Published online Mar 27, 2020. doi: 10.4240/wjgs.v12.i3.123
Peer-review started: October 14, 2019
First decision: November 6, 2019
Revised: November 20, 2019
Accepted: December 14, 2019
Article in press: December 14, 2019
Published online: March 27, 2020
Processing time: 136 Days and 17.5 Hours
Isolated tuberculosis of the gallbladder is extremely rare due to its intrinsic resistance to tuberculous infections. There are reports of gallbladder tuberculosis mimicking cholecystitis or malignancy. However, these presentations were chronic. The diagnosis of gallbladder tuberculosis warrants the need for investigation of additional sites of inoculation and contact tracing of all tuberculosis contacts. Gallbladder tuberculosis is a rare entity but should be suspected in patients from endemic regions with risk factors such as underlying immunosuppression or history of tuberculosis.
We present a case of gallbladder tuberculosis presenting as acute cholecystitis. A 44-year-old Filipino lady presented with a 11-d history of right hypochondrium and epigastric pain which worsened after meals with no significant past medical history. She underwent laparoscopic cholecystectomy on the presumptive diagnosis of acute cholecystitis and diagnosed as gallbladder tuberculosis after histopathological examination. The patient did not have features of pulmonary or systemic tuberculosis nor was she immunocompromised. She recovered uneventfully. She was subsequently discharged and followed-up at a hospital in her home country due to financial and social reasons.
Clinicians should have a high index of suspicion for patients in endemic regions presenting with cholecystitis.
Core tip: Isolated tuberculosis of the gallbladder is extremely rare due to its intrinsic resistance to tuberculous infections. We present a rare case of isolated gallbladder tuberculosis presenting as acute cholecystitis. Clinical examination revealed positive Murphy’s sign. The patient underwent laparoscopic cholecystectomy within the same admission. Histology shows necrotizing granulomatous inflammation with rare acid-fast bacilli which was identified on Ziehl-Neelsen stain. This case highlights the multivariable clinical presentations of gallbladder tuberculosis. Clinicians should have a high index of suspicion for patients in endemic regions presenting with cholecystitis to obtain a pre-operative diagnosis.
- Citation: Chan KS, Shelat VG, Tan CH, Tang YL, Junnarkar SP. Isolated gallbladder tuberculosis mimicking acute cholecystitis: A case report. World J Gastrointest Surg 2020; 12(3): 123-128
- URL: https://www.wjgnet.com/1948-9366/full/v12/i3/123.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v12.i3.123
Abdominal tuberculosis (TB) is uncommon, with an incidence of 3.5% of all extra-pulmonary TB[1]. TB of the hepatobiliary system is rare and isolated gallbladder TB in the absence of any active pulmonary infection is extremely rare[2-4]. Gallbladder TB remains a diagnostic challenge as clinical presentation mimics other gallbladder diseases such as cholecystitis and imaging features may mimic gallbladder carcinoma[5]. There are reports describing varied clinical profile and associations with gallbladder TB[2,4,6]. Majority of reports describe patients presenting with constitutional symptoms such as fever, anorexia, weight loss and/or an underlying immuno-suppressed state in patients with gallbladder TB. In this report, we present a case of isolated gallbladder TB mimicking acute cholecystitis in an immunocompetent patient with no significant past medical history.
A 44-year-old Filipino lady presented with a 11-d history of right hypochondrium and epigastric pain which worsened after meals.
A 44-year-old Filipino lady presented with a 11-d history of right hypochondrium and epigastric pain which worsened after meals. There was no history of fever, night sweats, cough with hemoptysis, tea-coloured urine, pale stools or unintentional weight loss.
She had no significant past history.
On examination, there was no scleral icterus and Murphy’s sign was positive. There was no cervical lymphadenopathy. Physical examination was otherwise unremarkable.
Serum biochemistry revealed neutrophil-predominant leukocytosis with normal liver and renal function tests. Her blood cultures did not reveal microbial growth.
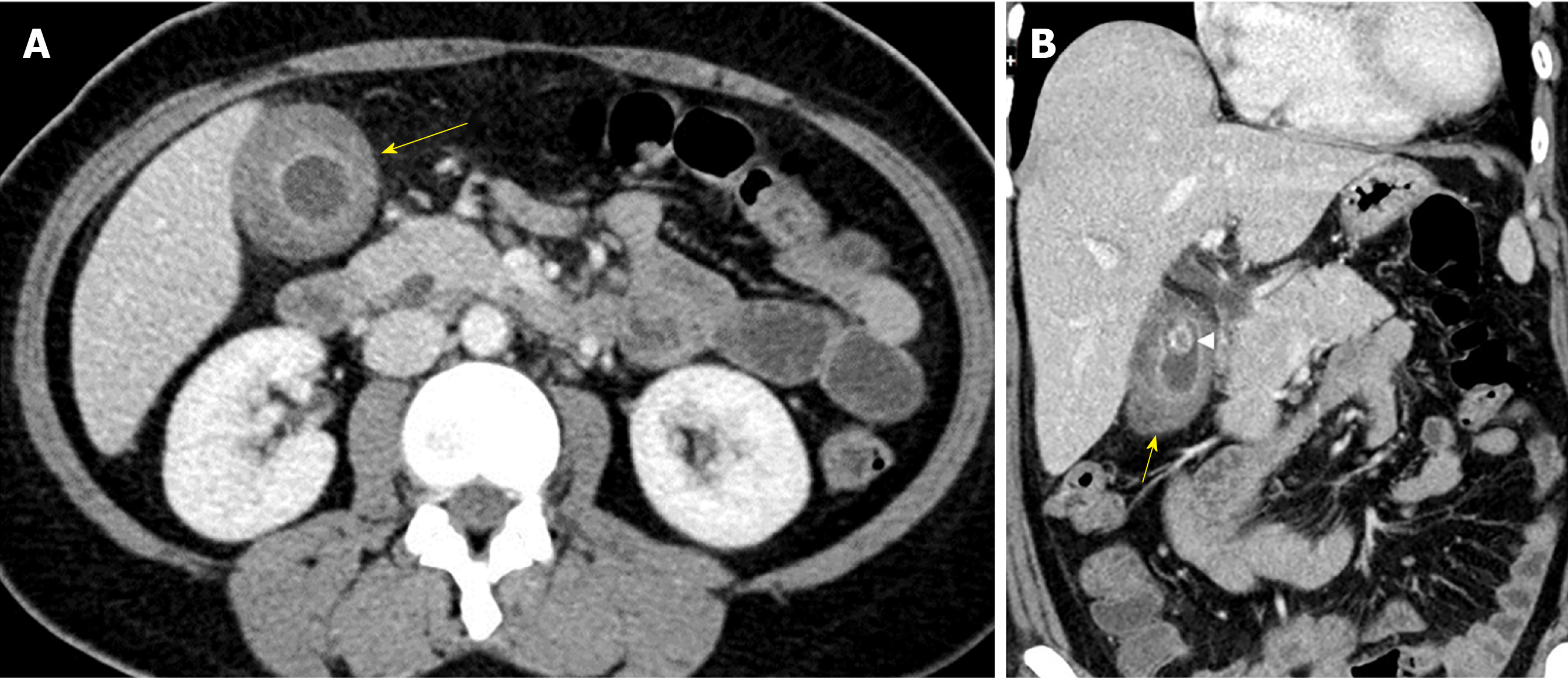
Chest x-ray was normal and computerized tomography scan of the abdomen and pelvis (CTAP) showed heterogeneous density of the gallbladder wall with marked gallbladder wall edema and a gallstone (Figure 1). The gallbladder wall thickness was 15 mm; the size of the extrahepatic common bile duct was 8.5 mm and the intrahepatic bile ducts were not dilated. CTAP also showed mesenteric and retroperitoneal lymphadenopathy which was deemed non-specific by size criteria.
A final diagnosis of acute on chronic cholecystitis secondary to gallbladder TB was made.
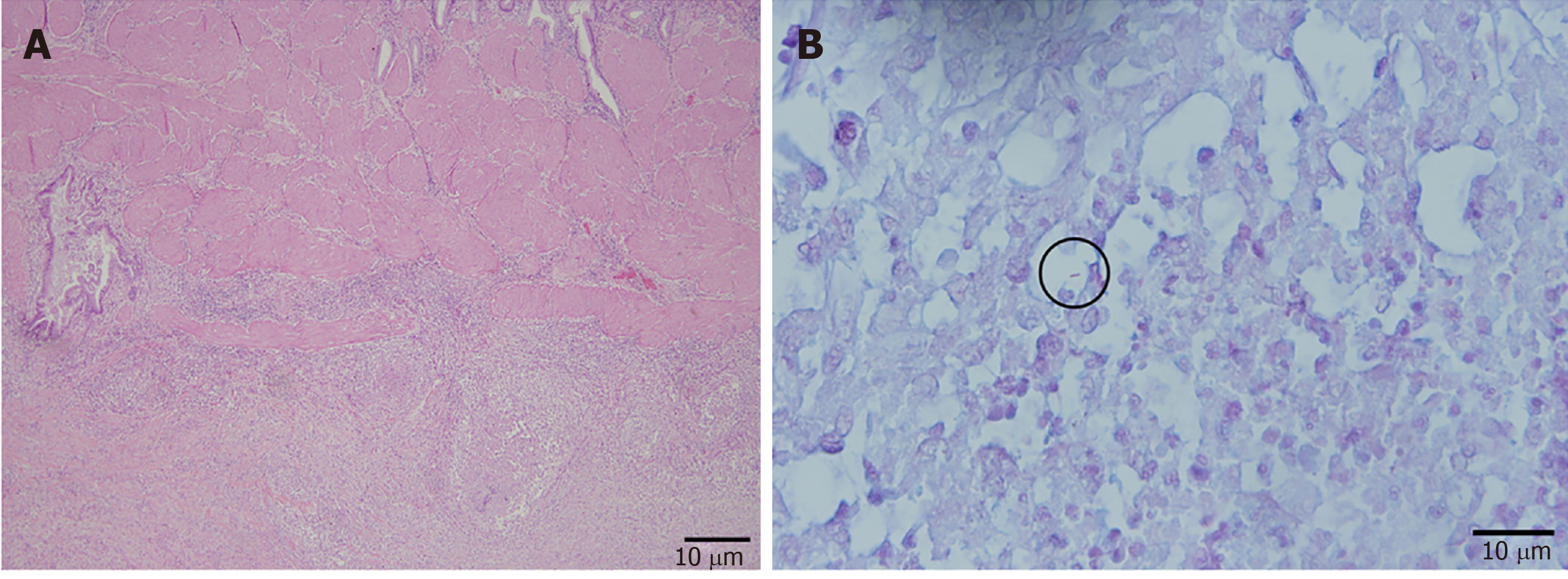
She was started on empiric antibiotics according to local antibiogram[7] and a laparoscopic cholecystectomy was scheduled during the admission[8]. The 10-point intra-operative gallbladder scoring system (G10) operation score was 5[9]. Intra-operatively, a chronically thickened and acutely inflamed gallbladder was covered by moderate grade omental adhesions. The gallbladder contained a 3 cm stone. On histology, the sections of the gallbladder revealed features of acute on chronic cholecystitis as well as necrotizing granulomatous inflammation. Rare acid-fast bacilli (AFB) was identified on Ziehl-Neelsen stain (Figure 2).
The patient recovered uneventfully. She was subsequently discharged and followed-up at a hospital in her home country due to financial and social reasons. Details on her follow-up are unfortunately unavailable.
Gallbladder TB is a rare entity due to population vaccination and intrinsic resistance for tuberculous infections[2,10]. It is associated with concomitant gallbladder lesions, especially cholelithiasis[2-4,11]. Epidemiologically, TB involving the hepatobiliary system is more common in Filipino patients like ours[1].
Four distinct clinical manifestations of gallbladder TB have been described[12,13]: (1) As part of miliary TB; (2) As part of disseminated abdominal TB; (3) As isolated gallbladder TB often found incidentally on microscopic examination of resected gallbladder; and (4) As part of an immunocompromised state such as uraemia, cancer or acquired immunodeficiency syndrome[10]. Our patient presented with a clinical profile consistent with acute cholecystitis and diagnosis was incidental on final histology.
Gallbladder TB remains a diagnostic challenge due to its rarity, non-specific presentation and investigation results. Common presentations of gallbladder TB include abdominal pain, fever, anorexia and weight loss[14]. Gallbladder perforation with intrahepatic biloma is also described[4]. Initial biochemical investigations for gallbladder TB are non-specific, such as a neutrophilic-predominant leukocytosis. A study by Xu et al[5] also showed that CTAP imaging for gallbladder TB may mimic a polyp, cholecystitis or carcinoma. The presence of heterogenous enhancement of the gallbladder may suggest caseating or liquefactive necrosis, which was found in our patient (Figure 1). However, the possibility of gallbladder TB was not a consideration in this patient with no significant past medical history and absence of immunosuppression. Prominent retroperitoneal and mesenteric nodes are likely to be reactive and non-specific. The possibility of a gallbladder TB based on the CTAP finding is only able to be considered retrospectively after histopathological analysis reveals AFB. Ultrasound-guided fine needle aspiration cytology of the gallbladder, although not commonly performed in clinical practice, may suggest the presence of gallbladder TB: Multiple granulomas with inflammatory and multinucleated giant cells and a positive Ziehl-Neelsen stain[15]. Histology is confirmatory and pre-operative predictors of gallbladder TB are not specific or validated due to paucity of data[2,3,14,16]. Cholecystectomy during the initial hospitalisation is recommended for patients with acute cholecystitis as it reduces length of stay, reduces cost and also restores quality of life[17].
The diagnosis of gallbladder TB warrants the need for investigation of additional sites of inoculation of TB – via AFB smear and culture of induced sputum, blood culture and polymerase chain reaction (PCR) assay. Positive pulmonary TB results warrant the need for contact tracing and screening of all TB contacts under the local TB guidelines[18]. This was not possible as our patient defaulted the follow-up. Should there be presence of biliary involvement, pre-operative diagnostic aids include the use of polymerase chain reaction of biliary aspirate via endoscopic retrograde cholangiopancreatography, which is more sensitive as compared to AFB staining[19].
The management of gallbladder TB is similar to the management of pulmonary and/or intra-abdominal TB. The use of quadruple therapy (inclusive of rifampicin, isoniazid, pyrazinamide and ethambutol) remains the gold standard[20]. If the disease is complicated by biliary obstruction, endoscopic or surgical management is still essential to relieve the obstruction in addition to anti-tuberculous treatment[21].
This case illustrates gallbladder TB with acute presentation in a previously well patient. The findings on CTAP imaging similarly mimics acute cholecystitis and a definite diagnosis was only reached post-operatively after histopathological confirmation. This report highlights the multivariable clinical presentations of gallbladder TB. Clinicians should have a high index of suspicion for patients in endemic regions presenting with cholecystitis to obtain a pre-operative diagnosis. Gallbladder TB is a rare entity but should be suspected in patients from endemic regions with risk factors such as underlying immunosuppression or history of TB. Gallbladder TB may mimic various pathologies such as cholecystitis or malignancy.
We would like to thank the Department of General Surgery, Radiology and Pathology of Tan Tock Seng Hospital for the support.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Singapore
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Donmez T, Gumbs A, Qayed E S-Editor: Yan JP L-Editor: A E-Editor: Ma YJ
| 1. | Chaudhary P. Hepatobiliary tuberculosis. Ann Gastroenterol. 2014;27:207-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 2. | Jain R, Sawhney S, Bhargava D, Berry M. Gallbladder tuberculosis: sonographic appearance. J Clin Ultrasound. 1995;23:327-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Abu-Zidan FM, Zayat I. Gallbladder tuberculosis (case report and review of the literature). Hepatogastroenterology. 1999;46:2804-2806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 4. | Hahn ST, Park SH, Shin WS, Kim CY, Shinn KS. Gallbladder tuberculosis with perforation and intrahepatic biloma. J Clin Gastroenterol. 1995;20:84-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Xu XF, Yu RS, Qiu LL, Shen J, Dong F, Chen Y. Gallbladder tuberculosis: CT findings with histopathologic correlation. Korean J Radiol. 2011;12:196-202. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Bergdahl L, Boquist L. Tuberculosis of the gall-bladder. Br J Surg. 1972;59:289-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Shelat VG, Wang Q, Chia CL, Wang Z, Low JK, Woon WW. Patients with culture negative pyogenic liver abscess have the same outcomes compared to those with Klebsiella pneumoniae pyogenic liver abscess. Hepatobiliary Pancreat Dis Int. 2016;15:504-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Amirthalingam V, Low JK, Woon W, Shelat V. Tokyo Guidelines 2013 may be too restrictive and patients with moderate and severe acute cholecystitis can be managed by early cholecystectomy too. Surg Endosc. 2017;31:2892-2900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 57] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 9. | Sugrue M, Coccolini F, Bucholc M, Johnston A, Contributors from WSES. Intra-operative gallbladder scoring predicts conversion of laparoscopic to open cholecystectomy: a WSES prospective collaborative study. World J Emerg Surg. 2019;14:12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 53] [Article Influence: 7.6] [Reference Citation Analysis (4)] |
| 10. | Yu R, Liu Y. Gallbladder tuberculosis: case report. Chin Med J (Engl). 2002;115:1259-1261. [PubMed] |
| 11. | Rouas L, Mansouri F, Jahid A, Zouaidia F, Saïdi H, Nabih N, Benabdellah M, Laraqui L, Mahassini N, Bernoussi Z, Elhachimi A. [Gallbladder tuberculosis associated with cholelithiasis]. Rev Med Liege. 2003;58:757-760. [PubMed] |
| 12. | Weitz G. [Tuberculosis of the gallbladder]. Langenbecks Arch Klin Chir Ver Dtsch Z Chir. 1955;280:318-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 13. | Piper C, Gamstätter G, Bettendorf U, von Egidy H. [Gallbladder tuberculosis. Review and case report of a patient with advanced renal failure]. Leber Magen Darm. 1987;17:381-382, 385-386. [PubMed] |
| 14. | Saluja SS, Ray S, Pal S, Kukeraja M, Srivastava DN, Sahni P, Chattopadhyay TK. Hepatobiliary and pancreatic tuberculosis: a two decade experience. BMC Surg. 2007;7:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 83] [Cited by in RCA: 78] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 15. | Rana C, Krishnani N, Kumari N. Ultrasound-guided fine needle aspiration cytology of gallbladder lesions: a study of 596 cases. Cytopathology. 2016;27:398-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Ramia JM, Muffak K, Fernández A, Villar J, Garrote D, Ferron JA. Gallbladder tuberculosis: false-positive PET diagnosis of gallbladder cancer. World J Gastroenterol. 2006;12:6559-6560. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 39] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Yu H, Chan EE, Lingam P, Lee J, Woon WWL, Low JK, Shelat VG. Index admission laparoscopic cholecystectomy for acute cholecystitis restores Gastrointestinal Quality of Life Index (GIQLI) score. Ann Hepatobiliary Pancreat Surg. 2018;22:58-65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Ministry of Health Singapore. Prevention, Diagnosis and Management of Tuberculosis. 2016; Available from: https://www.moh.gov.sg/docs/librariesprovider4/guidelines/moh-tb-cpg-full-version-for-website.pdf. |
| 19. | Govindasamy M, Srinivasan T, Varma V, Mehta N, Yadav A, Kumaran V, Nundy S. Biliary tract tuberculosis--a diagnostic dilemma. J Gastrointest Surg. 2011;15:2172-2177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Getahun H, Matteelli A, Abubakar I, Aziz MA, Baddeley A, Barreira D, Den Boon S, Borroto Gutierrez SM, Bruchfeld J, Burhan E, Cavalcante S, Cedillos R, Chaisson R, Chee CB, Chesire L, Corbett E, Dara M, Denholm J, de Vries G, Falzon D, Ford N, Gale-Rowe M, Gilpin C, Girardi E, Go UY, Govindasamy D, D Grant A, Grzemska M, Harris R, Horsburgh CR, Ismayilov A, Jaramillo E, Kik S, Kranzer K, Lienhardt C, LoBue P, Lönnroth K, Marks G, Menzies D, Migliori GB, Mosca D, Mukadi YD, Mwinga A, Nelson L, Nishikiori N, Oordt-Speets A, Rangaka MX, Reis A, Rotz L, Sandgren A, Sañé Schepisi M, Schünemann HJ, Sharma SK, Sotgiu G, Stagg HR, Sterling TR, Tayeb T, Uplekar M, van der Werf MJ, Vandevelde W, van Kessel F, van't Hoog A, Varma JK, Vezhnina N, Voniatis C, Vonk Noordegraaf-Schouten M, Weil D, Weyer K, Wilkinson RJ, Yoshiyama T, Zellweger JP, Raviglione M. Management of latent Mycobacterium tuberculosis infection: WHO guidelines for low tuberculosis burden countries. Eur Respir J. 2015;46:1563-1576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 393] [Cited by in RCA: 441] [Article Influence: 40.1] [Reference Citation Analysis (0)] |
| 21. | Iwai T, Kida M, Kida Y, Shikama N, Shibuya A, Saigenji K. Biliary tuberculosis causing cicatricial stenosis after oral anti-tuberculosis therapy. World J Gastroenterol. 2006;12:4914-4917. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |