Published online Nov 27, 2024. doi: 10.4240/wjgs.v16.i11.3511
Revised: September 26, 2024
Accepted: October 11, 2024
Published online: November 27, 2024
Processing time: 65 Days and 5.9 Hours
There remain controversies regarding the surgical treatment of extrahepatic bile duct stones (EHBDSs) in clinical practice.
To explore the curative effect of laparoscopic cholecystectomy (LC) plus common bile duct exploration (CBDE) for the surgical treatment of EHBDSs and to analyze the risk factors that affect postoperative stone recurrence.
Eighty-two patients with EHBDSs admitted between March 2017 and March 2023 were selected. Among them, patients treated with open choledocholithotomy plus LC or open cholecystectomy (OC) were set as the control group (n = 40), and those treated with LC plus CBDE served as the observation group (n = 42). The surgical outcomes of the two groups were compared, the surgical complications and Gas
The two groups were comparable in the stone residual rate (P > 0.05). The ope
LC plus CBDE for patients with EHBDSs can reduce stone residuals, intraoperative bleeding, complications, and postoperative recurrence.
Core Tip: This research project included 82 patients with extrahepatic bile duct stones (EHBDSs) for a comparative analysis of the clinical advantages of laparoscopic cholecystectomy (LC) plus common bile duct exploration (CBDE) vs open choledocholithotomy plus LC or open cholecystectomy for EHBDSs and an exploration of the risk factors for postoperative stone recurrence. It was found that for patients with EHBDSs, treatment with LC plus CBDE can reduce stone residue and intraoperative bleeding, as well as lower complication and postoperative recurrence rates. Our findings can shed new light on the optimization of treatment for patients with EHBDSs.
- Citation: Liao JH, Li JS, Wang TL, Liu WS. Laparoscopic cholecystectomy plus common bile duct exploration for extrahepatic bile duct stones and postoperative recurrence-associated risk factors. World J Gastrointest Surg 2024; 16(11): 3511-3519
- URL: https://www.wjgnet.com/1948-9366/full/v16/i11/3511.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i11.3511
Cholelithiasis, including gallstones and bile duct stones (BDSs), is a commonly occurring disease that frequently requires hepatobiliary surgery[1] and affects approximately 10%-15% of the adult population[2]. With the improved living stan
BDSs can be classified into primary and secondary types. The former is directly formed within the extrahepatic bile duct, which may be related to bacterial infections or abnormal bilirubin metabolism[7], while the latter is mostly caused by the displacement of gallbladder stones or intrahepatic BDSs to the extrahepatic bile duct[8]. Although the mortality rate of BDSs is not high, its incidence cannot be overlooked[9]. A previous study collected statistics on 262 patients with BDSs and found that the postoperative recurrence rate was 19.48%[10].
Conventional treatment approaches, such as open cholecystectomy (OC) plus common bile duct exploration (CBDE), have definite therapeutic efficacy; however, they present with various issues such, as numerous T-tube-related compli
There is some controversy about using this technology for the treatment of extrahepatic BDSs (EHBDSs)[14,15]. This study aims to explore the clinical effect of LC plus CBDE in treating EHBDSs.
This was a retrospective study, and the research subjects were 82 patients with EHBDSs who were admitted to Shaoyang Central Hospital between March 2017 and March 2023. Among them, the control group consisted of 40 patients who were treated with open choledocholithotomy plus LC or OC, of which there were 18 males and 22 females. In addition, the observation group comprised 42 patients who were treated with LC plus CBDE, of which there were 17 males and 25 females.
Inclusion criteria: All patients were diagnosed with EHBDSs based on their clinical symptoms in combination with laboratory and imaging examination results, aged ≥ 18 years, and had complete medical records.
Exclusion criteria: Patients with intrahepatic BDSs, bile duct tumors, or bile duct malformations, those intolerant to the surgical method or allergic to the drugs used, as well as those with abnormal coagulation mechanisms, were excluded.
