Published online Jan 27, 2024. doi: 10.4240/wjgs.v16.i1.13
Peer-review started: November 21, 2023
First decision: December 11, 2023
Revised: December 21, 2023
Accepted: January 8, 2024
Article in press: January 8, 2024
Published online: January 27, 2024
Processing time: 65 Days and 2.2 Hours
Liver transplantation is the primary therapeutic intervention for end-stage liver disease. However, vascular complications, particularly those involving the hepatic artery, pose significant risks to patients. The clinical manifestations associated with early arterial complications following liver transplantation are often non
Core Tip: The clinical manifestations associated with early arterial complications following liver transplantation are often nonspecific. Without timely intervention, these complications can result in graft failure or patient mortality. Early diagnosis and the formulation of an optimal treatment plan are imperative. Ultrasound examination remains the predominant imaging modality for detecting complications post liver transplantation. And ultrasound has the advantages of convenience, safety, effectiveness, and non-invasiveness, and enables real-time, dynamic, and accurate evaluation, making it the preferred diagnostic method for post-liver transplantation evaluation.
- Citation: Zhao NB, Chen Y, Xia R, Tang JB, Zhao D. Prognostic value of ultrasound in early arterial complications post liver transplant. World J Gastrointest Surg 2024; 16(1): 13-20
- URL: https://www.wjgnet.com/1948-9366/full/v16/i1/13.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i1.13
Liver transplantation stands as the primary therapeutic approach for end-stage liver disease. Continuous advancements in surgical techniques and the application of novel immunosuppressive agents contribute to ongoing improvements in the success rate and overall survival in patients undergoing liver transplantation procedures. Despite these advan
During the intraoperative phase, an ultrasound examination is typically conducted to evaluate the hepatic artery anas
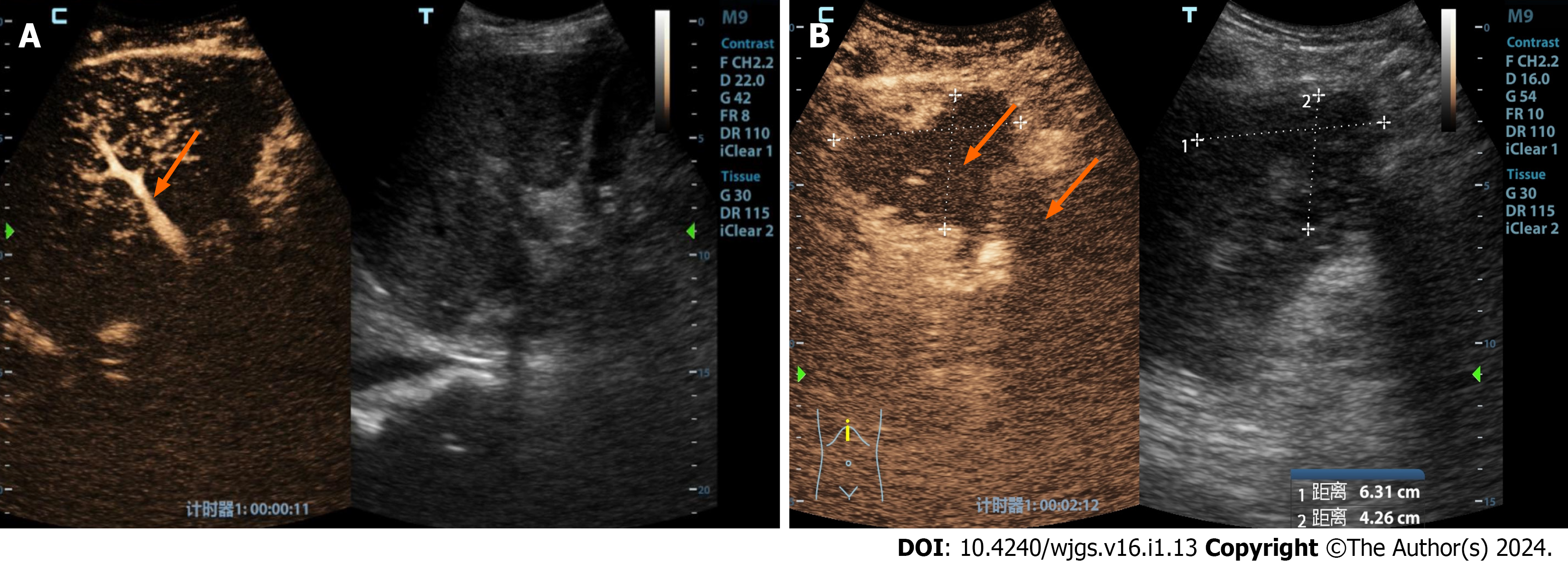
Hepatic artery thrombosis (HAT) represents a serious complication following liver transplantation, with an incidence rate ranging from 3% to 5%[2,3]. Early risk factors for HAT encompass ABO-blood type incompatibility, prolonged cold ischemia time for the donor’s liver, acute rejection reaction, hepatic artery spasm, intimal dissection, perianastomotic hematoma compression, arterial torsion, undersized donor hepatic artery diameter, and mismatched anastomotic size[4,5]. HAT leads to a reduction in blood supply to the liver, particularly in the early postoperative period, and can result in severe complications, with mortality rates reaching 20%-60%. Clinical presentations of HAT include severe hepatic pain, fever, ascites, abrupt elevation of serum aminotransferases, decreased bile flow, altered bile properties, prolonged pro
HAT is characterized by the absence of color Doppler and spectral Doppler signals in the region of the hepatic artery’s course. However, blood flow signals may still be detected in some HAT cases due to the development of hepatic arterial collateral circulation, which can occur as early as 2 wk postoperatively. Color Doppler ultrasound can detect blood flow signals in the hepatic artery after the formation of collateral circulation, showing tardus-parvus waveforms with specific features (RI < 0.5 and SAT > 80 ms). It is important to note that the inability to detect hepatic artery blood flow signals using Doppler ultrasound is not a definitive diagnostic criterion for hepatic artery occlusion. Studies indicate that the accuracy of using color Doppler in diagnosing HAT is only 64%, influenced by factors such as operator experience, equip
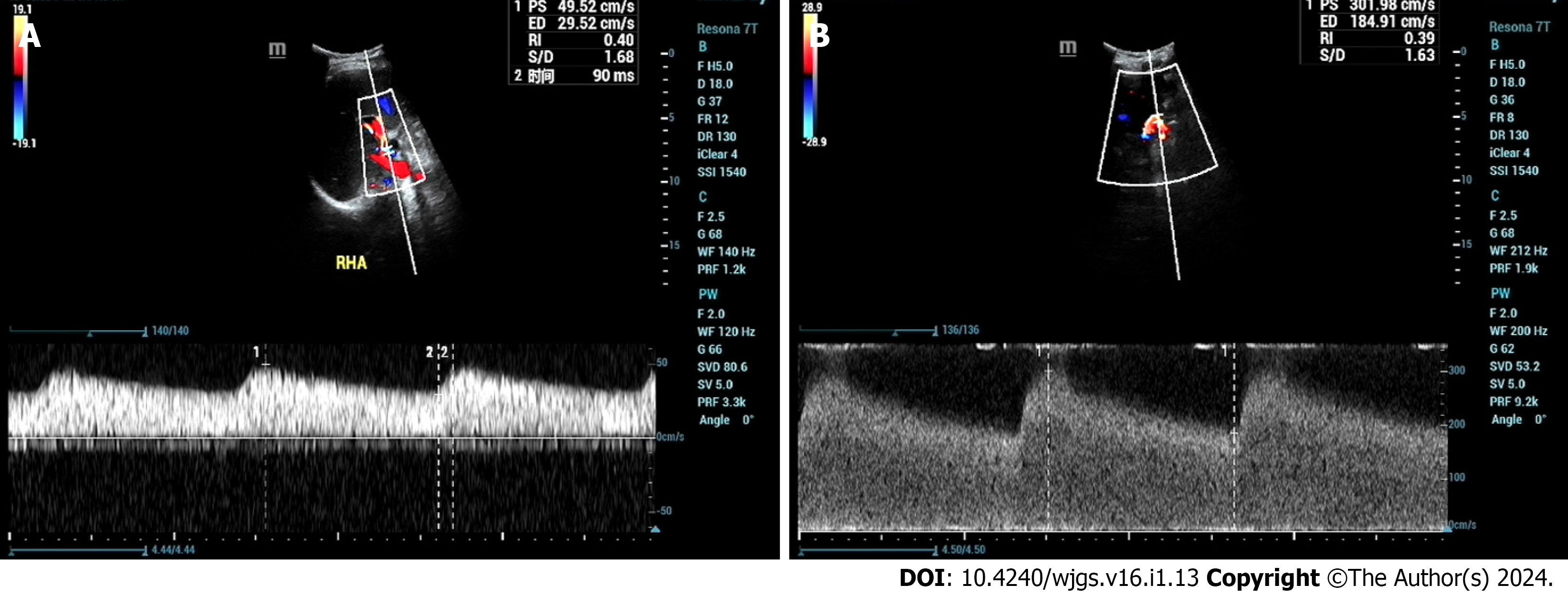
Hepatic artery stenosis (HAS) is a relatively common vascular complication after liver transplantation, with a high inci
Direct visualization of the HAS site by ultrasound is typically challenging, relying on the indirect diagnosis of intra
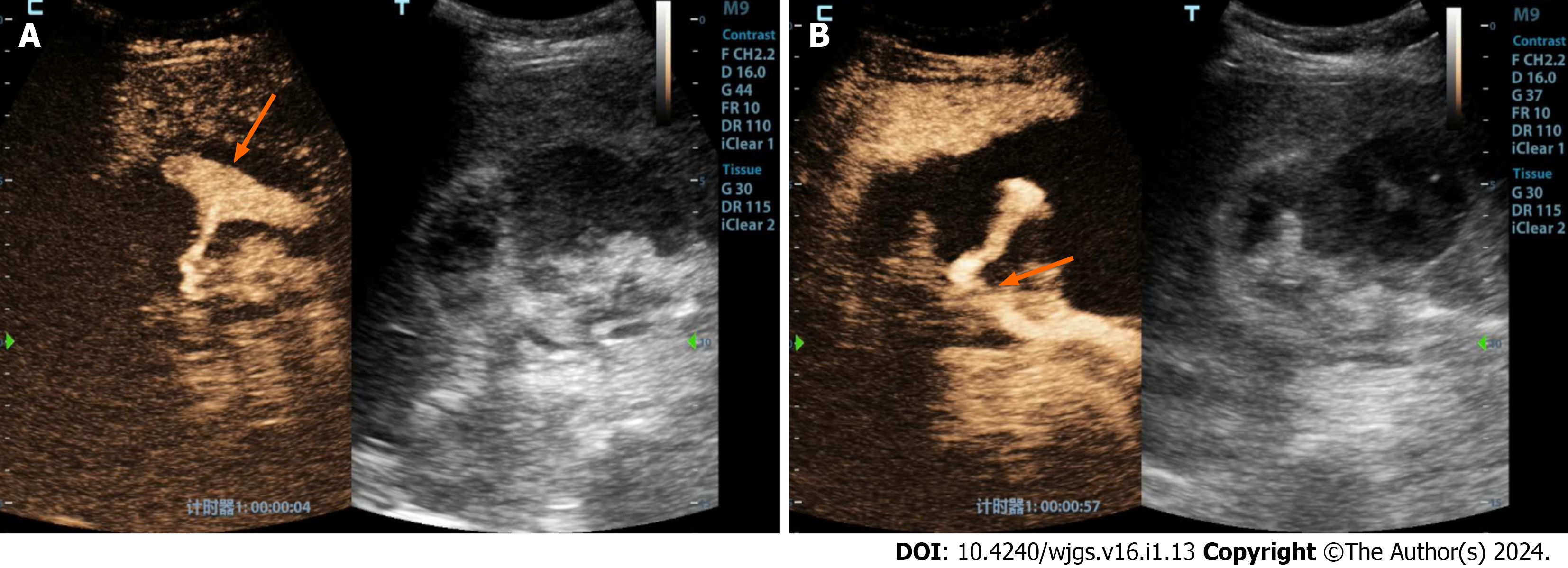
Hepatic artery aneurysm (HAA) is relatively rare following liver transplantation[20,21]. There are three main types of HAA: Congenital or acquired true HAA caused by factors such as atherosclerosis, fungal infections, necrotizing vascu
HAP often occurs at the arterial anastomosis site or at the site of intervention or puncture[25]. The peripheral soft tissue wrapping hematoma forms due to the ruptured hemorrhage of the arterial wall[26,27]. Gray-scale ultrasound shows the cystic anechoic area of the hepatic artery with a clear boundary. Color Doppler presents characteristic red and blue alter
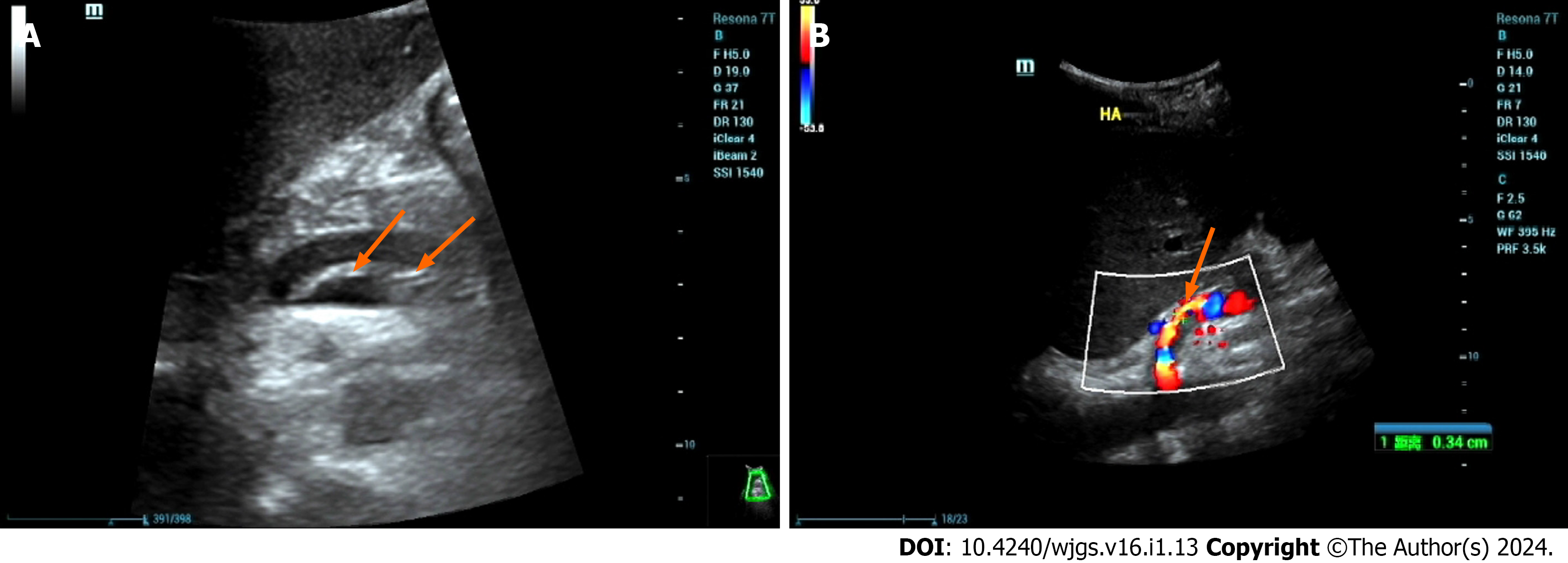
HDA often results from the rupture of the intima and media layers due to various factors, leading to the entry of blood into the medial layer, causing the neoplastic structure to tear, resulting in the stratification of the vessel wall, and dividing the artery into true and false lumens. These lumens may or may not communicate through the rupture site. Ultrasound reveals the following characteristics: (1) Intimal stratification signs, where the separated intima may be fixed or float with the bloodstream. True and false cavities may have inlet and outlet connections or exist as separate structures (Figure 3A); (2) an increase in arterial diameter; (3) blood flow stratification phenomenon, where the separated intima divides arterial blood flow into two layers, representing the blood flow in the true lumen and the false lumen, each with distinct blood flow spectra (Figure 3B); (4) thrombosis in the false lumen; and (5) vascular narrowing in the true lumen.
The following features indicate that urgent intervention is necessary for a dissecting aneurysm: (1) Tardus-parvus waveform observed in the hepatic artery of the liver; (2) an increase in peak contraction velocity at the tumor body (> 200 cm/s); and (3) absence of blood flow signal in the liver[28].
Hepatic artery vasospasm (HAV) is characterized by intense constriction of the arterial vessel wall, resulting in rigidity, narrowing, or occlusion of the affected portion or the entire vessel[29]. This common complication during the recipient’s surgical process is often secondary to excessive manipulation and suturing. Despite a lack of sufficient data and widely recognized diagnostic criteria, animal and clinical studies suggest that elevated serum norepinephrine levels may influ
Doppler ultrasound lacks uniform diagnostic criteria for HAV, with manifestations such as arterial shortening, na
Hepatic artery distortion (HAD) is a common condition in liver transplant surgery, where the recipient’s hepatic artery is lengthened to reduce tension at the anastomosis site, resulting in a twisted appearance near the liver hilum. This twisting generally does not affect hepatic blood supply, and color Doppler shows a bright blood flow signal in the distorted seg
Hepatic artery rupture (HAR) carries severe consequences, potentially leading to hemorrhagic shock or even death[34]. Immediate intervention through surgical or vascular procedures is essential once the diagnosis is confirmed. Ruptures typically occur near the anastomosis site and can result from various factors, including suture line failure, avascular ne
In conclusion, the clinical presentations associated with early arterial complications after liver transplantation are often nonspecific. Without timely intervention, these complications can lead to graft failure or patient mortality. Early diag
| 1. | Kok T, Haagsma EB, Klompmaker IJ, Zwaveling JH, Peeters PM, Bijleveld CM, Meerman L, Slooff MJ. Doppler ultrasound of the hepatic artery and vein performed daily in the first two weeks after orthotopic liver transplantation. Useful for the diagnosis of acute rejection? Invest Radiol. 1996;31:173-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Nickel KJ, Morzycki A, Visser L, Bell E, Ladak A. Effect of magnification in pediatric liver transplantation: A systematic review and meta-analysis. Pediatr Transplant. 2022;26:e14223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Warner P, Fusai G, Glantzounis GK, Sabin CA, Rolando N, Patch D, Sharma D, Davidson BR, Rolles K, Burroughs AK. Risk factors associated with early hepatic artery thrombosis after orthotopic liver transplantation - univariable and multivariable analysis. Transpl Int. 2011;24:401-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 71] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 4. | Vasant Kulkarni S, Rao PP, Naidu CS, Pathak N, Singh AK. Evaluation of implantable Doppler probe continuous monitoring of hepatic artery anastomosis after liver transplantation. Med J Armed Forces India. 2021;77:349-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Yang Y, Zhao JC, Yan LN, Ma YK, Huang B, Yuan D, Li B, Wen TF, Wang WT, Xu MQ, Yang JY. Risk factors associated with early and late HAT after adult liver transplantation. World J Gastroenterol. 2014;20:10545-10552. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 51] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (1)] |
| 6. | Mine T, Murata S, Ueda T, Takeda M, Onozawa S, Yamaguchi H, Kawano Y, Kumita S. Contribution of extrahepatic collaterals to liver parenchymal circulation after proper hepatic artery embolization. J Gastroenterol Hepatol. 2014;29:1515-1521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Harihara Y, Makuuchi M, Takayama T, Kawarasaki H, Kubota K, Ito M, Tanaka H, Aoyanagi N, Matsukura A, Kita Y, Saiura A, Sakamoto Y, Kobayashi T, Sano K, Hashizume K, Nakatsuka T. Arterial waveforms on Doppler ultrasonography predicting or supporting hepatic arterial thrombosis in liver transplantation. Transplant Proc. 1998;30:3188-3189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Ren J, Wu T, Zheng BW, Tan YY, Zheng RQ, Chen GH. Application of contrast-enhanced ultrasound after liver transplantation: Current status and perspectives. World J Gastroenterol. 2016;22:1607-1616. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 21] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Kim JS, Kim KW, Lee J, Kwon HJ, Kwon JH, Song GW, Lee SG. Diagnostic Performance for Hepatic Artery Occlusion After Liver Transplantation: Computed Tomography Angiography Versus Contrast-Enhanced Ultrasound. Liver Transpl. 2019;25:1651-1660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Lu Q, Zhong XF, Huang ZX, Yu BY, Ma BY, Ling WW, Wu H, Yang JY, Luo Y. Role of contrast-enhanced ultrasound in decision support for diagnosis and treatment of hepatic artery thrombosis after liver transplantation. Eur J Radiol. 2012;81:e338-e343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Kim JS, Kim KW, Choi SH, Jeong SY, Kwon JH, Song GW, Lee SG. Hepatic Artery Occlusion after Liver Transplantation in Patients with Doppler Ultrasound Abnormality: Increasing Sensitivity of Contrast-Enhanced Ultrasound Diagnosis. Korean J Radiol. 2019;20:459-468. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Ningbo Z, Yu Z, Rui S, Feng K, Yi C, Nan J. Changfeng D. Multimodal Imaging Technique Value in The diagnosis and treatment of acute hepatic artery occlusion after liver transplantation. Rare J Dis. 2021;28:62-66. [DOI] [Full Text] |
| 13. | Dodd GD 3rd, Memel DS, Zajko AB, Baron RL, Santaguida LA. Hepatic artery stenosis and thrombosis in transplant recipients: Doppler diagnosis with resistive index and systolic acceleration time. Radiology. 1994;192:657-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 265] [Cited by in RCA: 237] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 14. | Amesur NB, Zajko AB. Interventional radiology in liver transplantation. Liver Transpl. 2006;12:330-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Zhao NB, Feng WX, Deng F, Dong CF, Zhou P, Gong XH. Clinical value of Tardus Parvus waveform and microperfusion after liver transplantation. Zhongguo Linchuang Jiepouxue Zazhi. 2020;38:723-727. [DOI] [Full Text] |
| 16. | Bude RO, Rubin JM, Platt JF, Fechner KP, Adler RS. Pulsus tardus: its cause and potential limitations in detection of arterial stenosis. Radiology. 1994;190:779-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 65] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Zheng BW, Tan YY, Fu BS, Tong G, Wu T, Wu LL, Meng XC, Zheng RQ, Yi SH, Ren J. Tardus parvus waveforms in Doppler ultrasonography for hepatic artery stenosis after liver transplantation: can a new cut-off value guide the next step? Abdom Radiol (NY). 2018;43:1634-1641. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Dravid VS, Shapiro MJ, Needleman L, Bonn J, Sullivan KL, Moritz MJ, Gardiner GA Jr. Arterial abnormalities following orthotopic liver transplantation: arteriographic findings and correlation with Doppler sonographic findings. AJR Am J Roentgenol. 1994;163:585-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Gómez Rodríguez R. Contrast-enhanced ultrasonography - An indispensable tool in the hands of any hepatologist. Rev Esp Enferm Dig. 2019;111:335-337. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 20. | Maggi U, Dondossola D, Consonni D, Gatti S, Arnoldi R, Bossi M, Rossi G. Visceral artery aneurysms in liver transplant candidates and in patients after liver transplantation. PLoS One. 2011;6:e29544. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Leelaudomlipi S, Bramhall SR, Gunson BK, Candinas D, Buckels JA, McMaster P, Mirza DF, Mayer AD. Hepatic-artery aneurysm in adult liver transplantation. Transpl Int. 2003;16:257-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 22. | Asonuma K, Ohshiro H, Izaki T, Okajima H, Ueno M, Kodera A, Inomata Y. Rescue for rare complications of the hepatic artery in living donor liver transplantation using grafts of autologous inferior mesenteric artery. Transpl Int. 2004;17:639-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Shimata K, Sugawara Y, Irie T, Sambommatsu Y, Kadohisa M, Ibuki S, Kawabata S, Isono K, Honda M, Yamamoto H, Hibi T. Asymptomatic hepatic artery dissection early after living-donor liver transplantation with simultaneous splenectomy: two case reports. BMC Gastroenterol. 2020;20:378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Vignali C, Bargellini I, Cioni R, Petruzzi P, Cicorelli A, Lazzereschi M, Urbani L, Filipponi F, Bartolozzi C. Diagnosis and treatment of hepatic artery stenosis after orthotopic liver transplantation. Transplant Proc. 2004;36:2771-2773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 25. | Marshall MM, Muiesan P, Srinivasan P, Kane PA, Rela M, Heaton ND, Karani JB, Sidhu PS. Hepatic artery pseudoaneurysms following liver transplantation: incidence, presenting features and management. Clin Radiol. 2001;56:579-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 100] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 26. | Jia F, Xia G, Zhu Q, Yu S, Hu N, Zhang H. Hepatic artery pseudoaneurysm caused by chronic pancreatitis: Case report and literature review. Medicine (Baltimore). 2023;102:e32834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 27. | Stephenson K, Kalkwarf K, Giorgakis E. Application of resuscitative endovascular balloon occlusion in post-transplant mycotic hepatic artery pseudoaneurysm rupture in the setting of Aspergillus Constellatus bacteremia. Ann Hepatobiliary Pancreat Surg. 2021;25:126-131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 28. | Breguet R, Dondero F, Pupulim L, Goossens N, Sepulveda A, Francoz C, Durand F, Terraz S, Vilgrain V, Ronot M. Endovascular Treatment of Arterial Complications After Liver Transplantation: Long-Term Follow-Up Evaluated on Doppler Ultrasound and Magnetic Resonance Cholangiopancreatography. Cardiovasc Intervent Radiol. 2019;42:381-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Sakamoto Y, Harihara Y, Nakatsuka T, Kawarasaki H, Takayama T, Kubota K, Kimura W, Kita Y, Tanaka H, Ito M, Hashizume K, Makuuchi M. Rescue of liver grafts from hepatic artery occlusion in living-related liver transplantation. Br J Surg. 1999;86:886-889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 30. | Acosta F, Diaz J, Sansano T, Palenciano CG, Reche M, Beltran R, Roques V, Robles R, Bueno FS, Ramirez P, Parrilla P. Evolution of the plasma concentration of norepinephrine in cirrhotic patients during liver transplantation. Transplant Proc. 2000;32:2659-2660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 31. | Hiraki Y, Uchida K, Nishida S, Levi DM, Selvaggi G, Tekin A, Fan J, Froud T, Tzakis AG. A Case Report of Severe Hepatic Artery Vasospasm Induced by Hepatic Arterial Buffer Response After Liver Transplantation. Transplant Proc. 2016;48:3167-3170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 32. | Temiz G, Mezili C, Tiftikçioğlu YÖ, Şirinoğlu H, Çinar M, Kismali E, Nart D, Gürler T, Alper M. Evaluation of the Effects of Bile on the Arterial Tonus in a Rabbit Model. Plast Reconstr Surg Glob Open. 2015;3:e570. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 33. | Richards RR, Seaber AV, Urbaniak JR. Chemically induced vasospasm: the effect of ischemia, vessel occlusion, and adrenergic blockade. Plast Reconstr Surg. 1985;75:238-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 34. | Golse N, Spina A, Abdelaal A, Mennesson N, Feugier P, Dumortier J, Boillot O, Adham M. Extra-anatomical hepatic artery reconstruction following post-embolization iatrogenic dissection and arterial anastomotic rupture in two liver transplant recipients. Gastroenterol Clin Biol. 2010;34:111-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 35. | Durkin N, Deganello A, Sellars ME, Sidhu PS, Davenport M, Makin E. Post-traumatic liver and splenic pseudoaneurysms in children: Diagnosis, management, and follow-up screening using contrast enhanced ultrasound (CEUS). J Pediatr Surg. 2016;51:289-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 62] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tovikkai C, Thailand S-Editor: Chen YL L-Editor: Wang TQ P-Editor: Xu ZH