Published online Nov 27, 2021. doi: 10.4240/wjgs.v13.i11.1509
Peer-review started: April 11, 2021
First decision: June 17, 2021
Revised: July 2, 2021
Accepted: October 11, 2021
Article in press: October 11, 2021
Published online: November 27, 2021
Processing time: 228 Days and 23.5 Hours
One of the most popular bariatric procedures is sleeve gastrectomy, and it has become significantly more common in recent years.
To evaluate the research activity in sleeve gastrectomy over the last two decades, and to visualize the hot spots and emerging trends in this type of bariatric surgery using bibliometric methods.
The Scopus database was used to search for publications related to sleeve gastrectomy. The retrieved publications were reviewed in terms of year of publication, type of study, country of origin, institutions, journals, and citation patterns by using descriptive analysis. Collaboration network and term co-occurrence analysis were visualized by using VOSviewer software.
The search strategy yielded a total of 6508 publications on sleeve gastrectomy from 2001 to 2020. As regards the document type, the majority were articles (n = 5230; 80.36%), followed by reviews (n = 544; 8.36%). The top three countries are the United States, with 1983 publications (30.47%), followed by France (600; 9.22%) and Italy (417; 6.71%). The most cited publication was published in 2012 by Schauer et al in the New England Journal of Medicine (n = 1435 citations). This publication found that weight loss was greater in the sleeve gastrectomy group than in the medical therapy group. Furthermore, this study demonstrated that 12 mo of medical therapy plus bariatric surgery greatly improved glycemic regulation in obese patients with uncontrolled type 2 diabetes compared with medical therapy alone. The focus of the current literature on sleeve gastrectomy was directed toward several themes such as morbidity and potential complications, the complexity of the procedure and different surgical approaches, and diabetes and body mass index in correlation to sleeve gastrectomy.
The number of sleeve gastrectomy publications has gradually grown over the last 20 years. This bibliometric analysis could help researchers better understand the knowledge base and research frontiers surrounding sleeve gastrectomy. In addition, future studies may focus on emerging research hotspots.
Core Tip: One of the most popular bariatric procedures is sleeve gastrectomy, and it has become significantly more common in recent years. Therefore, this study intends to evaluate the research activity in sleeve gastrectomy over the last two decades and quantitatively estimate the hot spots and emerging trends in this type of bariatric surgery with bibliometric methods and enable researchers to identify new areas for potential development. The current literature on sleeve gastrectomy was directed toward several themes such as morbidity and potential complications, the complexity of the procedure and different surgical approaches, and diabetes mellitus and body mass index in correlation with sleeve gastrectomy.
- Citation: Barqawi A, Abushamma FA, Akkawi M, Al-Jabi SW, Shahwan MJ, Jairoun AA, Zyoud SH. Global trends in research related to sleeve gastrectomy: A bibliometric and visualized study. World J Gastrointest Surg 2021; 13(11): 1509-1522
- URL: https://www.wjgnet.com/1948-9366/full/v13/i11/1509.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v13.i11.1509
Bariatric surgery has been trending since the twentieth century as hundreds of articles discussed different surgical approaches in the prospect of feasibility, complication rate, and long-term outcomes[1]. Bariatric surgery is a broad term that does entail different surgical approaches, including open and laparoscopic surgery. In 2018, 696191 surgical and endoluminal procedures were performed under the umbrella of bariatric surgery[2]. Most of the procedures were surgical approaches rather than endoluminal, such as sleeve gastrectomy (SG), one anastomosis gastric bypass (OAGB), and Roux-en-Y gastric bypass (RYGB). Sleeve gastrectomy remains the most popular procedure worldwide, with thousands of articles and reviews debating its benefits, complications, and long-term outcomes[3-10]. The reasons behind sleeve gastrectomy being a trending topic over the last twenty years are that sleeve gastrectomy is technically less demanding, the learning curve is shorter than other surgical approaches, and it is purely physiological as no anastomosis or bypass is required. The previously mentioned facts support sleeve gastrectomy as it should be associated with less nutritional deficiency and low short-term complications[11-13].
The volume of scientific evidence related to sleeve gastrectomy is enormous, and the annually published article curve is steeply growing[14,15]. Still, it is poorly correlated and not connected to a simple algorithm or graph to explain the pattern and to display the topics that still demand more scientific input so researchers can work on them. Bibliometric analysis revealed that surgical activity and scientific publications in bariatric surgery is a rapidly developing research field[14-18]. However, a quantitative analysis of sleeve gastrectomy has not yet been conducted. Therefore, this study intends to evaluate the research activity in sleeve gastrectomy over the last two decades and quantitatively estimate the hot spots and emerging trends in this type of bariatric surgery with bibliometric methods and enable researchers to identify new areas for potential development.
We downloaded and extracted the publications from the Scopus database. All data were acquired on January 9, 2021. Despite the fact that there are many databases available for worldwide research evaluation, the current study selected the Scopus database because it included rich information such as country distribution and citation analysis. It has been widely used in the field of bibliometric studies[19-22].
The published papers were searched in the recent twenty years (from 2001 to 2020). We used the keyword “Sleeve gastrectomy” or "Gastric Sleeve" in the title and/or abstracts because we are concerned with sleeve gastrectomy per se rather than related terminology. The search strategy was as follows: (TITLE-ABS ("Sleeve gastrectomy") OR TITLE-ABS ("Gastric Sleeve")) AND PUBYEAR > 2000 AND PUBYEAR < 2021.
In this analysis, descriptive statistics are primarily used. Scopus's intrinsic role categorized and analyzed research trends and publication features, such as the distribution of countries, organizations, journals, and citation pattern areas. Besides, the top 20 most cited articles were also listed.
The Visualization of Similarity viewer (VOSviewer 1.6.16) software[23] was used to create collaboration network maps regarding the cooccurrences of all terms in the title and abstract to determine the hotspots related to sleeve gastrectomy research. The visualization of international collaboration to identify the most prominent countries visualizing their relationships was also accomplished using VOSviewer. The data are compared over three 20-year time spans to see how the term used has evolved over time.
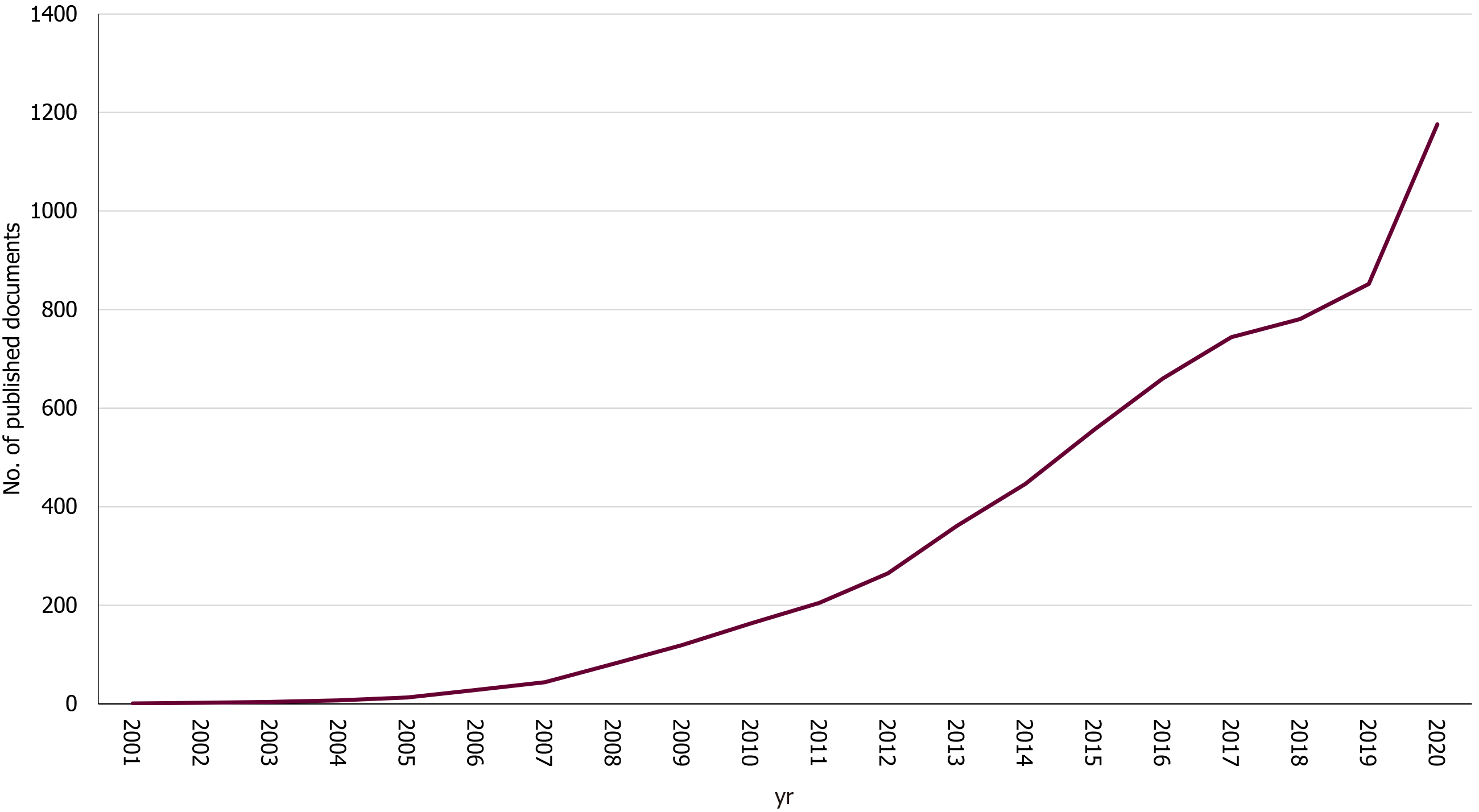
The search strategy yielded a total of 6,508 publications on sleeve gastrectomy from 2001 to 2020. As regards the document type, the majority were articles (n = 5230; 80.36%), followed by reviews (n = 544; 8.36%), letters (n = 250; 3.84%), editorials (n = 172; 2.64%). Other document types such as notes, conferences, papers, or errata amounted to 312 (4.79%) publications. The growth track over the last 20 years (Figure 1) has seen two stages: the first (2001–2010), which had a very slow development period, and the second (2011–2020), which had a very fast development period. The average publication output increased from 46.2 publications per year in the initial period to 604.6 publications per year in the development period. Furthermore, the number of publication outputs during the development period increased from 205 publications in 2011 to 1,176 publications in 2020.
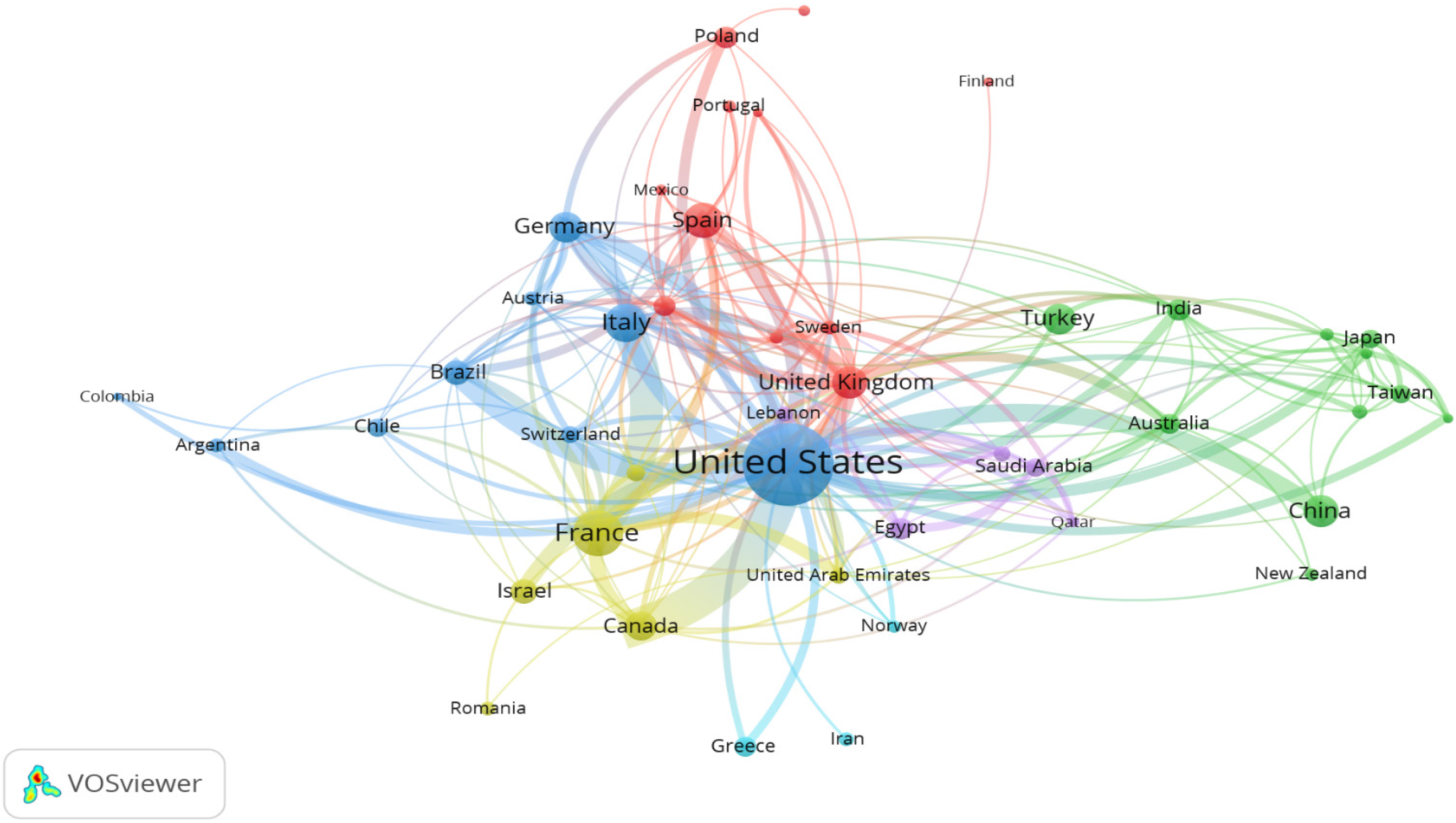
The contributions from each country were counted. The top ten most profitable countries for sleeve gastrectomy are listed in Table 1, along with the total number of publications for each region. Researchers from the United States of America reported about 1983 publications (30.5%) of the science material relating to sleeve gastrectomy over the last 20 years, resulting in the highest pool of evidence about sleeve gastrectomy. France (n = 600, 9.2%) and Italy (n = 417, 6.4%) are the next two countries. Figure 2 illustrates a network mapping of international research collaboration between countries with a minimum research output of 10 documents on sleeve gastrectomy. The United States and France are the countries with the most active research and collaboration.
| Ranking | Country | Number of publications | % |
| 1st | United States | 1983 | 30.47 |
| 2nd | France | 600 | 9.22 |
| 3rd | Italy | 417 | 6.41 |
| 4th | Spain | 356 | 5.47 |
| 5th | United Kingdom | 316 | 4.86 |
| 6th | China | 297 | 4.56 |
| 7th | Germany | 281 | 4.32 |
| 8th | Turkey | 272 | 4.18 |
| 9th | Canada | 243 | 3.73 |
| 10th | Israel | 190 | 2.92 |
Table 2 shows each institution's contribution to the top ten most profitable institutions for sleeve gastrectomy research. The United States and France share six out of the ten most productive institutions for sleeve gastrectomy. The top institution is Cleveland Clinic Foundation with a total of 130 publications (2%). The second and third institutions were France-based as both Inserm institution and AP-HP Assistance Publique - Hopitaux de Paris shared 125 (3.4%) published articles.
| Ranking | Institute | Country | Number of publications | % |
| 1st | Cleveland Clinic Foundation | United States | 130 | 2.00 |
| 2nd | Inserm | France | 118 | 1.81 |
| 3rd | AP-HP Assistance Publique - Hopitaux de Paris | France | 107 | 1.64 |
| 4th | Università degli Studi di Roma La Sapienza | Italy | 93 | 1.43 |
| 5th | Tel Aviv University | Israel | 84 | 1.29 |
| 6th | University of Michigan, Ann Arbor | United States | 82 | 1.26 |
| 7th | Harvard Medical School | United States | 81 | 1.24 |
| 8th | Università degli Studi di Napoli Federico II | Italy | 70 | 1.08 |
| 9th | Centre Hospitalier Universitaire de Nice, Hôpital l'Archet | France | 68 | 1.04 |
| 10th | Hôpital du Sacré-Cœur-de-Montréal | Canada | 65 | 1.00 |
Concerning the individual journals, Obesity Surgery published the largest number of sleeve gastrectomy publications (n = 1744, 27%). This is followed by Surgery for Obesity and Related Diseases (n = 1040, 16%). Both journals share the major output of research and articles related to sleeve gastrectomy. Surgical endoscopy is the third on the list with 304 (4.7%) published articles. Table 3 lists the top ten most productive journals for sleeve gastrectomy research.
| Ranking | Journal | Number of publications | % | IFa |
| 1st | Obesity Surgery | 1744 | 26.80 | 3.412 |
| 2nd | Surgery for Obesity and Related Diseases | 1040 | 15.98 | 3.812 |
| 3rd | Surgical Endoscopy | 304 | 4.67 | 3.149 |
| 4th | Bariatric Surgical Practice and Patient Care | 85 | 1.31 | 0.391 |
| 5th | Journal of Laparoendoscopic and Advanced Surgical Techniques | 75 | 1.15 | 1.310 |
| 6th | Surgical Laparoscopy Endoscopy and Percutaneous Techniques | 61 | 0.94 | 1.382 |
| 7th | International Journal of Surgery | 57 | 0.88 | 3.352 |
| 8th | Annals of Surgery | 56 | 0.86 | 10.130 |
| 9th | Journal of Gastrointestinal Surgery | 54 | 0.83 | 2.573 |
| 10th | International Journal of Surgery Case Reports | 53 | 0.81 | NA |
The top 20 most cited papers on sleeve gastrectomy are summarized in Table 4. The top 20 most cited articles had citations ranging from 556 to 1435[1,24-42]. The top-cited article is bariatric surgery vs intensive medical therapy in obese patients with diabetes, published in 2012 in the New England Journal of Medicine with 1435 citations. The second top-cited article is Bariatric surgery vs intensive medical therapy for diabetes - 3-Year outcomes, which was published in 2014 in the New England Journal of Medicine with 983 citations. The third and fourth top-cited publications were published in Obesity Surgery in 2013 and 2015 with 1751 total citations per both documents, retrospectively. A Cochrane review was published in 2014 with total 806 citations discussing surgery for weight loss in adults, which was written by Colquitt JL.
| Ranking | Authors | Title | Year | Source title | Cited by |
| 1st | Schauer et al[42] | “Bariatric surgery versus intensive medical therapy in obese patients with diabetes” | 2012 | New England Journal of Medicine | 1435 |
| 2nd | Schauer et al[41] | “Bariatric surgery versus intensive medical therapy for diabetes – 3 yr outcomes” | 2014 | New England Journal of Medicine | 983 |
| 3rd | Buchwald and Oien[25] | “Metabolic/bariatric surgery worldwide 2011” | 2013 | Obesity Surgery | 902 |
| 4th | Angrisani et al[1] | “Bariatric Surgery Worldwide 2013” | 2015 | Obesity Surgery | 849 |
| 5th | Schauer et al[40] | “Bariatric surgery versus intensive medical therapy for diabetes – 5 yr outcomes” | 2017 | New England Journal of Medicine | 845 |
| 6th | Colquitt et al[27] | “Surgery for weight loss in adults” | 2014 | Cochrane Database of Systematic Reviews | 806 |
| 7th | Chang et al[26] | “The effectiveness and risks of bariatric surgery an updated systematic review and meta-analysis, 2003-2012” | 2014 | JAMA Surgery | 768 |
| 8th | Buchwald and Oien[24] | “Metabolic/bariatric surgery worldwide 2008” | 2009 | Obesity Surgery | 635 |
| 9th | Mechanick et al[34] | “Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient-2013 update: Cosponsored by American association of clinical endocrinologists, the obesity society, and American society for metabolic and bariatric surgery” | 2013 | Obesity | 634 |
| 10th | Picot et al[36] | “The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: A systematic review and economic evaluation” | 2009 | Health Technology Assessment | 616 |
| 11th | Karamanakos et al[33] | “Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide-yy levels after roux-en-y gastric bypass and sleeve gastrectomy a prospective, double blind study” | 2008 | Annals of Surgery | 596 |
| 12th | Regan et al[37] | “Early Experience with Two-Stage Laparoscopic Roux-en-Y Gastric Bypass as an Alternative in the Super-Super Obese Patient” | 2003 | Obesity Surgery | 592 |
| 13th | Rosenthal et al[38] | “International sleeve gastrectomy expert panel consensus statement: Best practice guidelines based on experience of > 12,000 cases” | 2012 | Surgery for Obesity and Related Diseases | 556 |
| 14th | Ryan et al[39] | FXR is a molecular target for the effects of vertical sleeve gastrectomy” | 2014 | Nature | 545 |
| 15th | Himpens et al[30] | “A prospective randomized study between laparoscopic gastric banding and laparoscopic isolated sleeve gastrectomy: Results after 1 and 3 years” | 2006 | Obesity Surgery | 500 |
| 16th | Himpens et al[31] | “Long-term results of laparoscopic sleeve gastrectomy for obesity” | 2010 | Annals of Surgery | 498 |
| 17th | Colquitt et al[28] | “Surgery for obesity” | 2009 | Cochrane Database of Systematic Reviews | 489 |
| 18th | Cottam et al[29] | “Laparoscopic sleeve gastrectomy as an initial weight-loss procedure for high-risk patients with morbid obesity” | 2006 | Surgical Endoscopy and Other Interventional Techniques | 473 |
| 19th | Hutter et al[32] | “First report from the American College of Surgeons Bariatric Surgery Center Network: Laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass” | 2011 | Annals of Surgery | 438 |
| 20th | Peterli et al[35] | “Improvement in glucose metabolism after bariatric surgery: Comparison of laparoscopic roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy: A prospective randomized trial” | 2009 | Annals of Surgery | 437 |
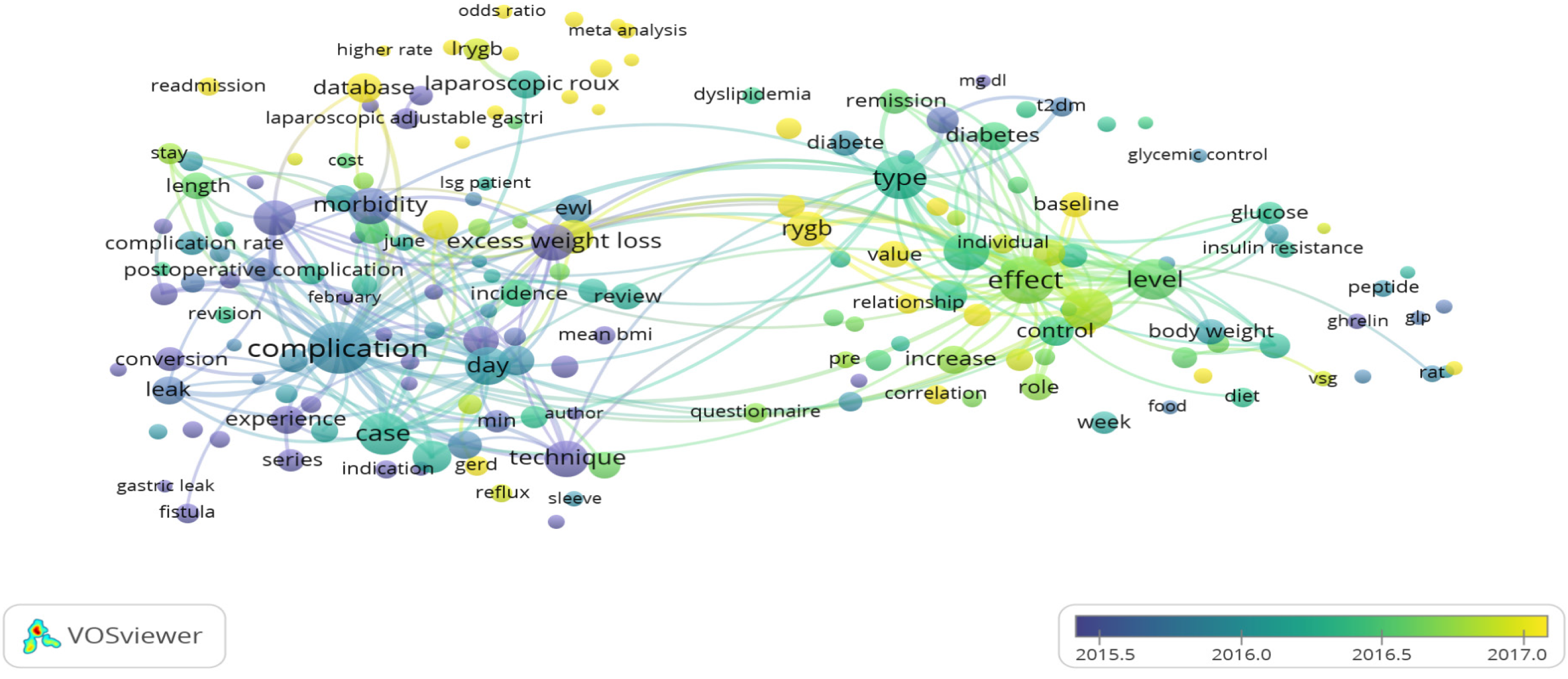
The visualization of the most frequently found terms in the title and abstracts of the collected documents (a minimum of 50 times) resulted in three major colored clusters (red, green, and blue), which reflect the three research topics as the highest research priority topics (Figure 3). Cluster number 1 (red color) included terms related to morbidity and potential complications topics such as conversion, leak, and fistula; Cluster number 2 (blue color) included terms related to the complexity of the procedure and different surgical approach topics such laparoscopy; and Cluster number 3 (green color) included terms related to diabetes and BMI in correlation to sleeve gastrectomy. Figure 4 shows an overlay visualization in which the VOSviewer was used to add colors to the terms according to the year of publication. Blue terms emerged first, followed by yellow terms later. Most sleeve gastrectomy research centered on terms relating to morbidity and surgical complications before 2016, namely, in the early stages of research in this field. The current trends presented the terms associated with surgical techniques and the correlation of sleeve gastrectomy to diabetes mellitus and body mass index.
This bibliometric analysis presents a comprehensive overview of the growth of the scientific literature regarding sleeve gastrectomy research in the recent twenty years. Sleeve gastrectomy is one of the most common bariatric procedures and one of the most researched[14,15,17,18,43-46]. The global patterns of published papers in sleeve gastrectomy research showed statistically continued growth over time. While the number of publications increased gradually, the year-over-year percentage of publications increased noticeably in the last two years. Thus, sleeve gastrectomy-related research has recently shown considerable growth, which can be recognized by researchers’ contributions globally. To evaluate the research contributions at the global level, total research publication output in the field of sleeve gastrectomy has been applied as an indicator for scientific research production. In accordance with the observed increase of research regarding morbidity and surgical complications in general[47-53], our results demonstrated a continued increase of sleeve gastrectomy literature since 2001. This progress was particularly prominent since 2010, which coincided with the shift in focusing on developing tools for surgical techniques[54-57] and the correlation of sleeve gastrectomy with diabetes mellitus and body mass index[58-67].
In the current study, the United States has the highest publication rate in research production with sleeve gastrectomy, which matches what has also been found in other therapeutic approaches to obesity treatment[14,15,18,43-46]. France was ranked as the second in the number of publications in the field of sleeve gastrectomy, followed by Italy. This can be attributed to the development of countries’ scientific systems and the number of researchers[68] or due to the high prevalence of overweight and obesity in these countries[69,70].
According to Angrisani et al[1] the United States had the largest number of bariatric procedures and the United States is the leading country globally. In addition, according to a review of bariatric practice in the United States, laparoscopic sleeve gastrectomy has become the most commonly performed bariatric procedure[71]. According to data from Europe, France currently has the highest rate of bariatric surgery[72]. Despite the comparatively low prevalence rates of 3.1% and 1.2% for grade II and III obesity, respectively, in France in comparison to other European countries, this may be clarified by a favorable policy contextual and unrestricted access to bariatric surgery in France[73]. France's current distinction in comparison to other European countries is the current and increasing preference for laparoscopic sleeve gastrectomy over other procedures[73].
The current findings are in accord with a previous bibliometric study indicating that the United States were the most productive country in research related to the microbiome related to irritable bowel syndrome[74]. These findings seem to be in agreement with other bibliometric research that found the United States and France were the leading scientific countries on Chagas cardiomyopathy[75]. On the other hand, as revealed by previous bibliometric studies[76-80], the United States took the first international collaborative articles position. The importance of international collaboration was not only focusing on advancing knowledge and strengthening research capacity[81]; it also might increase citation rates and improve research quality[82,83].
The most cited publication was published in 2012 by Schauer et al[42] in the New England Journal of Medicine (n = 1435 citations). This publication found that weight loss was greater in the sleeve gastrectomy group than in the medical therapy group. Furthermore, this study demonstrated that 12 mo of medical therapy plus bariatric surgery greatly improved glycemic regulation in obese patients with uncontrolled type 2 diabetes compared with medical therapy alone[42]. The second most cited publication (n = 983 citations) was published in 2014 in the New England Journal of Medicine by Schauer et al[41], it presented the outcomes 3 years obese patients with uncontrolled type 2 diabetes were randomly assigned to undergo either intensive medical therapy alone or intensive medical therapy plus sleeve gastrectomy or Roux-en-Y gastric bypass. This study proved that 3 years of medical therapy plus bariatric surgery greatly improved glycemic regulation in obese patients with uncontrolled type 2 diabetes compared to medical therapy alone[41]. Finally, the third paper (n = 902 citations), published in 2013 in Obesity Surgery by Buchwald and Oien[25], found that the most commonly performed bariatric procedures were Roux-en-Y gastric bypass and sleeve gastrectomy.
The major limitation of this study is related to the database used to collect publications related to sleeve gastrectomy. However, the Scopus database does not represent all scientific journals. However, it is the largest database of peer-reviewed scientific journals[84]. Another limitation is that certain articles' titles and abstracts did not include the term "sleeve gastrectomy" or related expressions, so not all articles regarding sleeve gastrectomy might be considered. Furthermore, the majority of publications were published and indexed in 2020, but since new journal issues are still being released and indexed, therefore, the amount of scientific research productivity this year could be higher.
The number of sleeve gastrectomy publications has gradually grown over the last 20 years. The current study's findings were biased in favor of high-income countries. In this domain, the United States and France had a significant impact. The current literature on sleeve gastrectomy was directed toward several themes such as morbidity and potential complications, the complexity of the procedure and different surgical approaches, and diabetes mellitus and body mass index in correlation with sleeve gastrectomy. This bibliometric analysis could help researchers better understand the knowledge base and research frontiers surrounding sleeve gastrectomy. In addition, future studies may focus on emerging research hotspots.
Sleeve gastrectomy has grown in popularity among laparoscopic surgeons who do bariatric surgery and has shown to be an effective way of obtaining significant weight loss in a short period of time.
The amount of scientific evidence relating to sleeve gastrectomy is massive, and the annually published article curve is sharply increasing. It is still weakly correlated and unconnected to a simple algorithm or graph to describe the pattern and highlight the issues that require more scientific input so that researchers may work on them.
The goal of this study is to use bibliometric approaches to assess the research activity in sleeve gastrectomy over the last two decades and to visualize the hot areas and developing trends in this type of bariatric surgery.
On January 9, 2021, we performed a literature search utilizing the Scopus database to gather papers from 2001 to 2020 for this retrospective research. Bibliometric characteristics such as publication output, countries, institutions, journals, citation frequency, and research hotspots were evaluated by using Excel 2013 and VOSviewer.
Over the previous 20 years, the number of publications on sleeve gastrectomy has progressively increased. The outcomes of the current study were skewed in favor of high-income nations. The United States and France have a big effect in this sector.
The present literature on sleeve gastrectomy focused on numerous issues, including morbidity and possible complications, the procedure's complexity and various surgical methods, and diabetes mellitus and body mass index in connection to sleeve gastrectomy.
This bibliometric study may aid researchers in better understanding the current state of knowledge and research horizons in the field of sleeve gastrectomy.
| 1. | Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, Scopinaro N. Bariatric Surgery Worldwide 2013. Obes Surg. 2015;25:1822-1832. |
| 2. | Angrisani L, Santonicola A, Iovino P, Ramos A, Shikora S, Kow L. Bariatric Surgery Survey 2018: Similarities and Disparities Among the 5 IFSO Chapters. Obes Surg. 2021;31:1937-1948. |
| 3. | Thereaux J, Lesuffleur T, Czernichow S, Basdevant A, Msika S, Nocca D, Millat B, Fagot-Campagna A. Long-term adverse events after sleeve gastrectomy or gastric bypass: a 7-year nationwide, observational, population-based, cohort study. Lancet Diabetes Endocrinol. 2019;7:786-795. |
| 4. | Hofsø D, Fatima F, Borgeraas H, Birkeland KI, Gulseth HL, Hertel JK, Johnson LK, Lindberg M, Nordstrand N, Cvancarova Småstuen M, Stefanovski D, Svanevik M, Gretland Valderhaug T, Sandbu R, Hjelmesæth J. Gastric bypass vs sleeve gastrectomy in patients with type 2 diabetes (Oseberg): a single-centre, triple-blind, randomised controlled trial. Lancet Diabetes Endocrinol. 2019;7:912-924. |
| 5. | Steenackers N, Vanuytsel T, Augustijns P, Tack J, Mertens A, Lannoo M, Van der Schueren B, Matthys C. Adaptations in gastrointestinal physiology after sleeve gastrectomy and Roux-en-Y gastric bypass. Lancet Gastroenterol Hepatol. 2021;6:225-237. |
| 6. | Madsbad S, Dirksen C, Holst JJ. Mechanisms of changes in glucose metabolism and bodyweight after bariatric surgery. Lancet Diabetes Endocrinol. 2014;2:152-164. |
| 7. | Guetta O, Vakhrushev A, Dukhno O, Ovnat A, Sebbag G. New results on the safety of laparoscopic sleeve gastrectomy bariatric procedure for type 2 diabetes patients. World J Diabetes. 2019;10:78-86. |
| 8. | Wang JW, Chen CY. Current status of endoscopic sleeve gastroplasty: An opinion review. World J Gastroenterol. 2020;26:1107-1112. |
| 9. | Benaiges D, Más-Lorenzo A, Goday A, Ramon JM, Chillarón JJ, Pedro-Botet J, Flores-Le Roux JA. Laparoscopic sleeve gastrectomy: More than a restrictive bariatric surgery procedure? World J Gastroenterol. 2015;21:11804-11814. |
| 10. | Langer FB, Reza Hoda MA, Bohdjalian A, Felberbauer FX, Zacherl J, Wenzl E, Schindler K, Luger A, Ludvik B, Prager G. Sleeve gastrectomy and gastric banding: effects on plasma ghrelin levels. Obes Surg. 2005;15:1024-1029. |
| 11. | Lupoli R, Lembo E, Saldalamacchia G, Avola CK, Angrisani L, Capaldo B. Bariatric surgery and long-term nutritional issues. World J Diabetes. 2017;8:464-474. |
| 12. | Jamil O, Gonzalez-Heredia R, Quadri P, Hassan C, Masrur M, Berger R, Bernstein K, Sanchez-Johnsen L. Micronutrient Deficiencies in Laparoscopic Sleeve Gastrectomy. Nutrients. 2020;12. |
| 13. | Krzizek EC, Brix JM, Stöckl A, Parzer V, Ludvik B. Prevalence of Micronutrient Deficiency after Bariatric Surgery. Obes Facts. 2021;14:197-204. |
| 14. | Ozsoy Z, Demir E. Which Bariatric Procedure Is the Most Popular in the World? Obes Surg. 2018;28:2339-2352. |
| 15. | Paolino L, Pravettoni R, Epaud S, Ortala M, Lazzati A. Comparison of Surgical Activity and Scientific Publications in Bariatric Surgery: an Epidemiological and Bibliometric Analysis. Obes Surg. 2020;30:3822-3830. |
| 16. | AlMarri F, Al Sabah S, Al Haddad E, Vaz JD. A Call for More Research from the Arabian Gulf. Obes Surg. 2017;27:2034-2043. |
| 17. | Stefura T, Kacprzyk A, Droś J, Chłopaś K, Wysocki M, Rzepa A, Pisarska M, Małczak P, Pędziwiatr M, Nowakowski M, Budzyński A, Major P. The hundred most frequently cited studies on sleeve gastrectomy. Wideochir Inne Tech Maloinwazyjne. 2020;15:249-267. |
| 18. | Zhao N, Tao K, Wang G, Xia Z. Global obesity research trends during 1999 to 2017: A bibliometric analysis. Medicine (Baltimore). 2019;98:e14132. |
| 19. | AlRyalat SAS, Malkawi LW, Momani SM. Comparing Bibliometric Analysis Using PubMed, Scopus, and Web of Science Databases. J Vis Exp. 2019;. |
| 20. | Bakkalbasi N, Bauer K, Glover J, Wang L. Three options for citation tracking: Google Scholar, Scopus and Web of Science. Biomed Digit Libr. 2006;3:7. |
| 21. | Falagas ME, Pitsouni EI, Malietzis GA, Pappas G. Comparison of PubMed, Scopus, Web of Science, and Google Scholar: strengths and weaknesses. FASEB J. 2008;22:338-342. |
| 22. | Kulkarni AV, Aziz B, Shams I, Busse JW. Comparisons of citations in Web of Science, Scopus, and Google Scholar for articles published in general medical journals. JAMA. 2009;302:1092-1096. |
| 23. | van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84:523-538. |
| 26. | Chang SH, Stoll CR, Song J, Varela JE, Eagon CJ, Colditz GA. The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003-2012. JAMA Surg. 2014;149:275-287. |
| 27. | Colquitt JL, Pickett K, Loveman E, Frampton GK. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014;CD003641. |
| 28. | Colquitt JL, Picot J, Loveman E, Clegg AJ. Surgery for obesity. Cochrane Database Syst Rev. 2009;CD003641. |
| 29. | Cottam D, Qureshi FG, Mattar SG, Sharma S, Holover S, Bonanomi G, Ramanathan R, Schauer P. Laparoscopic sleeve gastrectomy as an initial weight-loss procedure for high-risk patients with morbid obesity. Surg Endosc. 2006;20:859-863. |
| 30. | Himpens J, Dapri G, Cadière GB. A prospective randomized study between laparoscopic gastric banding and laparoscopic isolated sleeve gastrectomy: results after 1 and 3 years. Obes Surg. 2006;16:1450-1456. |
| 31. | Himpens J, Dobbeleir J, Peeters G. Long-term results of laparoscopic sleeve gastrectomy for obesity. Ann Surg. 2010;252:319-324. |
| 32. | Hutter MM, Schirmer BD, Jones DB, Ko CY, Cohen ME, Merkow RP, Nguyen NT. First report from the American College of Surgeons Bariatric Surgery Center Network: laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ann Surg. 2011;254:410-20; discussion 420. |
| 33. | Karamanakos SN, Vagenas K, Kalfarentzos F, Alexandrides TK. Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide-YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy: a prospective, double blind study. Ann Surg. 2008;247:401-407. |
| 34. | Mechanick JI, Youdim A, Jones DB, Garvey WT, Hurley DL, McMahon MM, Heinberg LJ, Kushner R, Adams TD, Shikora S, Dixon JB, Brethauer S; American Association of Clinical Endocrinologists; Obesity Society; American Society for Metabolic and Bariatric Surgery. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient--2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic and Bariatric Surgery. Obesity (Silver Spring). 2013;21 Suppl 1:S1-27. |
| 35. | Peterli R, Wölnerhanssen B, Peters T, Devaux N, Kern B, Christoffel-Courtin C, Drewe J, von Flüe M, Beglinger C. Improvement in glucose metabolism after bariatric surgery: comparison of laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy: a prospective randomized trial. Ann Surg. 2009;250:234-241. |
| 36. | Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, Clegg AJ. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess. 2009;13:1-190, 215. |
| 37. | Regan JP, Inabnet WB, Gagner M, Pomp A. Early experience with two-stage laparoscopic Roux-en-Y gastric bypass as an alternative in the super-super obese patient. Obes Surg. 2003;13:861-864. |
| 38. | Rosenthal RJ; International Sleeve Gastrectomy Expert Panel, Diaz AA, Arvidsson D, Baker RS, Basso N, Bellanger D, Boza C, El Mourad H, France M, Gagner M, Galvao-Neto M, Higa KD, Himpens J, Hutchinson CM, Jacobs M, Jorgensen JO, Jossart G, Lakdawala M, Nguyen NT, Nocca D, Prager G, Pomp A, Ramos AC, Rosenthal RJ, Shah S, Vix M, Wittgrove A, Zundel N. International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of >12,000 cases. Surg Obes Relat Dis. 2012;8:8-19. |
| 39. | Ryan KK, Tremaroli V, Clemmensen C, Kovatcheva-Datchary P, Myronovych A, Karns R, Wilson-Pérez HE, Sandoval DA, Kohli R, Bäckhed F, Seeley RJ. FXR is a molecular target for the effects of vertical sleeve gastrectomy. Nature. 2014;509:183-188. |
| 40. | Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Aminian A, Brethauer SA, Navaneethan SD, Singh RP, Pothier CE, Nissen SE, Kashyap SR; STAMPEDE Investigators. Bariatric Surgery versus Intensive Medical Therapy for Diabetes - 5-Year Outcomes. N Engl J Med. 2017;376:641-651. |
| 41. | Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Brethauer SA, Navaneethan SD, Aminian A, Pothier CE, Kim ES, Nissen SE, Kashyap SR; STAMPEDE Investigators. Bariatric surgery versus intensive medical therapy for diabetes--3-year outcomes. N Engl J Med. 2014;370:2002-2013. |
| 42. | Schauer PR, Kashyap SR, Wolski K, Brethauer SA, Kirwan JP, Pothier CE, Thomas S, Abood B, Nissen SE, Bhatt DL. Bariatric surgery vs intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366:1567-1576. |
| 43. | Choi HS, Chun HJ. Recent Trends in Endoscopic Bariatric Therapies. Clin Endosc. 2017;50:11-16. |
| 44. | Dabi Y, Darrigues L, Katsahian S, Azoulay D, De Antonio M, Lazzati A. Publication Trends in Bariatric Surgery: a Bibliometric Study. Obes Surg. 2016;26:2691-2699. |
| 45. | Ozsoy Z, Demir E. The Evolution of Bariatric Surgery Publications and Global Productivity: A Bibliometric Analysis. Obes Surg. 2018;28:1117-1129. |
| 46. | Toro-Huamanchumo CJ, Morán-Mariños C, Salazar-Alarcon JL, Barros-Sevillano S, Huamanchumo-Suyon ME, Salinas-Sedo G. Latin American Research on Bariatric Surgery: a Bibliometric Study. Obes Surg. 2021;31:1869-1876. |
| 47. | Sarkhosh K, Birch DW, Sharma A, Karmali S. Complications associated with laparoscopic sleeve gastrectomy for morbid obesity: a surgeon's guide. Can J Surg. 2013;56:347-352. |
| 48. | Lalor PF, Tucker ON, Szomstein S, Rosenthal RJ. Complications after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2008;4:33-38. |
| 49. | Frezza EE, Reddy S, Gee LL, Wachtel MS. Complications after sleeve gastrectomy for morbid obesity. Obes Surg. 2009;19:684-687. |
| 50. | Triantafyllidis G, Lazoura O, Sioka E, Tzovaras G, Antoniou A, Vassiou K, Zacharoulis D. Anatomy and complications following laparoscopic sleeve gastrectomy: radiological evaluation and imaging pitfalls. Obes Surg. 2011;21:473-478. |
| 51. | Mittermair R, Sucher R, Perathoner A. Results and complications after laparoscopic sleeve gastrectomy. Surg Today. 2014;44:1307-1312. |
| 52. | Iannelli A, Treacy P, Sebastianelli L, Schiavo L, Martini F. Perioperative complications of sleeve gastrectomy: Review of the literature. J Minim Access Surg. 2019;15:1-7. |
| 53. | Monkhouse SJ, Morgan JD, Norton SA. Complications of bariatric surgery: presentation and emergency management--a review. Ann R Coll Surg Engl. 2009;91:280-286. |
| 54. | Braghetto I, Korn O, Valladares H, Gutiérrez L, Csendes A, Debandi A, Castillo J, Rodríguez A, Burgos AM, Brunet L. Laparoscopic sleeve gastrectomy: surgical technique, indications and clinical results. Obes Surg. 2007;17:1442-1450. |
| 55. | Felsenreich DM, Bichler C, Langer FB, Gachabayov M, Prager G. Sleeve Gastrectomy: Surgical Technique, Outcomes, and Complications. Surg Technol Int. 2020;36:63-69. |
| 56. | Hayes K, Eid G. Laparoscopic Sleeve Gastrectomy: Surgical Technique and Perioperative Care. Surg Clin North Am. 2016;96:763-771. |
| 57. | Varban OA, Thumma JR, Finks JF, Carlin AM, Kemmeter PR, Ghaferi AA, Dimick JB. Assessing variation in technique for sleeve gastrectomy based on outcomes of surgeons ranked by safety and efficacy: a video-based study. Surg Endosc. 2019;33:895-903. |
| 58. | Ichikawa H, Imoto H, Tanaka N, Musha H, Sawada S, Naitoh T, Kamei T, Unno M. Efficacy of laparoscopic sleeve gastrectomy for patient with morbid obesity and type 1 diabetes mellitus: a case report. Surg Case Rep. 2021;7:7. |
| 59. | Lewis KH, Arterburn DE, Zhang F, Callaway K, Wallace J, Fernandez A, Ross-Degnan D, Wharam JF. Comparative Effectiveness of Vertical Sleeve Gastrectomy Versus Roux-en-Y Gastric Bypass for Diabetes Treatment: A Claims-based Cohort Study. Ann Surg. 2021;273:940-948. |
| 60. | Nudotor RD, Prokopowicz G, Abbey EJ, Gonzalez A, Canner JK, Steele KE. Comparative Effectiveness of Roux-en Y Gastric Bypass Versus Vertical Sleeve Gastrectomy for Sustained Remission of Type 2 Diabetes Mellitus. J Surg Res. 2021;261:407-416. |
| 61. | Castellana M, Procino F, Biacchi E, Zupo R, Lampignano L, Castellana F, Sardone R, Palermo A, Cesareo R, Trimboli P, Giannelli G. Roux-en-Y Gastric Bypass vs Sleeve Gastrectomy for Remission of Type 2 Diabetes. J Clin Endocrinol Metab. 2021;106:922-933. |
| 62. | Rafey MF, Fang CEH, Ioana I, Griffin H, Hynes M, O'Brien T, McAnena O, O'Shea P, Collins C, Davenport C, Finucane FM. The leptin to adiponectin ratio (LAR) is reduced by sleeve gastrectomy in adults with severe obesity: a prospective cohort study. Sci Rep. 2020;10:16270. |
| 63. | Salman AA, Salman MA, Marie MA, Rabiee A, Helmy MY, Tourky MS, Qassem MG, Shaaban HE, Sarhan MD. Factors associated with resolution of type-2 diabetes mellitus after sleeve gastrectomy in obese adults. Sci Rep. 2021;11:6002. |
| 64. | Vennapusa A, Bhargav Panchangam R, Kesara C, Vyshnavi Vanta GR, Madivada MS. Metabolic efficacy following laparoscopic sleeve gastrectomy with loop duodenal switch surgery for type 2 diabetes in Indian patients with severe obesity. Diabetes Metab Syndr. 2021;15:581-587. |
| 65. | Vrakopoulou GZ, Theodoropoulos C, Kalles V, Zografos G, Almpanopoulos K. Type 2 diabetes mellitus status in obese patients following sleeve gastrectomy or one anastomosis gastric bypass. Sci Rep. 2021;11:4421. |
| 66. | Yan Y, Wang F, Chen H, Zhao X, Yin D, Hui Y, Ma N, Yang C, Zheng Z, Zhang T, Xu N, Wang G. Efficacy of laparoscopic gastric bypass vs laparoscopic sleeve gastrectomy in treating obesity combined with type-2 diabetes. Br J Biomed Sci. 2021;78:35-40. |
| 67. | Koch TR, Shope TR. Laparoscopic Vertical Sleeve Gastrectomy as a Treatment Option for Adults with Diabetes Mellitus. Adv Exp Med Biol. 2021;1307:299-320. |
| 68. | Ramos JM, González-Alcaide G, Bolaños-Pizarro M. Bibliometric analysis of leishmaniasis research in Medline (1945-2010). Parasit Vectors. 2013;6:55. |
| 69. | Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF, Abraham JP, Abu-Rmeileh NM, Achoki T, AlBuhairan FS, Alemu ZA, Alfonso R, Ali MK, Ali R, Guzman NA, Ammar W, Anwari P, Banerjee A, Barquera S, Basu S, Bennett DA, Bhutta Z, Blore J, Cabral N, Nonato IC, Chang JC, Chowdhury R, Courville KJ, Criqui MH, Cundiff DK, Dabhadkar KC, Dandona L, Davis A, Dayama A, Dharmaratne SD, Ding EL, Durrani AM, Esteghamati A, Farzadfar F, Fay DF, Feigin VL, Flaxman A, Forouzanfar MH, Goto A, Green MA, Gupta R, Hafezi-Nejad N, Hankey GJ, Harewood HC, Havmoeller R, Hay S, Hernandez L, Husseini A, Idrisov BT, Ikeda N, Islami F, Jahangir E, Jassal SK, Jee SH, Jeffreys M, Jonas JB, Kabagambe EK, Khalifa SE, Kengne AP, Khader YS, Khang YH, Kim D, Kimokoti RW, Kinge JM, Kokubo Y, Kosen S, Kwan G, Lai T, Leinsalu M, Li Y, Liang X, Liu S, Logroscino G, Lotufo PA, Lu Y, Ma J, Mainoo NK, Mensah GA, Merriman TR, Mokdad AH, Moschandreas J, Naghavi M, Naheed A, Nand D, Narayan KM, Nelson EL, Neuhouser ML, Nisar MI, Ohkubo T, Oti SO, Pedroza A, Prabhakaran D, Roy N, Sampson U, Seo H, Sepanlou SG, Shibuya K, Shiri R, Shiue I, Singh GM, Singh JA, Skirbekk V, Stapelberg NJ, Sturua L, Sykes BL, Tobias M, Tran BX, Trasande L, Toyoshima H, van de Vijver S, Vasankari TJ, Veerman JL, Velasquez-Melendez G, Vlassov VV, Vollset SE, Vos T, Wang C, Wang X, Weiderpass E, Werdecker A, Wright JL, Yang YC, Yatsuya H, Yoon J, Yoon SJ, Zhao Y, Zhou M, Zhu S, Lopez AD, Murray CJ, Gakidou E. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766-781. |
| 70. | NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627-2642. |
| 71. | Spaniolas K, Kasten KR, Brinkley J, Sippey ME, Mozer A, Chapman WH, Pories WJ. The Changing Bariatric Surgery Landscape in the United States. Obes Surg. 2015;25:1544-1546. |
| 72. | Borisenko O, Colpan Z, Dillemans B, Funch-Jensen P, Hedenbro J, Ahmed AR. Clinical Indications, Utilization, and Funding of Bariatric Surgery in Europe. Obes Surg. 2015;25:1408-1416. |
| 73. | Czernichow S, Paita M, Nocca D, Msika S, Basdevant A, Millat B, Fagot-Campagna A. Current challenges in providing bariatric surgery in France: A nationwide study. Medicine (Baltimore). 2016;95:e5314. |
| 74. | Zyoud SH, Smale S, Waring WS, Sweileh W, Al-Jabi SW. Global research trends in the microbiome related to irritable bowel syndrome: A bibliometric and visualized study. World J Gastroenterol. 2021;27:1341-1353. |
| 75. | Al-Jabi SW. Current global research landscape on COVID-19 and depressive disorders: Bibliometric and visualization analysis. World J Psychiatry. 2021;11:253-264. |
| 76. | González-Alcaide G, Salinas A, Ramos JM. Scientometrics analysis of research activity and collaboration patterns in Chagas cardiomyopathy. PLoS Negl Trop Dis. 2018;12:e0006602. |
| 77. | Liu F, Lin A, Wang H, Peng Y, Hong S. Global research trends of geographical information system from 1961 to 2010: a bibliometric analysis. Scientometrics. 2016;106:751-768. |
| 78. | Cheng T, Zhang G. Worldwide research productivity in the field of rheumatology from 1996 to 2010: a bibliometric analysis. Rheumatology (Oxford). 2013;52:1630-1634. |
| 79. | Zyoud SH, Al-Jabi SW. Mapping the situation of research on coronavirus disease-19 (COVID-19): a preliminary bibliometric analysis during the early stage of the outbreak. BMC Infect Dis. 2020;20:561. |
| 80. | Zyoud SH. The Arab region's contribution to global COVID-19 research: Bibliometric and visualization analysis. Global Health. 2021;17:31. |
| 81. | Sweileh WM. Bibliometric analysis of peer-reviewed literature on antimicrobial stewardship from 1990 to 2019. Global Health. 2021;17:1. |
| 82. | Søreide K, Alderson D, Bergenfelz A, Beynon J, Connor S, Deckelbaum DL, Dejong CH, Earnshaw JJ, Kyamanywa P, Perez RO, Sakai Y, Winter DC; International Research Collaboration in Surgery (IRIS) ad-hoc working group. Strategies to improve clinical research in surgery through international collaboration. Lancet. 2013;382:1140-1151. |
| 83. | Stek PE, van Geenhuizen MS. The influence of international research interaction on national innovation performance: A bibliometric approach. Technol Forecast Soc. 2015;Article in Press. |
| 84. | Elsevier. Scopus Quick Reference Guide 2019. [cited 9 April 2021]. Available from: https://supportcontent.elsevier.com/RightNow%20Next%20Gen/Scopus/Files/Scopus_User_Guide.pdf. |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Specialty type: Surgery
Country/Territory of origin: Palestine
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dong Y S-Editor: Wang LL L-Editor: A P-Editor: Wang LL