The control group was treated with the conventional open choledocholithotomy plus LC or OC. In some cases, the abdominal cavity was accessed via a 10-15 cm incision in the right abdomen. After locating the gallbladder, separation and resection were performed according to the conventional procedure. The common bile duct, cystic duct, and common hepatic duct were identified, and their positions were confirmed via syringe puncture. The peritoneal tissue on the anterior wall of the common bile duct was dissected, and a longitudinal incision of approximately 1 cm was made on the anterior wall of the common bile duct. An electronic choledochoscope was inserted for exploration, and the stones were removed using a stone extractor. In other cases, the gallbladder was routinely removed laparoscopically after the pneu
In the observation group, LC plus CBDE was performed. Routine disinfection and draping were performed before the operation. Then, a small 2-3 cm incision was made below the umbilicus, and a CO2 pneumoperitoneum environment was established via puncture. Subsequently, laparoscopic instruments were introduced into the abdominal cavity for explo
After the procedure, bile drainage was regularly monitored, and the timing of the T-tube removal was determined based on the nature of the drainage fluid.
Both surgical techniques employed standardized surgical practices and the surgical skills or experience of the surgeons performing the operations on patients in both groups were comparable.
(1) Statistics and comparison of baseline data (gender, age, stone diameter, number of stones, disease course, and sphincter of Oddi function with sphincter of Oddi dysfunction meeting the Rome IV criteria[16]) of the two groups was performed; (2) The surgical outcomes of the two groups were compared, including stone residuals, operation time, and intraoperative bleeding; (3) The surgical complications of the two groups were statistically analyzed, including bile leakage, abdominal pain, biliary tract infection, and diarrhea; (4) The patient’s quality-of-life levels in both groups before and six months after surgery were assessed using the Gastrointestinal Quality of Life Index (GIQLI)[17]. The total score of this index is 144, and the score is directly proportional to the patient’s quality-of-life level; (5) The recurrence of the two groups one year after the surgery was statistically recorded. All patients were followed up for 12 months after the end of treatment, with outpatient reexamination performed once every three months. The recurrence of stones was examined by magnetic resonance imaging, computed tomography, and B-ultrasound, and the recurrence rate was recorded; and (6) Univariate and multivariate analyses were performed to detect the independent factors of postoperative recurrence.
The evaluators who collected and statistically analyzed the above data were unaware of the experimental purpose and information related to this study. Moreover, the measurement methods for the aforementioned observation indicators were standardized and uniform throughout the study, and the collection, management, and analysis of data adhered to the same protocol.
In this study, the statistical analysis software SPSS 20.0 (SPSS Inc., Chicago, IL, United States) was used to conduct statistical analyses on the collected data. To determine whether the differences were statistically significant (threshold: P < 0.05), the count data were tested using the chi-square test and expressed as χ2; the measurement data (mean ± SD) were confirmed using the Shapiro-Wilk test to determine the normal distribution, and a two-tailed independent sample t-test was utilized for comparisons between the two groups. A binary logistic regression test was adopted for the multivariate analysis of postoperative recurrence. In addition, the sample size of this study was estimated by using the sample size calculation formula for binomial proportions. This study met the minimum sample size requirement for each group (approximately 21 cases per group).
The comparison of the patient’s baseline data, presented in Table 1, showed no statistical inter-group differences in sex, age, stone diameter, number of stones, disease course, and sphincter of Oddi function (P > 0.05) to suggest comparability.
| Control group (n = 40) | Observation group (n = 42) | χ2 | P value | |
| Sex | ||||
| Male | 18 | 17 | ||
| Female | 22 | 25 | 0.171 | 0.679 |
| Age | ||||
| ≤ 65 years old | 12 | 16 | ||
| > 65 years old | 28 | 26 | 0.597 | 0.440 |
| Stone diameter | ||||
| ≤ 10 mm | 19 | 24 | ||
| > 10 mm | 21 | 18 | 0.764 | 0.382 |
| Number of stones | ||||
| Single | 30 | 28 | ||
| Multiple | 10 | 14 | 0.687 | 0.407 |
| Disease course | ||||
| ≤ 2 years | 25 | 21 | ||
| > 2 years | 15 | 21 | 1.300 | 0.254 |
| Sphincter of Oddi function | ||||
| Normal | 28 | 32 | ||
| Abnormal | 12 | 10 | 0.400 | 0.527 |
The inter-group comparison of surgical outcomes (Table 2) demonstrated a comparable stone residual rate (P > 0.05) but shorter operation time (P < 0.05) and less intraoperative bleeding (P < 0.05) in the observation group compared to the control group.
| Stone residual | Operation time (min) | Intraoperative bleeding (mL) | |
| Control group (n = 40) | 7 | 171.25 ± 48.51 | 52.05 ± 72.34 |
| Observation group (n = 42) | 2 | 144.24 ± 47.89 | 20.60 ± 16.94 |
| t/χ2 | 3.402 | 2.537 | 2.741 |
| P value | 0.065 | 0.013 | 0.008 |
By comparing the occurrence of postoperative complications, it was found that both groups experienced bile leakage, abdominal pain, biliary tract infection, diarrhea, and gastrointestinal bleeding after surgery. However, the total com
| Bile leakage | Abdominal pain | Biliary tract infection | Diarrhea | Gastrointestinal bleeding | Total | |
| Control group (n = 40) | 2 | 5 | 3 | 3 | 1 | 14 |
| Observation group (n = 42) | 0 | 2 | 1 | 1 | 0 | 4 |
| χ2 | 7.761 | |||||
| P value | 0.005 |
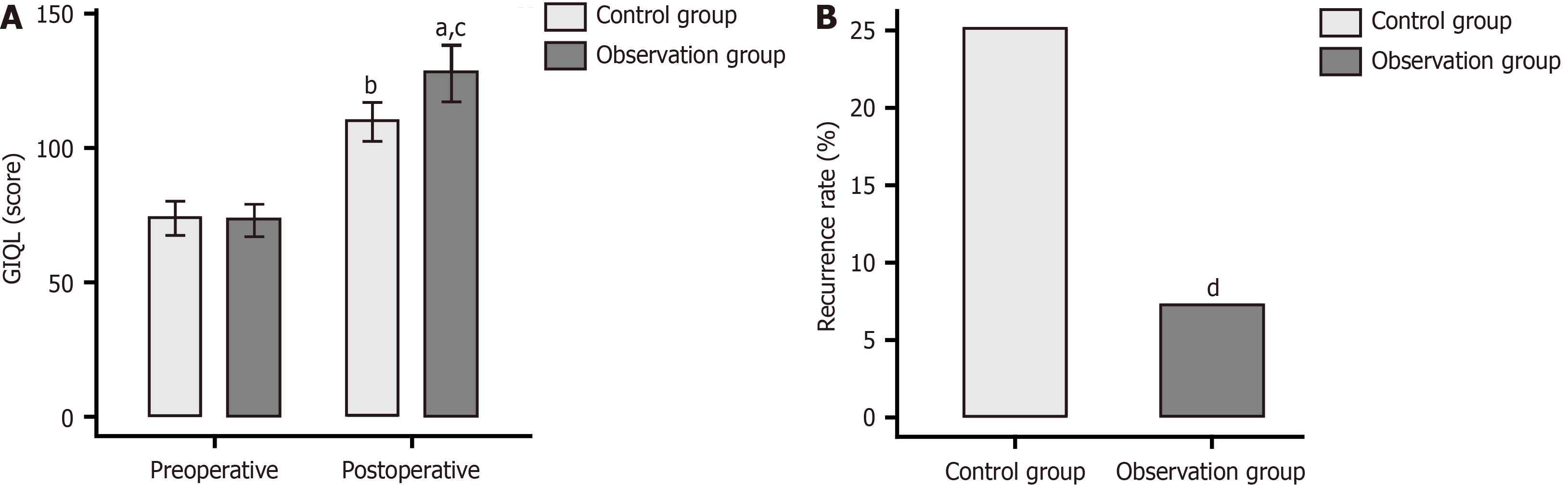
The impact of surgical techniques on the overall health of patients was analyzed using the GIQLI (Figure 1A). The data showed no significant inter-group difference in GIQL scores before the operation (P > 0.05). A marked rise in the GIQL score was observed postoperatively in both groups, with higher scores in the observation group compared to the control group (P < 0.05).
The recurrence rates of the two groups one year after the surgery were compared. There were 3 cases of recurrence in the observation group, compared to 10 cases in the control group. The recurrence rate in the observation group was statistically lower than that in the control group (P = 0.027), as shown in Figure 1B.
We divided the patients into recurrence and non-recurrence groups according to stone recurrence. Through univariate analysis, it was found that the sphincter of Oddi function and treatment scheme were statistically different between the recurrence and non-recurrence groups (P < 0.05), which suggests that these factors were potential influencing factors for recurrence one year after surgery (Table 4).
| Recurrence group (n = 13) | Non-recurrence group (n = 69) | χ2 | P value | |
| Sex | ||||
| Male | 6 | 29 | ||
| Female | 7 | 40 | 0.076 | 0.783 |
| Age | ||||
| ≤ 65 years old | 3 | 36 | ||
| > 65 years old | 10 | 33 | 3.713 | 0.054 |
| Stone diameter | ||||
| ≤ 10 mm | 6 | 39 | ||
| > 10 mm | 7 | 30 | 0.475 | 0.491 |
| Number of stones | ||||
| Single | 6 | 36 | ||
| Multiple | 7 | 33 | 0.159 | 0.690 |
| Disease course | ||||
| ≤ 2 years | 11 | 46 | ||
| > 2 years | 2 | 23 | 1.663 | 0.197 |
| Sphincter of Oddi function | ||||
| Normal | 5 | 53 | ||
| Abnormal | 8 | 16 | 7.771 | 0.005 |
| Treatment scheme | ||||
| Open choledocholithotomy plus laparoscopic or open cholecystectomy | 10 | 30 | ||
| Laparoscopic cholecystectomy plus common bile duct exploration | 3 | 39 | 4.897 | 0.027 |
Values were assigned to the sphincter of Oddi function and treatment regimen that showed differences in the univariate analysis (Table 5), and a multivariate logistics regression analysis was performed. It was found that the sphincter of Oddi dysfunction [odds ratio (OR) = 5.712, P = 0.007] and the treatment regimen of open choledocholithotomy plus LC or OC (OR = 6.771, P = 0.008) were independent risk factors for stone recurrence in patients one year after the operation (Table 6).
| Variable | Assignment |
| Sphincter of Oddi function | Normal = 0, abnormal = 1 |
| Treatment scheme | Open choledocholithotomy plus laparoscopic or open cholecystectomy = 1, laparoscopic cholecystectomy plus common bile duct exploration = 0 |
| Estimate | Std Error | P value | OR | Lower 95%CI | Upper 95%CI | |
| Sphincter of Oddi function | 1.743 | 0.643 | 0.007 | 5.712 | 1.620 | 20.143 |
| Treatment scheme | 1.913 | 0.726 | 0.008 | 6.771 | 1.631 | 28.102 |
In recent years, the incidence of cholecystitis and gallstones has been increasing annually, which has become an in
The comparison of surgical outcomes revealed that despite an equivalent stone residual rate, the operation time and intraoperative bleeding were significantly lower in patients undergoing LC plus CBDE compared with those undergoing open choledocholithotomy plus LC or OC. Thus reflecting the superiority of LC plus CBDE in terms of safety, precision, and efficiency. The possible reason for these improvements could be that laparoscopic surgery, as a minimally invasive technique, accesses the abdominal cavity via small incisions, thus minimizing damage to the surrounding tissues and reducing intraoperative bleeding[22]. In addition, laparoscopy offers an enlarged surgical field of vision and a direct view of the interior of the biliary tract, thereby facilitating more accurate stone localization and stone removal operations and reducing the likelihood of stone residuals[23].
