Published online Jul 27, 2023. doi: 10.4240/wjgs.v15.i7.1434
Peer-review started: April 19, 2023
First decision: April 28, 2023
Revised: May 18, 2023
Accepted: June 2, 2023
Article in press: June 2, 2023
Published online: July 27, 2023
Processing time: 93 Days and 6.1 Hours
Perforated peptic ulcer (PPU) is a common emergency surgical condition and a significant cause of morbidity and mortality worldwide. While advances in surgical techniques have improved outcomes for patients with PPU, many factors still affect postoperative hospital stay and overall prognosis. One potential factor is the serum albumin (SA) level, a widely utilized marker of nutritional status that has been associated with length of stay and complications in various surgical procedures.
To clarify the correlation of SA level on postoperative day 2 with hospital length of stay (HLOS) in patients undergoing emergency surgery for perforated peptic ulcer (PPU).
We retrospectively collected and analyzed clinical baseline data, including blood routine and SA levels, of patients who underwent emergency PPU surgery and postoperative treatment at the Lingnan Hospital, the Third Affiliated Hospital of Sun Yat-sen University between December 2012 and September 2021. Patients were grouped according to HLOS with 7 d as the cut-off value, and relevant indicators were analyzed using SPSS 26.0.
Of the 37 patients undergoing emergency surgery for PPU referred to our department, 33 had gastric and 4 had duodenal ulcer perforation. The median HLOS was 10 d. There were 8 patients in the ≤ 7-d group (median HLOS: 7 d) and 29 patients in the > 7-d group (median HLOS: 10 d). The ≤ 7-d group had markedly higher SA on postoperative day 2 than the > 7-d group (37.7 g/L vs 32.6g/L; P < 0.05). The SA level on postoperative day 2 was a protective factor for patients with HLOS > 7 d (Odds ratio = 0.629, P = 0.015). The cut-off of SA on postoperative day 2 was 30.6g/L, with an area under the curve of 0.86 and a negative predictive value of 100% for the prediction of HLOS ≤ 7 d.
The SA level on postoperative day 2 was associated with the HLOS in patients undergoing emergency surgery for PPU. The pre- and post-operative albumin levels should be monitored, and infusion of human SA should be considered in a timely manner.
Core Tip: Serum albumin (SA) level is a useful marker of nutritional status and has been associated with postoperative outcomes in various surgical procedures. This study found that lower SA levels on postoperative day 2 were significantly associated with longer hospital length of stay in patients undergoing emergency surgery for perforated peptic ulcer. Monitoring and optimizing SA levels may be an important aspect of perioperative care for this high-risk patient population.
- Citation: Xie D, Lu PL, Xu W, You JY, Bi XG, Xian Y. Correlation of serum albumin level on postoperative day 2 with hospital length of stay in patients undergoing emergency surgery for perforated peptic ulcer. World J Gastrointest Surg 2023; 15(7): 1434-1441
- URL: https://www.wjgnet.com/1948-9366/full/v15/i7/1434.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i7.1434
As an acute complication of peptic ulcer disease, perforated peptic ulcer (PPU) is clinically characterized by acute abdomen and is a serious and life-threatening condition that requires prompt diagnosis and treatment. It occurs when an ulcer in the stomach or duodenum erodes through the wall of the organ, causing leakage of digestive juices into the abdominal cavity. This can lead to peritonitis-a severe infection of the abdominal lining which can be fatal if left un
The causes of PPU are multifactorial, with Helicobacter pylori infection and nonsteroidal anti-inflammatory drugs being the most common culprits[2]. Patients with this condition typically present with sudden onset of severe abdominal pain, vomiting, and signs of shock such as low blood pressure. PPU is usually diagnosed based on clinical presentations, imaging results, and laboratory tests. After the diagnosis, immediate surgical intervention is required to repair the perforation and prevent further spread of infection. Administration of antibiotics is also recommended to treat existing infection[3]. Delayed treatment can result in serious complications and a mortality rate of up to 30%. Multiple studies have investigated the risk factors for PPU-associated mortality and complications, pointing out that hypoalbuminemia can independently influence the mortality and occurrence of gastrointestinal leakage[4,5]. Preoperative high white blood cell count and platelet/lymphocyte ratio, and low lymphocyte count have been suggested to be associated with prolonged hospital length of stay (HLOS) following PPU repair. Operation interval > 12 h has also been shown to be a risk factor for extended HLOS in PPU patients[6]. However, no relevant study has reported the correlation of SA level with HLOS in such patients.
By collecting the clinical data of PPU patients who were referred to our department for treatment after emergency surgery, this paper retrospectively analyzed the correlation of SA level with HLOS.
This study retrospectively selected PPU patients who received emergency surgery and postoperative treatment in the Lingnan Hospital, the Third Affiliated Hospital of Sun Yat-sen University from December 2012 to September 2021.
Inclusion criteria: (1) Patients who had undergone laparoscopic surgery, gastrectomy, laparotomy or laparoscopic conversion to laparotomy for gastric perforation repair or duodenal perforation repair; (2) Patients with pathologically confirmed ulcer perforation; and (3) Patients whose participation in the study had been reviewed and approved by the Hospital Medical Ethics Committee.
Exclusion criteria: (1) Patients with a history of drug or alcohol dependence; (2) Patients with mental disorders; and (3) Patients with malignant tumors.
Clinical and laboratory data of the patients were collected for retrospective analyses. The data included sex, age, perforation site, perforation diameter, operation method, operation time, complications (pulmonary infection, localized ascites, pleural effusion), HLOS, duration of intensive care unit (ICU) stay, as well as preoperative blood routines, albumin (ALB) levels on preoperative, the 1st, 2nd, and 3rd postoperative days, and ALB infusion. The patient groups were determined based on their HLOS using previously published criteria[7-9]. Patients with HLOS ≤ 7 d or > 7 d were assigned to the ≤ 7-d group or > 7-d group, respectively.
The Excel software was utilized for data entry of the selected patients, and SPSS 26.0 was used for statistical analysis and data processing. Normally distributed quantitative data were expressed as mean ± SD, and were compared between groups with a t-test. Quantitative data that did not follow normal distribution were represented by medians (upper and lower quartiles) and compared between groups with a rank sum test. Count data were expressed as frequencies and percentages, and inter-group differences were analyzed using either the four-table χ2 test or Fisher's exact test. The significance level was set at α = 0.05, and P < 0.05 indicated statistically significant differences. Univariate logistic analysis was performed on all variables, and those with P < 0.1 were further subjected to multivariate logistical analysis using enter method to screen independent variables. The odds ratio (OR) value [95% confidence interval (CI)] was calculated to determine the relative risk, and receiver operating characteristic (ROC) curves were plotted to identify the optimal cutoff based on the Youden index.
From December 2012 to September 2021, a total of 37 patients received emergency surgery for PPU were admitted to our department, including 29 males and 8 females. The age range of the patients was 20-95 years old, with a mean age of 58.24 years. Among them, 33 patients had gastric ulcers and 4 patients had duodenal ulcers. The median HLOS was 9 d, and HLOS of 7 d was used as the cutoff value. Thus, 8 patients with HLOS ≤ 7 d were included in the ≤ 7-d group with a median HLOS of 7 d, while the remaining 29 patients with HLOS > 7 d were in the > 7-d group with a median HLOS of 10 d. One patient died due to myocardial infarction during hospitalization with an HLOS of 2 d, and another patient developed hemiplegia and coma. However, the family refused head computed tomography, and the patient was voluntarily discharged after 5 d of hospitalization.
In the ≤ 7-d group, 3 patients underwent laparotomy (2 cases of gastric perforation repair, and 1 duodenal perforation repair), and 5 patients underwent laparoscopic surgery (4 cases of laparoscopic gastric perforation repair, 1 case of abdominal lavage for no perforation found). In the > 7-d group, 14 patients underwent laparotomy (12 cases of gastric perforation repair, and 1 duodenal repair, one patient with perforation in both the anterior and posterior walls of the gastric antrum and pylorus, closely adhered to the head of the pancreas, underwent major gastrectomy + Bi II gastrojejunostomy + jejunostomy). Besides, 13 patients underwent laparoscopic surgery (12 cases of gastric perforation repair, and 1 duodenal perforation repair), while 2 patients underwent laparoscopic conversion to open surgery (1 patient with gastric antrum perforation due to repair operation for severe abdominal adhesions and 1 patient undergoing laparoscopic exploration conversion to open surgery for the repair of duodenal ulcer + cholecystostomy + gastrostomy).
In terms of complications, 8 cases were observed to have pleural effusion (1 case in the ≤ 7-d group; 7 cases in the > 7-d group, of which 3 cases underwent thoracentesis). Five patients developed localized perihepatic effusion located in different areas, one case was observed in the ≤ 7-d group, and the remaining four were in the > 7-d group. Four of the five patients underwent puncture and drainage with color Doppler ultrasound technology.
Retrospective data indicated that not all patients were tested for ALB levels. However, ALB levels were measured before surgery, on the first (D1), second (D2), and third (D3) postoperative days in most patients. Specifically, 35 patients had their ALB levels measured before surgery, 26 patients on D1, 30 patients on D2, and 28 patients on D3. In the > 7-d group, 2 patients did not receive human ALB infusion due to an ALB level over 35 g/L, while other patients received ALB infusion based on their ALB levels and economic status. See detailed information in Table 1.
| ≤ 7-d group (n = 8) | > 7-d group (n = 29) | P value | |
| Age | 54.38 ± 27.25 | 59.31 ± 18.433 | 0.551b |
| Sex | 0.332c | ||
| Female | 3 (37.5) | 5 (17.2) | |
| Male | 5 (62.5) | 24 (82.8) | |
| Perforation site | 1c | ||
| Stomach | 7 (87.5) | 26 (89.7) | |
| Duodenum | 1 (12.5) | 3 (10.3) | |
| Treatment time | 47 (1, 720) | 47 (1, 168) | 0.67a |
| Surgical approach | 0.811c | ||
| Open abdomen | 3 (37.5) | 14 (48.3) | |
| Laparoscopy | 5 (62.5) | 13 (44.8) | |
| Laparoscopic laparotomy | 0 | 2 (6.9) | |
| Piercing Diameter (cm) | 0.9 ± 0.5 | 1 (0.5, 1.1) | 0.718a |
| Operation time (min) | 94 ± 22 | 120 (82, 145) | 0.133a |
| Empyema | 0.701c | ||
| Little-medium | 3 (37.5) | 14 (48.3) | |
| Many - a lot | 5 (62.5) | 15 (51.7) | |
| ICU length of stay (d) | 1.8 ± 1.5 | 1 (0.6, 2.5) | 0.763a |
| Lung infection | 4 (50) | 13 (44.8) | 1c |
| Pleural effusion | 1 (12.5) | 7 (24.1) | 0.655c |
| Localized ascites | 1 (12.5) | 4 (13.8) | 1c |
| Preoperative leukocytes (× 109/L) | 13.94 ± 5.22 | 12.32 ± 5.52 | 0.463b |
| Preoperative centriocytes (× 109/L) | 12.43 (6.47, 16.89) | 10.55 ± 5.26 | 0.483a |
| Preoperative lymphocytes (× 109/L) | 0.86 ± 0.46 | 1.17 ± 0.73 | 0.255b |
| Preoperative platelets (×109/L) | 268 ± 135 | 230 (197, 315) | 0.543a |
| Preoperative N/LR | 18.07 ± 10.84 | 8.51 (5.8, 17.57) | 0.097a |
| Preoperative P/LR | 497.20 ± 515.11 | 303.08 ± 198.75 | 0.328b |
| Albumin (preoperative, g/L) (n, mean ± SD) | 7 (39.3 ± 6.3) | 28 (39.9 ± 5.1) | 0.778b |
| Albumin (D1, g/L) (n, mean ± SD) | 6 (32.2 ± 5.1) | 20 (30.6 ± 3.4) | 0.379b |
| Albumin (D2, g/L) (n, mean ± SD) | 7 (37.7 ± 3.7) | 23 (32.6 ± 3.3) | 0.009b |
| Albumin (D3, g/L) (n, mean ± SD) | 4 (38.6 ± 6.1) | 24 (33.6 ± 2.8) | 0.201b |
No significant differences were observed between the two groups in terms of age, sex, perforation site, visit time, operation method, perforation diameter, operation time, empyema, ICU stay, complications (pulmonary infection, pleural effusion, localization) and preoperative leukocytes, centrocytes, lymphocytes, platelets, neutrophil/lymphocyte ratio (N/LR), platelet/lymphocyte ratio (P/LR), and ALB levels (preoperative D1 and D3), with P values greater than 0.05 (see Table 1 for details). However, the ALB level on postoperative D2 was significantly higher in the ≤ 7-d group (37.7 g/L) than that in the > 7-d group (32.6 g/L), with statistical significance (P = 0.009).
Univariate logistic analysis was performed on the above indicators. The ALB level on postoperative D2 and D3 and the preoperative N/LR showed P values < 0.1, with the P values being 0.015, 0.043, and 0.01, respectively. Following the overlap of clinical significance of ALB on postoperative D2 and D3, t test was conducted and found no statistical inter-group difference on D3. Therefore, the ALB on postoperative D2 and the preoperative N/LR were further analyzed using the multivariate binary logistic model.
The multivariate analysis identified ALB level on postoperative D2 (OR = 1.535, 95%CI: 1.033-2.283, P = 0.034) as a risk factor for HLOS ≤ 7 (Table 2), and the ALB level on postoperative D2 (OR = 0.651, 95%CI: 0.438-0.968, P = 0.034) as a protective factor for HLOS > 7 d (Table 3).
| Regression coefficient B | SE | Relative risk | 95%CI | P value | |
| Albumin (D2) | -0.429 | 0.202 | 1.535 | 1.033-2.283 | 0.034 |
| Preoperative N/LR | -0.029 | 0.068 | 1.029 | 0.901-1.175 | 0.673 |
| Regression coefficients B | SE | Relative risk | 95%CI | P value | |
| Albumin (D2) | 0.429 | 0.202 | 0.651 | 0.438-0.968 | 0.034 |
| Preoperative N/LR | 0.029 | 0.068 | 0.972 | 0.851-1.11 | 0.673 |
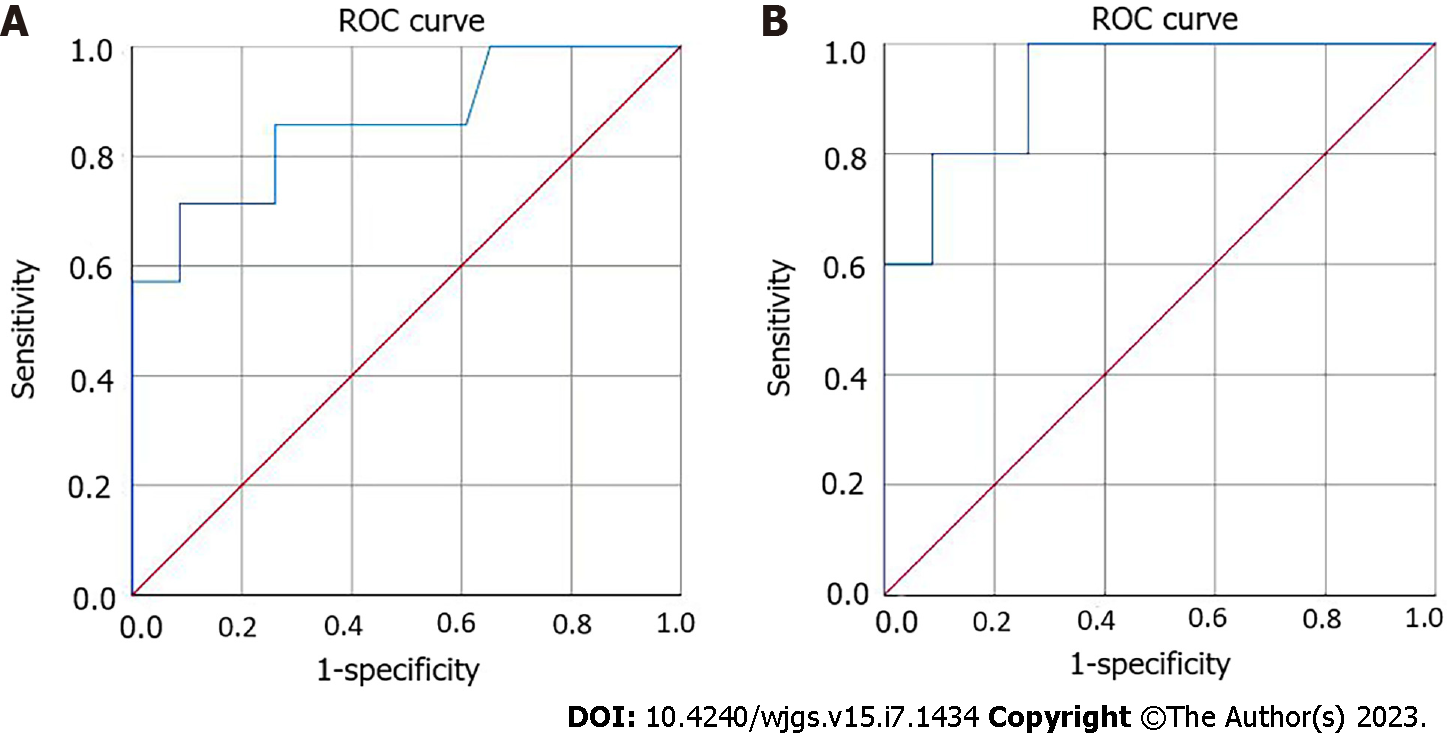
To evaluate the predictive value of ALB level on postoperative D2 for hospital stay ≤ 7 d, ROC curve was plotted and exhibited an area under the curve (AUC) of 0.86 (P = 0.004) (Figure 1A). When the cut-off value was 30.6 g/L, the Youden index value was the largest, which was 0.348. The sensitivity and specificity of ALB on postoperative D2 in predicting hospital stay ≤ 7 d were 100% and 34.8%, respectively, and the positive and negative predictive values were 31.8% and 100%, respectively.
