Published online Nov 27, 2023. doi: 10.4240/wjgs.v15.i11.2579
Peer-review started: July 17, 2023
First decision: August 8, 2023
Revised: August 13, 2023
Accepted: October 27, 2023
Article in press: October 27, 2023
Published online: November 27, 2023
Processing time: 133 Days and 8.7 Hours
Indications for surgery in inflammatory bowel disease (IBD) include treatment-refractory disease or severe complications such as obstruction, severe colitis, dysplasia, or neoplasia. Infectious complications following colorectal surgery in IBD are significant, particularly in high-risk patients.
To gather evidence on risk factors associated with increased post-operative infectious complications in IBD and explore management strategies to reduce morbidity and mortality.
A systematic review adhering to PRISMA-P guidelines was conducted. MEDLINE (PubMed) and Cochrane Library databases were searched using specific key
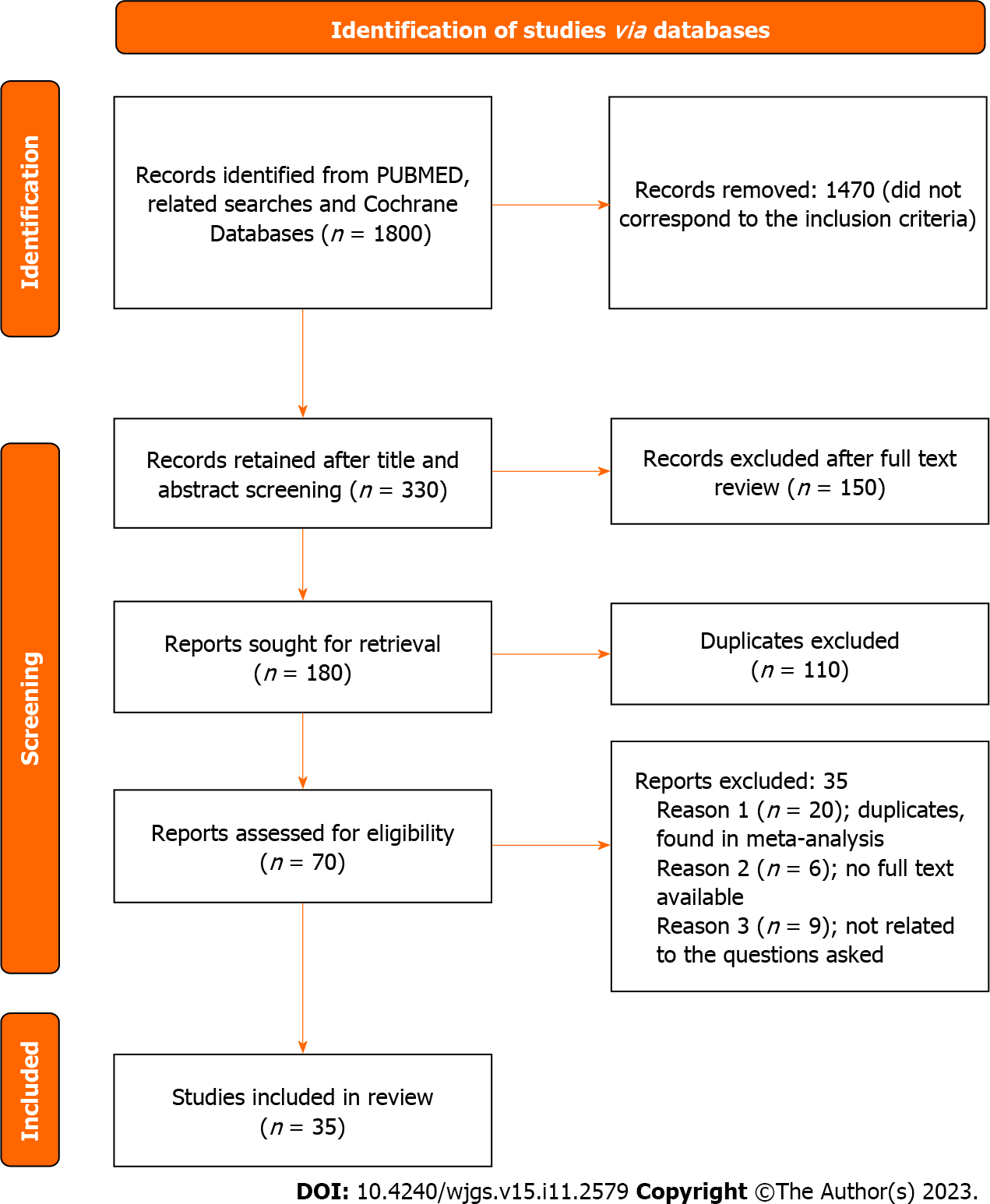
The initial database search yielded 1800 articles, with 330 articles undergoing full-text review. After excluding duplicates and irrelevant papers, 35 articles were included for analysis. Risk factors for post-operative complications in patients with IBD included hypoalbuminemia, malnutrition, preoperative abscess, and obesity. Perioperative blood transfusion was associated with increased infectious complications. Medications such as 5-aminosalicylates and immunomodulators did not increase post-operative complications. Corticosteroids were associated with an increased risk of complications. Ustekinumab and vedolizumab showed similar rates of infectious complications compared to other treatments. The impact of minimally invasive surgery on post-operative complications varied across studies.
In order to reduce post-operative infectious complications in patients with IBD, a comprehensive approach involving multiple disciplines is necessary.
Core Tip: This paper highlights the risk factors associated with post-operative infectious complications in patients with inflammatory bowel disease (IBD) undergoing abdominal surgery and explores management strategies to reduce morbidity and mortality. Key findings include the association of hypoalbuminemia, malnutrition, preoperative abscess, obesity, and perioperative blood transfusion with increased infectious complications. Corticosteroids were found to be a risk factor, while medications such as 5-aminosalicylates and immunomodulators did not increase complications. Ustekinumab and vedolizumab showed comparable rates of infectious complications to other treatments. The impact of minimally invasive surgery on complications varied. This paper emphasizes the importance of a comprehensive approach involving multiple disciplines to mitigate post-operative infections in IBD patients. Understanding these risk factors and implementing appropriate management strategies can improve outcomes in this patient population.
- Citation: Mowlah RK, Soldera J. Risk and management of post-operative infectious complications in inflammatory bowel disease: A systematic review. World J Gastrointest Surg 2023; 15(11): 2579-2595
- URL: https://www.wjgnet.com/1948-9366/full/v15/i11/2579.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i11.2579
Inflammatory bowel disease (IBD) comprises ulcerative colitis (UC) and Crohn’s disease (CD), which are chronic auto-inflammatory conditions characterized by periods of relapses and remissions. UC affects the colon and rectum mucosa, while CD involves transmural inflammation in any part of the gastrointestinal tract. Both diseases can have extra
IBD can cause debilitating physical and psychosocial symptoms, resulting in a significant economic burden associated with diagnosis, follow-up, and treatment[3]. Medical therapies, including 5-aminosalicylates (5-ASA), steroids, immunomodulators, small molecules, and biologics, aim to alleviate symptoms and achieve mucosal healing based on disease severity. Current treatment approaches focus on achieving endoscopic and clinical remission. However, despite the availability of various medical treatments, approximately 50% of CD patients and 16% of UC patients require surgery within 10 years of diagnosis[1,2].
Indications for surgery in IBD include treatment-refractory disease or severe complications such as obstruction, severe colitis, dysplasia, or neoplasia[4]. Infectious complications following colorectal surgery in IBD are significant, particularly in high-risk patients[5]. Early post-operative complications within 30 d of surgery include abdominal wound infection, anastomotic leakage, and pelvic sepsis. Late complications involve anastomotic leakage with pelvic sepsis, anastomotic stricture, and pouchitis following ileal pouch anal anastomosis (IPAA). These post-operative infectious complications contribute to increased morbidity, mortality, length of hospital stay, and healthcare costs. Several factors, including a patient’s general status and medications, are associated with these infectious complications.
Surgical treatment in the emergency setting presents challenges due to limited time for multidisciplinary interventions and the typically unstable condition of patients. Indications for emergent surgery include lack of improvement with medical therapy within 48 to 96 h, hemodynamic instability with multi-organ failure, bleeding, toxic megacolon, bowel obstruction, perforation, and intra-abdominal abscess (IAA) in CD. In these cases, an open approach is recommended for faster procedures, as laparoscopy may pose difficulties in handling the bowels. Damage control surgery is typically performed, involving bowel resection, stapling off both ends, laparotomy, and subsequent return to the intensive care unit for continuous care. A second-look laparotomy is performed within 24-48 h for bowel inspection and consideration of a stoma or anastomosis.
Laparoscopic surgery is indicated for hemodynamically stable patients with local expertise available. It is known to reduce the length of hospital stay and infectious complications[6]. An open port insertion technique should be employed to prevent perforation of distended bowel loops, with a multi-port approach being preferable to a single-port approach. In the acute setting, subtotal colectomy with ileostomy is recommended. The decision on anastomosis after intestinal resection depends on the patient’s clinical status and the indication for surgery. In patients with a compromised general health status in the emergency setting, resection with a stoma is preferred. In elective scenarios, side-to-side anastomosis is preferred.
Elective surgery is indicated for cases of chronic active or steroid-dependent colitis that is refractory to conventional or biological maintenance therapies. Subtotal colectomy with subsequent IPAA is the treatment of choice for UC. For CD, the surgical treatment options depend on the affected intestinal segment and presence of complications, including subtotal colectomy with ileorectal anastomosis, total proctocolectomy, segmental bowel resection, and strictureplasty[7]. In elective settings, these procedures can be performed laparoscopically as one- or two-stage procedures, with a single-stage procedure being an option for selected patients.
Post-operative infectious complications in IBD include surgical site infections (SSI) and extra-abdominal infections. SSI encompasses superficial wound infections, deep wound infections affecting the fascia, and organ space infections such as abdominal and pelvic abscesses and anastomotic leakage. Diagnosis of SSI is based on the presence of purulent tissue discharge from the incision site or drain, isolation of organisms from culture of fluids or tissue obtained from the incision site, and the presence of an open wound with signs and symptoms of infection. Extra-abdominal infections include pneumonia and urinary tract infections. These infections can lead to life-threatening complications such as sepsis and septic shock[5].
One risk factor associated with patient general status is serum albumin[5,8]. Serum albumin plays a crucial role in wound healing and collagen synthesis at the anastomotic site. Hypoalbuminemia adversely affects the immune system, increasing the risk of post-operative morbidity. Preoperative correction of hypoalbuminemia is necessary, and in some cases, a diverting colostomy or ileostomy may be warranted. Early assessment and optimization of nutritional status are also essential[9,10].
The presence of preoperative abscess is another risk factor indicating advanced disease[5]. It independently increases the risk of intra-abdominal septic complications (IASC). In such cases, surgery should be avoided, and medical treatment, including percutaneous drainage with antibiotics, is preferred.
Additionally, obesity has been associated with an increased risk of post-operative complications in patients with IBD, possibly due to enhanced inflammatory processes[11].
Perioperative blood transfusion is an independent risk factor associated with adverse outcomes, suggesting the need for a restricted transfusion policy[12,13].
Certain medications used in the preoperative setting, such as steroids and biologics such as anti-tumor necrosis factor (TNF)-α, have been linked to increased post-operative infectious complications. A Cochrane systematic review by Law et al[14] reported higher rates of infectious complications in patients using steroids, likely due to impaired anastomotic healing and altered patient condition resulting from prolonged use[14]. The use of anti-TNF-α remains controversial. The Patients Undergoing Surgery to Identify Risk Factors for Postoperative Infection (PUCCINI) trial, a multicenter prospective cohort study, found no independent association between anti-TNF-α and increased infectious complications when used within 3 mo preoperatively or with detectable serum levels at the time of surgery[15]. However, the Cochrane review by Law et al[14] showed an overall increase in post-operative complications when anti-TNF-α was used in CD patients within 8 wk of surgery. Due to conflicting results, delaying surgery for patients who have taken their last dose of anti-TNF-α more than 4 wk before surgery is not justified.
For patients with risk factors, minimally invasive surgery offers advantages such as faster gastrointestinal function recovery, shorter hospital stays, and reduced scarring. Side-to-side stapled anastomosis following ileocolic resection is preferred, as it is associated with lower post-operative complications and a decreased need for reoperation due to restenosis[16,17].
This literature review aims to gather evidence on risk factors associated with increased post-operative infectious complications in IBD and explore management strategies to reduce morbidity and mortality.
This systematic review was performed adhering to the PRISMA-P guidelines[18]. The research aimed to identify, select, and critically appraise the existing literature to explore similarities and differences related to the research question.
Searches were conducted in the MEDLINE (PubMed) and Cochrane Library databases using the following command: (“inflammatory bowel disease” OR “Crohn’s disease” OR “Ulcerative Colitis”) AND (“Surgery” OR “Postoperative” OR “operation”) AND (“infection” OR “sepsis” OR “septic shock”). The retrieved data were categorized into different headings, including complications, medications, and risk factors. Papers unrelated to the topic were excluded, and a summary of the remaining papers was conducted, noting useful information and reviewing the selected articles. Reference Citation Analysis (https://www.referencecitationanalysis.com/) was used to supplement the search.
Systematic reviews, meta-analyses, retrospective cohort studies, prospective cohort studies, and case-control studies were included in the selection process. The search was expanded to include “related articles” from PubMed. Papers were restricted to English and French languages, with no date of publication restriction. All selected papers were manually searched.
The study included patients diagnosed with IBD (UC or CD) based on clinical, endoscopic, radiological, or histopathological evidence. These patients underwent elective or emergent abdominal surgery related to the disease in primary, secondary, or tertiary healthcare settings. Participants were aged over 18 years and experienced infectious complications within 30 d of surgery. Infectious complications encompassed organ space infections (IAA), pneumonia, SSI, deep SSI, anastomosis leakage, sepsis, fistula, or urinary tract infections.
Patients under 18 years of age and pregnant women were excluded. Complications other than infectious ones were also excluded. Additionally, infectious complications occurring after 30 d of surgery were not included.
The selected papers were analyzed to address key questions regarding post-operative infectious complications, the impact of medications used to relieve inflammation on their occurrence, and other patient and surgery-related factors contributing to these complications. The results were combined in a narrative analysis to provide evidence-based factors responsible for an increase in post-operative infectious complications and recommendations for their management to reduce morbidity and mortality.
The PUBMED database and its related searches yielded an initial pool of 1800 articles. After screening the titles and abstracts, 1470 articles were deemed irrelevant and excluded. The remaining 330 articles underwent full-text review, resulting in the exclusion of 150 articles. Further removal of duplicates was conducted, leaving 70 articles for eligibility assessment. Among these, 35 articles were excluded either due to duplication or unavailability of full text. Figure 1 summarizes the search strategy. The results will be categorized into three main areas: Risk factors for post-operative complications, medications used to treat IBD and their association with post-operative complications, and the impact of the choice of surgical procedure on the occurrence of surgical complications.
Hypoalbuminemia: Retrospective studies conducted by Nguyen et al[8], Liu et al[19], Ghoneima et al[4], and Yang et al[20] have consistently shown that hypoalbuminemia is associated with an increased risk of post-operative infectious complications. This finding was further supported by a meta-analysis of eight studies conducted by Huang et al[5]. Specifically, hypoalbuminemia can serve as a valuable predictive factor for post-operative infectious complications, including SSI (Table 1).
| Ref. | Year | Studies | Cohort | Results |
| Nguyen et al[8] | 2019 | Retrospective (2005-2012) | CD and UC | Moderate to severe hypoalbuminemia is associated with increased post-operative infection: CD 20% vs 13%, P < 0.01; UC 28% vs 15%, P < 0.01. In the case of severe hypoalbuminemia, increased risk of intra-abdominal infection, sepsis, shock and pneumonia; additional risk for urinary tract infection in UC |
| Huang et al[5] | 2015 | Meta-analysis: 8 studies for hypoalbuminemia: Cohort; case control; case control; case control; case control; case control; cohort; case control | CD | Hypoalbuminemia is a risk factor for infectious complications |
| Liu et al[19] | 2017 | Retrospective 2014-2016 | CD | Increased surgical site infection with hypoalbuminemia |
| Ghoneima et al[4] | 2019 | Retrospective 2012-2017 | CD | Hypoalbuminemia is a predictive risk for septic complications especially if associated with anemia and high CRP |
| Yang et al[20] | 2012 | Retrospective 1991-2010 | CD | Preoperative albumin < 30 g/L increased the risk of post-operative complication by 2.6 fold |
Malnutrition: This is a well-established risk factor for unfavorable post-operative outcomes[19]. It is defined by criteria such as weight loss exceeding 10%-15% within 6 mo, a body mass index (BMI) below 18.5 kg/m2, or a serum albumin level below 30 g/L. In a study conducted by Yamamoto et al[10], two groups of patients with IBD were compared to identify risk factors for infectious complications following surgery. One group received biological therapy, while the control group did not. Both groups included malnourished patients based on the aforementioned criteria. The results showed that poor nutritional status significantly increased the incidence of infectious complications in the group receiving biological therapy. In the control group, although the rate of infectious complications was also higher among those with poor nutrition, it did not reach statistical significance. However, a multivariate analysis involving 140 patients revealed that poor nutrition remained an independent risk factor for post-operative infectious complications[10]. In a separate retrospective study conducted by Maeda et al[9], Onodera’s Prognostic Nutritional Index (OPNI) was utilized to assess the nutritional status of patients with CD. The OPNI is calculated using two parameters: Serum albumin concentration and total lymphocyte count [OPNI: (10 × serum albumin g/dL) + (0.005 × Total lymphocyte count)]. The findings of this study also supported the notion that malnutrition is an independent risk factor for SSI[9]. These studies collectively underscore the importance of addressing and managing malnutrition as a critical factor in reducing post-operative infectious complications in patients with IBD (Table 2).
| Ref. | Year | Cohort | Studies | Results |
| Maeda et al[9] | 2014 | CD | Retrospective 2005-2013 | Increased surgical site infections |
| Liu et al[19] | 2017 | CD | Retrospective 2014-2016 | Increased surgical site infection |
| Yamamoto et al[10] | 2019 | UC and CD | Case control | Increased infectious complications postoperatively; this becomes significant when associated with biologics |
Preoperative abscess: One retrospective study and a meta-analysis were conducted to investigate the impact of preoperative abscess on post-operative outcomes. Morar et al[21] conducted a retrospective study spanning 6 years, involving 163 patients who underwent ileocolonic surgeries for CD. The primary objective of the study was to determine the incidence of IASC within 30 d following surgery. The presence of an IAA or intraoperative sepsis was identified as an independent risk factor for developing IASC[21]. These findings align with the results of a meta-analysis conducted by Huang et al[5], which included a comprehensive analysis of 12 studies[5]. The meta-analysis further supported the association between the presence of preoperative abscess and an increased risk of adverse post-operative outcomes (Table 3).
Obesity: Obese patients with IBD face a higher risk of experiencing post-operative infectious complications, including wound infections and SSIs, when compared to overweight or non-obese patients. This finding has been substantiated by a systematic review and meta-analysis conducted by Jiang. The analysis encompassed 15 retrospective observational studies, which involved a total of 2294 obese patients with IBD and 1119 overweight patients with IBD. Obesity was defined as having a BMI greater than 30 kg/m2, while overweight was defined as having a BMI between 25 and 30 kg/m2. Patients with a BMI below 25 kg/m2 were classified as normal weight. When comparing overweight patients to normal weight patients, the overweight group exhibited an increased risk of wound complications, such as incisional hernia and fasciothesis, as well as sepsis. However, the overall complications did not demonstrate a statistically significant difference between the two groups. Conversely, when comparing obese patients (including overweight individuals) to non-obese patients, there was a notable increase in overall post-operative complications, with a particular emphasis on wound infections and SSIs[11]. These findings emphasize the importance of considering obesity as a significant risk factor for post-operative infectious complications in patients with IBD (Table 4).
| Ref. | Year | Cohort | Studies | Results |
| Jiang et al[11] | 2022 | IBD | Systematic review and meta-analysis of 15 retrospective observational studies | Obesity increases post-operative infection, wound infection and surgical site infection |
Perioperative blood transfusion: Perioperative allogenic blood transfusion has been identified as an independent risk factor for increasing infectious complications in patients undergoing surgery for IBD. Madbouly conducted a study involving 1202 patients with UC who underwent IPAA. Among the participants, 240 received allogenic blood transfusion within 2 wk prior to surgery or 48 h postoperatively (TRAN group), while 962 did not receive any transfusion (NON group). The study found that the overall incidence of infectious complications was significantly higher in the TRAN group compared to the NON group[12]. Similarly, Lan et al[13] conducted a cohort study involving 10100 patients with CD between 2005 and 2013. Of these patients, 611 received perioperative blood transfusion. The study evaluated the presence of various post-operative infections, including superficial, deep, organ or space SSIs, wound dehiscence, pneumonia, urinary tract infection, sepsis, or septic shock within 30 d of surgery. The findings revealed an increased rate of post-operative infections among patients who received intraoperative or post-operative blood transfusion. The multivariate analysis, incorporating other statistically significant factors identified in the univariate analysis, showed an odds ratio (OR) of 2.1 [95% confidence interval (CI): 1.7-2.6] for post-operative infections associated with blood transfusion. Furthermore, the overall OR for infection was 1.3 (95%CI: 1.2-1.5) for each unit of blood transfused intraoperatively, indicating a dose-dependent relationship[13]. These studies highlight the potential detrimental effects of perioperative allogenic blood transfusion on infectious complications in patients with IBD undergoing surgery. The findings underscore the importance of considering alternative strategies to minimize the need for blood transfusion and mitigate the associated risks in this patient population (Table 5).
5-ASA: A comprehensive analysis conducted by Law et al[14] combined data from six studies to compare the use of 5-ASA vs controls in a cohort comprising patients with both UC and CD[14]. The findings of the study indicated that the use of 5-ASA did not result in an overall increase in infectious complications.
Immunomodulators: The study conducted by Aberra et al[22] did not observe an increase in post-operative infectious complications when using immunomodulators, specifically mercaptopurine/azathioprine (MCP/AZP), compared to placebo[22]. Similarly, a meta-analysis conducted by Law et al[14], which included 31 studies, found no statistically significant difference between the group receiving immunomodulators and the group receiving no immunomodulators[14]. The OR was 1.11, with a 95%CI ranging from 0.97 to 1.26.
Corticosteroids: The retrospective studies conducted by Aberra et al[22] and Nguyen et al[23], as well as the prospective study by the REMIND group and the meta-analysis by Subramanian et al[24] and Law et al[14], have consistently demonstrated an association between the preoperative use of corticosteroids and increased post-operative infectious complications[14,22-25]. Aberra et al[22] retrospectively investigated the risk of post-operative infection in 159 UC and CD patients undergoing elective bowel surgery. They compared patients who received corticosteroids and/or MCP/AZP prior to surgery with those who did not. The study concluded that preoperative corticosteroid use was associated with an increase in overall infectious complications, but this was not observed when MCP/AZP alone was used[22]. Nguyen et al[23] conducted a retrospective study using the ACS NSQIP database from 2005 to 2012, including 8260 CD patients and 7235 UC patients. This study provided a robust analysis due to its large sample size and inclusion of both UC and CD patients. The results showed an increase in post-operative infectious complications, such as sepsis, septic shock, intra-abdominal infection, and wound dehiscence, with the use of steroids prior to surgery[23]. The REMIND group, led by Fumery et al[25], performed a prospective study involving 209 CD patients who underwent ileocecal resections in nine nationwide French IBD centers from 2010 to 2014. They found that exposure to corticosteroids four weeks before surgery was associated with an overall increase in complications, including IASC and extra-abdominal septic complications[25]. Subramanian et al[24] conducted a meta-analysis of seven observational studies involving 1532 patients with IBD. The analysis revealed an increased rate of post-operative infectious complications when corticosteroids were used preoperatively, particularly when the dosage exceeded 40 mg/day[25]. Law et al[14] conducted a comprehensive analysis of 35 studies comparing the preoperative use of corticosteroids with no corticosteroid treatment in patients with IBD. The findings consistently showed an increase in overall infectious complications. Subgroup analyses focusing on UC and CD patients yielded similar results[14]. Overall, these studies provide strong evidence supporting the association between preoperative corticosteroid use and increased risk of post-operative infectious complications in patients with IBD (Table 6).
| Ref. | Year | Cohort | Study | Results |
| Aberra et al[22] | 2003 | UC and CD; 159 patients | Retrospective 1999-2000 | Increased post-operative infection; No increase observed when 6 MCP/AZP were used |
| Nguyen et al[23] | 2014 | UC and CD; 15945 patients | Retrospective 2005-2012 | Increased post-operative infection |
| Fumery et al[25] (REMIND group) | 2017 | CD; 209 patients | Prospective study 2010-2014 | Increased overall post-operative complications, intra- and extra-abdominal septic complications |
| Subramanian et al[24] | 2008 | UC and CD | Meta-analysis; 7 studies | Increased infectious complications postoperatively and these increase with a dose of > 40 mg/day of corticosteroids |
| Law et al[14] | 2020 | UC and CD | Meta-analysis; 35 studies | Increased infectious complications and intra-abdominal infections |
Anti-interleukin antibodies 12/23 (Ustekinumab): A meta-analysis was conducted to assess the use of Ustekinumab (UST) administered 12 to 16 wk prior to surgery in CD patients. The analysis included five retrospective studies in CD patients, comparing UST to different treatment modalities: UST vs anti-TNF in two studies; UST vs Vedolizumab (VDZ); UST vs a combination of anti-TNF, VDZ, or no biologics; UST vs no biologics. The meta-analysis found that the post-operative infectious complication rate in the UST group was comparable to that of the VDZ or anti-TNF groups. However, in the study comparing UST to no biologics, an increased incidence of intra-abdominal sepsis was observed in the UST group. This finding could potentially be attributed to the higher use of preoperative immunomodulators in that group and a larger number of patients in the no biologics group undergoing laparoscopic procedures. It is important to note that this meta-analysis had some limitations, including the inclusion of retrospective studies from small tertiary care referral centers and inconsistencies in the time period of preoperative UST administration across the studies. Nevertheless, the overall conclusion of the meta-analysis was that the preoperative use of UST appears to be safe when compared to VDZ or anti-TNF therapies[26] (Table 7).
| Ref. | Year | Study | Patient cohort | Last dose taken | Overall results |
| Garg et al[26] | 2021 | Meta-analysis 5 retrospective studies; comparison of UST to either VDZ, anti-TNF or no biologics | Crohn disease | 16 wk | Relative safety of UST use preoperatively |
Anti-integrin antibodies (VDZ and Natalizumab): Law et al[14] conducted a comprehensive meta-analysis involving 5 studies, which included a total of 307 patients receiving VDZ, 490 patients receiving anti-TNF drugs, and 535 patients who did not receive any biologic agents. The findings of this analysis indicated that there were no significant differences in the rates of overall infectious complications among individuals treated with VDZ compared to those receiving anti-TNF agents or those without biologic exposure[27]. Another meta-analysis conducted by Yung et al[28] included 4 studies encompassing a total of 1080 patients with either CD or UC. These patients were exposed to VDZ, anti-TNF agents, or no biologics. The results of the analysis showed that UC patients who were exposed to VDZ had a significantly lower overall post-operative complication rate compared to those exposed to anti-TNF agents. However, no significant differences were observed in terms of infectious complications or SSIs between VDZ and anti-TNF treatments in both UC and CD patients. Furthermore, no significant differences were found between VDZ and no biologic treatment in terms of infectious or SSIs[28]. Guo et al[29] conducted a larger-scale meta-analysis involving 12 studies and a total of 1925 patients with IBD. Among these patients, 709 received VDZ, while the remaining patients received either anti-TNF therapy, no biologics, other biological therapies, UST, or placebo. The analysis revealed an overall decrease in infectious complications; however, there was an increase in specific site infections[29]. These meta-analyses provide valuable insights into the comparative effectiveness of VDZ and other treatments in terms of infectious complications in patients with IBD (Table 8).
| Ref. | Year | Patient cohort | Studies comparing VDZ to either anti-TNF or no biologics | Last dose of VDZ | Overall results |
| Law et al[27] | 2018 | IBD: UC and CD | 5 studies: UC only, retrospective; Retrospective; Retrospective; Post hoc analysis; Retrospective | Within 16 wk; Within 12 wk; Within 12 wk; N/A; Within 4 wk | No significant increase in post-operative infectious complications when compared to anti-TNF treatment or no biologics |
| Yung et al[28] | 2018 | IBD: UC and CD | 4 studies: UC only, retrospective; CD only, retrospective; Retrospective; Retrospective | 16 wk; 12 wk; 12 wk; 4 wk | No significant differences in infectious complications and SSI were noted in the group VDZ vs anti-TNF or no biologics; the results were similar in UC and CD patients |
| Guo et al[29] | 2021 | IBD: UC and CD | 12 studies | 4-16 wk | Decreased risk of overall post-operative infection complications; however, risk of infection at specific sites-SSI, deep SSI increased |
Anti-TNF Therapy (infliximab, adalimumab, certolizumab): The findings regarding the use of anti-TNF therapy, specifically infliximab (IFX), in the perioperative period of patients with IBD are conflicting and have been subject to extensive research. In a meta-analysis conducted by Billioud et al[30] in 2013, it was concluded that preoperative use of anti-TNF agents slightly increased overall post-operative complications in patients with IBD, particularly infectious complications in patients with CD[30]. Similarly, Ahmed Ali et al[31], in a meta-analysis, also found a higher risk of complications in CD patients receiving preoperative anti-TNF agents[31]. Narula et al[32] (15 studies) and Yang et al[33] (10 studies) performed separate meta-analyses, both reporting higher rates of post-operative infectious complications in CD patients who received IFX within 30 d prior to surgery[32,33]. However, a Cochrane systematic review conducted by Law et al[14] in 2020 found that there was an increase in infectious complications in CD patients when anti-TNF therapy was used within 8 wk of surgery, but no such increase was observed when the therapy was initiated earlier than 8 wk before surgery[14]. On the other hand, Xu et al’s meta-analysis in 2019, which included 1407 patients with CD treated with IFX preoperatively, found no significant difference in the rates of infectious complications compared to 4589 patients who did not receive the treatment[34]. Yang et al[35] analyzed 13 studies involving 2933 UC patients receiving IFX and similarly found no correlation between IFX therapy and post-operative morbidity[35]. Rosenfeld et al[36] also reported similar results in patients with CD[36]. Most of these studies had limitations, such as being retrospective, conducted at single centers, having significant heterogeneity, and small sample sizes. There were also confounding variables that were not adequately controlled, such as concomitant medical therapy, with steroid use known to increase the risk of infectious complications in patients with IBD in the perioperative period. To address the conflicting results and provide more definitive answers, the Postoperative Cohort of UC and CD PUCCINI trial was conducted. This prospective, observational, multicenter study aimed to determine whether anti-TNF therapy is an independent risk factor for post-operative infectious complications within 30 d of surgery in patients with IBD. The trial enrolled 947 patients from September 2014 to June 2017 who underwent abdominal surgery, with 382 patients receiving preoperative anti-TNF therapy (within 12 wk of surgery) and 573 patients who did not. Preoperative serum anti-TNF levels were measured and reported as either detectable or undetectable. The investigators found no significant increase in the risk of any infection or SSIs in the anti-TNF patients compared to those not receiving anti-TNF therapy. Secondary analyses also did not find any association between detectable serum anti-TNF levels and post-operative infections. The large prospective nature of the PUCCINI trial makes it a valuable source of information on the preoperative management of anti-TNF therapy in patients with IBD undergoing abdominal surgery[15] (Table 9).
| Ref. | Year | Cohort | Studies | Results |
| Billioud et al[30] | 2013 | UC an-d CD | Meta-analysis | Slight increase in overall post-operative complications, infectious complications in CD patients in particular |
| Ahmed Ali et al[31] | 2014 | CD | Meta-analysis | Increased wound infection and sepsis |
| Yang et al[33] | 2014 | CD | Meta-analysis; 10 studies | Modest increase in post-operative infectious complications |
| Narula et al[32] | 2013 | UC and CD | Meta-analysis; 15 studies | Modest increase in post-operative infectious complications |
| Law et al[14] | 2020 | UC and CD | Systematic review; Cochrane | Increased infectious complications in CD patients when treatment started within 8 wk of surgery |
| Yang et al[35] | 2012 | UC | Meta-analysis; 13 studies | No increase in post-operative early complications |
| Rosenfeld et al[36] | 2013 | CD | Systematic review and meta-analysis: 6 studies; 1159 patients | No significant difference in major complications noted between infliximab and control groups |
| Xu et al[34] | 2019 | CD | Meta-analysis: 14 studies for infectious complications | No increased risk of post-operative infection with preoperative infliximab |
| Cohen et al[15] | 2019 | UC and CD | Prospective | No increase in infection or SSI |
Small molecules (Tofacitinib): Limited data are available regarding the perioperative use of tofacitinib, a new addition in the treatment of moderate to severe UC. Law et al[14], in their Cochrane systematic review, did not identify any eligible studies specifically assessing the perioperative use of tofacitinib[14]. Therefore, further research is needed to evaluate its efficacy and safety in the perioperative setting.
Several studies have compared minimally invasive surgery to open surgery in the context of IBD, and the results have been conflicting.
Dasari et al[37] conducted a Cochrane systematic review that included 120 patients from 2 randomized controlled trials (RCTs). They found no significant differences in perioperative complications, such as wound infection, IAA, or anastomotic leak, when comparing minimally invasive surgery to open surgery. However, the study was limited by its small sample size[37].
In contrast, other studies have reported different findings. Lee performed a retrospective analysis from 2005 to 2009, including 1917 cases, of which 644 underwent laparoscopic procedures. The laparoscopic group had a significantly lower rate of post-operative sepsis compared to the open surgery group[38].
Patel et al[39] conducted a meta-analysis of 33 studies (including observational studies and RCTs) involving patients with CD undergoing surgery. The laparoscopic group (1079 patients) had a decreased risk of perioperative complications compared to the open surgery group (1221 patients). Subgroup analysis of 2 RCTs yielded similar results[39].
Wu et al[40] conducted a meta-analysis specifically focusing on patients with UC undergoing laparoscopic surgery. The overall complication rate was lower in the laparoscopic group compared to the open surgery group[40].
Lo et al[41] conducted a large retrospective cohort study involving 8644 patients with UC who underwent total abdominal colectomy without ileoanal anastomosis. They concluded that there was a decreased rate of post-operative sepsis/septic shock in both elective and emergent procedures in the laparoscopic group. Similar results were observed in patients on steroids who underwent laparoscopic surgery[41].
Another retrospective study by Hota et al[42] compared outcomes in open, laparoscopic, and robotic surgery for patients with CD. The rates of anastomotic leaks were higher in the open surgery group (5%) compared to the minimally invasive groups (laparoscopic: 3%, robotic: 7%), and post-operative wound infections were higher in open ileocecectomy (16%) compared to laparoscopic (9%) or robotic (7%) surgery[42].
Overall, the literature provides mixed evidence regarding the comparison of minimally invasive surgery to open surgery in IBD. Further research is needed to better understand the potential benefits and risks associated with each approach (Table 10).
| Ref. | Year | Cohort | Study | Results |
| Dasari et al[37] | 2011 | CD | Meta-analysis of 2 RCTs | No differences found in post-operative infectious complications |
| Lee et al[38] | 2012 | CD | Retrospective | Decreased sepsis in laparoscopic group |
| Patel et al[39] | 2013 | CD | Meta-analysis | Decreased infectious complications in laparoscopic group |
| Wu et al[40] | 2010 | UC | Meta-analysis and systematic review | Decreased total complication rate |
| Lo et al[41] | 2021 | UC | Retrospective | Decreased sepsis, even in patients on steroids |
| Hota et al[42] | 2021 | CD | Retrospective | Decreased anastomotic leaks and wound infections in minimally invasive group |
Management of IBD requires a multidisciplinary approach, and post-operative infection is a significant concern that can impact patient outcomes. Hypoalbuminemia, characterized by serum albumin levels below 30 g/L, is a key factor associated with poor surgical outcomes in patients with IBD. It leads to tissue edema, collagen synthesis disorders, and impaired immune function, increasing the risk of complications[8]. Meta-analyses by Vincent et al[43] and Huang et al[5] have demonstrated the independent association between severe hypoalbuminemia and post-operative infectious complications in patients with IBD undergoing surgery[5,43].
Malnutrition is prevalent in the IBD population, particularly in patients with CD. Various factors contribute to malnutrition, including increased nutritional requirements, nutrient losses, reduced dietary intake, and intestinal inflammation[44]. The European Society for Clinical Nutrition and Metabolism (ESPEN) recommends regular screening for malnutrition and the use of tools like the OPNI to assess nutritional status[9]. Malnutrition has been identified as an independent risk factor for adverse post-operative outcomes, specifically SSIs[9,10,19].
Optimizing nutritional status is crucial to reduce these complications. ESPEN guidelines recommend delaying surgery for malnourished patients and initiating intensive artificial feeding. Enteral feeding is preferred over parenteral nutrition, with parenteral nutrition considered after seven days of enteral feeding if protein requirements are not met or if the enteral route is contraindicated[45].
Assessing and correcting preoperative nutritional needs can lead to improved surgical outcomes. However, the optimal timing for preoperative optimization with enteral or parenteral nutrition remains uncertain.
One of the complications of CD is spontaneous IAA with an incidence ranging from 10%-30%[46]. It remains an independent risk factor for post-operative IASC in patients undergoing intestinal resection. IASC is a term that collectively describes anastomotic leaks, pus collection, and intra-abdominal abscesses[47].
The pathophysiology of spontaneous IAA in CD patients is related to the transmural inflammatory nature of the disease, leading to deep fissuring, ulceration, and eventually perforation or fistulae in the bowel wall. The presence of exudates on the surface of the inflamed bowel attracts adjacent bowel loops, resulting in the formation of a localized walled-off abscess within an inflammatory mass[48].
IAA can arise from different regions such as the ileocecal region, presenting as a right iliac fossa mass, or from sigmoid disease or ileosigmoid fistula, presenting on the left side. Pelvic abscesses are also common and primarily originate from the terminal ileum or sigmoid disease.
The conventional treatment approach for IAA involves initial surgical incision and drainage of the abscess, followed by definitive resection of the diseased bowel or fistula. However, surgery performed in the presence of an abscess increases the risk of septic complications. Therefore, managing an IAA with active CD requires a multidisciplinary approach.
Percutaneous drainage of the abscess, guided by ultrasound or computed tomography, serves as a bridge to elective surgery and allows time for supportive treatment. It is indicated for technically accessible, well-defined abscesses where interventional radiology is available. Müller-Wille et al[46], in a prospective study of 25 patients, found a statistically significant difference in post-operative IASC between the group that underwent percutaneous abscess drainage and the group that had no preoperative drainage[46]. Similar results were reported by El-Hussuna et al[48] and Xie et al[49] in their retrospective studies[48,49].
Based on the evidence, preoperative percutaneous drainage combined with antibiotics should be the first-line treatment for preoperatively detected IAA in order to avoid emergency surgery. Elective surgery can be planned after an interval of 2-4 wk to allow for complete resolution of the abscess and preoperative optimization[48].
Obesity, defined by the World Health Organization as a BMI ≥ 30 kg/m², is prevalent among patients with IBD, ranging from 15%-40%[11]. Obesity has long been associated with poor post-operative outcomes in general surgical procedures. Jiang et al[11], in their meta-analysis of 15 studies on patients with IBD, found that compared to non-obese patients (including overweight), obese patients had an increased rate of post-operative infectious complications[11].
This can be attributed to the fact that obese patients are at an increased risk of other comorbidities such as diabetes, hypertension, renal impairment, and atherosclerotic vascular disease, which contribute to overall post-operative outcomes. Additionally, obesity affects the immune system and homeostasis.
Obesity is characterized by a state of low-grade inflammation with elevated C-reactive protein (CRP) levels, even in the absence of inflammation or infection. Cytokines, neuropeptides, and adipocytokines produced in adipocytes, macrophages, and lymphocytes infiltrating mesenteric fat play a role in this inflammatory state. The overexpression of these inflammatory mediators in mesenteric fat of CD patients may contribute to the pathogenesis of CD and the increased risk of infection[50,51].
Furthermore, the pharmacokinetics of drugs used in IBD management, such as 5-ASA, corticosteroids, anti-TNF agents, and anti-integrin drugs, may be altered in obese patients, resulting in reduced efficacy and lower drug concentrations[52]. These factors collectively contribute to the increased risk of post-operative infectious complications observed in obese patients.
Allogenic perioperative blood transfusion is commonly used in patients with IBD to correct anemia and manage intraoperative bleeding. However, the adverse effects of blood transfusion on post-operative outcomes, particularly infectious complications, are often overlooked. Studies by Madbouly et al[12] and Lan et al[13] demonstrated that perioperative blood transfusion is an independent risk factor for post-operative septic complications. Preoperative transfusion aimed at correcting anemia may improve overall health status and reduce complications. Restricting transfusion to patients with hemoglobin levels below 8 g/dL and addressing preoperative anemia with erythropoietin and iron can help minimize adverse outcomes[12,13].
Aminosalicylates, which inhibit macrophage chemotaxis and promote proliferation of intestinal epithelial cells, have shown no significant difference in overall post-operative infectious complications[14]. Therefore, the use of aminosalicylates in the preoperative period is considered safe.
Immunomodulators do not increase post-operative infection rates, as indicated by studies conducted by Law et al[14]. However, earlier studies showed an increase in infectious complications, which may be confounded by the severity of the disease. As a result, immunomodulators do not need to be stopped prior to surgery[14].
Corticosteroids, despite their immunosuppressive effects, are a matter of concern in the preoperative period due to their impact on wound healing and increased risk of post-operative infectious complications. Multiple studies, including the TREAT Registry, the REMIND Group, and meta-analyses by Subramanian et al[24] and Law et al[14], have demon
UST, approved for CD treatment, has shown comparable rates of infectious complications to VDZ and anti-TNF agents in a meta-analysis by Garg et al[26] The role of UST in the treatment algorithm for IBD is still being determined[26,54,55].
VDZ, which targets leukocyte migration, has not shown a significant difference in post-operative infection rates compared to anti-TNF agents or other biologics in meta-analyses. Pharmacokinetic studies suggest that a longer withdrawal period is not necessary for patients on VDZ, and surgery can be safely performed even when the drug was administered every 8 or 4 wk after induction[29,56,57].
The perioperative use of anti-TNF agents in patients with IBD has yielded mixed results in retrospective, prospective, and meta-analyses studies. The prospective PUCCINI trial, along with other meta-analyses, indicates the safety of anti-TNF agents in the preoperative setting. Delaying surgery is unnecessary if the last infusion dose was received more than 4 wk prior to surgery, considering the drug’s clearance time (half-life: 7-14 d). Measuring serum anti-TNF levels preoperatively does not provide additional benefit[15].
Limited data exist on the perioperative use of Tofacitinib in patients with IBD. Guidelines from the 2017 ACR/AAHKS recommend stopping Tofacitinib 7 d prior to surgery and resuming it 14 d after surgery. However, in urgent or emergent cases, surgery should not be delayed to avoid increased post-operative complications[58].
In the pre-biological era, a significant proportion of patients with IBD required intestinal surgery within 10 years of diagnosis, with high rates of recurrence[3,58]. However, the introduction of biological therapies has led to a decline in the surgery rate[3,58]. Nonetheless, a considerable number of CD and UC patients still require surgery within 1 year[2,3,58]. The choice of surgical approach depends on the patient’s condition and disease severity[3,58]. Emergency settings often result in extended intestinal resection and a higher stoma rate, which are associated with increased post-operative infections[3,58]. Laparoscopic surgery is the preferred option but should be limited to specialized tertiary centers with expertise in this field[3,58]. Minimally invasive surgery offers advantages such as shorter hospital stays, improved cosmetic outcomes, reduced morbidity, and faster recovery[3,58]. Side-to-side anastomosis has shown superior outcomes compared to end-to-end anastomosis in terms of reducing post-operative anastomotic leaks[16,17,37,59]. Furthermore, it is crucial to consider the potential presence of differential diagnosis and extra-intestinal manifestations and its impact on the overall management of these patients[3,58-64]. Additionally, post-operative CD recurrence typically presents on a continuum from histologic findings to endoscopic findings to clinical presentation, underscoring the need for early monitoring and tailored pharmacologic therapy[3]. The advancement of effective medical treatments for CD has led to a tendency to consider surgical treatment as a last resort, but the choice between surgery and medical treatment is a patient’s personal preference under the guidance of the treating physician[2,3,58-60,65].
To guide the care of patients with IBD, an algorithm proposed by Zangenberg et al[65] can be followed. This involves assessing the patient’s hemodynamic status, diagnosing disease severity using flexible sigmoidoscopy, considering medical therapy with IV corticosteroids and subsequent anti-TNF agents in cases of systemic toxicity, withdrawing corticosteroids if surgery is required, and reserving routine antibiotic administration for cases involving percutaneous drainage of an intra-abdominal abscess[65].
There are some recently added medications in the therapeutic arsenal for the treatment of patients with IBD, and their role in post-operative complications is yet to be determined. Ozanimod, a selective sphingosine-1-phosphate receptor modulator, has shown effectiveness in inducing and maintaining remission in patients with UC[66,67]. Risankizumab, an interleukin (IL)-23 p19 inhibitor, has demonstrated efficacy as induction and maintenance therapy for CD and is also being investigated as a therapy for UC[68-70]. Upadacitinib, an oral selective Janus kinase inhibitor, has shown promise in both induction and maintenance therapy for CD and UC[71,72]. These recent clinical trials highlight the expanding treatment options for patients with IBD, potentially improving their quality of life and disease management.
In conclusion, in order to reduce post-operative infectious complications in patients with IBD, a comprehensive approach involving multiple disciplines is necessary. The analysis of the literature highlights several key strategies: Firstly, preoperative optimization should include nutritional risk screening to identify and address any malnutrition. Additionally, addressing preoperative anemia is important to minimize the need for blood transfusion during or after surgery. Steroids should be gradually withdrawn and tapered to reach physiological levels prior to the surgical procedure. Regarding medication management, thiopurines can be safely used in patients with IBD. While biological agents appear to be relatively safe, it is advisable to plan the timing of surgery in relation to the last dose of the drug.
Inflammatory bowel disease (IBD), including ulcerative colitis and Crohn’s disease, are chronic auto-inflammatory conditions marked by relapses and remissions, with increasing prevalence due to dietary changes. These diseases bring substantial physical, psychosocial, and economic burdens. Despite various available treatments, a significant proportion of patients require surgery within a decade of diagnosis. Surgical intervention poses challenges, particularly in emergency cases, with infectious complications being a major concern. Surgical approaches range from open procedures for emergencies to laparoscopic techniques for stable patients, aiming to minimize complications and hospital stays.
The study’s focus stems from the escalating IBD prevalence, the inadequacies of current treatments leading to surgeries, and the associated risk of post-operative infections. Addressing these issues is vital to enhance patient outcomes and reduce healthcare costs. Identifying risk factors linked to infections post-surgery, such as patient general status, preoperative abscess presence, obesity, and perioperative blood transfusions, is pivotal for preemptive measures. Understanding the impact of medications, such as steroids and anti-tumor necrosis factor (TNF), on post-operative complications is essential for informed treatment decisions. The significance lies in improving surgical practices and patient management, subsequently curbing infection-related morbidity and mortality.
This study primarily aims to investigate risk factors contributing to heightened post-operative infectious complications in IBD patients undergoing surgery. By systematically analyzing patient factors such as serum albumin levels, preoperative abscess presence, obesity, and perioperative blood transfusion requirements, the study aims to elucidate their role in infection susceptibility. Furthermore, the research delves into the impact of medications, specifically steroids and anti-TNF-α, on post-operative infection rates. Achieving these objectives will furnish insights into preoperative assessment and optimization strategies, influencing surgical decisions and post-operative care. Ultimately, the study’s significance lies in refining surgical practices and patient care to ameliorate post-operative morbidity, mortality, and overall quality of life in IBD patients undergoing surgery.
The systematic review adhered to PRISMA-P guidelines and aimed to explore existing literature related to post-operative infectious complications in IBD surgery. Searches were conducted in MEDLINE (PubMed) and Cochrane Library using keywords related to IBD, surgery, and infection. The retrieved data were categorized into complications, medications, and risk factors. Inclusion criteria encompassed patients aged over 18, diagnosed with IBD, undergoing abdominal surgery, and experiencing infectious complications within 30 d post-surgery. Exclusions included patients under 18, pregnant women, and complications occurring after 30 d. Selected studies included systematic reviews, retrospective/prospective cohort studies, and case-control studies in English and French. The chosen papers were analyzed to address questions about infectious complications, medication impact, and contributing factors. The results underwent narrative analysis to derive evidence-based factors leading to increased complications and offer management recommendations.
The research outcomes contribute significant insights into post-operative complications in patients with IBD. The study encompassed a rigorous selection process, yielding 70 articles for analysis. Categorizing results into distinct domains highlighted the critical aspects of risk factors and medication effects on post-operative outcomes. The investigation identified several noteworthy risk factors, including hypoalbuminemia, malnutrition, preoperative abscess, obesity, and perioperative blood transfusion. Hypoalbuminemia consistently emerged as a predictor of infectious complications, emphasizing its clinical relevance. Malnutrition, determined by weight loss and serum albumin, consistently heightened the risk of complications, highlighting its importance in patient management. Further analysis revealed the impact of medications. 5-aminosalicylates demonstrated no overall increase in infectious complications. Immunomodulators, corticosteroids, and anti-interleukin antibodies displayed varying associations with post-operative outcomes. While some studies suggested increased infectious risks, others contradicted these findings. Additionally, anti-TNF therapy’s impact showed conflicting results, possibly influenced by timing and patient population. The inclusion of large prospective trials such as Patients Undergoing Surgery to Identify Risk Factors for Postoperative Infection contributed valuable evidence regarding the safety of anti-TNF therapy. Comparing minimally invasive (laparoscopic and robotic) open surgery yielded mixed findings. While some studies reported reduced complications with minimally invasive approaches, others showed no significant differences. The field benefits from these insights, although further research is needed to clarify the optimal surgical approach. Overall, this research advances the understanding of post-operative complications in IBD patients. By comprehensively addressing risk factors and medication effects, the study guides clinical decision-making and highlights areas for future investigation.
This study contributes significant insights into the management of post-operative complications in patients with IBD. The findings underscore the importance of addressing risk factors such as hypoalbuminemia and malnutrition, which have been consistently associated with increased infectious complications following surgery. The study highlights the critical role of optimizing nutritional status, utilizing tools like Onodera’s Prognostic Nutritional Index, and considering interventions such as percutaneous drainage for managing intra-abdominal abscesses. Obesity’s impact on immune function and altered pharmacokinetics of IBD medications emphasize its association with post-operative infectious complications. The research also provides clarity regarding the use of various medications, including corticosteroids, immunomodulators, and biologics, in the preoperative period, offering valuable guidance for clinical practice.
Future research should delve deeper into the dynamics of nutritional interventions to mitigate infectious complications in IBD patients undergoing surgery. Longitudinal studies exploring the influence of personalized nutritional strategies on surgical outcomes are warranted. Additionally, further investigation into the role of emerging therapies such as ustekinumab, vedolizumab, and tofacitinib in the perioperative setting is essential. Prospective studies with larger cohorts are needed to definitively determine the impact of anti-TNF agents on post-operative infections in IBD patients. The ongoing evolution of IBD management, including the emergence of new medications like ozanimod, risankizumab, and upadacitinib, necessitates comprehensive studies to ascertain their effects on surgical outcomes. Future research directions should aim to refine treatment algorithms, considering individual patient characteristics and disease severity, ultimately enhancing patient care and minimizing post-operative complications.
We would like to extend our sincere appreciation to the Acute Medicine MSc program at the University of South Wales for their invaluable assistance in our work. We acknowledge and commend the University of South Wales for their commitment to providing advanced problem-solving skills and life-long learning opportunities for healthcare professionals.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Federação Brasileira De Gastroenterologia; Sociedade Brasileira de Endoscopia Digestiva; Grupo de Estudos da Doença Inflamatória Intestinal do Brasil.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Parra RS, Brazil; Zhu L, China; Madnani M, Bahrain S-Editor: Fan JR L-Editor: Webster JR P-Editor: Yuan YY
| 1. | Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, Panaccione R, Ghosh S, Wu JCY, Chan FKL, Sung JJY, Kaplan GG. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017;390:2769-2778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2677] [Cited by in RCA: 4432] [Article Influence: 492.4] [Reference Citation Analysis (111)] |
| 2. | Dall'Oglio VM, Balbinot RS, Muscope ALF, Castel MD, Souza TR, Macedo RS, Oliveira TB, Balbinot RA, Balbinot SS, Brambilla E, Soldera J. Epidemiological profile of inflammatory bowel disease in Caxias do Sul, Brazil: a cross-sectional study. Sao Paulo Med J. 2020;138:530-536. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Reference Citation Analysis (0)] |
| 3. | Ahmed Ali U, Kiran RP. Surgery for Crohn's disease: upfront or last resort? Gastroenterol Rep (Oxf). 2022;10:goac063. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 4. | Ghoneima AS, Flashman K, Dawe V, Baldwin E, Celentano V. High risk of septic complications following surgery for Crohn's disease in patients with preoperative anaemia, hypoalbuminemia and high CRP. Int J Colorectal Dis. 2019;34:2185-2188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 5. | Huang W, Tang Y, Nong L, Sun Y. Risk factors for postoperative intra-abdominal septic complications after surgery in Crohn's disease: A meta-analysis of observational studies. J Crohns Colitis. 2015;9:293-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 137] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 6. | Buskens CJ, Sahami S, Tanis PJ, Bemelman WA. The potential benefits and disadvantages of laparoscopic surgery for ulcerative colitis: A review of current evidence. Best Pract Res Clin Gastroenterol. 2014;28:19-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (1)] |
| 7. | Atasoy D, Aghayeva A, Aytaç E, Erenler İ, Çelik AF, Baca B, Karahasanoğlu T, Hamzaoğlu İ. Surgery for Intestinal Crohn's Disease: Results of a multidisciplinary approach. Turk J Surg. 2018;34:225-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Nguyen GC, Du L, Chong RY, Jackson TD. Hypoalbuminaemia and Postoperative Outcomes in Inflammatory Bowel Disease: the NSQIP Surgical Cohort. J Crohns Colitis. 2019;13:1433-1438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 57] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 9. | Maeda K, Nagahara H, Shibutani M, Otani H, Sakurai K, Toyokawa T, Tanaka H, Kubo N, Muguruma K, Kamata N, Yamagami H, Hirakawa K. A preoperative low nutritional prognostic index correlates with the incidence of incisional surgical site infections after bowel resection in patients with Crohn's disease. Surg Today. 2015;45:1366-1372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Yamamoto T, Shimoyama T, Umegae S, Kotze PG. Impact of Preoperative Nutritional Status on the Incidence Rate of Surgical Complications in Patients With Inflammatory Bowel Disease With Vs Without Preoperative Biologic Therapy: A Case-Control Study. Clin Transl Gastroenterol. 2019;10:e00050. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 11. | Jiang K, Chen B, Lou D, Zhang M, Shi Y, Dai W, Shen J, Zhou B, Hu J. Systematic review and meta-analysis: association between obesity/overweight and surgical complications in IBD. Int J Colorectal Dis. 2022;37:1485-1496. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 12. | Madbouly KM, Senagore AJ, Remzi FH, Delaney CP, Waters J, Fazio VW. Perioperative blood transfusions increase infectious complications after ileoanal pouch procedures (IPAA). Int J Colorectal Dis. 2006;21:807-813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Lan N, Stocchi L, Li Y, Shen B. Perioperative blood transfusion is associated with post-operative infectious complications in patients with Crohn's disease. Gastroenterol Rep (Oxf). 2018;6:114-121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Law CCY, Koh D, Bao Y, Jairath V, Narula N. Risk of Postoperative Infectious Complications From Medical Therapies in Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis. Inflamm Bowel Dis. 2020;26:1796-1807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (1)] |
| 15. | Cohen BL, Fleshner P, Kane SV, Herfarth HH, Palekar N, Farraye FA, Leighton JA, Katz J, Cohen RD, Gerich ME, Cross RK, Higgins PD, Tinsley A, Glover SC, Siegel CA, Bohl JL, Iskandar H, Raymond S, Huang R, Suarez-Farinas M, Sands BE. Anti-tumor necrosis factor therapy is not associated with post-operative infection: results from a prospective cohort of ulcerative colitis and Crohn's disease patients undergoing surgery to identify risk factors for post-operative infection I (PUCCINI). Gastroenterology. 2019;156 Suppl 1:S-80. [DOI] [Full Text] |
| 16. | Resegotti A, Astegiano M, Farina EC, Ciccone G, Avagnina G, Giustetto A, Campra D, Fronda GR. Side-to-side stapled anastomosis strongly reduces anastomotic leak rates in Crohn's disease surgery. Dis Colon Rectum. 2005;48:464-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 91] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 17. | Simillis C, Purkayastha S, Yamamoto T, Strong SA, Darzi AW, Tekkis PP. A meta-analysis comparing conventional end-to-end anastomosis vs. other anastomotic configurations after resection in Crohn's disease. Dis Colon Rectum. 2007;50:1674-1687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 152] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 18. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44932] [Cited by in RCA: 50084] [Article Influence: 10016.8] [Reference Citation Analysis (2)] |
| 19. | Liu S, Miao J, Wang G, Wang M, Wu X, Guo K, Feng M, Guan W, Ren J. Risk factors for postoperative surgical site infections in patients with Crohn's disease receiving definitive bowel resection. Sci Rep. 2017;7:9828. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 20. | Yang SS, Yu CS, Yoon YS, Yoon SN, Lim SB, Kim JC. Risk factors for complications after bowel surgery in Korean patients with Crohn's disease. J Korean Surg Soc. 2012;83:141-148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 21. | Morar PS, Hodgkinson JD, Thalayasingam S, Koysombat K, Purcell M, Hart AL, Warusavitarne J, Faiz O. Determining Predictors for Intra-abdominal Septic Complications Following Ileocolonic Resection for Crohn's Disease-Considerations in Pre-operative and Peri-operative Optimisation Techniques to Improve Outcome. J Crohns Colitis. 2015;9:483-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 89] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 22. | Aberra FN, Lewis JD, Hass D, Rombeau JL, Osborne B, Lichtenstein GR. Corticosteroids and immunomodulators: postoperative infectious complication risk in inflammatory bowel disease patients. Gastroenterology. 2003;125:320-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 239] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 23. | Nguyen GC, Elnahas A, Jackson TD. The impact of preoperative steroid use on short-term outcomes following surgery for inflammatory bowel disease. J Crohns Colitis. 2014;8:1661-1667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 99] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 24. | Subramanian V, Saxena S, Kang JY, Pollok RC. Preoperative steroid use and risk of postoperative complications in patients with inflammatory bowel disease undergoing abdominal surgery. Am J Gastroenterol. 2008;103:2373-2381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 187] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 25. | Fumery M, Seksik P, Auzolle C, Munoz-Bongrand N, Gornet JM, Boschetti G, Cotte E, Buisson A, Dubois A, Pariente B, Zerbib P, Chafai N, Stefanescu C, Panis Y, Marteau P, Pautrat K, Sabbagh C, Filippi J, Chevrier M, Houze P, Jouven X, Treton X, Allez M; REMIND study group investigators. Postoperative Complications after Ileocecal Resection in Crohn's Disease: A Prospective Study From the REMIND Group. Am J Gastroenterol. 2017;112:337-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 143] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 26. | Garg R, Mohan BP, Ponnada S, Regueiro M, Lightner AL, Click B. Postoperative outcomes after preoperative ustekinumab exposure in patients with Crohn's disease: a systematic review and meta-analysis. Ann Gastroenterol. 2021;34:691-698. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 27. | Law CCY, Narula A, Lightner AL, McKenna NP, Colombel JF, Narula N. Systematic Review and Meta-Analysis: Preoperative Vedolizumab Treatment and Postoperative Complications in Patients with Inflammatory Bowel Disease. J Crohns Colitis. 2018;12:538-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 69] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 28. | Yung DE, Horesh N, Lightner AL, Ben-Horin S, Eliakim R, Koulaouzidis A, Kopylov U. Systematic Review and Meta-analysis: Vedolizumab and Postoperative Complications in Inflammatory Bowel Disease. Inflamm Bowel Dis. 2018;24:2327-2338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 50] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 29. | Guo D, Jiang K, Hong J, Zhang M, Shi Y, Zhou B. Association between vedolizumab and postoperative complications in IBD: a systematic review and meta-analysis. Int J Colorectal Dis. 2021;36:2081-2092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 30. | Billioud V, Ford AC, Tedesco ED, Colombel JF, Roblin X, Peyrin-Biroulet L. Preoperative use of anti-TNF therapy and postoperative complications in inflammatory bowel diseases: a meta-analysis. J Crohns Colitis. 2013;7:853-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 161] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 31. | Ahmed Ali U, Martin ST, Rao AD, Kiran RP. Impact of preoperative immunosuppressive agents on postoperative outcomes in Crohn's disease. Dis Colon Rectum. 2014;57:663-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 70] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 32. | Narula N, Charleton D, Marshall JK. Meta-analysis: peri-operative anti-TNFα treatment and post-operative complications in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2013;37:1057-1064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 130] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 33. | Yang ZP, Hong L, Wu Q, Wu KC, Fan DM. Preoperative infliximab use and postoperative complications in Crohn's disease: a systematic review and meta-analysis. Int J Surg. 2014;12:224-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 108] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 34. | Xu Y, Yang L, An P, Zhou B, Liu G. Meta-Analysis: The Influence of Preoperative Infliximab Use on Postoperative Complications of Crohn's Disease. Inflamm Bowel Dis. 2019;25:261-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 35. | Yang Z, Wu Q, Wang F, Wu K, Fan D. Meta-analysis: effect of preoperative infliximab use on early postoperative complications in patients with ulcerative colitis undergoing abdominal surgery. Aliment Pharmacol Ther. 2012;36:922-928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 36. | Rosenfeld G, Qian H, Bressler B. The risks of post-operative complications following pre-operative infliximab therapy for Crohn's disease in patients undergoing abdominal surgery: a systematic review and meta-analysis. J Crohns Colitis. 2013;7:868-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 85] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 37. | Dasari BV, McKay D, Gardiner K. Laparoscopic versus Open surgery for small bowel Crohn's disease. Cochrane Database Syst Rev. 2011;CD006956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 68] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 38. | Lee Y, Fleming FJ, Deeb AP, Gunzler D, Messing S, Monson JR. A laparoscopic approach reduces short-term complications and length of stay following ileocolic resection in Crohn's disease: an analysis of outcomes from the NSQIP database. Colorectal Dis. 2012;14:572-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 73] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 39. | Patel SV, Patel SV, Ramagopalan SV, Ott MC. Laparoscopic surgery for Crohn's disease: a meta-analysis of perioperative complications and long term outcomes compared with open surgery. BMC Surg. 2013;13:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 81] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 40. | Wu XJ, He XS, Zhou XY, Ke J, Lan P. The role of laparoscopic surgery for ulcerative colitis: systematic review with meta-analysis. Int J Colorectal Dis. 2010;25:949-957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 41. | Lo BD, Stem M, Zhang GQ, Oduyale O, Brocke T, Efron JE, Atallah C, Safar B. The reduced risk of septic shock/sepsis with laparoscopic surgery among ulcerative colitis patients with preoperative chronic steroid use. Surgery. 2021;170:1047-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 42. | Hota S, Parascandola S, Smith S, Tampo MM, Amdur R, Obias V. Robotic and laparoscopic surgical techniques in patients with Crohn's disease. Surg Endosc. 2021;35:4602-4608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 43. | Vincent JL, Dubois MJ, Navickis RJ, Wilkes MM. Hypoalbuminemia in acute illness: is there a rationale for intervention? A meta-analysis of cohort studies and controlled trials. Ann Surg. 2003;237:319-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 422] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 44. | Triantafillidis JK, Papalois AE. The role of total parenteral nutrition in inflammatory bowel disease: current aspects. Scand J Gastroenterol. 2014;49:3-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 45. | Forbes A, Escher J, Hébuterne X, Kłęk S, Krznaric Z, Schneider S, Shamir R, Stardelova K, Wierdsma N, Wiskin AE, Bischoff SC. ESPEN guideline: Clinical nutrition in inflammatory bowel disease. Clin Nutr. 2017;36:321-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 342] [Cited by in RCA: 444] [Article Influence: 44.4] [Reference Citation Analysis (0)] |
| 46. | Müller-Wille R, Iesalnieks I, Dornia C, Ott C, Jung EM, Friedrich C, Schill G, Hoffstetter P, Zorger N, Schreyer AG. Influence of percutaneous abscess drainage on severe postoperative septic complications in patients with Crohn's disease. Int J Colorectal Dis. 2011;26:769-774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 47. | Yamamoto T, Allan RN, Keighley MR. Risk factors for intra-abdominal sepsis after surgery in Crohn's disease. Dis Colon Rectum. 2000;43:1141-1145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 270] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 48. | El-Hussuna A, Karer MLM, Uldall Nielsen NN, Mujukian A, Fleshner PR, Iesalnieks I, Horesh N, Kopylov U, Jacoby H, Al-Qaisi HM, Colombo F, Sampietro GM, Marino MV, Ellebæk M, Steenholdt C, Sørensen N, Celentano V, Ladwa N, Warusavitarne J, Pellino G, Zeb A, Di Candido F, Hurtado-Pardo L, Frasson M, Kunovsky L, Yalcinkaya A, Tatar OC, Alonso S, Pera M, Granero AG, Rodríguez CA, Minaya A, Spinelli A, Qvist N. Postoperative complications and waiting time for surgical intervention after radiologically guided drainage of intra-abdominal abscess in patients with Crohn's disease. BJS Open. 2021;5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 49. | Xie Y, Zhu W, Li N, Li J. The outcome of initial percutaneous drainage versus surgical drainage for intra-abdominal abscesses in Crohn's disease. Int J Colorectal Dis. 2012;27:199-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 50. | Boutros M, Maron D. Inflammatory bowel disease in the obese patient. Clin Colon Rectal Surg. 2011;24:244-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 51. | Karagiannides I, Pothoulakis C. Substance P, obesity, and gut inflammation. Curr Opin Endocrinol Diabetes Obes. 2009;16:47-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 52. | Singh S, Dulai PS, Zarrinpar A, Ramamoorthy S, Sandborn WJ. Obesity in IBD: epidemiology, pathogenesis, disease course and treatment outcomes. Nat Rev Gastroenterol Hepatol. 2017;14:110-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 339] [Article Influence: 37.7] [Reference Citation Analysis (0)] |
| 53. | Lichtenstein GR, Feagan BG, Cohen RD, Salzberg BA, Diamond RH, Price S, Langholff W, Londhe A, Sandborn WJ. Serious infection and mortality in patients with Crohn's disease: more than 5 years of follow-up in the TREAT™ registry. Am J Gastroenterol. 2012;107:1409-1422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 536] [Cited by in RCA: 614] [Article Influence: 43.9] [Reference Citation Analysis (0)] |
| 54. | Sands BE, Sandborn WJ, Panaccione R, O'Brien CD, Zhang H, Johanns J, Adedokun OJ, Li K, Peyrin-Biroulet L, Van Assche G, Danese S, Targan S, Abreu MT, Hisamatsu T, Szapary P, Marano C; UNIFI Study Group. Ustekinumab as Induction and Maintenance Therapy for Ulcerative Colitis. N Engl J Med. 2019;381:1201-1214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 498] [Cited by in RCA: 905] [Article Influence: 129.3] [Reference Citation Analysis (1)] |
| 55. | Feagan BG, Sandborn WJ, Gasink C, Jacobstein D, Lang Y, Friedman JR, Blank MA, Johanns J, Gao LL, Miao Y, Adedokun OJ, Sands BE, Hanauer SB, Vermeire S, Targan S, Ghosh S, de Villiers WJ, Colombel JF, Tulassay Z, Seidler U, Salzberg BA, Desreumaux P, Lee SD, Loftus EV Jr, Dieleman LA, Katz S, Rutgeerts P; UNITI-IM-UNITI Study Group. Ustekinumab as Induction and Maintenance Therapy for Crohn's Disease. N Engl J Med. 2016;375:1946-1960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1467] [Cited by in RCA: 1421] [Article Influence: 142.1] [Reference Citation Analysis (0)] |
| 56. | Rosario M, Dirks NL, Milch C, Parikh A, Bargfrede M, Wyant T, Fedyk E, Fox I. A Review of the Clinical Pharmacokinetics, Pharmacodynamics, and Immunogenicity of Vedolizumab. Clin Pharmacokinet. 2017;56:1287-1301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 128] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 57. | Sandborn WJ, Feagan BG, Rutgeerts P, Hanauer S, Colombel JF, Sands BE, Lukas M, Fedorak RN, Lee S, Bressler B, Fox I, Rosario M, Sankoh S, Xu J, Stephens K, Milch C, Parikh A; GEMINI 2 Study Group. Vedolizumab as induction and maintenance therapy for Crohn's disease. N Engl J Med. 2013;369:711-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1416] [Cited by in RCA: 1624] [Article Influence: 124.9] [Reference Citation Analysis (1)] |
| 58. | Lee KE, Cantrell S, Shen B, Faye AS. Post-operative prevention and monitoring of Crohn's disease recurrence. Gastroenterol Rep (Oxf). 2022;10:goac070. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 59. | Goodman SM, Springer B, Guyatt G, Abdel MP, Dasa V, George M, Gewurz-Singer O, Giles JT, Johnson B, Lee S, Mandl LA, Mont MA, Sculco P, Sporer S, Stryker L, Turgunbaev M, Brause B, Chen AF, Gililland J, Goodman M, Hurley-Rosenblatt A, Kirou K, Losina E, MacKenzie R, Michaud K, Mikuls T, Russell L, Sah A, Miller AS, Singh JA, Yates A. 2017 American College of Rheumatology/American Association of Hip and Knee Surgeons Guideline for the Perioperative Management of Antirheumatic Medication in Patients With Rheumatic Diseases Undergoing Elective Total Hip or Total Knee Arthroplasty. J Arthroplasty. 2017;32:2628-2638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 68] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 60. | De Simone B, Davies J, Chouillard E, Di Saverio S, Hoentjen F, Tarasconi A, Sartelli M, Biffl WL, Ansaloni L, Coccolini F, Chiarugi M, De'Angelis N, Moore EE, Kluger Y, Abu-Zidan F, Sakakushev B, Coimbra R, Celentano V, Wani I, Pintar T, Sganga G, Di Carlo I, Tartaglia D, Pikoulis M, Cardi M, De Moya MA, Leppaniemi A, Kirkpatrick A, Agnoletti V, Poggioli G, Carcoforo P, Baiocchi GL, Catena F. WSES-AAST guidelines: management of inflammatory bowel disease in the emergency setting. World J Emerg Surg. 2021;16:23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 61. | Ballotin VR, Bigarella LG, Riva F, Onzi G, Balbinot RA, Balbinot SS, Soldera J. Primary sclerosing cholangitis and autoimmune hepatitis overlap syndrome associated with inflammatory bowel disease: A case report and systematic review. World J Clin Cases. 2020;8:4075-4093. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 62. | Brambilla B, Barbosa AM, Scholze CDS, Riva F, Freitas L, Balbinot RA, Balbinot S, Soldera J. Hemophagocytic Lymphohistiocytosis and Inflammatory Bowel Disease: Case Report and Systematic Review. Inflamm Intest Dis. 2020;5:49-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 63. | Kanika A, Soldera J. Pulmonary cytomegalovirus infection: A case report and systematic review. World J Meta-Anal. 2023;11:151-166. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (6)] |
| 64. | da Cruz ER, Forno AD, Pacheco SA, Bigarella LG, Ballotin VR, Salgado K, Freisbelen D, Michelin L, Soldera J. Intestinal Paracoccidioidomycosis: Case report and systematic review. Braz J Infect Dis. 2021;25:101605. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 65. | Zangenberg MS, Horesh N, Kopylov U, El-Hussuna A. Preoperative optimization of patients with inflammatory bowel disease undergoing gastrointestinal surgery: a systematic review. Int J Colorectal Dis. 2017;32:1663-1676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 66. | Sandborn WJ, Feagan BG, D'Haens G, Wolf DC, Jovanovic I, Hanauer SB, Ghosh S, Petersen A, Hua SY, Lee JH, Charles L, Chitkara D, Usiskin K, Colombel JF, Laine L, Danese S; True North Study Group. Ozanimod as Induction and Maintenance Therapy for Ulcerative Colitis. N Engl J Med. 2021;385:1280-1291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 368] [Article Influence: 73.6] [Reference Citation Analysis (0)] |
| 67. | Feagan BG, Schreiber S, Afzali A, Rieder F, Hyams J, Kollengode K, Pearlman J, Son V, Marta C, Wolf DC, D'Haens GG. Ozanimod as a novel oral small molecule therapy for the treatment of Crohn's disease: The YELLOWSTONE clinical trial program. Contemp Clin Trials. 2022;122:106958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 68. | Ferrante M, Panaccione R, Baert F, Bossuyt P, Colombel JF, Danese S, Dubinsky M, Feagan BG, Hisamatsu T, Lim A, Lindsay JO, Loftus EV Jr, Panés J, Peyrin-Biroulet L, Ran Z, Rubin DT, Sandborn WJ, Schreiber S, Neimark E, Song A, Kligys K, Pang Y, Pivorunas V, Berg S, Duan WR, Huang B, Kalabic J, Liao X, Robinson A, Wallace K, D'Haens G. Risankizumab as maintenance therapy for moderately to severely active Crohn's disease: results from the multicentre, randomised, double-blind, placebo-controlled, withdrawal phase 3 FORTIFY maintenance trial. Lancet. 2022;399:2031-2046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 228] [Article Influence: 57.0] [Reference Citation Analysis (0)] |
| 69. | D'Haens G, Panaccione R, Baert F, Bossuyt P, Colombel JF, Danese S, Dubinsky M, Feagan BG, Hisamatsu T, Lim A, Lindsay JO, Loftus EV Jr, Panés J, Peyrin-Biroulet L, Ran Z, Rubin DT, Sandborn WJ, Schreiber S, Neimark E, Song A, Kligys K, Pang Y, Pivorunas V, Berg S, Duan WR, Huang B, Kalabic J, Liao X, Robinson A, Wallace K, Ferrante M. Risankizumab as induction therapy for Crohn's disease: results from the phase 3 ADVANCE and MOTIVATE induction trials. Lancet. 2022;399:2015-2030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 274] [Article Influence: 68.5] [Reference Citation Analysis (0)] |
| 70. | Almradi A, Hanzel J, Sedano R, Parker CE, Feagan BG, Ma C, Jairath V. Clinical Trials of IL-12/IL-23 Inhibitors in Inflammatory Bowel Disease. BioDrugs. 2020;34:713-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 77] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 71. | Loftus EV Jr, Panés J, Lacerda AP, Peyrin-Biroulet L, D'Haens G, Panaccione R, Reinisch W, Louis E, Chen M, Nakase H, Begun J, Boland BS, Phillips C, Mohamed MF, Liu J, Geng Z, Feng T, Dubcenco E, Colombel JF. Upadacitinib Induction and Maintenance Therapy for Crohn's Disease. N Engl J Med. 2023;388:1966-1980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 283] [Article Influence: 94.3] [Reference Citation Analysis (0)] |
| 72. | Danese S, Vermeire S, Zhou W, Pangan AL, Siffledeen J, Greenbloom S, Hébuterne X, D'Haens G, Nakase H, Panés J, Higgins PDR, Juillerat P, Lindsay JO, Loftus EV Jr, Sandborn WJ, Reinisch W, Chen MH, Sanchez Gonzalez Y, Huang B, Xie W, Liu J, Weinreich MA, Panaccione R. Upadacitinib as induction and maintenance therapy for moderately to severely active ulcerative colitis: results from three phase 3, multicentre, double-blind, randomised trials. Lancet. 2022;399:2113-2128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 393] [Article Influence: 98.3] [Reference Citation Analysis (0)] |