = 82%. Meta-analysis showed that the experimental group was earlier than the control group in terms of first anal defecation after electrical stimulation. The difference was significant (OR: -0.98, 95%CI: -1.19 to -0.78, P < 0.00001; Figure 3C).
Three studies reported the length of hospital stay after electrical stimulation, heterogeneity between the 2 groups was P < 0.00001 (I2 = 94%). Meta-analysis showed that in terms of length of stay, the experimental group was significantly shorter than the control group, with significant differences (OR: -1.10, 95%CI: -1.37 to -0.84, P < 0.00001; Figure 3D).
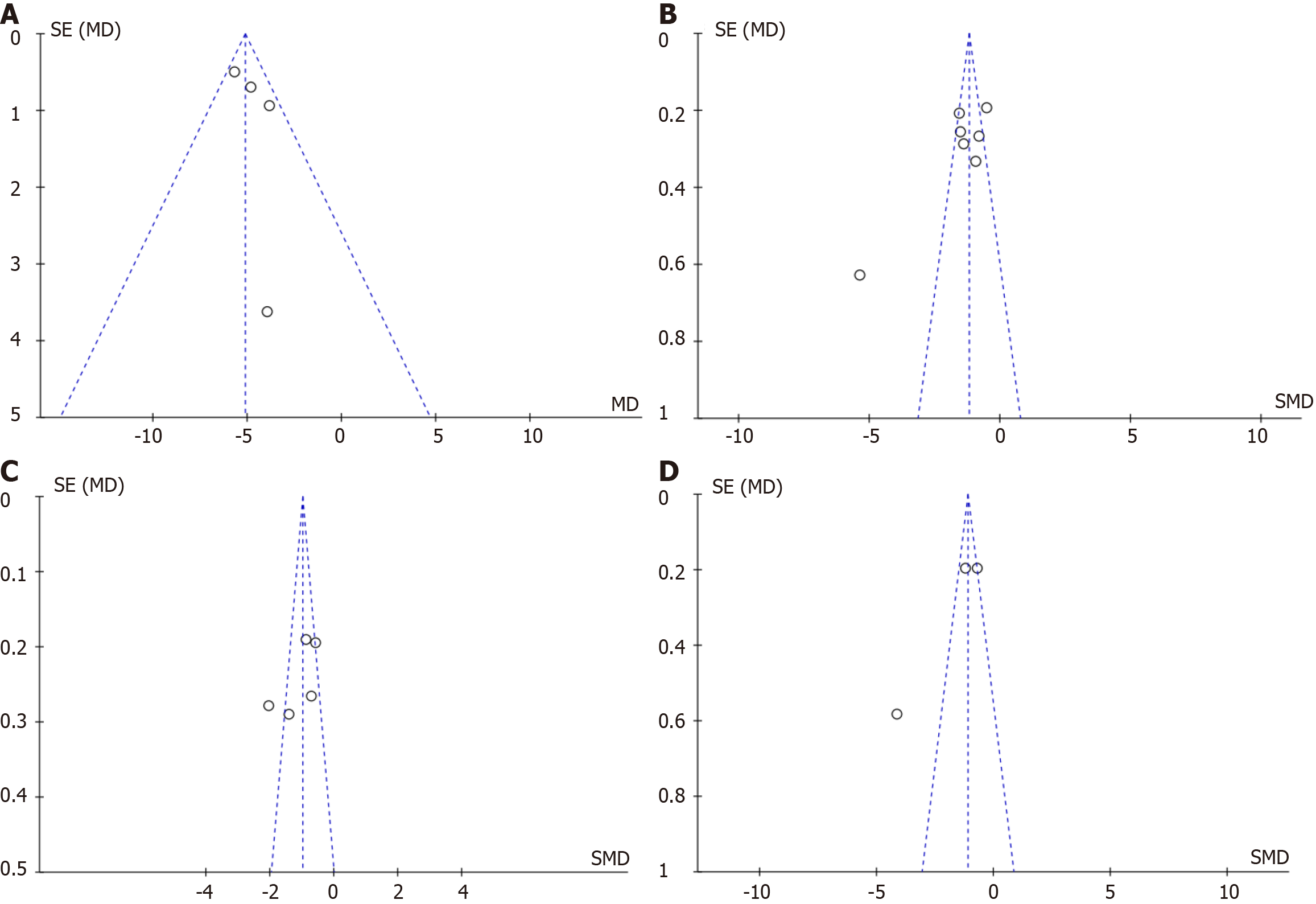
The funnel plot of each study indicated the scatter is uniformly symmetric and inverted funnel; so, no bias occurred (Figure 4).