After excluding death due to myocardial infarction and voluntary discharge due to hemiplegia and coma during hospitalization, the median HLOS of the remaining 35 patients was 10 (8, 12) d. Among them, there were 6 cases in the ≤ 7-d group with a median HLOS of 7 (7, 7) d, and 29 cases in the > 7-d group with a median HLOS of 10 (8, 15) d. The ALB levels on postoperative D2 were detected in 5 cases and 23 cases in the ≤ 7-d and > 7-d groups, respectively, and these values followed a normal distribution. The mean values were 38.5 ± 2.6 and 32.6 ± 3.3, respectively, with a significant difference between the two groups (P = 0.001). No significant differences were observed in other indicators between the two groups (all P > 0.05). In the univariate logistic analysis, only the P values of the ALB levels on postoperative D1 and D2 and the preoperative N/LR were less than 0.1, which were 0.075, 0.031, and 0.06, respectively. However, because of the overlap of the clinical significance of ALB levels on postoperative D1 and D2, only the ALB level on postoperative D2 and preoperative N/LR were further analyzed using a multivariate binary logistic model, with P values being 0.047 and 0.86, respectively. The ALB level on postoperative D2 was found to be a protective factor for HLOS > 7 d (OR = 0.466, 95%CI: 0.22-0.989, P = 0.047), and a risk factor for HLOS ≤ 7 d (OR=2.146, 95%CI: 1.011-4.553, P = 0.047). The ROC curve was plotted with an AUC of 0.93 (P = 0.003) (Figure 1B). The largest Youden index value of 0.739 was obtained when the cut-off value was 35.2 g/L. The sensitivity, specificity, positive predictive value, and negative predictive value of ALB level on postoperative D2 in predicting hospital stay ≤ 7 d were all 100%, 73.9%, 45%, and 100%, respectively.
Previous studies have shown[1,10,11,14] that hypoalbuminemia is a risk factor for 30- and 90-d, as well as 1- and 2-year mortality in patients with PPU. In addition, hypoalbuminemia is indicated to elevate the risk of PPU complicated by gastrointestinal leakage[12,15]. So how does hypoalbuminemia affect the HLOS? This study collected the clinical data and blood results of 37 PPU patients referred to our department for postoperative care and treatment from December 2012 to September 2021. Referring to previous studies on the HLOS in patients undergoing (laparoscopic and laparoscopic) operations for PPU[7,9], and the time point selected by Al -Yahri O et al[8], we grouped the patients with a HLOS cut-off value of 7 d. Our results showed that only the ALB level on postoperative D2 was significantly different between the two groups, and no difference was identified in the other indicators. Although Al -Yahri O et al[8] reported that preoperative high white blood cell count and platelet/lymphocyte ratio, and low lymphocyte count were associated with extended HLOS, no significant statistical differences were found in these indexes in this study, which may be due to the small number of cases (n = 37).
The present study aimed to investigate the association between SA level and HLOS in patients with PPU following emergency surgery. Our results indicated that the SA level on postoperative D2 was significantly associated with prolonged HLOS in PPU patients. Specifically, binary logistic analysis suggested that SA on postoperative D2 was a protective factor against prolonged HLOS.
Furthermore, we conducted ROC curve analysis to determine the predictive value of SA level on postoperative D2 for hospital stay ≤ 7 d. The AUC was found to be 0.86, indicating good accuracy in predicting short HLOS. The Youden index value was the largest when the cut-off value was 30.6 g/L, with a sensitivity, specificity, and positive and negative predictive values of 100%, 34.8%, 31.8%, and 100%, respectively.
After excluding death due to myocardial infarction and voluntary discharge due to hemiplegia and coma during hospitalization, we further analyzed the ROC curve and found that the AUC was 0.93. When the cut-off value for ALB on postoperative D2 was set at 35.2 g/L, the Youden index value was the largest at 0.739, with a sensitivity and specificity, and positive and negative predictive values of 100%, 73.9%, 45%, and 100%, respectively. In addition, our study also found that patients with hypoalbuminemia had increased risk for adverse outcomes. Thorsen K et al. reported that hypoalbuminemia ≤ 37 g/L was associated with an 8.7-fold increased risk of 30-d mortality with an AUC of 0.78[1]. Moreover, Prakash et al[3] reported that patients with ALB level < 3.5 g/dL were at an increased risk of complications as compared with those with ALB level > 3.5 g/dL. Lund et al[14]. demonstrated that ALB < 3.5 g/dL was a risk factor for gastrointestinal leakage in PPU patients. These findings, combined with our study results, suggest that SA levels should be monitored before and after surgery, and SA supplementation may help reduce HLOS and improve patient outcomes. It is also suggested that a cut-off of 35.2 g/L may be more appropriate than 30.6 g/L, which was proposed by previous studies as it exhibited higher sensitivity and specificity[14,16].
Previously, studies have reported that for patients with bleeding peptic ulcer with ALB < 3 g/dL, infusion of human SA can shorten the HLOS of patients[13,17,18]. In our study, two patients with ALB levels above 35 g/L did not receive ALB infusion, yet their total HLOS was still longer than 7 d. This finding suggests that further prospective controlled trials are required to validate whether human SA infusion can shorten HLOS in PPU patients.
The present study has several limitations that should be considered when interpreting the results. The relatively small sample size with only 37 cases collected over 9 years may limit the generalizability of the findings to other populations. Additionally, some patients were not measured for SA level, which may affect the statistical results. Therefore, a multicenter study with a larger sample size is needed to conduct in-depth analysis and validate the results.
In conclusion, monitoring SA levels on postoperative D2 and necessary supplementation may contribute significantly to shortening HLOS in PPU patients following emergency surgery. Additional research is needed to investigate the potential beneficial effects of human ALB infusion on patient outcomes.
Perforated peptic ulcer (PPU) is a medical emergency that requires immediate surgical intervention. Despite significant advances in surgical techniques, postoperative complications and prolonged hospitalization can still occur and impact patient morbidity and healthcare costs. Serum albumin (SA) level, a widely used marker of nutritional status, has shown to be a reliable predictor of postoperative outcomes in various surgical procedures. However, little is known about its relationship with hospital length of stay (HLOS) in PPU patients undergoing emergency surgery.