Both groups of patients presented with complications, such as abdominal pain, biliary tract infection, and diarrhea. The overall complication rate in patients treated with open choledocholithotomy plus LC or OC was significantly higher than those treated with LC plus CBDE. Both surgical approaches may result in bile leakage, but LC may increase the risk of bile leakage because of the limited operating space and high technical difficulty. Biliary tract infection is a common complication of biliary tract surgeries. Open surgeries have a relatively higher risk of infection because of the prolonged operation time and extensive trauma. Therefore, laparoscopic surgeries offer enhanced safety. The study by Tracy et al[24] mentioned that prolonged surgery may increase the incidence of biliary complications associated with cholecystectomy. Moreover, the GIQLI score of the observation group after the operation was significantly higher compared with the preoperative level and that of the control group, indicating that LC plus CBDE is more conducive to improving the patient’s quality of life. This may be because the observation group had relatively better surgical outcomes and a sig
Further analysis revealed that the recurrence rate of open choledocholithotomy plus LC or OC was significantly higher than that of LC plus CBDE. This may be because laparoscopic surgery allows doctors to identify and handle the biliary structures more clearly, which may contribute to reducing the risks of stone residuals and recurrence. Finally, through binary logistic multivariate analysis of the influencing factors for one-year recurrence after surgery, we discovered that the sphincter of Oddi dysfunction and treatment scheme of open choledocholithotomy plus LC or OC were independent risk factors. The sphincter of Oddi governs the process of bile flowing from the liver into the small intestine[25]. Sphincter of Oddi dysfunction may result in cholestasis and bacterial infection in the biliary tract, thus creating an environment that is conducive to stone formation and increasing the risk of postoperative recurrence[26]. Open choledocholithotomy plus LC or OC results in greater surgical trauma and a longer recovery period, which may increase the risk of postoperative complications, including biliary stricture and infection, which leads to the recurrence of stones. This also raises our awareness of the importance of the evaluation and management of the sphincter of Oddi function, and selecting the most suitable surgical method may help diminish the risk of recurrence. Furthermore, Chae et al[27] found through multi
This study has several limitations. First, the sample size included in this study was relatively small. When grouping based on the recurrence status, the number of patients was further reduced, which may influence the stability of the multivariate analysis. Second, not all patients with BDSs were suitable for laparoscopic surgery. For those with severe adhesions or abnormal anatomical structures, open surgery may be necessary. Third, as this study is a single-center analysis, the research findings obtained may not apply to other settings or populations. If a multi-center study can be conducted, more diverse data can be obtained, and the results can be verified in different settings. Fourth, as a re
In conclusion, for patients with EHBDSs, the treatment modality of LC plus CBDE can reduce stone residuals, intraoperative bleeding, complications, and postoperative recurrence.
| 1. | Littlefield A, Lenahan C. Cholelithiasis: Presentation and Management. J Midwifery Womens Health. 2019;64:289-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 49] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 2. | Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver. 2012;6:172-187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 556] [Cited by in RCA: 775] [Article Influence: 55.4] [Reference Citation Analysis (0)] |
| 3. | Wang H, He YQ, Dong SY, Zhong W, Tao P, Yang SY, Liu ZJ. Recurrence of common bile duct stones after choledocholithotomy in elderly patients: risk factor analysis and clinical prediction model development. Front Med (Lausanne). 2023;10:1239902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 4. | Marcelino LP, Thofehrn S, Eyff TF, Bersch VP, Osvaldt AB. Factors predictive of the successful treatment of choledocholithiasis. Surg Endosc. 2022;36:1838-1846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Mohseni S, Bass GA, Forssten MP, Casas IM, Martin M, Davis KA, Haut ER, Sugrue M, Kurihara H, Sarani B, Cao Y, Coimbra R. Common bile duct stones management: A network meta-analysis. J Trauma Acute Care Surg. 2022;93:e155-e165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 6. | Cianci P, Restini E. Management of cholelithiasis with choledocholithiasis: Endoscopic and surgical approaches. World J Gastroenterol. 2021;27:4536-4554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 99] [Cited by in RCA: 90] [Article Influence: 18.0] [Reference Citation Analysis (21)] |
| 7. | Tazuma S. Gallstone disease: Epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic). Best Pract Res Clin Gastroenterol. 2006;20:1075-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 317] [Article Influence: 15.9] [Reference Citation Analysis (2)] |
