Published online Feb 27, 2023. doi: 10.4240/wjgs.v15.i2.169
Peer-review started: November 4, 2022
First decision: November 27, 2022
Revised: November 27, 2022
Accepted: January 16, 2023
Article in press: January 16, 2023
Published online: February 27, 2023
Processing time: 115 Days and 6.8 Hours
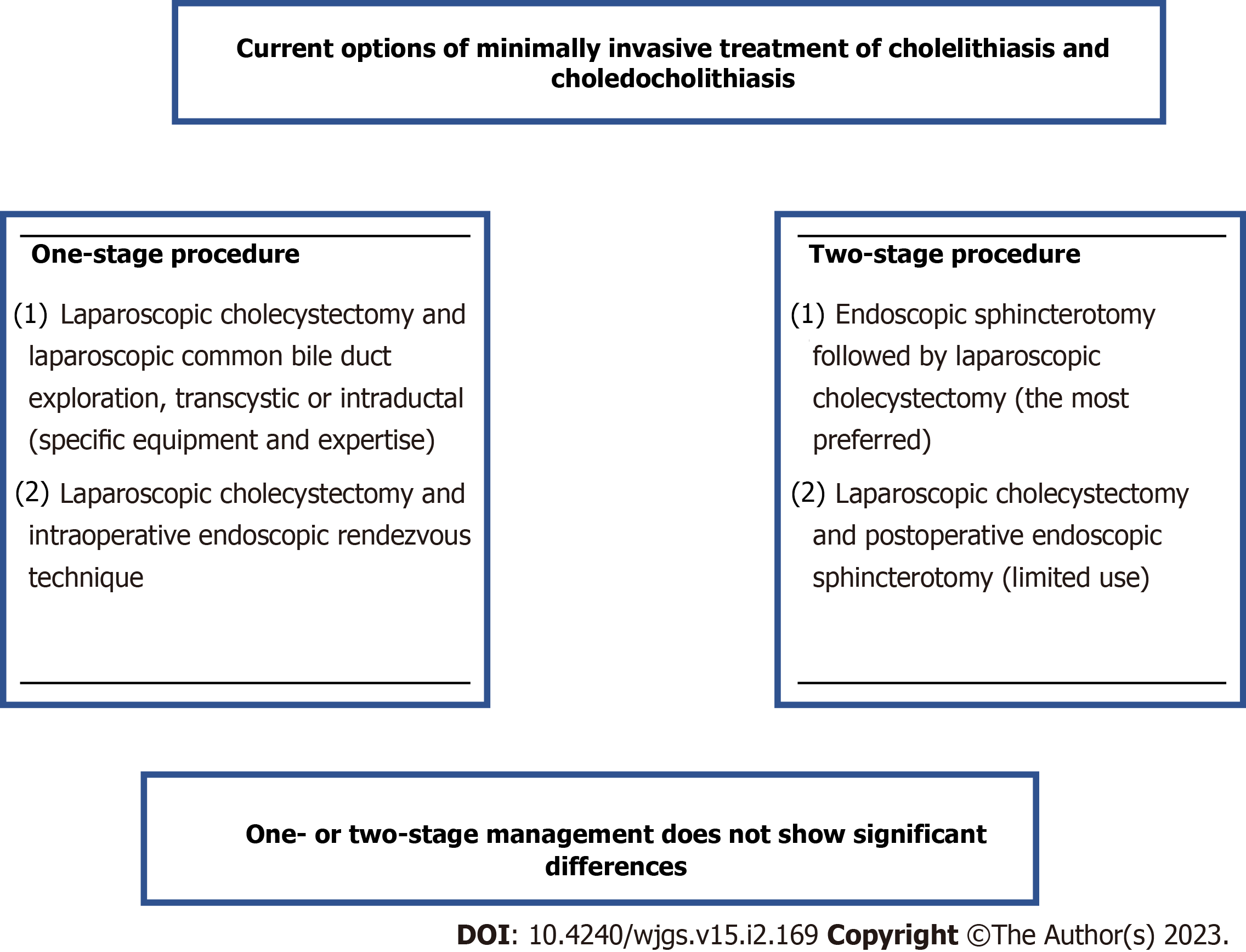
The management policy of concomitant cholelithiasis and choledocholithiasis is based on a one- or two-stage procedure. It basically includes either laparoscopic cholecystectomy (LC) with laparoscopic common bile duct (CBD) exploration (LCBDE) in the same operation or LC with preoperative, postoperative and even intraoperative endoscopic retrograde cholangiopancreatography-endoscopic sphincterotomy (ERCP-ES) for stone clearance. The most frequently used worldwide option is preoperative ERCP-ES and stone removal followed by LC, preferably on the next day. In cases where preoperative ERCP-ES is not feasible, the proposed alternative of intraoperative rendezvous ERCP-ES simultaneously with LC has been advocated. The intraoperative extraction of CBD stones is superior to postoperative rendezvous ERCP-ES. However, there is no consensus on the superiority of laparoendoscopic rendezvous. This is equivalent to a traditional two-stage procedure. Endoscopic papillary large balloon dilation reduces recurrence. LCBDE and intraoperative ERCP have similar good outcomes. The risk of recurrence after ERCP-ES is greater than that after LCBDE. Laparoscopic ultrasonography may delineate the anatomy and detect CBD stones. The majority of surgeons prefer the transcductal instead of the transcystic approach for CBDE with or without T-tube drainage, but the transcystic approach must be used where possible. LCBDE is a safe and effective choice when performed by an experienced surgeon. However, the requirement of specific equipment and advanced training are drawbacks. The percutaneous approach is an alternative when ERCP fails. Surgical or endoscopic reintervention for retained stones may be needed. For asymptomatic CBD stones, ERCP clearance is the first-choice method. Both one-stage and two-stage management are acceptable and can ensure improved quality of life.
Core Tip: One- or two-stage management of concurrent cholelithiasis and choledocholithiasis is safe and acceptable and does not show significant differences. Current diagnostic tools and interventional techniques can offer the optimal outcome, especially in difficult cases or recurrent stones. The relevant training and gained expertise play an essential role in performing the kind of available and acceptable method of minimally invasive treatment.
- Citation: Pavlidis ET, Pavlidis TE. Current management of concomitant cholelithiasis and common bile duct stones. World J Gastrointest Surg 2023; 15(2): 169-176
- URL: https://www.wjgnet.com/1948-9366/full/v15/i2/169.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i2.169
Cholelithiasis is a common disease affecting up to 20% of the adult population in Western countries but is usually asymptomatic. Common bile duct (CBD) stones are secondary in the vast majority of cases coexisting with cholelithiasis (10%-15%) originating from the gallbladder through the cystic duct. Its incidence increases with advancing age. Primary or native stones are relatively rare[1-5]. One-stage or two-stage management continues to be controversial, but both provide equivalent outcomes[4,6].
Patients with symptomatic cholelithiasis have a 10% possibility of concomitant CBD stones without causing symptoms. A study from the United States found that laparoscopic cholecystectomy (LC) accompanied by routine intraoperative cholangiography, in cases of symptomatic cholelithiasis with asymptomatic choledocholithiasis, was better than preoperative magnetic resonance cholangiopancreatography (MRCP) in terms of effectiveness and cost analysis[7]. However, the latter is the preferred method in clinical practice in symptomatic cases with transient obstructive jaundice or elevated liver function tests and previous episodes of acute pancreatitis[8]. A debate still exists about the routine or selective use of intraoperative cholangiography[9], but it seems more reasonable in the era of MRCP availability based on well-defined indications[10].
A recent study demonstrated advantages of intraoperative cholangiography compared to preoperative endoscopic retrograde cholangiopancreatography (ERCP)[11]. A recent meta-analysis showed that prophylactic cholecystectomy after ERCP- endoscopic sphincterotomy (ERCP-ES) CBD stone clearance was better than the wait-and-see policy. It was associated with fewer complications (acute cholecystitis, acute cholangitis, acute pancreatitis and biliary colic)[12]. However, it should be particularly considered in extremely elderly patients with limited life expectancy or unfit frail patients. A recent controversy has emerged about the role of routine prophylactic cholecystectomy after ERCP, postulating that it must be re-evaluated given the low risk of the above complications[13].
A previous nationwide study from the United States found a conversion rate from laparoscopic to open cholecystectomy of between 5%-10%; major conversion factors were recognized as acute cholecystitis, choledocholithiasis, male sex and obesity[14]. However, since then, much progress has been made in the laparoscopic management of choledocholithiasis.
The most widely used approach for concomitant gallbladder and CBD stones is ERCP-ES then LC followed by simultaneous LC and CBD exploration and intraoperative ERCP-ES and LC[6,15-17]. A recent survey among surgeons from the United Kingdom showed that for suspected choledocholithiasis, MRCP was the preferred first choice by the vast majority (80.0%), and intraoperative imaging was preferred by the remaining minority (14.4%). Intraoperative cholangiography (83.0%) prevailed over intraoperative ultrasound (17.0%). ERCP-ES followed by LC (two-stage procedure, 62.1%) prevailed over LC and laparoscopic common bile duct exploration (LCBDE) (one-stage procedure, 33.4%). For LCBDE, the preferred route was through the CBD (62.5%) using T-tube drainage selectively. The requirement of specific equipment and advanced training are drawbacks for LCBDE[8]. LCBDE and intraoperative ERCP have similar good outcomes[18].
A previous similar scoring system was proposed[19], but the guidelines of the American Society for Gastrointestinal Endoscopy and the Society of American Gastrointestinal and Endoscopic Surgeons for the management of suspected choledocholithiasis have defined several graded predictors. They include the following: (1) Very strong (CBD stone on ultrasound, bilirubin > 4 mg/dL); (2) Strong (CBD > 6 mm, bilirubin 1.8-4 mg/dL); and (3) Moderate (abnormal liver function tests other than bilirubin, age > 55 years, previous acute biliary pancreatitis)[20]. For suspected choledocholithiasis in acute cholecystitis, a model consisting of three preoperative predictive factors (increased serum glutamic pyruvic transaminase or alanine aminotransferase more than threefold, elevated alkaline phosphatase and CBD diameter more than 6 mm) was defined. When 0-1 factors exist, the possibility of CBD stone absence will be 98.6%, but when all three factors exist, the risk of CBD stones will be 77.8%[21].
The recurrence after successful CBD stone clearance reaches up to 8.4% within a median time of 2.5 years, and it is more often found after ERCP-ES than after LCBDE[18,22]. This is particularly related to some morphological subtypes (S and polyline type) of CBD[23], and regular follow-up is necessary in cases with risk factors[24].
In this mini review, we evaluated the current management options of concomitant gallbladder and CBD stones, highlighting the updated knowledge by selection and focus of the most relevant articles from PubMed. The current options of minimally invasive treatment of cholelithiasis and choledocholithiasis are summarized in Figure 1.
Rendezvous technique: This technique is a well-established method for the management of CBD stones that combines ERCP-ES stone clearance and LC in the same operation with the patient under general anesthesia[1,6,25]. It is feasible, safe and effective not only in elective but also in emergency cases, as shown in a recent study including 61 cases and 120 cases, respectively[26]. In addition, the method has applications in pediatric patients with excellent results[27]. A recent comparative study found that this intraoperative application of ERCP-ES was superior to its postoperative application regarding the better success rate and the decrease in postoperative acute pancreatitis, hospitalization and financial cost[28].
The Swedish National Registry for Gallstone Disease and ERCP included 1770 cases of rendezvous ERCP-ES, either intraoperative (n = 1205) or postoperative (n = 565). Comparison between the two groups found a higher rate of retained stones (5.5% vs 0.6%) and overall complications in the postoperative group (19.7% vs 14.0%). The main complications included post-ERCP acute pancreatitis (6.4% vs 3.2%) and postoperative infections (4.4% vs 2.3%). These differences were statistically significant (P < 0.005)[29]. Therefore, the postoperative rendezvous ERCP-ES has been limited but is still an acceptable alternative method when relevant equipment is unavailable[25].
A recent systematic review and meta-analysis including 1061 patients (542 with intraoperative rendezvous and 519 with two-stage preoperative ERCP and subsequent LC) found that no differences existed regarding stone clearance and postoperative bleeding, cholangitis or bile leak and conversion rate. However, the intraoperative rendezvous group had a longer operative time but less postoperative pancreatitis, morbidity and hospitalization[30]. A recent retrospective study from Italy demonstrated that laparoscopic rendezvous shortened the endoscopic time and may be a reasonable alternative to intraoperative ERCP[31].
Balloon sphincteroplasty by a transcystic wire balloon catheter to dilate the sphincter of Oddi and saline flushing may facilitate stone passage in 75% of cases[32]. Intervention vs surveillance to clear CBD stones during LC is better and has been recommended[33].
LC and LCBDE: This approach has all the benefits of a minimally invasive operation and ensures the resolution of concomitant gallbladder and CBD stones in a single session, as does traditional open CBD exploration[34], thus avoiding any complications of preoperative ERCP-ES (pancreatitis, cholangitis, bleeding, duodenal perforation)[35,36]. However, it requires specific equipment and advanced training that encourage the vast majority of surgeons to prefer the two-stage procedure by preoperative ERCP-ES[5]. Subsequently, the one-stage LC and LCBDE is a safe and cost-effective choice but only where expertise and equipment are available[37].
Severe ischemic heart disease, American Society of Anesthesiologists III or IV score is not a contraindication for LC and LCBDE. However, its safe performance requires both surgical and anesthesiological experience, continuous intraoperative monitoring and low-pressure pneumoperitoneum of 10-12 mmHg. After the latter’s abolition, the patient’s condition will be better because of the minimal invasiveness application[38].
A recent study from the United Kingdom including 311 cases of LCBDE [the majority (66%) were emergency procedures] showed laparoscopic ultrasound as the main diagnostic tool (73%). The completion rate was 94%. The route through choledochotomy was 56%, and transcystic was 44%. Bile leak occurred in 4.2% of patients, retained stones after 3 mo were present in 3.9% of patients, and the mortality rate was 0.66%[39]. Laparoscopic ultrasound instead of intraoperative cholangiography is a reasonable alternative performed during LC because it may delineate the anatomy and detect CBD stones[40].
Another recent retrospective multicenter study including 3950 cases of LCBDE showed a prevalence of the transcystic approach (63.1%), with a failure rate of 4% and a morbidity rate of 13.6%. However, most importantly, a survey defined a high rate (82.4%) of poor or very poor current training[41]. For primary CBD stones without cholelithiasis, LCBDE preserving the gallbladder has been recently reported[42]. A recent study from Scotland including 1318 LC and LCBDE among 5739 total LC performed (23%) showed a rate of intraoperative cholangiography of 98%, the transcystic approach rate of 66%, a conversion rate of 2.1%, retained stones in 2.1% of patients, a morbidity rate of 18.7% and a mortality rate of 0.2%[37].
A recent systematic review and meta-analysis found that LC and LCBDE after previous ERCP-ES failed CBD clearance had acceptable results and constituted a reliable alternative choice after endoscopic failure[43]. A recent retrospective study from the United Kingdom found that the transcystic or transductal approach for LCBDE had similar results regarding stone clearance, conversion to open surgery and mortality, but morbidity and complications were higher in the transductal route[44]. For LCBDE, an impacted stone may have a more difficult extraction, and multiple CBD stones are associated with a higher complication risk[45].
Primary closure of the CBD without T-tube placement after LCBDE has been proposed as a safe and feasible choice even in patients ≥ 70-years-old[46] and in cases of acute cholangitis[47]. In patients > 75-years-old, one-stage LC and CBDE were found to be better than two-stage ERCP-ES and LC. However, for multiple stones, a choledochoduodenal anastomosis may be an acceptable choice[48]. Choledochoscopic CBD exploration at the time of LC vs ERCP has been proposed with a stone clearance success rate of 84% and a risk of recurrence of 2%[49].
ERCP-ES and subsequent LC, the most preferred method worldwide[4,17,50], is a safe management process even in patients with cardiovascular disease[51]. A randomized controlled study showed that routine nasobiliary tubes after endoscopic CBD stone clearance can facilitate subsequent LC by the ability of the intraoperative cholangiography and ensure the anatomical integrity of the CBD[52].
In the United States, 10%-15% of ERCP CBD stone-clearance cases are difficult or complex[53]. In difficult CBD stones, step-by-step management is indicated. ES and large balloon dilation is the initial approach. Mechanical lithotripsy or preferably cholangioscopy-assisted lithotripsy are alternative options, but the latter may be used as the initial step[54,55]. Additionally, fully covered metal stents are safe and may be useful when they remain for more than 1 mo, especially in males and stone sizes less than 2 cm[56].
A national survey from South Korea on the management of difficult CBD stones (above 15-20 mm in size) showed the following findings: (1) In the vast majority (74.4%), a large balloon dilation after ES was the followed method or alone in cases of bleeding predisposition; (2) Double wire use in periampullary diverticulum and cannulation difficulty; and (3) Percutaneous transhepatic cholangioscopy or cap-fitted endoscopy in cases of previous gastrectomy[57].
A recent large study from China found differences between two expertise centers in choledocholithiasis characteristics and ERCP stone clearance with emphasis on the presence of periampullary diverticulum. After ERCP, the complications and residual stones did not differ between patients with or without a periampullary diverticulum, but the diameter of the CBD was wider in those with it than those without it[58].
A recent randomized controlled trial from China showed that CBD stone recurrence and re-recurrence after ERCP were reduced efficiently by endoscopic papillary large balloon dilation at a median follow-up of 56 mo[59]. A recent study determined predictive factors of ERCP-ES failure for stone clearance by multivariate analysis. They included previous biliary exploration, advanced age, intrahepatic stones, elevated serum total bilirubin, stones in the cystic duct or Mirizzi syndrome, CBD dilatation and the need for suprapapillary opening[60]. After ERCP-ES failure, LCBDE is feasible and safe[61].
In selected cases of cholelithiasis and choledocholithiasis, endoscopic ultrasound-guided gallbladder drainage combined with ERCP-ES is a reasonable modern approach that can manage the disease by endoscopic means[62]. When ERCP-ES is not possible for various reasons, a reliable alternative is the percutaneous management of CBD stones that is feasible and safe[3]. Reinterventions in stone recurrence, mainly ERCP or surgical (laparoscopic or open), may be needed[63].
For asymptomatic CBD stones, ERCP-ES is the first choice of recommended management despite the higher complication rate, especially of acute pancreatitis, than that of symptomatic cases. However, it is not yet clear by evidence-based data that this approach is justifiable[50]. The opposite point of view postulates by assessing the natural history that while early endoscopic removal of silent stones does not absolutely prevent further biliary complications, it has the risk of post-ERCP severe pancreatitis (5.2%). Therefore, wait-and-see management has been considered as the best choice for asymptomatic CBD stones[64].
In patients with acute cholecystitis and CBD stones, early management either by preoperative ERCP-ES followed by LC or LC and LCBDE is acceptable for both, with similar results[65]. In cases of severe acute biliary pancreatitis, CBD stenting by preventing stone passage reduces the risk of recurrence from the recommended delayed cholecystectomy[66]. The assessment of quality of life showed similar satisfaction of improvement between preoperative ERCP-ES followed by LC or LC and LCBDE[67].
The experience of general surgery residents on CBD exploration has decreased due to the application of ERCP-ES. This training deficiency should be managed effectively[68].
Much progress has been made in the current management of concomitant gallbladder and CBD stones in recent years. Preoperative ERCP-ES followed by LC is the most commonly used method in clinical practice. LCBDE is a safe and effective choice when it is performed by an experienced surgeon and the required equipment with all facilities is available. The rendezvous technique ensures a single intervention combining ERCP-ES and LC. Both one-stage and two-stage management have equivalent results. In difficult or recurrent cases, advanced endoscopic, radiologic and minimally invasive techniques are in use but require expertise. The surgeon must choose the most appropriate intervention for accurate diagnosis and the best management based on his or her own experience, the preoperative assessment and intraoperative findings.
| 1. | Vaccari S, Minghetti M, Lauro A, Bellini MI, Ussia A, Khouzam S, Marino IR, Cervellera M, D'Andrea V, Tonini V. Destiny for Rendezvous: Is Cholecysto/Choledocholithiasis Better Treated with Dual- or Single-Step Procedures? Dig Dis Sci. 2022;67:1116-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (3)] |
| 2. | Akmal AM, Putra BP, Darmaningrat CIAA, Nariswari IGARC, Srigede LD, Budyono C. Management of Cholelithiasis with Concomitant Choledocholithiasis. Acta Med Indones. 2022;54:151-157. [PubMed] |
| 3. | Ozcan N, Riaz A, Kahriman G. Percutaneous Management of Biliary Stones. Semin Intervent Radiol. 2021;38:348-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 4. | Cianci P, Restini E. Management of cholelithiasis with choledocholithiasis: Endoscopic and surgical approaches. World J Gastroenterol. 2021;27:4536-4554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 99] [Cited by in RCA: 91] [Article Influence: 18.2] [Reference Citation Analysis (21)] |
| 5. | Jorba R, Pavel MC, Llΰcer-Millαn E, Estalella L, Achalandabaso M, Juliΰ-Verdaguer E, Nve E, Padilla-Zegarra ED, Badia JM, O'Connor DB, Memba R. Contemporary management of concomitant gallstones and common bile duct stones: a survey of Spanish surgeons. Surg Endosc. 2021;35:5024-5033. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 6. | Kattih O, Velanovich V. Comparing One-Stage vs Two-Stage Approaches for the Management of Choledocholithiasis. J Gastrointest Surg. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 7. | Epelboym I, Winner M, Allendorf JD. MRCP is not a cost-effective strategy in the management of silent common bile duct stones. J Gastrointest Surg. 2013;17:863-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Tanase A, Dhanda A, Cramp M, Streeter A, Aroori S. A UK survey on variation in the practice of management of choledocholithiasis and laparoscopic common bile duct exploration (ALiCE Survey). Surg Endosc. 2022;36:5882-5896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (1)] |
| 9. | Georgiou K, Sandblom G, Alexakis N, Enochsson L. Intraoperative cholangiography 2020: Quo vadis? Hepatobiliary Pancreat Dis Int. 2022;21:145-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 10. | Brunt LM. Should We Utilize Routine Cholangiography? Adv Surg. 2022;56:37-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 11. | Tsikis S, Yin SH, Odom SR, Narula N. Intraoperative cholangiography: a stepping stone to streamlining the treatment of choledocholithiasis. Surg Endosc. 2022;36:4885-4892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 12. | Mc Geehan G, Melly C, O' Connor N, Bass G, Mohseni S, Bucholc M, Johnston A, Sugrue M. Prophylactic cholecystectomy offers best outcomes following ERCP clearance of common bile duct stones: a meta-analysis. Eur J Trauma Emerg Surg. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 13. | Toogood K, Pike T, Coe P, Everett S, Huggett M, Paranandi B, Bassi V, Toogood G, Smith A. The role of cholecystectomy following endoscopic sphincterotomy and bile duct stone removal. Ann R Coll Surg Engl. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Livingston EH, Rege RV. A nationwide study of conversion from laparoscopic to open cholecystectomy. Am J Surg. 2004;188:205-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 234] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 15. | Sharma A, Dahiya P, Khullar R, Soni V, Baijal M, Chowbey PK. Management of common bile duct stones in the laparoscopic era. Indian J Surg. 2012;74:264-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (2)] |
| 16. | Duncan CB, Riall TS. Evidence-based current surgical practice: calculous gallbladder disease. J Gastrointest Surg. 2012;16:2011-2025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 89] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 17. | Guo T, Wang L, Xie P, Zhang Z, Huang X, Yu Y. Surgical methods of treatment for cholecystolithiasis combined with choledocholithiasis: six years' experience of a single institution. Surg Endosc. 2022;36:4903-4911. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 18. | Mohseni S, Bass GA, Forssten MP, Casas IM, Martin M, Davis KA, Haut ER, Sugrue M, Kurihara H, Sarani B, Cao Y, Coimbra R. Common bile duct stones management: A network meta-analysis. J Trauma Acute Care Surg. 2022;93:e155-e165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 19. | Pejoviζ T, Stojadinoviζ MM. Scoring System Development and Validation for Prediction Choledocholithiasis before Open Cholecystectomy. Srp Arh Celok Lek. 2015;143:681-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Tracy BM, Poulose BK, Paterson CW, Mendoza AE, Gaitanidis A, Saxe JM, Young AJ, Zielinski MD, Sims CA, Gelbard RB; EAST Retained Common Bile Duct Stones Study Group. National adherence to the ASGE-SAGES guidelines for managing suspected choledocholithiasis: An EAST multicenter study. J Trauma Acute Care Surg. 2022;92:305-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Chisholm PR, Patel AH, Law RJ, Schulman AR, Bedi AO, Kwon RS, Wamsteker EJ, Anderson MA, Elta GH, Govani SM, Prabhu A. Preoperative predictors of choledocholithiasis in patients presenting with acute calculous cholecystitis. Gastrointest Endosc. 2019;89:977-983.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 22. | Gonzαlvez-Guardiola P, Payα-Llorente C, Domingo-Del Pozo C, Martνnez-Pιrez A. Predictors for stone recurrence after a successful common bile duct surgical exploration for choledocholithiasis. Langenbecks Arch Surg. 2022;407:1545-1552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Reference Citation Analysis (0)] |
| 23. | Saito H, Tada S. Risk prediction of common bile duct stone recurrence based on new common bile duct morphological subtypes. World J Gastrointest Surg. 2022;14:874-876. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Kim KH. Need to identify the risk factor for stone recurrence after common bile duct exploration. J Minim Invasive Surg. 2021;24:8-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 25. | Syrιn EL, Sandblom G, Eriksson S, Eklund A, Isaksson B, Enochsson L. Postoperative rendezvous endoscopic retrograde cholangiopancreaticography as an option in the management of choledocholithiasis. Surg Endosc. 2020;34:4883-4889. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 26. | Pizzicannella M, Barberio M, Lapergola A, Gregori M, Maurichi FA, Gallina S, Benedicenti P, Viola MG. One-stage approach to cholecystocholedocholithiasis treatment: a feasible surgical strategy for emergency settings and frail patients. Surg Endosc. 2022;36:8560-8567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Gee KM, Jones RE, Casson C, Barth B, Troendle D, Beres AL. More Is Less: The Advantages of Performing Concurrent Laparoscopic Cholecystectomy and Endoscopic Retrograde Cholangiopancreatography for Pediatric Choledocholithiasis. J Laparoendosc Adv Surg Tech A. 2019;29:1481-1485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 28. | Di Lascia A, Tartaglia N, Pavone G, Pacilli M, Ambrosi A, Buccino RV, Petruzzelli F, Menga MR, Fersini A, Maddalena F. One-step versus two-step procedure for management procedures for management of concurrent gallbladder and common bile duct stones. Outcomes and cost analysis. Ann Ital Chir. 2021;92:260-267. [PubMed] |
| 29. | Noel R, Arnelo U, Swahn F. Intraoperative versus postoperative rendezvous endoscopic retrograde cholangiopancreatography to treat common bile duct stones during cholecystectomy. Dig Endosc. 2019;31:69-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 30. | Lin Y, Su Y, Yan J, Li X. Laparoendoscopic rendezvous versus ERCP followed by laparoscopic cholecystectomy in the management of cholecystocholedocholithiasis: a systemic review and meta-analysis. Surg Endosc. 2020;34:4214-4224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 31. | Lagouvardou E, Martines G, Tomasicchio G, Laforgia R, Pezzolla A, Caputi Iambrenghi O. Laparo-endoscopic management of chole-choledocholithiasis: Rendezvous or intraoperative ERCP? Front Surg. 2022;9:938962. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 32. | Bosley ME, Ganapathy AS, Nunn AM, Westcott CJ, Neff LP. Outcomes following balloon sphincteroplasty as an adjunct to laparoscopic common bile duct exploration. Surg Endosc. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 33. | Johansson E, Φsterberg J, Sverdιn E, Enochsson L, Sandblom G. Intervention versus surveillance in patients with common bile duct stones detected by intraoperative cholangiography: a population-based registry study. Br J Surg. 2021;108:1506-1512. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (1)] |
| 34. | Lien HH, Huang CC, Huang CS, Shi MY, Chen DF, Wang NY, Tai FC. Laparoscopic common bile duct exploration with T-tube choledochotomy for the management of choledocholithiasis. J Laparoendosc Adv Surg Tech A. 2005;15:298-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 35. | Lauter DM, Froines EJ. Laparoscopic common duct exploration in the management of choledocholithiasis. Am J Surg. 2000;179:372-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 36. | Campbell J, Pryor A, Docimo S Jr. Transcystic Choledochoscopy Utilizing a Disposable Choledochoscope: How We Do It. Surg Laparosc Endosc Percutan Tech. 2022;32:616-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 37. | Nassar AHM, Ng HJ, Katbeh T, Cannings E. Conventional Surgical Management of Bile Duct Stones: A Service Model and Outcomes of 1318 Laparoscopic Explorations. Ann Surg. 2022;276:e493-e501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 38. | Salameh JR, Franklin ME Jr. Acute cholecystitis and severe ischemic cardiac disease: is laparoscopy indicated? JSLS. 2004;8:61-64. [PubMed] |
| 39. | Kostalas M, Christopoulos P, Platt T, Sinha S, Bowling K, Srinivas G, Andrews S. Delivery of a Laparoscopic Bile Duct Exploration Service as a Primary Treatment Modality for Choledocholithiasis within the NHS Healthcare System. Surg Endosc. 2022;36:7462-7470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 40. | Deziel DJ. Laparoscopic Ultrasound for Bile Duct Imaging during Cholecystectomy: Clinical Impact in 785 Consecutive Cases. J Am Coll Surg. 2022;234:849-860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 41. | Lopez-Lopez V, Gil-Vazquez PJ, Ferreras D, Nassar AHM, Bansal VK, Topal B, Zhu JG, Chuang SH, Jorba R, Bekheit M, Martinez-Cecilia D, Parra-Membrives P, Sgourakis G, Mattila A, Bove A, Quaresima S, Barreras Gonzαlez JE, Sharma A, Ruiz JJ, Sαnchez-Bueno F, Robles-Campos R, Martinez-Isla A. Multi-institutional expert update on the use of laparoscopic bile duct exploration in the management of choledocholithiasis: Lesson learned from 3950 procedures. J Hepatobiliary Pancreat Sci. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 42. | Wang H, Zhang J, Lin X, Ou Y. Laparoscopic Common Bile Duct Exploration with Gallbladder Preservation: An Innovative Technique for Primary Common Bile Duct Stones. J Laparoendosc Adv Surg Tech A. 2022;32:974-977. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 43. | Zhu J, Zhang Y, Du P, Hu W, Xiao W, Li Y. Systematic Review and Meta-analysis of Laparoscopic Common Bile Duct Exploration in Patients With Previous Failed Endoscopic Retrograde Cholangiopancreatography. Surg Laparosc Endosc Percutan Tech. 2021;31:654-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 44. | Navaratne L, Martinez Isla A. Transductal versus transcystic laparoscopic common bile duct exploration: an institutional review of over four hundred cases. Surg Endosc. 2021;35:437-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 45. | Kao CT, Seagar R, Heathcock D, Tacey M, Lai JM, Yong T, Houli N, Bird D, Hodgson R. Factors That Predict the Success of Laparoscopic Common Bile Duct Exploration for Choledocholithiasis: A 10-Year Study. Surg Laparosc Endosc Percutan Tech. 2021;31:565-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 46. | Wu X, Huang ZJ, Zhong JY, Ran YH, Ma ML, Zhang HW. Laparoscopic common bile duct exploration with primary closure is safe for management of choledocholithiasis in elderly patients. Hepatobiliary Pancreat Dis Int. 2019;18:557-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 47. | Wang Y, Huang Y, Shi C, Wang L, Liu S, Zhang J, Wang W. Efficacy and safety of laparoscopic common bile duct exploration via choledochotomy with primary closure for the management of acute cholangitis caused by common bile duct stones. Surg Endosc. 2022;36:4869-4877. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 48. | Gantois D, Goudard Y, Bourgouin S, Pauleau G, de La Villιon B, Balandraud P. One-stage laparoscopic procedure versus two-stage procedure in the management of common bile duct stones in patients aged 75 and more. J Visc Surg. 2020;157:99-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 49. | Al-Habbal Y, Reid I, Tiang T, Houli N, Lai B, McQuillan T, Bird D, Yong T. Retrospective comparative analysis of choledochoscopic bile duct exploration versus ERCP for bile duct stones. Sci Rep. 2020;10:14736. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 50. | Saito H, Kadono Y, Shono T, Kamikawa K, Urata A, Nasu J, Imamura H, Matsushita I, Tada S. Remaining issues of recommended management in current guidelines for asymptomatic common bile duct stones. World J Gastroenterol. 2021;27:2131-2140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (3)] |
| 51. | Syrιn EL, Enochsson L, Eriksson S, Eklund A, Isaksson B, Sandblom G. Cardiovascular complications after common bile duct stone extractions. Surg Endosc. 2021;35:3296-3302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 52. | Sewefy AM, Elsageer EM, Kayed T, Mohammed MM, Taha Zaazou MM, Hamza HM. Nasobiliary guided laparoscopic cholecystectomy following endoscopic retrograde cholangiopancreatography, randomized controlled trial. Surgeon. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 53. | Podboy A, Gaddam S, Park K, Gupta K, Liu Q, Lo SK. Management of Difficult Choledocholithiasis. Dig Dis Sci. 2022;67:1613-1623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 54. | Tringali A, Costa D, Fugazza A, Colombo M, Khalaf K, Repici A, Anderloni A. Endoscopic management of difficult common bile duct stones: Where are we now? World J Gastroenterol. 2021;27:7597-7611. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (3)] |
| 55. | Lesmana CRA, Paramitha MS, Lesmana LA. Innovation of endoscopic management in difficult common bile duct stone in the era of laparoscopic surgery. World J Gastrointest Endosc. 2021;13:198-209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (2)] |
| 56. | Grande G, Pigς F, Avallone L, Bertani H, Mangiafico S, Russo S, Cocca S, Lupo M, Caruso A, Conigliaro R. Is the use of fully covered metal stents effective in the treatment of difficult lithiasis of the common bile duct? Surg Endosc. 2022;36:5684-5691. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 57. | Lee YS, Jeon TJ, Paik WH, Ahn DW, Chung KH, Son BK, Song TJ, Moon SH, Lee ES, Lee JM, Yoon SB, Paik CN, Lee YN, Park JS, Lee DW, Park SW, Chon HK, Cho KB, Park CH; Committee of Policy and Quality Management in Korean Pancreatobiliary Association. National Survey Regarding the Management of Difficult Bile Duct Stones in South Korea. Gut Liver. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 58. | Zhu KX, Yue P, Wang HP, Meng WB, Liu JK, Zhang L, Zhu XL, Zhang H, Miao L, Wang ZF, Zhou WC, Suzuki A, Tanaka K, Li X. Choledocholithiasis characteristics with periampullary diverticulum and endoscopic retrograde cholangiopancreatography procedures: Comparison between two centers from Lanzhou and Kyoto. World J Gastrointest Surg. 2022;14:132-142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 59. | Wang X, Wang X, Sun H, Ren G, Wang B, Liang S, Zhang L, Kang X, Tao Q, Guo X, Luo H, Pan Y. Endoscopic Papillary Large Balloon Dilation Reduces Further Recurrence in Patients With Recurrent Common Bile Duct Stones: A Randomized Controlled Trial. Am J Gastroenterol. 2022;117:740-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 60. | Marcelino LP, Thofehrn S, Eyff TF, Bersch VP, Osvaldt AB. Factors predictive of the successful treatment of choledocholithiasis. Surg Endosc. 2022;36:1838-1846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 61. | Al-Ardah M, Barnett RE, Whewell H, Boyce T, Rasheed A. Laparoscopic Common Bile Duct Clearance, is It Feasible and Safe After Failed Endoscopic Retrograde Cholangiopancreatography? J Laparoendosc Adv Surg Tech A. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 62. | Torres Yuste R, Garcia-Alonso FJ, Sanchez-Ocana R, Cimavilla Roman M, Peρas Herrero I, Carbajo AY, De Benito Sanz M, Mora Cuadrado N, De la Serna Higuera C, Perez-Miranda M. Safety and efficacy of endoscopic ultrasound-guided gallbladder drainage combined with endoscopic retrograde cholangiopancreatography in the same session. Dig Endosc. 2020;32:608-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 63. | Ng HJ, Nassar AHM. Reinterventions following laparoscopic cholecystectomy and bile duct exploration. A review of prospective data from 5740 patients. Surg Endosc. 2022;36:2809-2817. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 64. | Hakuta R, Hamada T, Nakai Y, Oyama H, Kanai S, Suzuki T, Sato T, Ishigaki K, Saito K, Saito T, Takahara N, Mizuno S, Kogure H, Watadani T, Tsujino T, Tada M, Abe O, Isayama H, Koike K. Natural history of asymptomatic bile duct stones and association of endoscopic treatment with clinical outcomes. J Gastroenterol. 2020;55:78-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 65. | Yan Y, Sha Y, Yuan W, Yuan H, Zhu X, Wang B. One-stage versus two-stage management for acute cholecystitis associated with common bile duct stones: a retrospective cohort study. Surg Endosc. 2022;36:920-929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 66. | Hormati A, Ghadir MR, Alemi F, Eshraghi M, Dehghan K, Sarkeshikian SS, Ahmadpour S, Jabbari A, Sivandzadeh GR, Mohammadbeigi A. Efficacy of Common Bile Duct Stenting on the Reduction in Gallstone Migration and Symptoms Recurrence in Patients with Biliary Pancreatitis Who Were Candidates for Delayed Cholecystectomy. Dig Dis Sci. 2022;67:315-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 67. | Asuri K, Jain M, Maheshwari P, Prakash O, Kumar S, Garg P, Sagar R, Bansal VK. Quality of Life Outcomes Following Single-stage Laparoscopic Common Bile Duct Exploration Versus 2-stage Endoscopic Sphincterotomy Followed by Laparoscopic Cholecystectomy in Management of Cholelithiasis With Choledocholithiasis. Surg Laparosc Endosc Percutan Tech. 2021;31:285-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (1)] |
| 68. | Warner RL, Coleman KC, Musgrove KA, Bardes JM, Borgstrom DC, Grabo DJ. A review of general surgery resident experience in common bile duct exploration in the ERCP era. Am J Surg. 2020;220:899-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Morera-Ocon FJ, Spain; Tomasicchio G, Italy S-Editor: Liu GL L-Editor: Filipodia P-Editor: Liu GL