Published online Jun 27, 2023. doi: 10.4240/wjgs.v15.i6.1211
Peer-review started: January 25, 2023
First decision: February 21, 2023
Revised: March 14, 2023
Accepted: April 17, 2023
Article in press: April 17, 2023
Published online: June 27, 2023
Processing time: 140 Days and 23.8 Hours
Difficult bile duct intubation is a big challenge for endoscopists during endoscopic retrograde cholangiopancreatography (ERCP) procedure. We report a case of percutaneous transhepatic cholangial drainage (PTCD)-guided methylene blue for fistulotomy using dual-knife for bile duct intubation.
A 50-year-old male patient had developed obstructive jaundice, and ERCP procedure need to be performed to treat the obstructive jaundice. But intubation cannot be performed if the duodenal papilla cannot be identified because of previous surgery for a perforated descending duodenal diverticulum. We used PTCD-guided methylene blue to identify the intramural common bile duct before dual-knife fistulotomy, and bile duct intubation was successfully completed.
The method that combing methylene blue and dual-knife fistulotomy to achieve bile duct intubation during difficult ERCP is safe and effective.
Core Tip: We report a case of difficult bile duct intubation during endoscopic retrograde cholangiopancreatography (ERCP) procedure. We introduce the clinical features, findings of ERCP, and response to treatment in this male patient.
- Citation: Tang BX, Li XL, Wei N, Tao T. Percutaneous transhepatic cholangial drainage-guided methylene blue for fistulotomy using dual-knife for bile duct intubation: A case report. World J Gastrointest Surg 2023; 15(6): 1211-1215
- URL: https://www.wjgnet.com/1948-9366/full/v15/i6/1211.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i6.1211
Endoscopic retrograde cholangiopancreatography (ERCP) has currently become an essential diagnostic and treatment method for pancreatobiliary diseases. However, the failure rate of routine bile duct intubation during ERCP is 10%[1,2]. Methylene blue can be used to identify the duodenal papilla for bile duct intubation[3], and dual-knife fistulotomy is an effective and safe method for accessing the bile duct[4]. We combined these two methods in a patient undergoing surgery for a perforated descending duodenal diverticulum.
A 50-year-old male patient with developed jaundice was transferred to our outpatient service in October 2022.
The patient underwent surgery for a perforated descending duodenal diverticulum. He had duodenal diverticulum resection, partial small bowel resection, cholecystostomy, and jejunostomy. After the cholecystostomy tube was removed, obstructive jaundice appeared to develop.
In medical history the patient alleged healthy and denied a history of heart illness and inspiratory illness.
From the patient’s medical history, we precluded a history of allergies, asthma, and alcoholism. His father and mother had no hereditary diseases and were all healthy.
On admission we performed a physical examination on the patient, and the result revealed yellow staining of the skin and sclera, but there were no enlarged superficial lymph nodes. There were no abnormal cardiopulmonary and abdominal examinations.
Laboratory results revealed that the blood count of the patient was normal, the patinet’s renal function, carcinoembryonic antigen, cancer antigen 125, cancer antigen 19-9, carcinoembryonic antigen, and alpha-fetoprotein values were also normal. Liver fibrosis test of the patient was normal, and the levels of immunoglobulins immunoglobulin (Ig) A, IgM, and IgG were also normal. As for the levels of serum type III procollagen, type IV collagen, laminin, and hyaluronic acid, all normal. But the liver function was abnormal and total bilirubin was 130.8 µmol/L, direct bilirubin was 98.5 µmol/L, and indirect bilirubin was 32.3 µmol/L.