| 8. | Feng R, Zhang T, Kayani MUR, Wang Z, Shen Y, Su KL, Bielike K, Chen L. Patients with Primary and Secondary Bile Duct Stones Harbor Distinct Biliary Microbial Composition and Metabolic Potential. Front Cell Infect Microbiol. 2022;12:881489. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Kozyk M, Giri S, Harindranath S, Trivedi M, Strubchevska K, Barik RK, Sundaram S. Recurrence of common bile duct stones after endoscopic clearance and its predictors: A systematic review. DEN Open. 2024;4:e294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 10. | Lujian P, Xianneng C, Lei Z. Risk factors of stone recurrence after endoscopic retrograde cholangiopancreatography for common bile duct stones. Medicine (Baltimore). 2020;99:e20412. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | Warchałowski Ł, Łuszczki E, Bartosiewicz A, Dereń K, Warchałowska M, Oleksy Ł, Stolarczyk A, Podlasek R. The Analysis of Risk Factors in the Conversion from Laparoscopic to Open Cholecystectomy. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 12. | Mannam R, Sankara Narayanan R, Bansal A, Yanamaladoddi VR, Sarvepalli SS, Vemula SL, Aramadaka S. Laparoscopic Cholecystectomy Versus Open Cholecystectomy in Acute Cholecystitis: A Literature Review. Cureus. 2023;15:e45704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 13. | Montenegro DM, Chukwu M, Ehsan P, Aburumman RN, Muthanna SI, Menon SR, Vithani V, Sutariya B, Yu AK. The Safety of Minimally Invasive and Open Cholecystectomy in Elderly Patients With Acute Cholecystitis: A Systematic Review. Cureus. 2022;14:e31170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Guo T, Wang L, Xie P, Zhang Z, Huang X, Yu Y. Surgical methods of treatment for cholecystolithiasis combined with choledocholithiasis: six years' experience of a single institution. Surg Endosc. 2022;36:4903-4911. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 15. | Liu YY, Li TY, Wu SD, Fan Y. The safety and feasibility of laparoscopic approach for the management of intrahepatic and extrahepatic bile duct stones in patients with prior biliary tract surgical interventions. Sci Rep. 2022;12:14487. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Afghani E, Lo SK, Covington PS, Cash BD, Pandol SJ. Sphincter of Oddi Function and Risk Factors for Dysfunction. Front Nutr. 2017;4:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 17. | Fuchs KH, Musial F, Retzbach L, Hann A, Meining A. Quality of life in benign colorectal disease-a review of the assessment with the Gastrointestinal Quality of Life Index (GIQLI). Int J Colorectal Dis. 2023;38:172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 18. | Ramírez-Giraldo C, Torres-Cuellar A, Van-Londoño I. State of the art in subtotal cholecystectomy: An overview. Front Surg. 2023;10:1142579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 25] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 19. | Wilkins T, Agabin E, Varghese J, Talukder A. Gallbladder Dysfunction: Cholecystitis, Choledocholithiasis, Cholangitis, and Biliary Dyskinesia. Prim Care. 2017;44:575-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 20. | Mencarini L, Vestito A, Zagari RM, Montagnani M. The Diagnosis and Treatment of Acute Cholecystitis: A Comprehensive Narrative Review for a Practical Approach. J Clin Med. 2024;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 27] [Reference Citation Analysis (0)] |
| 21. | Xiao J, Chen M, Hong T, Qu Q, Li B, Liu W, He X. Surgical Management and Prognosis of Congenital Choledochal Cysts in Adults: A Single Asian Center Cohort of 69 Cases. J Oncol. 2022;2022:9930710. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 22. | Nakamura T, Sato T, Naito M, Ogura N, Yamanashi T, Miura H, Tsutsui A, Yamashita K, Watanabe M. Laparoscopic Surgery is Useful for Preventing Recurrence of Small Bowel Obstruction After Surgery for Postoperative Small Bowel Obstruction. Surg Laparosc Endosc Percutan Tech. 2016;26:e1-e4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 23. | Madani A, Namazi B, Altieri MS, Hashimoto DA, Rivera AM, Pucher PH, Navarrete-Welton A, Sankaranarayanan G, Brunt LM, Okrainec A, Alseidi A. Artificial Intelligence for Intraoperative Guidance: Using Semantic Segmentation to Identify Surgical Anatomy During Laparoscopic Cholecystectomy. Ann Surg. 2022;276:363-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 202] [Article Influence: 50.5] [Reference Citation Analysis (0)] |
| 24. | Tracy BM, Paterson CW, Torres DM, Young K, Hochman BR, Zielinski MD, Burruss SK, Mulder MB, Yeh DD, Gelbard RB; EAST Retained Common Bile Duct Stones Study Group. Risk factors for complications after cholecystectomy for common bile duct stones: An EAST multicenter study. Surgery. 2020;168:62-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Villavicencio Kim J, Wu GY. Update on Sphincter of Oddi Dysfunction: A Review. J Clin Transl Hepatol. 2022;10:515-521. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 26. | Zhang Q, Ye M, Su W, Chen Y, Lou Y, Yang J, Ma T, Chen W, Gao S, Que R, Zhang B, Li H, Bai X, Liang T. Sphincter of Oddi laxity alters bile duct microbiota and contributes to the recurrence of choledocholithiasis. Ann Transl Med. 2020;8:1383. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Chae MK, Lee SH, Joo KR. Assessment of the possible risk factors for primary common bile duct stone recurrence after cholecystectomy. Surg Endosc. 2021;35:6497-6504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/