PPU is a common and potentially life-threatening medical emergency that requires prompt surgical intervention. While significant advances have been made in surgical techniques, postoperative complications and prolonged hospitalization remain a challenge. Malnutrition and hypoalbuminemia are common in PPU patients and have been associated with unfavorable postoperative outcomes. SA level, a widely used marker of nutritional status, has shown to be a valuable predictor of postoperative outcomes in various surgical procedures. However, its relationship with HLOS in PPU patients undergoing emergency surgery is not well understood. Therefore, this study aims to fill this gap and potentially provide insights into optimizing perioperative care for PPU patients, improving outcomes, and reducing healthcare costs.
The objective of this study is to investigate the correlation between SA levels on postoperative day 2 and HLOS in patients undergoing emergency surgery for PPU. Specifically, the study aims to determine whether lower SA levels on postoperative day 2 are associated with longer HLOS in PPU patients. The findings of this study will provide valuable insights into optimizing perioperative care for PPU patients, potentially reducing the burden of prolonged hospitalization and improving patient outcomes in this high-risk patient population.
In this study, we conducted a retrospective analysis of clinical baseline data, blood routine tests, and SA levels of patients who underwent emergency surgery for PPU at the Lingnan Hospital, the Third Affiliated Hospital of Sun Yat-sen University between December 2012 and September 2021. Patients were categorized based on their HLOS into two groups: Those with HLOS of ≤ 7 d and those with HLOS of > 7 d. Relevant indices were analyzed using SPSS 26.0 software.
On postoperative day 2, the ≤ 7-d group had significantly higher SA levels than the > 7-d group (37.7 g/L vs 32.6 g/L, P < 0.05). We found that the SA level on postoperative day 2 was a protective factor for patients with an HLOS > 7 d (OR = 0.629, P = 0.015). The cut-off value for SA on postoperative day 2 was 30.6 g/L, with an AUC of 0.86 and a negative predictive value of 100% for predicting an HLOS of ≤ 7 d.
Our study, which investigated the correlation between SA levels on postoperative day 2 and HLOS in patients undergoing emergency surgery for PPU, found that lower SA levels on postoperative day 2 were associated with longer HLOS in PPU patients. We also found that SA level on postoperative day 2 was a protective factor for patients with an HLOS greater than 7 d. Furthermore, we established a cut-off value for SA level on postoperative day 2 that effectively predicts an HLOS of ≤ 7 d. Our findings highlight the potential benefits of monitoring SA levels during the perioperative period of PPU patients, which may improve patient outcomes, reduce healthcare costs, and optimize perioperative care strategies for this high-risk population.
The correlation between SA levels and HLOS in patients undergoing emergency surgery for PPU remains an important area of research. Future studies could focus on examining the association between SA levels and postoperative complications, such as infection, sepsis, and mortality. Additionally, further research could investigate the underlying mechanisms through which SA levels influence HLOS in these patients. This could include exploring the role of albumin in modulating inflammation, oxidative stress, and wound healing. A better understanding of these mechanisms may provide new therapeutic targets for improving outcomes in PPU patients. Finally, future studies could examine the feasibility and effectiveness of interventions aimed at optimizing SA levels in this patient population, including nutritional support, perioperative albumin infusion, and other interventions. Overall, continued research in this area has the potential to improve patient outcomes and identify new approaches to perioperative care in PPU patients.
| 1. | Thorsen K, Søreide JA, Søreide K. What is the best predictor of mortality in perforated peptic ulcer disease? A population-based, multivariable regression analysis including three clinical scoring systems. J Gastrointest Surg. 2014;18:1261-1268. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 63] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 2. | Tang JT, Xie WB. [Prevention and treatment of suture leakage after perforated peptic ulcer repair]. Guoji Waikexue Zazhi. 2019;46:652-655. [DOI] [Full Text] |
| 3. | Prakash KRB, Mohan M, Patil S. Pre-operative serum albumin and body mass index as predictors of post-operative morbidity and mortality in perforation peritonitis secondary to peptic ulcer disease. Int Surg J. 2021;8:589. [DOI] [Full Text] |
| 4. | Møller MH, Adamsen S, Thomsen RW, Møller AM. Preoperative prognostic factors for mortality in peptic ulcer perforation: a systematic review. Scand J Gastroenterol. 2010;45:785-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 71] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Lin CP. [Influence of laparoscopic repair on complications and rehabilitation of patients with perforated peptic ulcer]. Zhongguo Yaowu Yu Linchuang. 2019;19:2584-2586. [DOI] [Full Text] |
| 6. | Alhaj Saleh A, Esquivel EC, Lung JT, Eaton BC, Bruns BR, Barmparas G, Margulies DR, Raines A, Bryant C, Crane CE, Scherer EP, Schroeppel TJ, Moskowitz E, Regner J, Frazee R, Campion EM, Bartley M, Mortus J, Ward J, Almekdash MH, Dissanaike S. Laparoscopic omental patch for perforated peptic ulcer disease reduces length of stay and complications, compared to open surgery: A SWSC multicenter study. Am J Surg. 2019;218:1060-1064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Hermansson M, Staël von Holstein C, Zilling T. Surgical approach and prognostic factors after peptic ulcer perforation. Eur J Surg. 1999;165:566-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 52] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Al-Yahri O, Saafan T, Abdelrahman H, Aleter A, Toffaha A, Hajjar M, Aljohary H, Alfkey R, Zarour A, Al-Mudares S, El-Menyar A. Platelet to Lymphocyte Ratio Associated with Prolonged Hospital Length of Stay Postpeptic Ulcer Perforation Repair: An Observational Descriptive Analysis. Biomed Res Int. 2021;2021:6680414. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Sanabria A, Villegas MI, Morales Uribe CH. Laparoscopic repair for perforated peptic ulcer disease. Cochrane Database Syst Rev. 2013;CD004778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Li W Li N, Li SL. [Correlation between albumin level and acute kidney injury after major abdominal surgery in critically ill patients]. Zhonghua Weizhongbing Jijiu Yixue. 2021;33:955-961. [RCA] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 11. | Yan ZZ, Wang JX, Chai JS, Gao F, Xing J. [Application of laparoscopy in perforated peptic ulcer surgery]. Zhongguo Yaowu Yu Linchuang. 2018;18:2. [DOI] [Full Text] |
| 12. | Ni ZZ, Wang S, Zhu LC, Huang CS, Ge BJ, Huang Q. [Long-term efficacy of perforated peptic ulcer repair]. Zhongguo Putong Waike Zazhi. 2021;36:47-49. [DOI] [Full Text] |
| 13. | Cheng HC, Chang WL, Chen WY, Tsai YC, Yeh YC, Sheu BS. Intravenous albumin shortens the duration of hospitalization for patients with hypoalbuminemia and bleeding peptic ulcers: a pilot study. Dig Dis Sci. 2013;58:3232-3241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Thorsen K, Søreide JA, Søreide K. Long-Term Mortality in Patients Operated for Perforated Peptic Ulcer: Factors Limiting Longevity are Dominated by Older Age, Comorbidity Burden and Severe Postoperative Complications. World J Surg. 2017;41:410-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Lund S, Chauhan KK, Zietlow J, Stephens D, Zietlow S, Strajina V, Turay D, Zielinski M. Risk Factors for Gastrointestinal Leak after Perforated Peptic Ulcer Disease Operative Repair. Am Surg. 2021;87:1879-1885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 16. | Lv GW. [Effect of laparoscopic gastric perforation repair on postoperative gastrointestinal function and pain in elderly patients with perforated peptic ulcer]. Xiandai Zhenduan Yu Zhiliao. 2020;31:1944-1946. |
| 17. | Hu L, Cai SS, Tang XL Yang J. [A retrospective study on the effect of human serum albumin supplementation in patients with hypoalbuminemia after abdominal surgery]. Zhongguo Yaoye. 2020;29:81-83. [DOI] [Full Text] |
| 18. | Wang CY, Liang Y, Xie WB. [A brief discussion on the application status, causes and countermeasures of laparoscopic repair of peptic ulcer perforation]. Guoji Waikexue Zazhi. 2021;48:649-654. [DOI] [Full Text] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kinami S, Japan; Kong SH, South Korea S-Editor: Ma YJ L-Editor: A P-Editor: Yu HG