Published online Jun 27, 2021. doi: 10.4240/wjgs.v13.i6.537
Peer-review started: February 7, 2021
First decision: March 16, 2021
Revised: March 29, 2021
Accepted: June 2, 2021
Article in press: June 2, 2021
Published online: June 27, 2021
Processing time: 130 Days and 21.9 Hours
Pancreato-biliary disorders are still incredibly challenging in the field of gastroenterology, as they would sometimes require multi-approach interventional procedures. Recently, therapeutic interventional endoscopic ultrasound (EUS) has emerged as a potential alternative to surgical or percutaneous approaches. Unfortunately, considering the high cost of EUS, lack of facility and expertise, most gastroenterologists still often refer cases to undergo surgical interventions without contemplating the possibility of utilizing EUS first. EUS-guided biliary drainage has become one of the best choices for establishing access to biliary system, given the clear visualization of pancreas, gallbladder, and common bile duct. Although there are still only a few studies which directly compare EUS-guided and surgical approaches for biliary drainage, current evidence demonstr
Core Tip: Pancreato-biliary disorders sometimes require multi-approach interventional procedures. Therapeutic interventional endoscopic ultrasound (EUS) has emerged as a potential alternative to surgical or percutaneous approach. Application of EUS-guided approach resulted in lower adverse events and re-intervention rates, with similar high technical and clinical success rates in comparison to percutaneous and surgical approaches, especially in patients with history of failed endoscopic retrograde cholangiopancreatography attempt. Comparison between EUS-guided and surgical approach in pancreatic fluid collection drainage demonstrated commensurable success rates and shorter length of hospital stay in favor of EUS-guided approach. Application of EUS is a potential field in replacing surgery to manage gastric outlet obstruction.
- Citation: Lesmana CRA, Paramitha MS, Gani RA. Therapeutic interventional endoscopic ultrasound in pancreato-biliary disorders: Does it really replace the surgical/percutaneous approach? World J Gastrointest Surg 2021; 13(6): 537-547
- URL: https://www.wjgnet.com/1948-9366/full/v13/i6/537.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v13.i6.537
In Western countries and some developed Asian countries, endoscopic ultrasound (EUS) has been demonstrated as an encouraging development for diagnostic, as well as, therapeutic modality throughout these years. Pancreato-biliary disorders are still incredibly challenging in the field of gastroenterology, as they would require comprehensive assessment, good diagnostic performance, and sometimes multi-approach interventional procedures. Recently, therapeutic interventional EUS has emerged as a potential alternative to surgical and percutaneous approaches, such as EUS-guided biliary drainage (EUS-BD), EUS-guided pancreatic fluid collection (PFC) drainage, and EUS-guided gastro-jejunostomy (EUS-GJ). Unfortunately, considering the high cost of EUS, lack of facility and expertise, most gastroenterologists still often refer cases to undergo surgical interventions without contemplating the possibility of utilizing EUS first. Additionally, the superiority of percutaneous approaches as a less invasive op
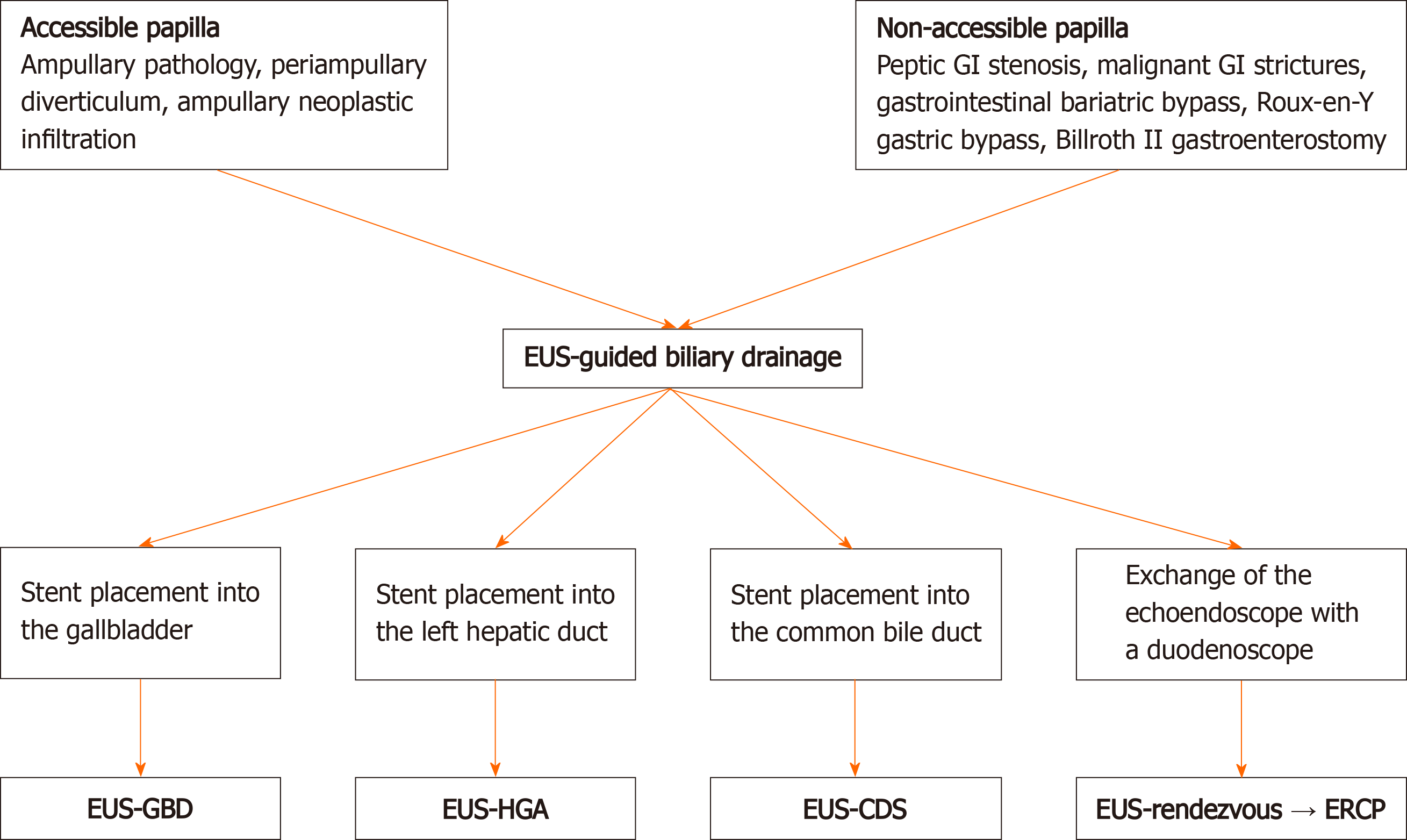
EUS-BD has become one of the best choices for establishing access to biliary system, given the clear visualization of pancreas, gallbladder, and common bile duct (CBD). The access established by EUS-BD allows endoscopic retrograde cholangiopancreatography (ERCP) to be performed through rendezvous technique (EUS-RV) in the cases of failed cannulation during conventional ERCP when the second part of duodenum and the papilla can still be accessed easily. Meanwhile, the intrahepatic approach, EUS-guided hepatogastrostomy (EUS-HGA) or antegrade stent placement is usually conducted in cases of malignant gastric outlet obstruction where the papilla cannot be accessed easily with scope, or in patients with altered anatomy (e.g., post Whipple procedure). Failed selective cannulation of common biliary duct due to tight distal CBD stenosis or neoplasm (e.g., pancreatic head cancer) can be approached with EUS-guided choledochoduodenostomy (EUS-CDS) technique. EUS-guided drainage can also be advantageous for malignant biliary obstruction by lowering the possibility of adverse effects related to long-term percutaneous drainage tubes and as an alternative to surgical therapies in high-risk patients with many co-morbidities[3,4].
Choosing the most appropriate technique for EUS-BD can be challenging because it needs to be adjusted with the clinical background and long-term management plan for the patients. As one of the techniques for EUS-BD, rendezvous technique is conducted by using EUS scope to insert a wire into biliary tree. This technique consists of several steps. Firstly, the wire can be inserted through the duodenum by trans-duodenal biliary rendezvous (TD-BR) method or through the stomach by trans-gastric transhepatic biliary rendezvous (TGTH-BR). After the wire has been introduced, the EUS scope will be changed into a duodenoscope, and biliary cannulation will be attempted again. Several technical challenges can be encountered while performing TD-BR, such as appropriate positioning of the scope in the duodenum in order to ensure the caudal orientation of needle puncture, difficult structural anomalies (stricture, anastomosis), possibility of dislodging the wire, removing EUS scope without losing the wire access, retrieving the end of the wire through channel of the scope or removal of the scope from the mouth of the patient, and ensuring the cannulation is conducted properly after reaching the papillary orifice. Conditions, in which technical difficulties may be encountered with TGTH-BR, include advancement of the wire according to the position of distal bile duct, lowering the risk of leakage and bleeding since the access to the intrahepatic duct needs to be established across the gastric wall and liver, and deployment of stent. Another technique, which can be done entirely with EUS scope, is EUS-guided trans-gastric and trans-hepatic antegrade drainage. In this technique, the wire is introduced into a branch of left intrahepatic duct across surgical biliary anastomosis. The stent will then be located anterograde across the intended anatomical location[3,4].
Several promising results have been demonstrated with the application of EUS-RV. In the case of failed selective biliary cannulation, EUS-RV can be conducted as a salvage method. A review of case series reported by Isayama et al[5] showed 74% of overall success rate from 247 cases with 11% of total complication rate. Several major complications which could be found were bile leakage, bleeding, peritonitis, pancreatitis, and pneumoperitoneum. The authors also compared various approach routes and concluded that the trans-gastric route had a lower tendency to cause bile leakage compared to the trans-duodenal route. Trans-gastric route also demonstrated a good guide-wire stability after the scope is withdrawn. A single-center retrospective study in 39 subjects who underwent EUS-RV after failed ERCP also showed similar technical success rate (78.6%) with slightly higher complication rate (16.7%) compared to the previous evidence. In this study, the most common reasons of failed EUS-RV were kinking of a guidewire and failure of passing through the strictures[6]. To our knowledge, there has not been any study which directly compares the effectiveness of EUS-RV to surgical approaches in pancreatobiliary disorders. A literature review by Vanbrugghe et al[7] exhibited the possible advantage of EUS-RV in managing late post-operative complication from pancreatoduodenectomy in the form of pancreatico-enteric anastomotic stenosis. The success rate of EUS-RV technique in treating this condition may reach up to 85%.
On the other hand, direct EUS-BD technique is performed by making an anastomosis between gastrointestinal tract and biliary tree. There are two common approaches in direct EUS-BD technique, i.e., EUS-CDS, which is done by making an anastomosis between duodenum and CBD, and EUS-HGA, which is done by making an anastomosis between stomach and left lobe of the liver. The important aspects to be considered in both techniques are the position of the scope, the puncture towards target site, and the placement of the stent[3].
Generally, self-expanding metal stent (SEMS), which was initially designed for ERCP, can be placed uncovered, partially covered, or fully covered for EUS-BD[4]. Nonetheless, recently, the use of lumen apposing metal stent (LAMS) for EUS-CDS has been significantly noticed. Particularly, cautery-assisted LAMS is known to decrease the risk of pneumoperitoneum and bile leakage during EUS-CDS by applying a cutting current by electro-cautery tip of the catheter when the catheter is inserted into the CBD. The application of one catheter system also reduces the duration of access and deployment of the stent[8,9]. Nevertheless, how to maintain the visualization of duct and/or gallbladder during the deployment of LAMS, as well as the possibilities of leakage and perforation by electro-cautery tip still become a problem in the application of direct EUS-BD[3].
Potential adverse events, clinical success rates, and technical difficulties of EUS-BD still become significant contributors to EUS-related morbidity, especially in comparison with other modalities. A meta-analysis by Sharaiha et al[10] demonstrated significantly higher clinical success, fewer adverse events, and fewer re-intervention rates in EUS-BD application compared to percutaneous transhepatic biliary drainage (PTBD) when ERCP fails to provide biliary drainage. Similarly, high success rate was also demonstrated by another meta-analysis, with low-rate of overall procedure-related complications (18.04%) in EUS-BD procedure performed in patients with inoperable malignant biliary strictures who experienced failed ERCP attempt[11]. In contrast, a 2-year retrospective study conducted in a tertiary referral private hospital in Indonesia showed no significant difference in technical and clinical success rates between EUS-BD and PTBD for advanced malignant biliary obstruction. In the same study, the median survival of patients who underwent PTBD also tended to be higher. Despite the type of procedure, shorter survival rate was significantly affected by the presence of metastasis[12]. Comparable result was also obtained from a retrospective study performed by Khashab et al[13], in which higher technical and clinical success rates were observed from PTBD compared to EUS-BD, but with lower number of adverse events and shorter length of hospital stay in EUS-BD. Another retrospective study by Téllez-Ávila et al[14] indicated higher technical and clinical success rates with lower number of complications and shorter length of hospital stay in patients treated with EUS-BD compared to PTBD. Nevertheless, the overall technical and clinical success rates in EUS-BD have been proven to be remarkable in both operable and non-operable biliary obstruction cases, suggesting that EUS-BD can be an alternative approach if surgical approach is not feasible to be performed[15,16]. Additionally, a comparison between EUS-BD and ERCP as the first line approach for inoperable malignant biliary obstruction also demonstrated superiority of EUS-BD, which was shown in higher success rates and lower number of complications[17]. A prospective randomized trial comparing malignant distal biliary obstruction cases (with history of previous failed ERCP attempt) demonstrated similar success rates and complications between EUS-CDS and surgical hepaticojejunostomy. Nonetheless, the median survival was higher and 90-d mortality rate was lower in patients treated with EUS-CDS, suggesting its potential over surgery or percutaneous approaches[18,19] (Table 1).
| Ref. | Design | Cases | Number of patients | Success rates | Complication rate |
| Tyberg et al[15] | Retrospective study | Patients with biliary obstruction who failed conventional ERCP | 52 | Technical success rate: 96%. Clinical success rate: 77% | Adverse events: 10% |
| Khashab et al[13] | Retrospective comparative cohort study | Patients who underwent EUS-BD or PTBD with distal malignant biliary obstruction after at least one failed ERCP attempt | 73 | Technical success rate: EUS-BD vs PTBD: 86.4% vs 100%. Clinical success rate: EUS-BD vs PTBD: 86.4% vs 92.2% | Adverse events: EUS-BD vs PTBD: 18.2% vs 39.2%. Re-intervention: EUS-BD vs PTBD: 15.7% vs 80.4% |
| Sharaiha et al[10] | Systematic review and meta-analysis | Patients who underwent EUS-BD or PTBD with biliary obstruction and failure of ERCP to obtain drainage | 483 | Technical success rate: OR 1.78 (P = 0.25). Clinical success rate: OR 0.45 (P = 0.66) in favor of EUS-BD | Adverse events: OR 0.23 (P = 0.02). Re-intervention: OR 0.13 (P = 0.77) in favor of EUS-BD |
| Téllez-Ávila et al[14] | Retrospective comparative study | Patients who underwent EUS-BD or PTBD with biliary obstruction and had at least one previous failed ERCP attempt or difficulty in accessing the second portion of duodenum | 90 | Technical success rate: EUS-BD vs PTBD: 90% vs 78% (P = 0.3). Clinical success rate: EUS-BD vs PTBD: 96% vs 63% (P = 0.04) | Complications: EUS-BD vs PTBD: 6.6% vs 28% (P = 0.04). Length of hospital stay: EUS-BD vs PTBD: 6.5 d vs 12.5 d (P = 0.009) |
| Poincloux et al[16] | Retrospective study | Patients with malignant and benign biliary obstruction with previous failed ERCP attempt who underwent EUS intra- or extra-hepatic approach with transluminal stenting or rendezvous procedure with trans-papillary stent placement | 101 | Technical success rate: 98%. Clinical success rate: 92.1% | Adverse event rate: 11.9%. Six procedure-related deaths |
| Lesmana et al[12] | Retrospective study | Patients with advanced malignant biliary obstruction, who underwent EUS-BD after failed ERCP attempt | 38 | Technical success rate: EUS-BD vs PTBD: 87.5%% vs 86.7% (P = 1.000). Clinical success rate: EUS-BD vs PTBD: 62.5% vs 93.3% (P = 0.5) | Adverse events: EUS-BD vs PTBD: 1 patient vs 0 patient |
| Han et al[17] | Systematic review and meta-analysis | Patients with malignant distal biliary obstruction who underwent EUS-BD with transmural metal stenting or ERCP for primary palliative treatment | 756 | Technical success rate: EUS-BD vs ERCP: 94.8% vs 96.5%. Clinical success rate: EUS-BD vs ERCP: 93.8% vs 95.7% | Adverse event rate: EUS-BD vs ERCP: 16.3% vs 18.3% |
| Moole et al[11] | Systematic review and meta-analysis | Patients with inoperable malignant biliary strictures with a failed ERCP attempt, who underwent EUS-BD or PTBD | 528 | Success rate: EUS-BD vs PTBD (pooled OR): 3.06 | Risk difference for overall procedure-related complications in EUS-BD vs PTBD: -0.21. Relative risk for infectious complications and bile leak: EUS-BD vs PTBD: 0.25 vs 0.33 |
| Artifon et al[18] | Prospective and randomized trial | Patients with unresectable malignant distal biliary obstruction (with history of failed standard ERCP) treated with EUS-guided choledochoduodenostomy (EUS-CDT) or surgical biliary bypass or hepaticojejunostomy (HJT) | 32 | Technical success rates: EUS-CDT vs HJT: 88% vs 94% (P = 0.598). Clinical success rates: EUS-CDT vs HJT: 71% vs 93% (P = 0.169) | Complication rates: EUS-CDT vs HJT: 21.42% vs 13.33% (P = 0.651). Median survival: EUS-CDT vs HJT: 82.36 d vs 82.27 d. 90-d mortality: EUS-CDT vs HJT: 42.9% vs 60% (P = 0.389) |
The limitations of EUS-BD, which have been widely addressed, are particularly related to operational expertise and limited tools and devices (e.g., stents, guide wires) available for EUS-BD[11,12]. The availability of hands-on-training and structured EUS training program in a wider scale is still required since it is critical for the operator to understand the basic skills of performing endoscopy, ultrasound imaging, knowledge of human anatomy, and knowledge of the accessories to be used in order to avoid possible life-threatening complications, for instance, bile leakage, bleeding, or bowel perforation[1].
Cholecystitis is also one of the challenging biliary disorders as it can result in biliary sepsis, and perforated gallbladder. In the case of severe cholecystitis with biliary sepsis or empyema, percutaneous cholecystostomy has become the first management approach, especially in patients with unstable clinical condition. Recently, EUS-guided gallbladder drainage (EUS-GBD) has emerged as a treatment of choice, especially in cholecystitis patients who are not able to undergo cholecystectomy. The access to gallbladder is established through duodenal or gastric wall. In comparison to percutaneous gallbladder drainage (PTGBD), EUS-GBD has been associated with higher technical (90%-98%) and clinical (89%-97%) success rates[2]. This is partly because tube dislodgement often occurs as a complication of PTGBD procedure. Another study, comparing the performance of EUS-GBD and PTGBD in acute cholecystitis patients, showed similar technical success with lower post-procedural adverse events with EUS-GBD[11]. EUS-GBD has also been correlated with shorter hospital stays and significantly lower number of re-interventions (P = 0.005) or unplanned re-admissions rates (P = 0.003) in patients with acute cholecystitis compared to percutaneous cholecystostomy[20].
A variety of stents has been introduced in the application of EUS, which includes plastic stents, SEMSs, and lumen-apposing metal stents (LAMSs). Nowadays, the preferred stent to be used in EUS-GBD procedure is LAMS due to its width, lumen apposition, and practical deployment[2]. Previous clinical evidence showed the possibility of EUS-GBD with LAMS as a safe and effective procedure with high pooled technical and clinical success rates (93.86% and 92.48%, respectively) with acceptable stent-related complication rate (8.16%)[21]. A systematic review by Anderloni et al[22] showed no significant differences in technical and clinical success rates between SEMSs and LAMSs in high-risk patients with acute cholecystitis (98.6% vs 91.5% and 94.4% vs 90.1%, respectively). The frequency of adverse events, however, was lower in LAMSs (9.9%) compared to SEMSs (12.3%). Overall, the EUS-BD approach is determined by the accessibility of papilla and the location of stent placement[4] (Figure 1).
The most common implementation of EUS in managing pancreatic problems is through drainage of PFCs, such as from pseudocysts and walled-off necrosis. Encapsulated fluid and necrotic collections can occur as localized complications of pancreatitis. The fluid collection is commonly located in the peripancreatic retroperitoneal space next to the stomach and duodenum. It may, however, spread retroperitoneally into the pelvic region or intraperitoneally to mesentery. As a result, multidisciplinary approach is necessary to manage these problems comprehensively. EUS-guided drainage of PFCs can be performed for the pseudocyst, while endoscopic debridement or necrosectomy can be utilized to treat the solid necrosis component of walled-off necrosis. Several indications for drainage are the presence of infection, signs of gastric outlet obstruction, persistent abdominal pain, failure to thrive, biliary obstruction, or large sized non-resolving PFCs[23].
Aside from more appropriate evaluation of the PFC, EUS also serves as an appropriate tool to identify a good needle trajectory by evaluating the transmural vasculature. In addition, the results of EUS-guided PFCs continue to improve as the knowledge about stent placement also advances. Currently, the use of LAMSs is widely proposed to conquer the limitations of plastic and/or SEMSs. As a new cautery-enhanced stent, LAMS can perform electrocautery and provide an access through a puncture at the same step. LAMS also has 2 anchoring ends which can improve the migration process. Although high technical success rate (93.5%-93.9%) has been demonstrated from previous studies for pancreatic pseudocysts and walled-off necrosis[24,25], higher overall adverse event rate was also observed in groups treated with LAMS (41.9%), especially in walled-off necrosis cases[25]. Another meta-analysis by Mohan, et al also stated that no superiority was demonstrated by LAMS in the drainage of pancreatic walled-off necrosis in comparison to plastic stents (clinical success rates: 88.5% vs 88.1%) with slightly lower overall adverse events in LAMS (11.2% vs 15.9%, P = 0.38)[26]. On the other hand, a retrospective study comparing LAMS and double pigtail plastic stents in the management of pancreatic walled-off necrosis indicated better resolution (86.9 d vs 133.6 d, P = 0.038) with lower recurrence rate in LAMS (6.3% vs 23.1%, P = 0.032). Interestingly, this study also indicated lower requirement for surgical treatment in the utilization of LAMS when compared to traditional surgical cyst-enterostomy procedure (0% vs 12.8%, P = 0.031), since no patients in the study needed to undergo surgical necrosectomy after initial LAMS cyst-enterostomy procedure[27]. Further evidence showing superiority of LAMS compared to plastic stents in pancreatic walled-off necrosis was established by Chen et al[28], showing higher clinical success rate in LAMS (80.4% vs 57.5%, P = 0.001) and higher necessity for surgical approach in the use of plastic stents (16.1% in plastic stents vs 5.6% in LAMS, P = 0.02). The most common adverse event from utilizing LAMS is bleeding due to mechanical trauma and/or infection due to occluded lumen of the stent in the necrotic cavity. An approach to reduce the risk of these complications is by placing coaxial plastic stents throughout the lumen of LAMS[29].
As a less invasive technique with lower recurrence rate when compared to percutaneous approach, endoscopic approach has been contemplated as a replacement of surgical approach throughout these years[30]. Comparable results between endoscopic and surgical approaches for pancreatic pseudocysts have been exhibited through two meta-analyses[30,31]. Shorter length of hospital stay, however, was shown by endoscopic approach[32]. Another meta-analysis by Szakó et al[31] demonstrated lower success rate of endoscopic approach but shorter length of hospital stays and similar mortality rates when compared to surgical approach (Table 2).
| Ref. | Design | Cases | Number of patients | Technical success rate | Complication rate |
| Farias et al[30] | Systematic review and meta-analysis | Pancreatic pseudocysts | 342 | Risk difference: -0.09 (P = 0.07) | Drainage-related adverse events: risk difference: -0.02 (P = 0.48). General adverse events: risk difference: -0.05 (P = 0.13). |
| Szakó et al[31] | Meta-analysis | Pseudocysts and walled-off necrosis | 842-896 | OR 0.59 (P = 0.022): lower clinical success of endoscopic approach | Mortality: OR 0.86 (P = 0.870): similar result. Post-operative length of hospital stay: -3.67 (P < 0.001) |
| Varadarajulu et al[32] | Randomized trial | Pancreatic pseudocysts | 40 | Risk difference: -5% (P = 0.5) | Risk difference: -10% (P = 0.24). Median of hospital stay: -4 days (P < 0.001): shorter in endoscopic cytogastrostomy |
Related to the complications of pancreatic tumors or malignant distal CBD with duodenal infiltration, a mechanical obstruction of the distal stomach or proximal duodenum may occur. As a result, EUS application in the creation of gastroenterostomy or jejunostomy to tackle this problem has also emerged with endoscopic intrinsic stent placement as the standard of care. Nowadays, there are three methods of EUS-guided gastroenterostomy (EUS-GE) with placement of a LAMS: Direct EUS-GE, assisted EUS-GE, and EUS-guided double balloon occluded gastrojejunostomy bypass (EPASS). Since direct EUS-GE procedure involves a puncture of small bowel loop from the stomach, the risk of leakage or perforation is also higher since it requires the correct puncturing of the loop. Meanwhile, assisted EUS-GE technique requires jejunal loops to be distended distal to the location of the stricture with infusion of normal saline through an endoscope or by passing and inflating a balloon over a wire into the jejunum. Lastly, EPASS technique requires oral insertion of special double-balloon enteric tube (filled with normal saline) over a wire (Figure 2)[33]. Complications of this procedure may include perforation, pneumoperitoneum, bleeding, and stent migration[23]. Regardless, a systematic review involving 285 patients who underwent EUS-GE procedure showed high technical [92%, 95% confidence interval (CI): 88-95] and clinical (90%, 95%CI: 85-94) success rates with low number of recurrence of symptoms or unintentional re-intervention (9%, 95%CI: 8-16)[34].
As an alternative to surgical therapy, EUS-GE and EUS-GJ showed potentially promising results. In a multicenter retrospective study comparing between EUS-GE and surgical gastrojejunostomy, although higher technical success rate was shown by surgical gastrojejunostomy (100% vs 87% in EUS-GE, P = 0.009), similar clinical success rate, as well as lower adverse event and symptoms recurrence rate were found from groups treated with EUS-GE[35]. Significantly lower adverse event rate in EUS-GJ was also implicated by Perez-Miranda et al[36], in comparison to laparoscopic gastrojejunostomy, even though the authors also address the technical difficulties of performing EUS-GJ. A recent systematic review and meta-analysis by Jayaraj et al[37] also supported the previous findings by providing significantly lower overall adverse event rate in EUS-GE groups compared to the groups treated with surgical gastroenterostomy. The technical and clinical success rates between both groups were comparable. Similarly, a recent single-center retrospective study also reported that significant faster resumption of oral intake and shorter length of hospital stay were observed in EUS-GE group in comparison with open gastrojejunostomy group. No significant difference was observed in technical and clinical success rates, as well as symptoms recurrence and 30-d readmission rates[38] (Table 3).
| Ref. | Design | Cases | Number of patients | Technical success rate | Complication rate |
| Khashab et al[35] | Retrospective study | Patients with malignant gastric outlet obstruction who underwent EUS-GE or surgical gastrojejunostomy (SGJ) | 93 | Technical success rate: EUS-GE vs SGJ: 87% vs 100% (P = 0.009). Clinical success rate: EUS-GE vs SGJ: 87% vs 90% (P = 0.8) | Recurrence rate: EUS-GE vs SGJ: 3% vs 14% (P = 0.2). Adverse event rate: EUS-GE vs SGJ: 16% vs 25% (P = 0.3). Length of stay: EUS-GE vs SGJ: 11.6 ± 6.6 d vs 12 ± 8.2 d (P = 0.35) |
| Perez-Miranda et al[36] | Retrospective study | Patients with gastric outlet obstruction who underwent EUS-guided gastrojejunostomy (EUS-GJ) or laparoscopic gastrojejunostomy (Lap-GJ) | 54 | Technical success rate: EUS-GJ vs Lap-GJ: 88% vs 100% (P = 0.11). Clinical success rate: EUS-GJ vs Lap-GJ: 84% vs 90% (P = 0.11) | Adverse event rate: EUS-GJ vs Lap-GJ: 12% vs 41% (P = 0.0386) |
| Jayaraj et al[37] | Systematic review and meta-analysis | Patients with malignant gastric outlet obstruction who underwent EUS-GE and surgical GE | 171 | Technical success rate: pooled OR: 0.16 (P = 0.033). Clinical success rate: pooled OR: 0.98 (P = 0.984) | Overall adverse event rate: pooled OR: 0.35 (P = 0.014) |
| Kouanda et al[38] | Retrospective study | Patients with gastric outlet obstruction who underwent EUS-GE or open gastrojejunostomy (OGJ) | 66 | Technical success rate: EUS-GE vs OGJ: 92.5% vs 100% (P = 0.15) | Recurrence of the symptoms: EUS-GE vs OGJ: 17.5% vs 19.2% (P = 0.34). Re-intervention rate: EUS-GE vs OGJ: 20% vs 11.5% (P = 0.78). Resumption of oral intake: EUS-GE vs OGJ: 1.3 d vs 4.7 d (P < 0.001). Length of hospital stay: EUS-GE vs OGJ: 5 d vs 14.5 d (P < 0.001). 30-d readmission rate: EUS-GE vs OGJ: 17.5% vs 24.1% (P = 0.37) |
As a rapidly evolving field, studies about therapeutic interventional EUS continue to emerge in pancreato-biliary disorders. Encouraging evidence of interventional EUS as an alternative approach to percutaneous method or as a possible option to put major surgery as the second choice of treatment, has been demonstrated by comparable technical and success rates, as well as lower adverse event rate. Introduction of multiple devices for EUS-guided thermal ablation is also considered as a potentially safer technique since it minimizes damage to the surrounding organs. Cost-effectiveness, however, still becomes a challenge in many interventional EUS methods. Moreover, additional training or advanced endoscopy fellowship, as well as sufficient facilities, are compulsory to perform interventional EUS since the procedure still carries potential risks.
| 1. | Lesmana CRA, Ho KY. Training of interventional endoscopic ultrasonography (EUS) in pancreato-biliary disorders: An Asian perspective. Digest System. 2018;2:1-2. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | DeWitt JM, Arain M, Chang KJ, Sharaiha R, Komanduri S, Muthusamy VR, Hwang JH; AGA Center for GI Innovation and Technology. Interventional Endoscopic Ultrasound: Current Status and Future Directions. Clin Gastroenterol Hepatol. 2021;19:24-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (1)] |
| 3. | Yarmohammadi H, Covey AM. Percutaneous biliary interventions and complications in malignant bile duct obstruction. Chin Clin Oncol. 2016;5:68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Salerno R, Davies SEC, Mezzina N, Ardizzone S. Comprehensive review on EUS-guided biliary drainage. World J Gastrointest Endosc. 2019;11:354-364. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 28] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Isayama H, Nakai Y, Kawakubo K, Kawakami H, Itoi T, Yamamoto N, Kogure H, Koike K. The endoscopic ultrasonography-guided rendezvous technique for biliary cannulation: a technical review. J Hepatobiliary Pancreat Sci. 2013;20:413-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Okuno N, Hara K, Mizuno N, Hijioka S, Tajika M, Tanaka T, Ishihara M, Hirayama Y, Onishi S, Niwa Y, Yamao K. Endoscopic Ultrasound-guided Rendezvous Technique after Failed Endoscopic Retrograde Cholangiopancreatography: Which Approach Route Is the Best? Intern Med. 2017;56:3135-3143. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Vanbrugghe C, Campanile M, Caamaño A, Pol B. Management of delayed stenosis of pancreatico-enteric anastomosis following pancreatoduodenectomy. J Visc Surg. 2019;156:30-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Binmoeller KF, Shah J. A novel lumen-apposing stent for transluminal drainage of nonadherent extraintestinal fluid collections. Endoscopy. 2011;43:337-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 172] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 9. | El Chafic AH, Shah JN, Hamerski C, Binmoeller KF, Irani S, James TW, Baron TH, Nieto J, Romero RV, Evans JA, Kahaleh M. EUS-Guided Choledochoduodenostomy for Distal Malignant Biliary Obstruction Using Electrocautery-Enhanced Lumen-Apposing Metal Stents: First US, Multicenter Experience. Dig Dis Sci. 2019;64:3321-3327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 69] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 10. | Sharaiha RZ, Khan MA, Kamal F, Tyberg A, Tombazzi CR, Ali B, Tombazzi C, Kahaleh M. Efficacy and safety of EUS-guided biliary drainage in comparison with percutaneous biliary drainage when ERCP fails: a systematic review and meta-analysis. Gastrointest Endosc. 2017;85:904-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 299] [Article Influence: 33.2] [Reference Citation Analysis (2)] |
| 11. | Moole H, Bechtold ML, Forcione D, Puli SR. A meta-analysis and systematic review: Success of endoscopic ultrasound guided biliary stenting in patients with inoperable malignant biliary strictures and a failed ERCP. Medicine (Baltimore). 2017;96:e5154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 77] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 12. | Lesmana CRA, Gani RA, Hasan I, Sulaiman AS, Ho KY, Dhir V, Lesmana LA. Palliative Endoscopic Ultrasound Biliary Drainage for Advanced Malignant Biliary Obstruction: Should It Replace the Percutaneous Approach? Case Rep Gastroenterol. 2019;13:385-397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Khashab MA, Valeshabad AK, Afghani E, Singh VK, Kumbhari V, Messallam A, Saxena P, El Zein M, Lennon AM, Canto MI, Kalloo AN. A comparative evaluation of EUS-guided biliary drainage and percutaneous drainage in patients with distal malignant biliary obstruction and failed ERCP. Dig Dis Sci. 2015;60:557-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 162] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 14. | Téllez-Ávila FI, Herrera-Mora D, Duarte-Medrano G, Lopez-Arce G, Lindoro-Barraza D, Casanova I, Elizondo-Rivera J, Ramírez-Luna M, Valdovinos-Andraca F. Biliary Drainage in Patients With Failed ERCP: Percutaneous Versus EUS-guided Drainage. Surg Laparosc Endosc Percutan Tech. 2018;28:183-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 15. | Tyberg A, Desai AP, Kumta NA, Brown E, Gaidhane M, Sharaiha RZ, Kahaleh M. EUS-guided biliary drainage after failed ERCP: a novel algorithm individualized based on patient anatomy. Gastrointest Endosc. 2016;84:941-946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 58] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 16. | Poincloux L, Rouquette O, Buc E, Privat J, Pezet D, Dapoigny M, Bommelaer G, Abergel A. Endoscopic ultrasound-guided biliary drainage after failed ERCP: cumulative experience of 101 procedures at a single center. Endoscopy. 2015;47:794-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 149] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 17. | Han SY, Kim SO, So H, Shin E, Kim DU, Park DH. EUS-guided biliary drainage vs ERCP for first-line palliation of malignant distal biliary obstruction: A systematic review and meta-analysis. Sci Rep. 2019;9:16551. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 63] [Article Influence: 9.0] [Reference Citation Analysis (1)] |
| 18. | Artifon EL, Loureiro JF, Baron TH, Fernandes K, Kahaleh M, Marson FP. Surgery or EUS-guided choledochoduodenostomy for malignant distal biliary obstruction after ERCP failure. Endosc Ultrasound. 2015;4:235-243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 19. | Khan MA, Atiq O, Kubiliun N, Ali B, Kamal F, Nollan R, Ismail MK, Tombazzi C, Kahaleh M, Baron TH. Efficacy and safety of endoscopic gallbladder drainage in acute cholecystitis: Is it better than percutaneous gallbladder drainage? Gastrointest Endosc. 2017;85:76-87.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 98] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 20. | Luk SW, Irani S, Krishnamoorthi R, Wong Lau JY, Wai Ng EK, Teoh AY. Endoscopic ultrasound-guided gallbladder drainage vs percutaneous cholecystostomy for high risk surgical patients with acute cholecystitis: a systematic review and meta-analysis. Endoscopy. 2019;51:722-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 76] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 21. | Kalva NR, Vanar V, Forcione D, Bechtold ML, Puli SR. Efficacy and Safety of Lumen Apposing Self-Expandable Metal Stents for EUS Guided Cholecystostomy: A Meta-Analysis and Systematic Review. Can J Gastroenterol Hepatol. 2018;2018:7070961. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 22. | Anderloni A, Buda A, Vieceli F, Khashab MA, Hassan C, Repici A. Endoscopic ultrasound-guided transmural stenting for gallbladder drainage in high-risk patients with acute cholecystitis: a systematic review and pooled analysis. Surg Endosc. 2016;30:5200-5208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 124] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 23. | Simons-Linares CR, Chahal P. Advances in Interventional Endoscopic Ultrasound (EUS): A Technical Review. J Clin Gastroenterol. 2020;54:579-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Chen YI, Khashab MA, Adam V, Bai G, Singh VK, Bukhari M, Brewer Gutierrez O, Elmunzer BJ, Moran RA, Fayad L, El Zein M, Kumbhari V, Repici A, Barkun AN. Plastic stents are more cost-effective than lumen-apposing metal stents in management of pancreatic pseudocysts. Endosc Int Open. 2018;6:E780-E788. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 25. | Bang JY, Navaneethan U, Hasan MK, Sutton B, Hawes R, Varadarajulu S. Non-superiority of lumen-apposing metal stents over plastic stents for drainage of walled-off necrosis in a randomised trial. Gut. 2019;68:1200-1209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 293] [Cited by in RCA: 261] [Article Influence: 37.3] [Reference Citation Analysis (0)] |
| 26. | Mohan BP, Jayaraj M, Asokkumar R, Shakhatreh M, Pahal P, Ponnada S, Navaneethan U, Adler DG. Lumen apposing metal stents in drainage of pancreatic walled-off necrosis, are they any better than plastic stents? Endosc Ultrasound. 2019;8:82-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 49] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 27. | Ge PS, Young JY, Jirapinyo P, Dong W, Ryou M, Thompson CC. Comparative Study Evaluating Lumen Apposing Metal Stents Versus Double Pigtail Plastic Stents for Treatment of Walled-Off Necrosis. Pancreas. 2020;49:236-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 28. | Chen YI, Yang J, Friedland S, Holmes I, Law R, Hosmer A, Stevens T, Franco MC, Jang S, Pawa R, Mathur N, Sejpal DV, Inamdar S, Trindade AJ, Nieto J, Berzin TM, Sawhney M, DeSimone ML, DiMaio C, Kumta NA, Gupta S, Yachimski P, Anderloni A, Baron TH, James TW, Jamil LH, Ona MA, Lo SK, Gaddam S, Dollhopf M, Bukhari MA, Moran R, Gutierrez OB, Sanaei O, Fayad L, Ngamruengphong S, Kumbhari V, Singh V, Repici A, Khashab MA. Lumen apposing metal stents are superior to plastic stents in pancreatic walled-off necrosis: a large international multicenter study. Endosc Int Open. 2019;7:E347-E354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 72] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 29. | Puga M, Consiglieri CF, Busquets J, Pallarès N, Secanella L, Peláez N, Fabregat J, Castellote J, Gornals JB. Safety of lumen-apposing stent with or without coaxial plastic stent for endoscopic ultrasound-guided drainage of pancreatic fluid collections: a retrospective study. Endoscopy. 2018;50:1022-1026. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 65] [Article Influence: 8.1] [Reference Citation Analysis (1)] |
| 30. | Farias GFA, Bernardo WM, De Moura DTH, Guedes HG, Brunaldi VO, Visconti TAC, Gonçalves CVT, Sakai CM, Matuguma SE, Santos MELD, Sakai P, De Moura EGH. Endoscopic vs surgical treatment for pancreatic pseudocysts: Systematic review and meta-analysis. Medicine (Baltimore). 2019;98:e14255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 7.3] [Reference Citation Analysis (1)] |
| 31. | Szakó L, Mátrai P, Hegyi P, Pécsi D, Gyöngyi Z, Csupor D, Bajor J, Erőss B, Mikó A, Szakács Z, Dobszai D, Meczker Á, Márta K, Rostás I, Vincze Á. Endoscopic and surgical drainage for pancreatic fluid collections are better than percutaneous drainage: Meta-analysis. Pancreatology. 2020;20:132-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 32. | Varadarajulu S, Bang JY, Sutton BS, Trevino JM, Christein JD, Wilcox CM. Equal efficacy of endoscopic and surgical cystogastrostomy for pancreatic pseudocyst drainage in a randomized trial. Gastroenterology 2013; 145: 583-90. e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 370] [Cited by in RCA: 338] [Article Influence: 26.0] [Reference Citation Analysis (2)] |
| 33. | Troncone E, Fugazza A, Cappello A, Del Vecchio Blanco G, Monteleone G, Repici A, Teoh AYB, Anderloni A. Malignant gastric outlet obstruction: Which is the best therapeutic option? World J Gastroenterol. 2020;26:1847-1860. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 47] [Cited by in RCA: 80] [Article Influence: 13.3] [Reference Citation Analysis (4)] |
| 34. | Iqbal U, Khara HS, Hu Y, Kumar V, Tufail K, Confer B, Diehl DL. EUS-guided gastroenterostomy for the management of gastric outlet obstruction: A systematic review and meta-analysis. Endosc Ultrasound. 2020;9:16-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 114] [Cited by in RCA: 115] [Article Influence: 19.2] [Reference Citation Analysis (1)] |
| 35. | Khashab MA, Bukhari M, Baron TH, Nieto J, El Zein M, Chen YI, Chavez YH, Ngamruengphong S, Alawad AS, Kumbhari V, Itoi T. International multicenter comparative trial of endoscopic ultrasonography-guided gastroenterostomy vs surgical gastrojejunostomy for the treatment of malignant gastric outlet obstruction. Endosc Int Open. 2017;5:E275-E281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 125] [Cited by in RCA: 176] [Article Influence: 19.6] [Reference Citation Analysis (2)] |
| 36. | Perez-Miranda M, Tyberg A, Poletto D, Toscano E, Gaidhane M, Desai AP, Kumta NA, Fayad L, Nieto J, Barthet M, Shah R, Brauer BC, Sharaiha RZ, Kahaleh M. EUS-guided Gastrojejunostomy Versus Laparoscopic Gastrojejunostomy: An International Collaborative Study. J Clin Gastroenterol. 2017;51:896-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 179] [Article Influence: 19.9] [Reference Citation Analysis (1)] |
| 37. | Jayaraj M, Singh DP, Gopalakrishnan R, Naveen P, Narala S, Krishnamoorthi R. EUS-guided gastroenterostomy (GE) vs surgical gastroenterostomy for patients with malignant gastric outlet obstruction: A systematic review and meta-analysis. Am J Gastroenterol. 2019;114:S510-S512. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 38. | Kouanda A, Binmoeller K, Hamerski C, Nett A, Bernabe J, Watson R. Endoscopic ultrasound-guided gastroenterostomy vs open surgical gastrojejunostomy: clinical outcomes and cost effectiveness analysis. Surg Endosc. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Indonesia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sugiura R S-Editor: Gao CC L-Editor: A P-Editor: Li JH