Published online Jan 27, 2024. doi: 10.4240/wjgs.v16.i1.21
Peer-review started: October 2, 2023
First decision: December 6, 2023
Revised: December 13, 2023
Accepted: December 28, 2023
Article in press: December 28, 2023
Published online: January 27, 2024
Processing time: 114 Days and 16.3 Hours
The maximum outer diameter (MOD) of the appendix is an essential parameter for diagnosing acute appendicitis, but there is space for improvement in ultra
To investigate whether combining the ratio of the cross diameters (RATIO) of the appendix with MOD of the appendix can enhance the diagnostic performance of acute appendicitis.
A retrospective study was conducted, and medical records of 233 patients with acute appendicitis and 112 patients with a normal appendix were reviewed. The MOD and RATIO of the appendix were calculated and tested for their diagnostic performance of acute appendicitis, both individually and in combination.
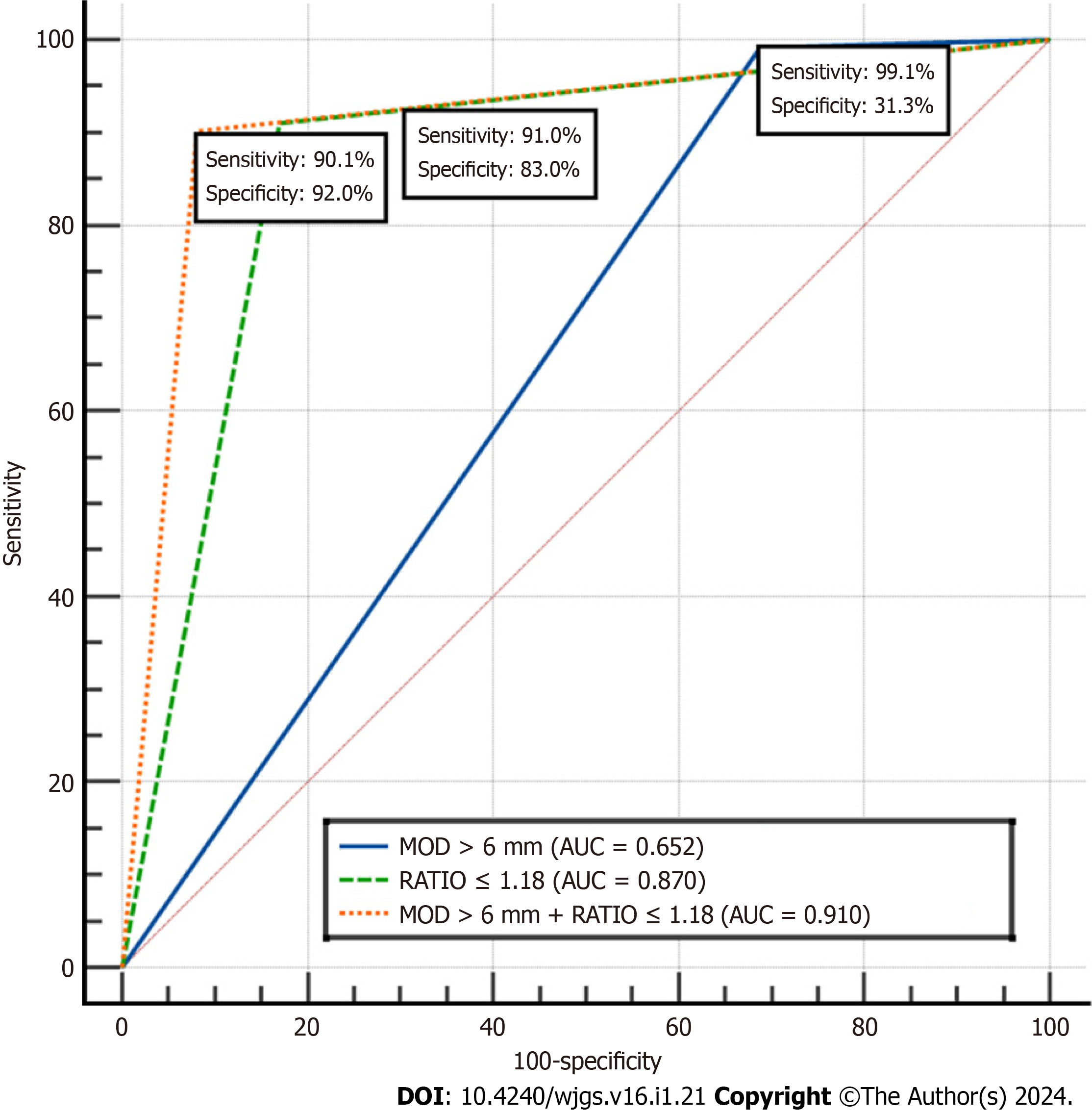
The RATIO for a normal appendix was 1.32 ± 0.16, while for acute appendicitis it was 1.09 ± 0.07. The cut-off value for RATIO was determined to be ≤ 1.18. The area under the receiver operating characteristic curve (AUC) for diagnosing acute appendicitis using RATIO ≤ 1.18 and MOD > 6 mm was 0.870 and 0.652, res
Combining RATIO of the appendix ≤ 1.18 and MOD > 6 mm can significantly improve the specificity, PPV, and AUC in the US diagnosis of acute appendicitis.
Core Tip: The maximum outer diameter (MOD) of the appendix has been an essential criterion for diagnosing acute appendicitis, but there is room for improvement in terms of sensitivity, specificity, and accuracy. In this study, we established a new parameter, the ratio of cross diameters on the transverse section of the appendix, for diagnosing acute appendicitis using ultrasound imaging. Combining this parameter with the MOD of the appendix can enhance diagnostic performance, making it more valuable in clinical practice.
- Citation: Gu FW, Wu SZ. Added value of ratio of cross diameters of the appendix in ultrasound diagnosis of acute appendicitis. World J Gastrointest Surg 2024; 16(1): 21-28
- URL: https://www.wjgnet.com/1948-9366/full/v16/i1/21.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i1.21
Acute appendicitis is the most common abdominal emergency in the world. The clinical diagnosis of acute appendicitis is based on history, physical examination, laboratory tests, and medical imaging. Although biomarkers and imaging are valuable adjuncts to history and physical examination, accurate preoperative diagnosis is still challenging[1]. Ultrasound (US) has been recommended for the evaluation of suspected appendicitis in recent dacades[2]. Previous studies[2-7] have showed that an appendix with a maximum outer diameter (MOD) of more than 6 mm, scanned at the point of maximum tenderness using US, is the main feature of acute appendicitis. Other findings include incompressibility of the enlarged appendix, presence of appendicoliths, equivocality or loss of mural stratification, increased echogenicity of periappen
In this cross-sectional retrospective study, medical documents of 21624 consecutive patients who had undergone US of the appendix for suspected acute appendicitis between January 2017 and August 2023 in a tertiary hospital were re
| Item | Normal appendix (n = 112) | Acute appendicitis (n = 233) | Statistics (t/χ2/Z) | P value |
| Sex, n (%) | 14.2882 | < 0.001 | ||
| Male | 29 (25.9) | 110 (47.2) | ||
| Female | 83 (74.1) | 123 (52.8) | ||
| Age (yr) M (IQR) | 31.0 (24.0, 39.8) | 37.0 (28.0, 49.5) | -3.4093 | 0.001 |
| Detectable length (mm) M (IQR) | 34.8 (29.8, 43.9) | 53.2 (45.0, 64.7) | -10.1643 | < 0.001 |
| SD (mm, mean ± SD) | 4.9 ± 0.9 | 9.9 ± 2.0 | -31.7221 | < 0.001 |
| LD (mm, mean ± SD) | 6.5 ± 1.0 | 10.7 ± 2.2 | -24.3401 | < 0.001 |
| RATIO (mean ± SD) | 1.32 ± 0.16 | 1.09 ± 0.07 | 15.0711 | < 0.001 |
| Mural lamina n (%) | 49.9492 | < 0.001 | ||
| Clear | 110 (98.2) | 146 (62.7) | ||
| Ambiguous | 2 (1.8) | 87 (37.3) | ||
| Mural vascularity, n (%) | 32.6942 | < 0.001 | ||
| Present | 12 (10.7) | 96 (41.2) | ||
| Absent | 100 (89.3) | 137 (58.8) | ||
| Luminal echogenicity, n (%) | ||||
| Thread-like high echoic | 62 (55.4) | 0 (0) | ||
| Anechoic | 2 (1.8) | 63 (27.0) | ||
| Hypoechoic | 36 (32.1) | 58 (24.9) | 197.3082 | < 0.001 |
| Isoechoic | 9 (8.0) | 13 (5.6) | ||
| Hyperechoic, shadowing | 1 (0.9) | 33 (14.2) | ||
| Complex echoic | 2 (1.8) | 66 (28.3) | ||
| MOD (mm), n (%) | ||||
| > 6 | 77 (68.8) | 231 (99.1) | 72.9712 | < 0.001 |
| ≤ 6 | 35 (31.2) | 2 (0.9) | ||
| > 7 | 30 (26.8) | 229 (98.3) | 206.6222 | < 0.001 |
| ≤ 7 | 82 (73.2) | 4 (1.7) | ||
| > 8 | 10 (8.9) | 212 (91.0) | 222.0152 | < 0.001 |
| ≤ 8 | 102 (91.1) | 21 (9.0) |
| Item | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | AUC (95%CI) |
| RATIO (1.18) | 91.0 | 83.0 | 91.8 | 81.6 | 0.870 (0.830-0.904) |
| MOD (> 6 mm) | 99.1 | 31.3 | 75.0 | 94.6 | 0.652 (0.599-0.702) |
| RATIO + MOD > 6 mm | 90.1 | 92.0 | 95.9 | 81.7 | 0.910 (0.875-0.938) |
Patients who were referred to a tertiary hospital with suspected acute appendicitis received an appendix examination by physicians skilled in US. These physicians had between 1 to 30 years of experience in performing appendix USs. Multi-parameter US systems (Mindray DC 8, Aloka Prosound α-7, Aloka Prosound α-10, Mindray Resona 7, Phillips EPIQ5, and GE Logiq E9) with a linear array transducer were used for the examination. The working frequencies ranged from 10 MHz to 15 MHz, but lower frequencies were used if the appendix could not be visualized.
During the examination, the US systems were adjusted to the small parts mode for bowel imaging. The patients were positioned supine on the table with their abdominal region fully exposed. The bowel and abdominal cavity were carefully scanned to detect any abnormalities. A graded compression US protocol was performed, allowing visualization of the right psoas muscle and right external iliac artery and vein during compression. Once the appendix was visualized, various characteristics were examined, including its location, shape, size, boundary, luminal and mural echogenicity, thickness and stratification of the appendiceal wall, vascularity, mesoappendix, periappendiceal epiploic appendages, omentum, periappendiceal fluid, and any associating findings (such as lymphadenitis). The size of the appendix was determined at its greatest dimension in both longitudinal and transverse views. The measurement of size in the trans
Two physicians-in-US (radiologists) (a junior with 2 years and a senior physician with 20 years of abdominal US experience) evaluated the images of all the patients. They assessed the shape, size, echogenicity of the appendiceal lumen and wall, thickness and lamina of the appendiceal wall, the ratio on transverse section (dividing the larger diameter by the smaller diameter), appendicolithiasis, and vascularity. Appendicolithiasis was defined as an intraluminal echogenic focus or foci with distal acoustic shadowing. Luminal obstruction was defined as appendicolithiasis in the proximal lumen and was accompanied by fluid or other substances filling the lumen. Fluid in the appendiceal lumen and vascu
The histopathology of acute appendicitis and its grade was recorded based on the post-surgical evaluation, which was assessed by two certified pathologists. Acute appendicitis was classified as phlegmonous, gangrenous, and perforated appendicitis.
Continuous variables with a normal distribution were represented as mean ± SD, while those that did not meet the normal distribution were represented as median (interquartile range). The Kolmogorov-Smirnov test was used for the distribution analysis. Categorical variables were represented as numbers (percentage). Primary descriptive statistics of the study were reported. Independent sample t-test and Mann-Whitney U test were used for the analysis of continuous variables with and without a normal distribution, respectively. The diagnostic performance of acute appendicitis was studied based on MOD > 6 mm on the transverse section of the appendix and a combination of RATIO ≤ 1.18 and MOD > 6 mm, as determined by literature and this study[2]. The χ2 test was used for the analysis of categorical variables. McNemar test was used to test the sensitivity, specificity positive predictive value (PPV), and negative predictive value (NPV). The ROC curve was drawn, the area under the ROC curve (AUC) was calculated, and the Youden index was determined to establish the cut-off value for sensitivity and specificity. PPV and NPV were also calculated. All analyses were conducted using SPSS software for Windows, version 26 (IBM Corp, Armonk, NY, United States) and/or Medcalc statistical software version 15.2.2 (Medcalc software BVBA, Ostend, Belgium). A two-tailed P < 0.05 was considered statistically significant.
The MODs and RATIOs of the normal appendix and acute appendicitis were 6.5 ± 1.0 mm and 10.7 ± 2.2 mm, and 1.32 ± 0.16 and 1.09 ± 0.07, respectively, with significant differences between them (all P < 0.001). The MODs on the transverse section and RATIOs of the normal appendix and acute appendicitis were all normally distributed. The baseline demo
The clinical manifestations of acute appendicitis vary greatly, and the diagnosis is usually comprehensive, often requiring medical imaging for many patients with suspected acute appendicitis[1]. US is an important technique in the study of appendicitis. A meta-analysis has shown that US, computed tomography, and magnetic resonance imaging have com
When using MOD > 6 mm as a reference for evaluating the appendix, the outcomes were a sensitivity of 99.1%, specificity of 31.3%, PPV of 75.0%, NPV of 94.6%, and AUC of 0.652. These results were lower than those reported by Rettenbacher et al[5],which showed a sensitivity of 100%, specificity of 68%, NPV of 100%, accuracy of 79%, and a lower PPV of 63%. The difference in sample size may contribute to the variation in outcomes. This finding is consistent with the study by Chicaiza et al[7], where using a cutoff of MOD 6 mm resulted in sensitivity and specificity of 100% and 43%, respectively, while using a cutoff of MOD 7 mm decreased the sensitivity to 94% and increased the specificity to 71%. Previous studies[16,17] have shown that lymphoid hyperplasia of the appendix, due to hypertrophy of lymphoid follicles in response to gastrointestinal inflammatory diseases, chronic constipation, and cystic fibrosis, can increase the MOD of the appendix. This can result in a noncompressible appendix with a borderline size of 6-8 mm in outer diameter, poten
In this study, when using MOD > 6 mm and a combination of RATIO ≤ 1.18 and MOD > 6 mm as references for evaluating the appendix, the AUC of the combination of RATIO ≤ 1.18 and MOD > 6 mm increased significantly, along with an increase in specificity and PPV, and a decrease in sensitivity and NPV compared to using MOD > 6mm alone. These findings indicate that the combination of RATIO ≤ 1.18 and MOD > 6mm can address the bias of using MOD > 6 mm alone and significantly improve specificity, PPV, and AUC.
The strengths of this study include a large sample of patients with histopathologically confirmed acute appendicitis, ensuring the reliability of the results. Additionally, the establishment of the RATIO of cross diameters on the transverse section of the appendix introduces a new concept, adding valuable information to the existing literature.
There were some potential limitations in this study. Firstly, the retrospective study design may have resulted in the loss of certain information regarding the appendiceal structure. Secondly, patients with appendiceal perforation and appendiceal tumors were excluded, which means that not all US features of acute appendicitis were collected and analyzed. The appendiceal MOD in patients with appendiceal perforation may be smaller than 6 mm, and the shape and RATIO of the cross diameters on the transverse section of the appendix may differ from those without appendiceal perforation. Additionally, the inter- and intra-observer agreements of appendiceal measurements by different US per
A combination of a ratio ≤ 1.18 on the cross diameters on the transverse section of the appendix and MOD > 6 mm can significantly increase the specificity, PPV, and AUC compared to using MOD > 6 mm alone.
Ultrasound (US) is commonly used for diagnosing acute appendicitis, but the diagnostic performance remains for further improvement. The size of the appendix is crucial for distinguishing between a normal appendix and acute appendicitis.
The maximal outside diameter on the cross section of the appendix > 6 mm has been recommended as a cut-off value for diagnosing acute appendicitis, but the minimal outside diameter and the ratio of the two outside diameters have not been adequately studied.
To investigate if the ratio of the two outside diameters on the cross section of the appendix is a useful parameter for diagnosing acute appendicitis.
The investigators measured the two outside diameters on the cross section of a normal appendix and acute appendicitis without perforation using ultrasonography and calculated their ratio. The diagnostic performance of the maximal outside diameter, the ratio of two diameters on the cross section of the appendix, and their combination were compared.
A ratio of the diameter on the cross section of the appendix ≤ 1.18 was identified as a cut-off value for predicting acute appendicitis. The diagnostic performance based on the ratio of two diameters on the cross section of the appendix ≤ 1.18 was significantly higher than that of the maximal outside diameter.
Combining the maximal outside diameter and the ratio of two diameters on the cross section of the appendix improved diagnostic performance compared to using the maximal outside diameter alone.
Further prospective studies are needed to validate the findings and the use of a combination of the maximal outside diameter and the ratio of two diameters for US diagnosis of acute appendicitis.
| 1. | Moris D, Paulson EK, Pappas TN. Diagnosis and Management of Acute Appendicitis in Adults: A Review. JAMA. 2021;326:2299-2311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 208] [Article Influence: 41.6] [Reference Citation Analysis (112)] |
| 2. | Dirks K, Calabrese E, Dietrich CF, Gilja OH, Hausken T, Higginson A, Hollerweger A, Maconi G, Maaser C, Nuernberg D, Nylund K, Pallotta N, Ripolles T, Romanini L, Saftoiu A, Serra C, Wüstner M, Sporea I. EFSUMB Position Paper: Recommendations for Gastrointestinal Ultrasound (GIUS) in Acute Appendicitis and Diverticulitis. Ultraschall Med. 2019;40:163-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 51] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 3. | Arruzza E, Milanese S, Li LSK, Dizon J. Diagnostic accuracy of computed tomography and ultrasound for the diagnosis of acute appendicitis: A systematic review and meta-analysis. Radiography (Lond). 2022;28:1127-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 26] [Reference Citation Analysis (0)] |
| 4. | Cho SU, Oh SK. Accuracy of ultrasound for the diagnosis of acute appendicitis in the emergency department: A systematic review. Medicine (Baltimore). 2023;102:e33397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 20] [Reference Citation Analysis (0)] |
| 5. | Rettenbacher T, Hollerweger A, Macheiner P, Rettenbacher L, Tomaselli F, Schneider B, Gritzmann N. Outer diameter of the vermiform appendix as a sign of acute appendicitis: evaluation at US. Radiology. 2001;218:757-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 78] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | Kessler N, Cyteval C, Gallix B, Lesnik A, Blayac PM, Pujol J, Bruel JM, Taourel P. Appendicitis: evaluation of sensitivity, specificity, and predictive values of US, Doppler US, and laboratory findings. Radiology. 2004;230:472-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 151] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 7. | Chicaiza HP, Malia L, Mulvey CH, Smith SR. Revisiting the Appendiceal Diameter via Ultrasound for the Diagnosis of Acute Appendicitis. Pediatr Emerg Care. 2018;34:757-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Ozel A, Orhan UP, Akdana B, Disli C, Erturk SM, Basak M, Karpat Z. Sonographic appearance of the normal appendix in children. J Clin Ultrasound. 2011;39:183-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Coyne SM, Zhang B, Trout AT. Does appendiceal diameter change with age? A sonographic study. AJR Am J Roentgenol. 2014;203:1120-1126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Sivit CJ. Diagnosis of acute appendicitis in children: spectrum of sonographic findings. AJR Am J Roentgenol. 1993;161:147-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 67] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Kim DW, Suh CH, Yoon HM, Kim JR, Jung AY, Lee JS, Cho YA. Visibility of Normal Appendix on CT, MRI, and Sonography: A Systematic Review and Meta-Analysis. AJR Am J Roentgenol. 2018;211:W140-W150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Eng KA, Abadeh A, Ligocki C, Lee YK, Moineddin R, Adams-Webber T, Schuh S, Doria AS. Acute Appendicitis: A Meta-Analysis of the Diagnostic Accuracy of US, CT, and MRI as Second-Line Imaging Tests after an Initial US. Radiology. 2018;288:717-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 60] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 13. | Ge H, Miao L, Zhang F, Lin Z, Zhang L, Dou R, Fang N, Song K. Overview of the ultrasonography techniques in the diagnosis of appendicitis - elaboration of a novel anatomy scanning method. Med Ultrason. 2020;22:334-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Sezer TO, Gulece B, Zalluhoglu N, Gorgun M, Dogan S. Diagnostic value of ultrasonography in appendicitis. Adv Clin Exp Med. 2012;21:633-636. [PubMed] |
| 15. | Rettenbacher T, Hollerweger A, Macheiner P, Gritzmann N, Daniaux M, Schwamberger K, Ulmer H, zur Nedden D. Ovoid shape of the vermiform appendix: a criterion to exclude acute appendicitis--evaluation with US. Radiology. 2003;226:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Aydın S, Karavas E, Şenbil DC. Imaging of acute appendicitis: Advances. World J Gastrointest Surg. 2022;14:370-373. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Reference Citation Analysis (0)] |
| 17. | Madhuripan N, Jawahar A, Jeffrey RB, Olcott EW. The Borderline-Size Appendix: Grayscale, Color Doppler, and Spectral Doppler Findings That Improve Specificity for the Sonographic Diagnosis of Acute Appendicitis. Ultrasound Q. 2020;36:314-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Montero JA S-Editor: Qu XL L-Editor: A P-Editor: Xu ZH