Abdominal surgery is a common gynecological procedure. Postoperatively, patients experience abdominal pain, distension, nausea and vomiting, and gastrointestinal dysfunction such as poor exhaust and defecation. If not properly handled in time, complications such as adhesion, tearing and intestinal obstruction may occur, aggravating patients' condition and prolonging their postoperative rehabilitation cycle[17]. Currently, gastrointestinal decompression and gastric motility drugs are commonly used to promote the recovery of gastrointestinal function in patients; however, their overall effect is slow, delaying the rehabilitation process of patients. Relevant studies have found that electrical sti
However, electrical stimulation can significantly improve gastric motility and stimulate the local nerve and muscle tissue of the abdomen of patients; using continuous and stable current[20] can regulate the gastrointestinal electrical rhythm, improve the level of gastrointestinal endocrine hormones, accelerate the recovery of postoperative gastroin
Seven studies There were 260 people in the control group and 260 in the experimental group. The recovery time of intestinal sounds after electrical stimulation, time of first anal exhaust, time of first anal bowel movement, and time of postoperative hospitalization the experimental group was superior as compared to the control group. The difference was significant (P < 0.05).
In this study, the control group received routine care such as early getting out of bed, gastric motility drugs, and gastrointestinal decompression. Getting out of bed early can induce intestinal reflex in patients by changing body position, accelerating systemic blood circulation, improving local gastrointestinal blood supply, and promoting intestinal group peristalsis, thus shortening the recovery time of intestinal sounds after gynecological abdominal surgery, but the overall effect is slow[22]. However, kinetotropic drugs can enhance the contractile force of the gastrointestinal smooth muscle, coordinate the gastrointestinal motility law, promote gastrointestinal emptying and transport, and promote the recovery of gastrointestinal function, but they are prone to intestinal torsion, anastomotic rupture, stump fistula, and other serious complications, which are not conducive to the condition of patients[23]. Enema and other gastrointestinal decompression measures can increase pain in patients and are not easily accepted. In this study, we found that electrical stimulation can significantly shortened the recovery time of intestinal sounds after gynecological abdominal surgery. This may be because electrical stimulation can improve the autonomic nervous function of innervating visceral organs, reduce the excitability of sympathetic nerves, increase the tension of parasympathetic nerves, promote the release of acety
In the process of abdominal surgery, external stimulation of the organs can cause reflex gastrointestinal smooth muscle spasm, which can lead to postoperative gastrointestinal dysfunction such as abdominal distension, abdominal pain, anal exhaust obstruction, and eventually intestinal paralysis, which seriously affects the appetite and psychological state of patients and is not conducive to later rehabilitation and nursing. At present, in clinical practice, the recovery of gas
Gastrointestinal disorders such as abdominal pain, distension, and poor defecation often occur after gynecological abdominal surgery and are prone to complications such as adhesion, tearing, and intestinal obstruction, which can prolong the postoperative recovery time of patients and are not conducive to postoperative rehabilitation. Therefore, the recovery of gastrointestinal function is a key component of rehabilitation after gynecological abdominal surgery. In this study, patients in the experimental group had their first anal defecation earlier than the control group after receiving electrical stimulation, which suggests that electrical stimulation can improve the time to anal defecation after gynaecological abdominal surgery, which is similar to the conclusion of Li et al[29]. This may be because electrical stimulation can stimulate local smooth muscle or skeletal muscle, act on Cajal interstitial cells, intestinal pacemaker cells, and autonomic nerves of the intestinal wall, enables the stimulation of muscle movement and the simulation of voluntary movement, thus effectively improving the function of some muscles in terms of activity and further promoting blood supply, enhancing colon peristalsis, and accelerating the time of anal bowel movement[30].
The postoperative hospitalization of gynecological abdominal surgery patients is mainly for observation, treatment, and rehabilitation. During hospitalization, doctors can closely observe changes in the patient's condition, deal with possible complications in a timely manner, ensure the safety of the patient, and formulate a personalized rehabilitation plan according to the patient's recovery situation to help the patient recover as soon as possible. In this study, the hospital stay of patients in the experimental group after electrical stimulation intervention was found to be shorter than that of the control group, indicating that electrical stimulation can improve hospital stay after gynecological abdominal surgery, which is similar to the conclusion by Lin et al[31]. The reasons for this may be: As a noninvasive treatment, electrical stimulation can promote the recovery of gastrointestinal function in patients, enabling them to resume normal diet and activities earlier, reduce the use of drugs, and reduce the burden on the body, thereby avoiding complications, improving the comfort and acceptance of patients, accelerating the overall rehabilitation process of patients, and ultimately shortening the length of postoperative hospitalization[32].
(1) Some studies did not mention explicit random methods and hidden methods, which may have caused a selectivity bias; (2) Due to the differences in disease and disease duration between the subjects in this study, it makes the final results of the meta-analysis will receive statistical and clinical heterogeneity; (3) Of the included studies, most were of low quality, and there is a high possibility of potential bias, which may affect the accuracy of the research results; and (4) The specific details of routine nursing operations, determination of outcome indicators, use of electrical stimulation, and course of treatment were inconsistent among the included patients, and there was some clinical heterogeneity, which led to the possibility of bias in the results of the meta-analysis. These limitations also suggest not only is it important to improve the quality of the trial, but also to expand the sample size to further confirm application value of electrical stimulation after gynecological abdominal surgery. Therefore, the validity of the study results can be further strengthened in subsequent studies to improve the overall quality of the trial by: (1) Use randomized controlled trials to expand the sample size of the study and strictly formulate the electrical stimulation operation method to obtain more accurate result data; (2) Establish standardized protocols for electrical stimulation interventions after gynecological surgery to enhance comparability between studies and thus reduce methodological variability; (3) Define demographic methods and indicator evaluation methods, and provide researchers with strict training. At the same time, standardized first-level literature is used to evaluate scale indicators, so as to reduce the impact of statisticians' subjective consciousness on research results; (4) In the process of result sorting, 2-3 result reviewers should be arranged to check the statistical results and eliminate the data results that are obviously low or high to ensure the universality of the results; and (5) Long-term follow-up of patients should be conducted to clarify the reported results of patients' length of stay, postoperative complications and postoperative quality of life, so as to better understand the clinical benefits of electrical stimulation.
The study revealed that electrical stimulation in the form of electrical stimulation can not only significantly shorten the recovery time of midgut sounds in patients during gynaecological abdominal surgery, but also reduce their time of defecation and hospital stay, which is conducive to promoting the recovery of patients, and deserves to be widely used in clinical practice. However, in this study, due to a variety of factors, therefore, further controlled trials based on the principles of multicentre, randomisation and double-blindness were conducted to test the results.
| 1. | Svensson-Raskh A, Schandl AR, Ståhle A, Nygren-Bonnier M, Fagevik Olsén M. Mobilization Started Within 2 Hours After Abdominal Surgery Improves Peripheral and Arterial Oxygenation: A Single-Center Randomized Controlled Trial. Phys Ther. 2021;101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 2. | Chen FQ, Xu WZ, Gao HY, Wu LJ, Zhang H, Cheng L, Mei JQ. Clinical effect of Changweishu on gastrointestinal dysfunction in patients with sepsis. J Int Med Res. 2020;48:300060520919579. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Zia Z, Riaz H, Imtiaz I. Effect of early physical therapy interventions on post-operative ileus following abdominal hysterectomy. J Pak Med Assoc. 2023;73:650-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 4. | Li Y, Sutedjo J, Chen YC, Gu JP. Efficacy of modified pressure cuff for thrombolytic treatment on lower extremity deep venous thrombosis. Medicine (Baltimore). 2021;100:e25664. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 5. | Wu Y, Cai Z, Liu L, Wang J, Li Y, Kang Y, An N. Impact of intravenous dexmedetomidine on gastrointestinal function recovery after laparoscopic hysteromyomectomy: a randomized clinical trial. Sci Rep. 2022;12:14640. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 6. | Catteau M, Passerieux E, Blervaque L, Gouzi F, Ayoub B, Hayot M, Pomiès P. Response to Electrostimulation Is Impaired in Muscle Cells from Patients with Chronic Obstructive Pulmonary Disease. Cells. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Hjuler KF, Dige A, Agnholt J, Laurberg TB, Loft AG, Møller LF, Christensen R, Iversen L. Effectiveness of interdisciplinary combined dermatology-gastroenterology-rheumatology clinical care compared to usual care in patients with immune-mediated inflammatory diseases: a parallel group, non-blinded, pragmatic randomised trial. BMJ Open. 2021;11:e041871. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 8. | Chen LP, Xu ZQ, Hou HJ, Zhao XH, Wu YJ, Wang DH, Xue JJ. [Transcutaneous electrical acupoint stimulation in promoting gastrointestinal function recovery after laparoscopic colorectal cancer surgery: a meta-analysis]. Linchuang Mazuixue Zazhi. 2023;39:952-958. [DOI] [Full Text] |
| 9. | Ding SH, Huang WH, Duan RR, Lu XT, Zhang J, Qin XY, Xue JJ. [Meta-analysis on influence of transcutaneous electrical acupoint stimulation on recovery of gastrointestinal function in parturients after cesarean section]. Guoji Yiyao Weisheng Daobao. 2022;28:3014-3019. [DOI] [Full Text] |
| 10. | Yang L, Dong MF. [Clinical effect of electric stimulation at Zusanli point in promoting anal exhaust in gynecological laparoscopic patients]. Shiyong Fuke Neifenmi Dianzi Zazhi. 2020;7:30+45. [DOI] [Full Text] |
| 11. | Cao H. [Effect of percutaneous acupoint electrical stimulation combined with diet nursing on the recovery of gastrointestinal function in parturients after cesarean section]. Jilin Yixue. 2023;44:1676-1679. [DOI] [Full Text] |
| 12. | Liang JH, Cai XS, Zhang HZ, Duan ZZ, Zhang WY. [Effect of acupuncture based on midnight-noon cycle of qi low frequency electrical stimulation therapy combined with traditional chinese medicine hot package on gastrointestinal function and pain after gynecological laparoscopy]. Huli Shijian Yu Yanjiu. 2021;18:25-28. [DOI] [Full Text] |
| 13. | Zhang WX, Zhang H, Jiang YP, Shi RX. [Application of percutaneous acupoint electrical stimulation therapy in rapid rehabilitation nursing after gynecological laparoscopic surgery]. Mingyi. 2020;230-231. |
| 14. | Chen L. [Effect of nursing intervention combined with pelvic floor electrical muscle stimulation on intestinal peristalsis recovery after abdominal operation]. Shijie Zuixin Yixue Xinxi Wenzhai. 2016;16:74 + 76. |
| 15. | Mu L, Gao H, Zhao ML, Ren HF, Ma HS. [Effect of transcutaneous electrical acupoint stimulation on recovery of gastrointestinal function after cesarean section]. Zhongguo Zhen Jiu. 2019;39:259-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 16. | Yin XQ, Zhou YC, Zhou H, Yang H, Wang YQ, Zhang H. [Effect of transcutaneous electrical stimulation of Zusanli (ST 36) and Liangqiu (ST 34) combined with general anesthesia on pain and gastrointestinal symptoms in patients undergoing gynecological laparoscopic operation]. Zhen Ci Yan Jiu. 2013;38:431-434. [PubMed] |
| 17. | Reintam Blaser A, Padar M, Mändul M, Elke G, Engel C, Fischer K, Giabicani M, Gold T, Hess B, Hiesmayr M, Jakob SM, Loudet CI, Meesters DM, Mongkolpun W, Paugam-Burtz C, Poeze M, Preiser JC, Renberg M, Rooijackers O, Tamme K, Wernerman J, Starkopf J. Development of the Gastrointestinal Dysfunction Score (GIDS) for critically ill patients - A prospective multicenter observational study (iSOFA study). Clin Nutr. 2021;40:4932-4940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 78] [Article Influence: 15.6] [Reference Citation Analysis (1)] |
| 18. | Miao WJ, Qi WH, Liu H, Song XL, Li Y, Cao Y. [Effect of transcutaneous electrical acupoint stimulation on labor analgesia]. Zhongguo Zhen Jiu. 2020;40:615-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 19. | Huang S, Tian W, Zheng D, Zhou J. Electrical Acupoint Stimulation with Low-Frequency Pulse in the Treatment of Urinary Incontinence after Prostatectomy. Arch Esp Urol. 2023;76:460-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 20. | Larauche M, Wang Y, Wang PM, Dubrovsky G, Lo YK, Hsiang EL, Dunn JCY, Taché Y, Liu W, Million M. The effect of colonic tissue electrical stimulation and celiac branch of the abdominal vagus nerve neuromodulation on colonic motility in anesthetized pigs. Neurogastroenterol Motil. 2020;32:e13925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Ban L, Pu Y, Huang H, You B, Chen W, Wang Y. Acupuncture Enhances Gastrointestinal Motility and Improves Autonomic Nervous Function in Patients with Septic Gastrointestinal Dysfunction. Comput Math Methods Med. 2022;2022:1653290. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 22. | Muwel S, Suryavanshi S, Damde HK, Mishra A, Yadav SK, Sharma D. Effect of chewing gum in reducing postoperative ileus after gastroduodenal perforation peritonitis surgery: A prospective randomised controlled trial. Trop Doct. 2024;54:237-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 23. | Lu Y, Fang PP, Yu YQ, Cheng XQ, Feng XM, Wong GTC, Maze M, Liu XS; POGF Study Collaborators. Effect of Intraoperative Dexmedetomidine on Recovery of Gastrointestinal Function After Abdominal Surgery in Older Adults: A Randomized Clinical Trial. JAMA Netw Open. 2021;4:e2128886. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 47] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 24. | Doren N, Chung HK, Grueschow M, Quednow BB, Hayward-Könnecke H, Jetter A, Tobler PN. Acetylcholine and noradrenaline enhance foraging optimality in humans. Proc Natl Acad Sci U S A. 2023;120:e2305596120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 25. | Elkan Kiyat Z, Kahyaoglu Sut H. The Effect of Xylitol Gum Chewing After Cesarean on Bowel Functions: A Randomized Controlled Study. J Perianesth Nurs. 2022;37:913-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 26. | Zhou AR. [Effect of low frequency electrical stimulation on gastrointestinal function recovery after cesarean section]. Shijie Zuixin Yixue Xinxi Wenzhai. 2019;19:382, 384. [DOI] [Full Text] |
| 27. | Tan Y, Ouyang W, Tang Y, Fang N, Fang C, Quan C. Effect of remimazolam tosilate on early cognitive function in elderly patients undergoing upper gastrointestinal endoscopy. J Gastroenterol Hepatol. 2022;37:576-583. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 67] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 28. | Yin C, Fang Y, Yao D, Zhang X. Influencing Mechanism of Cupping Moxibustion on Gastrointestinal Function and Immune Function in Patients with Functional Diarrhea. Cell Mol Biol (Noisy-le-grand). 2022;68:98-104. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 29. | Li H, Wen Q, Hu HQ, He Y, Pan H, Li N. [Transcutaneous electrical acupoint stimulation combined with electroacupuncture for rapid recovery after abdominal surgery: a randomized controlled trial]. Zhongguo Zhen Jiu. 2023;43:135-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 30. | Wang JX, Duan AH, Lu D, Zhang YD, Wu X, Wu J, Zhao X, Feng Y, Sun RY, Li Y. [Effectiveness of bionic electric stimulation on intestinal function recovery after enterodialysis during gynecological surgery]. Zhongguo Yikan. 2021;56:53-56. [DOI] [Full Text] |
| 31. | Lin HY, Liang C, Lin N. [Effect of acupoint combined with low-frequency pulse electrical stimulation on abdominal distension care after gynecological laparoscopic surgery]. Baojian Wenhui. 2020;27:217-218. [DOI] [Full Text] |
| 32. | Bai YF, Gao C, Li WJ, Du Y, An LX. Transcutaneous electrical acupuncture stimulation (TEAS) for gastrointestinal dysfunction in adults undergoing abdominal surgery: study protocol for a prospective randomized controlled trial. Trials. 2020;21:617. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/