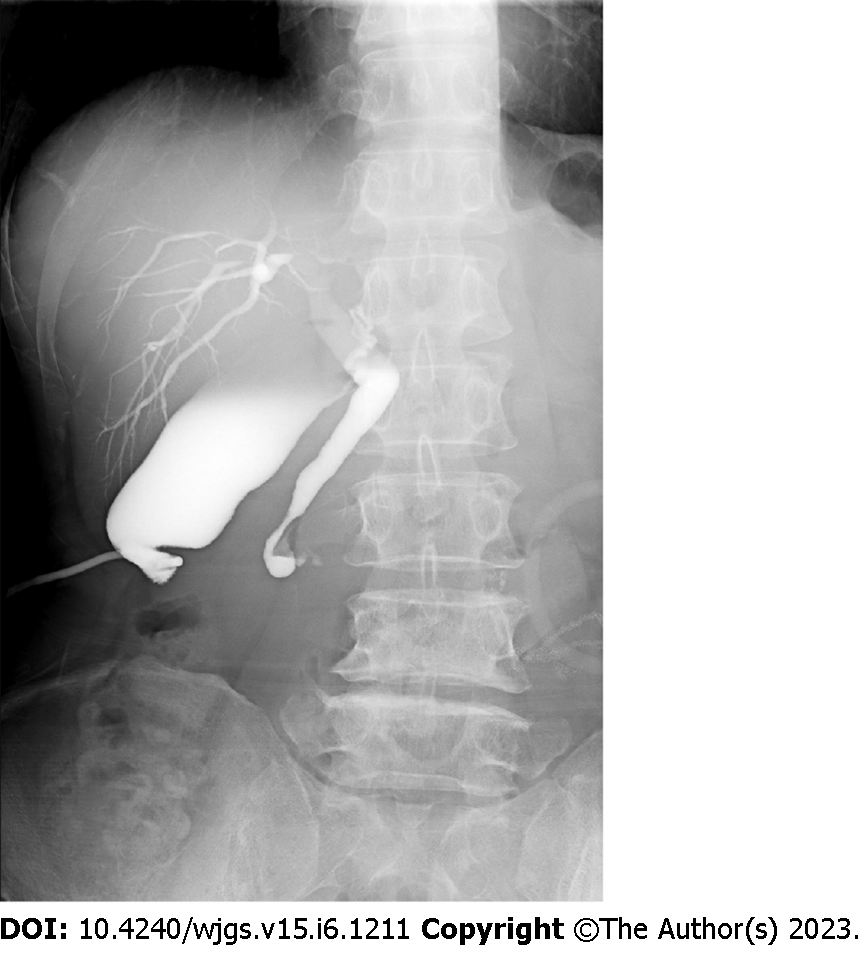
Postoperative cholecystostomy tube imaging (Figure 1) revealed slight dilation of the common bile duct and a small amount of contrast agent flowing into the duodenum.
The patient was diagnosed as obstructive jaundice.
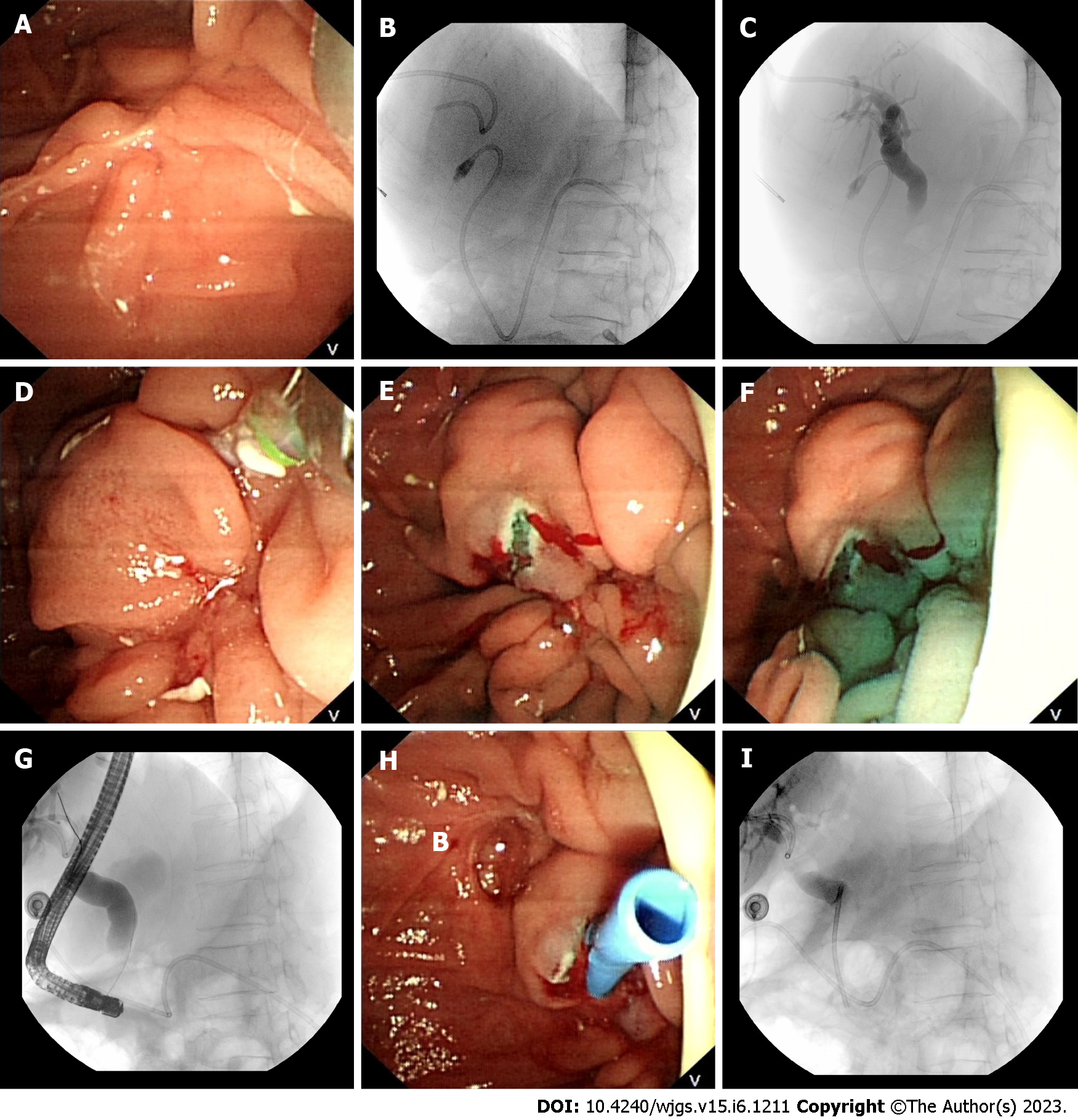
The patient was discharged after PTCD drainage. The daily drainage volume was 2500-2800 mL but the PTCD drainage tube could not be clamped outside of the hospital. ERCP was performed for internal drainage in the bile duct. During ERCP procedure, descending duodenal scarring was observed and the papilla could not be identified after repeated attempts (Figure 2A). Similarly, no ectopic papilla was observed. Insertion of a PTCD tube into the duodenum via a guidewire was attempted but we could not insert the guidewire into the common bile duct after repeated adjustments (Figures 2B and C). After injecting a combination of ioversol and methylene blue (Jichuan Pharmaceutical Group Co. LTD, Jiangsu Province, China) via the PTCD tube, pale blue-colored duodenal scar protrusions were observed, which were identified as the intramural common bile duct (Figure 2D). We used a dual-knife (KD-650 L; Olympus Medical Systems) to perform layer-by-layer resection. As a result, large amount of ioversol and methylene blue could be seen flowing out (Figure 2E and F). After routine intubation of the stoma was successful, an 8.5 Fr × 5.0 cm plastic stent was inserted and patent ioversol and methylene blue flow was observed (Figure 2G-I).
After the endoscopic procedure, the patient’s jaundice and liver function was relieved after 3 wk. Laboratory tests performed in December 2022 revealed that total bilirubin, direct bilirubin and indirect bilirubin was 31.8 µmol/L, 18.9 µmol/L, and 12.9 µmol/L respectively. Until November 2022, the patient was still undergoing follow-up.
A possible explanation for the increasing success rate of ERCP procedures is attributed to the excellent ERCP supporting facilities concerning ultrasonography and duodenoscopic viewing, and the application of adjunctive intubation methods to increase intubation success, reduce complications, and alleviate patient pain[5]. However, questions such as how the native papilla or biliopancreatoenteric anastomosis can be identified and cannulated were still challenging for endoscopists. The position of the native papilla in surgically altered anatomy differs greatly from that in the normal anatomy[5].
From the disease history we concluded that surgery was the cause of the obstructive jaundice in this case. As for the treatment of obstructive jaundice, ERCP has a lower incidence of complications and shorter hospital stays and a lower cost than other methods such as PTCD.
During ERCP, the duodenal papilla is usually identified using endoscope landmarks, such as an oral protrusion, duodenal folds, and a small belt formed by the anal columns. Occasionally, the duodenal papilla cannot be identified. Since our patient had undergone perforated descending duodenal diverticulum surgery, the duodenal papilla could not be located. After PTCD guidewire insertion failed, methylene blue was injected into the PTCD tube and visible protrusions in the intramural common bile duct were visualized as blue surfaces. This technique improved visualization of the intramural common bile duct and reduced the risk of complications due to inaccurate intramural common bile duct identification. After visualizing the position of common bile duct, we selected a dual-knife for fistulotomy because the front end of the dual-knife’s sheath was as short as 2 mm. The short knife tip of the dual knife can be directly applied to the mucosal surface to improve control of the incision depth and prevent injury to the posterior sphincter wall of the common bile duct. Therefore, dual-knife is safer than needle knife in our experience. Due to the unique design of the expansive tip, dual-knife can also be used to hook the bile duct to the intestinal cavity for incision, which cannot be achieved with needle knife[7]. We combined methylene blue tracer and dual-knife fistulotomy to successfully complete bile duct intubation and insert a plastic stent in the patient’s bile duct. This enabled internal bile drainage.
The combined use of methylene blue tracer and dual-knife incurs a lower risk and is effective method to achieve bile duct intubation during difficult ERCP.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tsutsumi K, Japan; Yildiz K, Turkey S-Editor: Chen YL L-Editor: A P-Editor: Wu RR
| 1. | Jang SI, Kim DU, Cho JH, Jeong S, Park JS, Lee DH, Kwon CI, Koh DH, Park SW, Lee TH, Lee HS. Primary Needle-Knife Fistulotomy Versus Conventional Cannulation Method in a High-Risk Cohort of Post-Endoscopic Retrograde Cholangiopancreatography Pancreatitis. Am J Gastroenterol. 2020;115:616-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 2. | Bailey AA, Bourke MJ, Williams SJ, Walsh PR, Murray MA, Lee EY, Kwan V, Lynch PM. A prospective randomized trial of cannulation technique in ERCP: effects on technical success and post-ERCP pancreatitis. Endoscopy. 2008;40:296-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 166] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 3. | Gjeorgjievski M, Ghaith G. ERCP after percutaneous cholecystostomy: methylene blue-assisted biliary cannulation for diminutive papilla. Gastrointest Endosc. 2021;93:984-985. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Liu H, Jiang CM, Qu B, Wang ZG. Snare-assisted precutting and dual-knife fistulotomy performed during difficult biliary cannulation in a patient with an ectopic papilla of Vater. J Int Med Res. 2021;49:3000605211035107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 5. | Krutsri C, Kida M, Yamauchi H, Iwai T, Imaizumi H, Koizumi W. Current status of endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy. World J Gastroenterol. 2019;25:3313-3333. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 48] [Cited by in RCA: 67] [Article Influence: 9.6] [Reference Citation Analysis (3)] |
| 6. | Moole H, Bechtold M, Puli SR. Efficacy of preoperative biliary drainage in malignant obstructive jaundice: a meta-analysis and systematic review. World J Surg Oncol. 2016;14:182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 111] [Cited by in RCA: 95] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 7. | Liu F, Liu J, Li Z. New role of the dual knife for precut papillotomy in difficult bile duct cannulation. Dig Endosc. 2013;25:329-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |