Published online May 27, 2023. doi: 10.4240/wjgs.v15.i5.978
Peer-review started: December 10, 2022
First decision: January 3, 2023
Revised: January 9, 2023
Accepted: April 7, 2023
Article in press: April 7, 2023
Published online: May 27, 2023
Processing time: 167 Days and 4.2 Hours
A combination of diseases is a rare phenomenon. Their clinical manifestations can vary, and the diagnosis can be challenging. Intestinal duplication is a rare congenital malformation, whereas retroperitoneal teratoma is a tumor in the retroperitoneal space, derived from the remaining embryonic tissue. There are relatively few clinical findings on adult retroperitoneal benign tumors. It is hard to believe that these two rare diseases can happen to the same person.
A 19-year-old woman complaining of abdominal pain with nausea and vomiting was admitted. Abdominal computed tomography angiography was suggested for invasive teratoma. Intraoperative exploration revealed that the giant teratoma was connected to an isolated intestinal tract in the retroperitoneum. The postoperative pathological examination revealed that mature giant teratoma was present with intestinal duplication. This was a rare intraoperative finding that was successfully treated surgically.
The clinical manifestations of intestinal duplication malformation are various, and difficult to diagnose before the operation. The possibility of intestinal replication should be considered when intraperitoneal cystic lesions are present.
Core Tip: Giant teratoma with intestinal duplication has not been reported yet. Here, we report a case of a 19-year-old woman with giant teratoma and isolated intestinal duplication who complained of abdominal pain with nausea and vomiting; a rare intraoperative finding successfully by surgery.
- Citation: Xiong PF, Yang L, Mou ZQ, Jiang Y, Li J, Ye MX. Giant teratoma with isolated intestinal duplication in adult: A case report and review of literature. World J Gastrointest Surg 2023; 15(5): 978-983
- URL: https://www.wjgnet.com/1948-9366/full/v15/i5/978.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i5.978
Intestinal duplication is a congenital malformation usually observed in pediatric patients[1]. However, its diagnosis in adults is rare, and preoperative diagnosis is difficult, particularly when combined with other diseases[2]. Teratomas are benign neoplasms, that arise from more than one embryonic germ layer. Morphologically, it can be divided into cystic and solid parts. Retroperitoneal teratomas are rare, and, patients often present compression symptoms due to large tumors[3]. A giant teratoma with intestinal duplication has not been reported yet.
A case of a 19-year-old woman admitted to the hospital suffering from abdominal pain for 5 d with nausea and vomiting for 2 d was investigated.
The patient had no obvious inducement of abdominal pain 5 d ago, nausea and vomiting for 2 d, chills, fever, and discomforts such as anus-stopping exhaust and defecation.
The patient had good health history.
The patient and her mother have mental retardation.
Hard round mass with a diameter of about 30 cm in the right abdomen.
Blood analysis revealed potassium level was 2.9 mmol/L (normal range: 3.5-5.5), carcinoembryonic antigen level was 7.16 μg/L (normal range: 0-5), and other tumor markers of the digestive tract and gynecology were normal. Blood routine count, liver function indexes, and renal function markers were also normal.
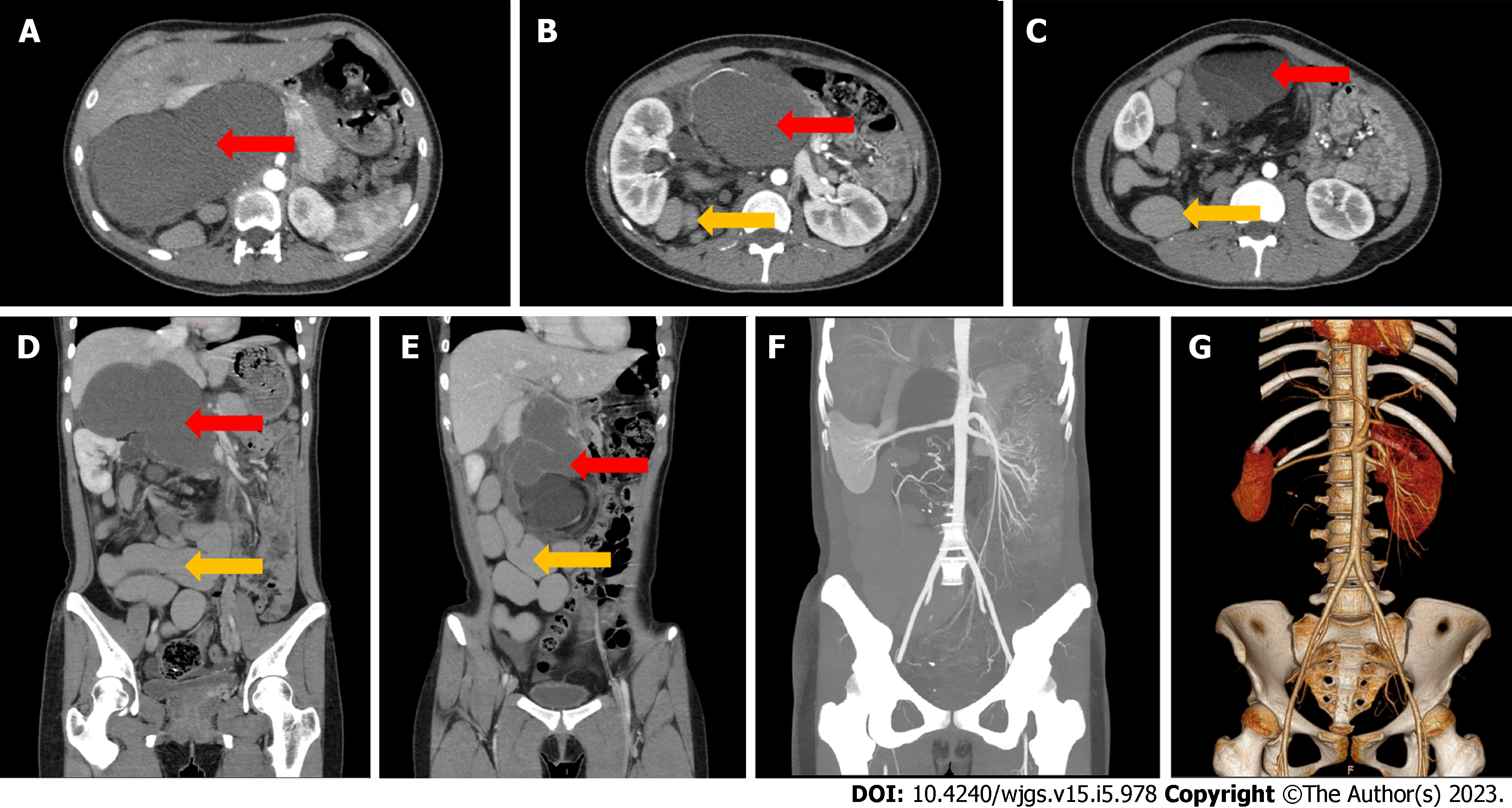
Computed tomography angiography (CTA) showed the presence of a huge (29.6 cm × 17.4 cm × 10.2 cm) mass with mixed density in the right retroperitoneum and irregular tortuous bowel canal (Figures 1A-E). The inferior vena cava was significantly compressed and became thinner and the lumen density was uneven. The right kidney was pushed outward, and the liver was pushed upward. Moreover, the gallbladder was compressed, the right renal vein and inferior vena cava were pushed forward, and the left renal vein, pancreas, gastric antrum, intestine, portal vein and mesenteric vessels were pushed to the left (Figures 1B-G).
The final diagnosis of the presented case was a benign tumor.
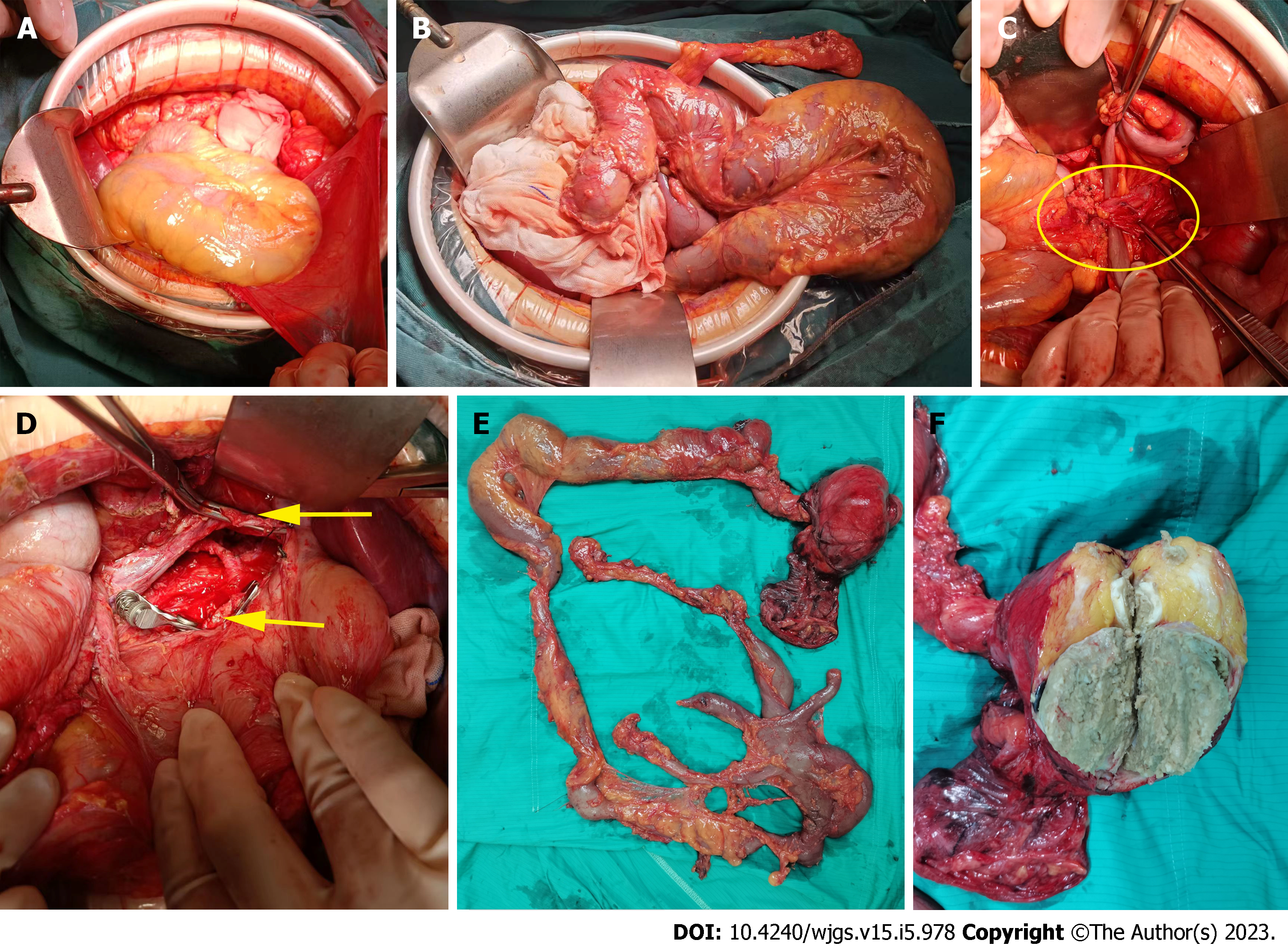
During the exploratory, a huge lobulated retroperitoneal tumor was observed. A jelly-like substance was found inside the tumor. The left renal vein was densely adhered and the tumor was connected to an isolated retroperitoneal intestinal tract (Figures 2A-D). The intestinal tube extended from the back of the inferior vena cava up to the middle peritoneum, and then down to the right retroperitoneum to form another 110 cm long blind end. It had multiple branches, with severe expansion and multiple localized stenosis (Figures 2E and F). It was not connected to the normal digestive tract, and was thus considered a repeat bowel tube. Further, we studied again in the order of stomach, duodenum, jejunum, ileum, cecum, colon and rectum, and found a complete digestive system, confirming isolated intestinal duplication. Intraoperative exploration did not reveal the presence of additional tumors or enlarged lymph nodes. Therefore, we performed retroperitoneal tumor resection, intestinal duplication resection, and left renal vein reconstruction. After resection, a large amount of turbid and viscous intestinal fluid was found through diagnostic puncture of intestinal duplication.
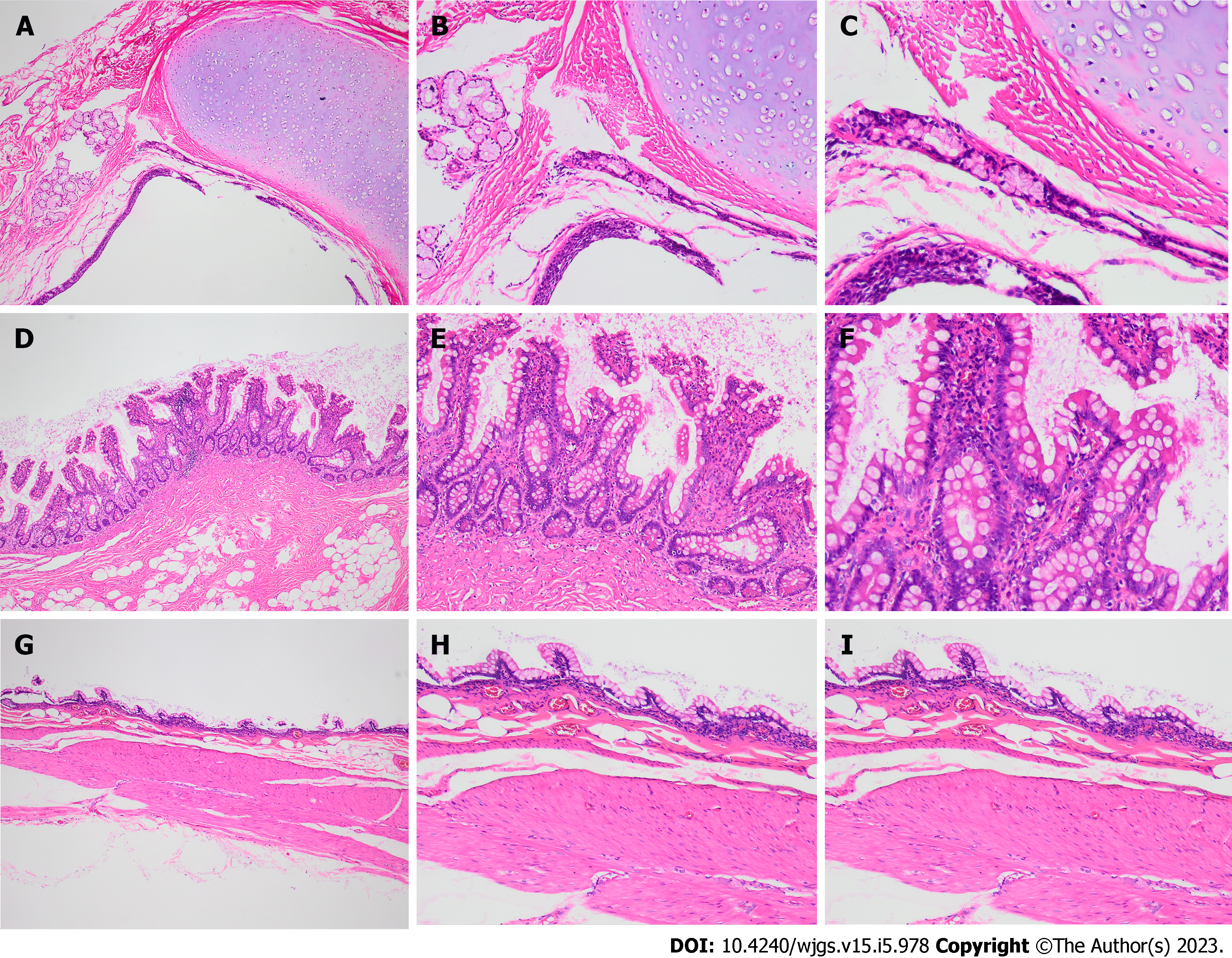
Post-operation the patient was given symptomatic treatment such as anti-infection and nutritional support. After three days, the patient was gradually shifted to a regular diet. One week later, the patient recovered and was discharged from the hospital. The patient was then followed up after a month, showing no discomfort. Specimen showed a lobulated tumor about 9.0 cm × 8.5 cm × 4.5 cm in the distal mucosa of the duplication malformation intestine (Figure 2F). Pathological examination of the excised tissue showed mature teratoma (Figures 3A-C) with intestinal duplication (Figures 3D-I).
Intestinal duplication is a rare congenital disease, more commonly found in children than adults[4]. Although intestinal duplication can affect any part of the digestive tract, 60% occurs in the ileum or cecum. At present, the mechanism of intestinal duplication is unclear. Theories suggest abnormal separation of notochord and gastrula, a vascular insult, persistence of embryonic diverticula, and partial twining[5-7]. Clinically, patients are often treated for abdominal mass, intestinal obstruction, perforation, enteritis, gastrointestinal bleeding, and peritonitis[1,2,8,9]. According to the pathological anatomy, Intestinal duplication can be divided into the intestinal septum, wall cyst, extraintestinal tube, extraintestinal cyst and isolated type. An independent structure without direct connection with the primary intestine characterizes the isolated type.
Teratoma is a germ cell tumor, that occurs in young women and infants. Mature cystic teratomas are the most common, accounting for 98% of teratomas[10]. Teratoma mainly occurs in the gonad, whereas those that occur in other parts are called extragonadal teratomas. They can occur on both sides of the midline of the body, such as the mediastinum, sacrococcygeal, retroperitoneal, and pineal[11]. Extragonadal teratomas can also occur in other parts, including the liver, hepatoduodenal ligament, hepatorenal space, diaphragm and abdominal wall[12].
Intestinal duplication with giant teratoma is rare. In the present study, the patient was prepared for surgical excision for a large retroperitoneal tumor. We found intestinal anatomical structure variation during the operation, and our exploration confirmed that it was an isolated intestinal duplication. Thus, the retroperitoneal tumor and the intestinal duplication were excised entirely. Post-operation, the abdominal CTA was re-read, and combined with the findings during the operation; it was found that the irregular tortuous bowel canal was an isolated intestinal duplication (Figures 1B-E).
Both the patient and her mother had mental retardation; thus, there could be a possibility of familial genetic history. Chromosome and gene testing can further confirm the correlation. However, the case was not been tested for chromosomes and genes in the present study. The possibility of a reabsorbed twin or chimera should also be considered.
Diagnosing a disease before the operation is quite challenging. Barium meal examination can diagnose intestinal duplication only when connected to the intestinal cavity. CT scan shows the focus. However, it is difficult to differentiate the disease from the mesenteric cyst, appendix abscess, and other abdominal cavity cystic lesions. The clinical diagnosis is generally complex, and most of them are diagnosed after laparotomy, similar to our case report. Three-dimensional reconstruction can show the location and scope, complications, related abnormalities, and anatomical relationship with surrounding structures of the repeated malformations. They mostly manifest as well-bounded, thick-walled cystic masses in flat, spherical, or tubular lesions without invading neighboring organs. Thus, it can advance the preoperative diagnostic rate. Therefore, the possibility of intestinal replication should be considered when intraperitoneal cystic lesions are present. Virtual colonoscopy can fully display the intestinal anatomy and lesion site, the anatomy and lesion of the intestinal cavity from both ends of the stenosis and obstruction. The combination of three-dimensional images can also help understand the conditions in the intestinal wall and outside the intestinal cavity, which has unique advantages for the combination of other diseases. Therefore, a virtual colonoscopy can help in the diagnosis of intestinal duplication. In conclusion, the clinical manifestations of intestinal duplication are varied, and preoperative diagnosis is difficult, which requires a combination of various imaging data. For asymptomatic recurrent intestinal malformations, especially for patients with intestinal abnormalities shown on imaging, careful exploration of intestinal conditions during the operation can avoid missed diagnosis.
The only treatment for giant teratoma with isolated intestinal duplication is surgery. For symptomatic intestinal duplication, it is recommended to remove the diseased bowel. For the asymptomatic intestinal duplication, the study believes that timely surgery after diagnosis can avoid complications such as perforation, bleeding, obstruction and malignant changes, and the incidence of complications of early resection is low, and the hospital stay is short. The most common surgical method for intestinal duplication is to remove the diseased intestine. In case of cyst type duplication, simple cyst resection and cyst mucosa stripping can be used. However, if there is communication with normal intestine, adjacent intestine should be removed to ensure complete cyst removal. If other diseases such as tumor and ectopic organ are combined, they should be treated together. However, the specific operation method should be determined according to the specific form of the diseased bowel.
Intestinal duplication with giant teratoma is rare, and preoperative diagnosis is very challenging. Combined with multiple imaging techniques, the diagnosis and its accuracy may can be improved. The anatomic variation is often found during surgery, and surgical resection is the only cure for this disease.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hashimoto K, Japan; Lindner C, Chile S-Editor: Wang JJ L-Editor: A P-Editor: Cai YX
| 1. | Zhou JL, Ge WP, Liu G, Zhu XC, Xiao SJ, Tan YP. A case of intestinal duplication. Arch Dis Child Fetal Neonatal Ed. 2015;100:F313. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Yang JG, Ma DQ, Hao RR, Li CL, Zou LF. Detection of double cystic intestinal duplication by Meckel's scan. Clin Nucl Med. 2009;34:105-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Kawano T, Sugita K, Kedoin C, Nagano A, Matsui M, Murakami M, Kawano M, Yano K, Onishi S, Harumatsu T, Yamada K, Yamada W, Masuya R, Matsukubo M, Muto M, Machigashira S, Nakame K, Mukai M, Kaji T, Ieiri S. Retroperitoneal teratomas in children: a single institution experience. Surg Today. 2022;52:144-150. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Matsukubo M, Muto M, Kedoin C, Matsui M, Murakami M, Sugita K, Yano K, Onishi S, Harumatsu T, Yamada K, Yamada W, Kaji T, Ieiri S. An unusual presentation of intestinal duplication mimicking torsion of Meckel's diverticulum: a rare report of a pediatric case. Surg Case Rep. 2022;8:53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 5. | Emura T, Hashizume K, Asashima M. Experimental study of the embryogenesis of gastrointestinal duplication and enteric cyst. Pediatr Surg Int. 2003;19:147-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Morris G, Kennedy A Jr. Small Bowel Congenital Anomalies: A Review and Update. Surg Clin North Am. 2022;102:821-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 7. | Stern LE, Warner BW. Gastrointestinal duplications. Semin Pediatr Surg. 2000;9:135-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 82] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 8. | Deng KH, Yuan Y, Liu W. Gastrointestinal Bleeding as Initial Presentation of Intestinal Duplication. J Pediatr Gastroenterol Nutr. 2022;74:e98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 9. | Cárdenas Elias MA, Vázaquez Rueda F, Betancourth-Alvarenga JE, Centeno Haro M, Murcia Pascual FJ, Paredes Esteban RM. [Intestinal duplication, a single experiencie center]. Cir Pediatr. 2016;29:54-57. [PubMed] |
| 10. | Gadducci A, Pistolesi S, Guerrieri ME, Cosio S, Carbone FG, Naccarato AG. Malignant Transformation in Mature Cystic Teratomas of the Ovary: Case Reports and Review of the Literature. Anticancer Res. 2018;38:3669-3675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | O'Donovan EJ, Thway K, Moskovic EC. Extragonadal teratomas of the adult abdomen and pelvis: a pictorial review. Br J Radiol. 2014;87:20140116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Kanneganti A, Bhadiraju P, Tong PSY. Extragonadal teratomas in women and adolescent girls: A systematic review. Eur J Obstet Gynecol Reprod Biol. 2021;262:134-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |