Published online Dec 27, 2020. doi: 10.4240/wjgs.v12.i12.534
Peer-review started: September 26, 2020
First decision: October 21, 2020
Revised: November 12, 2020
Accepted: December 2, 2020
Article in press: December 2, 2020
Published online: December 27, 2020
Processing time: 86 Days and 1.3 Hours
Liver tissue situated outside the liver with a hepatic connection is usually called an accessory liver, and that without a connection to the mother liver, is called ectopic liver tissue.
To identify studies in the literature on ectopic liver tissue located on the gallbladder surface or mesentery.
We present two patients and review published articles on ectopic liver tissue located on the gallbladder surface accessed via PubMed, MEDLINE, Google Scholar, and Google databases. Keywords used included accessory liver lobe, aberrant liver tissue, ectopic liver tissue, ectopic liver nodule, heterotopic liver tissue, hepatic choristoma, heterotopic liver tissue on the gallbladder, and ectopic liver tissue on the gallbladder. The search included articles published before June 2020 with no language restriction. Letters to the editor, case reports, review articles, original articles, and meeting presentations were included in the search. Articles or abstracts containing adequate information on age, sex, history of liver disease, preliminary diagnosis, radiologic tools, lesion size, surgical indication, surgical procedure, and histopathological features of ectopic liver tissue were included in the study.
A total of 72 articles involving 91 cases of ectopic liver tissue located on the gallbladder surface or mesentery were analyzed. Of these 91 patients, 62 were female and 25 were male (no gender available for 4 patients), and the age range was 5 d to 91 years. Forty-nine patients underwent surgery for chronic cholecystitis or cholelithiasis, and 14 patients underwent surgery for acute cholecystitis. The remaining 28 patients underwent laparotomy for other reasons. Cholecystectomy was laparoscopic in 69 patients and open in 11 patients. The remaining 19 patients underwent various other surgical procedures such as autopsy, liver transplantation, living donor hepatectomy, Whipple procedure, and liver segment V resection. Histopathologically, hepatocellular carcinoma was detected in the ectopic liver tissue of one patient.
Ectopic liver tissue is a rare developmental anomaly which is usually detected incidentally. Although most studies suggest that ectopic liver located outside the gallbladder has a high risk of hepatocellular carcinoma, this is not reflected in statistical analysis.
Core Tip: Ectopic liver tissue is a rare developmental anomaly usually detected incidentally. While it is often asymptomatic, there is a risk of malignant transformation and other complications such as bleeding and torsion. In this review, we present two cases of ectopic liver tissue located on the gallbladder surface and review published studies on ectopic liver tissue located on the gallbladder surface accessed via the PubMed, MEDLINE, Google Scholar, and Google databases. Although most studies suggest that ectopic liver located outside the gallbladder has a higher risk of hepatocellular carcinoma, this is not reflected in the statistical analysis.
- Citation: Akbulut S, Demyati K, Ciftci F, Koc C, Tuncer A, Sahin E, Karadag N, Yilmaz S. Ectopic liver tissue (choristoma) on the gallbladder: A comprehensive literature review. World J Gastrointest Surg 2020; 12(12): 534-548
- URL: https://www.wjgnet.com/1948-9366/full/v12/i12/534.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v12.i12.534
Ectopic liver tissue is a rare developmental anomaly in which the liver tissue is situated outside the liver. It is usually asymptomatic and is discovered incidentally during surgery or autopsy, but there are potential complications. Torsion, malignant transformation, compression of adjacent organs, and intra-peritoneal bleeding are among the possible complications[1-72].
Liver tissue situated outside the liver with a hepatic connection is usually called an accessory liver, and that without a connection to the main liver, is called ectopic liver tissue. Accessory liver and ectopic liver tissues were first described by Morgagni in 1767 and by Corsy in 1922, respectively[1,20,36,72]. Subsequent reports showed that the accessory liver lobe most commonly occurs in the gallbladder wall, under the surface of the liver, at the gastrohepatic ligament, umbilical cord, adrenal glands, pancreas, pylorus, diaphragm, and the splenic capsule if a portion of the pars hepatica is displaced[28,31,34,44,36]. The histological architecture of the ectopic tissue resembles normal liver, although it does not have a complete functional architecture, is metabolically handicapped, and is more prone to carcinogenesis[2,6,36,40,62,72]. In this article, we report two cases of ectopic liver tissue and review the literature for articles published on ectopic liver tissue on the gallbladder surface or gallbladder mesentery[1-72]. The clinical and pathological characteristics are described in addition to an analysis of the possible clinical implications including malignant transformation.
The primary aim of this study was to review the articles published in the literature on ectopic liver tissue on the gallbladder surface or gallbladder mesentery. To achieve this aim, a literature search was conducted on PubMed, MEDLINE, Google Scholar, and Google databases using the following keywords: Accessory liver lobe, aberrant liver tissue, ectopic liver tissue, ectopic liver nodule, heterotopic liver tissue, hepatic choristoma, liver, gallbladder, heterotopic liver tissue on the gallbladder, ectopic liver tissue on the gallbladder, accessory liver lobe on the gallbladder, accessory liver tissue on the gallbladder alone or in different combinations. Language restrictions were not applied in this literature review. All documents published on ectopic liver tissue related to the gallbladder before June 2020 were reviewed. Patients with ectopic liver tissue found in the gallbladder lumen incidentally were excluded from the study. As a result, articles without an accessible full-text version, those without adequate information in the abstract, and those that did not include comprehensive information compared to other studies were excluded. The following information was collected: Publication year, country, type of article available (full-text, abstract), age, sex, clinical presentation, diagnostic modalities, indication for surgery, surgical approach, postoperative complications, and histopathologic features of specimens. The details of the literature search are provided in Table 1. The secondary aim of this study was to present two cases of ectopic liver tissue attached to the gallbladder wall that was discovered during living donor hepatectomy and recipient hepatectomy.
| Ref. | Year | Country | Language | Age | Sex | History of liver disease | Preliminary diagnosis | Radiologic tools |
| Kachi et al[1] | 2020 | Lebanon | English | 44 | F | No | CC | US |
| 62 | F | No | CC | NA | ||||
| Avdaj et al[2] | 2020 | Kosovo | English | 47 | F | No | CC | US |
| Baral et al[3] | 2019 | United States | English | 67 | F | No | CC | US |
| Yuksel et al[4] | 2019 | Turkey | English | 34 | F | NA | CC | US |
| Mannan et al[5] | 2019 | S. Arabia | English | 38 | F | NA | AC | US |
| Isa et al[6] | 2019 | Bahrain | English | 42 | F | No | CC | US |
| Pandit et al[7] | 2019 | Nepal | English | 30 | F | NA | Biliary pancreatitis | US + MRCP |
| Granek et al[8] | 2019 | Australia | English | 36 | M | NA | AC | US |
| Lodha et al[9] | 2018 | India | English | 50 | M | NA | Kidney tumor | CT |
| Topcu et al[10] | 2018 | Turkey | English | 64 | F | NA | AC | US |
| 70 | F | NA | Icterus | US + CT + MR | ||||
| Burke et al[11] | 2018 | Ireland | English | 30 | F | NA | CC | US |
| Greenberg et al[12] | 2018 | United States | English | 52 | F | FLD | AP | US + CT |
| Termos et al[13] | 2017 | Kuwait | English | 73 | F | NA | GBC | US + CT |
| Weber-Alvarez et al[14] | 2017 | Mexico | English | 37 | F | NA | AC | US |
| Galimov et al[15] | 2017 | Russia | Russian | 70 | M | NA | AC | US |
| Handra-Luca et al[16] | 2016 | France | English | 68 | F | NA | CC | US |
| 56 | F | NA | CC | US | ||||
| Mani et al[17] | 2016 | United States | English | 56 | M | FLD | AC | CT |
| Ito et al[18] | 2016 | Japan | English | 59 | F | NA | CC | MR + CT |
| Leena et al[19] | 2016 | India | English | 25 | M | NA | Cadaver | Autopsy |
| Karaca et al[20] | 2016 | Turkey | English | 43 | F | NA | CC | US |
| Jaboury et al[21] | 2016 | Australia | English | 22 | F | NA | CC | NA |
| Yahya et al[22] | 2016 | Libya | English | 35 | F | NA | CC | US |
| 45 | F | NA | CC | US | ||||
| 45 | F | NA | CC | NA | ||||
| 20 | F | NA | Penetrating injury | NA | ||||
| Aslan et al[23] | 2016 | Turkey | English | 49 | F | NA | CC | US |
| Longjam et al[24] | 2016 | India | English | 42 | F | NA | CC | US |
| Kostov et al[25] | 2016 | Bulgaria | English | 49 | M | RCLM | RCLM | NA |
| Bal et al[26] | 2015 | Turkey | English | 51 | F | NA | CC | US |
| Smyth et al[27] | 2015 | Australia | English | 77 | F | NA | CC | US |
| Abhilash et al[28] | 2015 | India | English | 45 | F | NA | AC | US |
| Hussein et al[29] | 2015 | Lebanon | English | 49 | F | NA | AC | CT |
| Yankol et al[30] | 2015 | Turkey | English | 30 | M | No | Living donor | US + CT + MRCP |
| Arslan et al[31] | 2014 | Turkey | English | 59 | F | NA | CC | US |
| Pulle et al[32] | 2014 | India | English | 43 | F | NA | CC | US |
| Terakawa et al[33] | 2014 | Japan | Japanese | 33 | F | NA | CC | US + MRCP |
| Sirasanagandla et al[34] | 2013 | India | English | 62 | M | NA | Cadaver | NA |
| Hassan et al[35] | 2013 | India | English | 32 | F | NA | CC | US |
| Martinez et al[36] | 2013 | Brazil | English | 37 | F | NA | AC | US |
| Ozturk et al[37] | 2013 | Turkey | Turkish | 35 | F | No | CC | US |
| Yajima et al[38] | 2013 | Japan | Japanese | 73 | F | NA | CC | US + CT |
| Khan et al[39] | 2013 | India | English | 32 | F | NA | CC | NA |
| Karaman et al[40] | 2012 | Turkey | English | 63 | M | NA | CC | US |
| Patel et al[41] | 2012 | United Kingdom | English | 21 | F | NA | CC | US |
| Sozen et al[42] | 2012 | Turkey | Turkish | 40 | F | NA | CC | US |
| Catani et al[43] | 2011 | Italy | English | 72 | F | NA | AC | US |
| 83 | F | No | CC | US | ||||
| Dettmer et al[44] | 2011 | Switzerland | English | 91 | F | NA | AC | CT |
| Nagar et al[45] | 2011 | United States | English | 25 | F | NA | AP + Cystic mass | US + CT + MRCP |
| Ates et al[46] | 2010 | Turkey | Turkish | 64 | F | NA | AC | NA |
| 49 | M | NA | CC | US | ||||
| Triantafyllidis et al[47] | 2009 | Greece | English | 56 | F | NA | CC | US |
| Guzman et al[48] | 2009 | Mexico | Spanish | 36 | M | NA | CC | US |
| Kyeong et al[49] | 2008 | S. Korea | English | 66 | F | NA | CC | CT |
| Koh et al[50] | 2007 | Australia | English | 60 | F | NA | AC | NA |
| Malhas et al[51] | 2007 | United Kingdom | English | 42 | M | FLD | CC | US |
| 39 | F | NA | CC | US | ||||
| Soto et al[52] | 2007 | United States | English | 32 | F | NA | CC | US |
| Beltran et al[53] | 2007 | Chile | English | 47 | M | NA | CC | US |
| 33 | F | NA | CC | US | ||||
| 27 | M | NA | Gastric cancer | US + CT | ||||
| 35 | M | NA | Pancreatic pseudocyst | US + CT | ||||
| Wang et al[54] | 2006 | China | Chinese | 38 | M | NA | Gallbladder polyps | US |
| Ikeda et al[55] | 2006 | Japan | English | 70 | M | No | HCC + Cirr | US + CT |
| Ngowe et al[56] | 2006 | Cameroon | French | 46 | F | NA | CC | US |
| Lundy et al[57] | 2005 | United States | English | 38 | F | FLD | Liver tumor | US + CT |
| Leone et al[58] | 2004 | Italy | English | 54 | F | NO | GBC | US + CT |
| Griniatsos et al[59] | 2002 | United Kingdom | English | 39 | F | NA | CC | US |
| 49 | M | NA | CC | US | ||||
| Acar et al[60] | 2002 | Turkey | English | 55 | F | NA | CC | US |
| Sakarya et al[61] | 2002 | Turkey | English | NA | NA | NA | NA | NA |
| Arakawa et al[62] | 1999 | Japan | English | 48 | M | ALD | ALD | Autopsy |
| Hamdani et al[63] | 1994 | United States | English | 49 | M | Cirr | PSC | US + CT |
| Boyle et al[64] | 1992 | United States | English | 44 | F | No | AC | US |
| Tejada et al[65] | 1989 | United States | English | 43 | M | NA | CC + HS | US |
| Watanabe et al[66] | 1989 | Japan | English | 37 | M | CLL | CLL | CT |
| 54 | M | Cirr | ALD | Laparoscopy | ||||
| 64 | F | Cirr | Cirr | CT | ||||
| 71 | F | Cirr | Cirr | Laparoscopy | ||||
| Fellbaum et al[67] | 1987 | Austria | German | 34 | F | NA | CC | NA |
| Natori et al[68] | 1986 | Japan | English | 56 | F | NA | CC | CT |
| Ashby et al[69] | 1969 | United Kingdom | English | 42 | M | NA | Duodenal ulcer | NA |
| BASSIS et al[70] | 1956 | United States | English | NA | NA | NA | CC | NA |
| NA | NA | NA | CC | NA | ||||
| NA | NA | NA | CC | NA | ||||
| 5d | M | NA | Cadaver | No | ||||
| Thorsness et al[71] | 1941 | United States | English | 63 | F | NA | Cadaver | No |
| Cullen et al[72] | 1925 | United States | English | 33 | F | No | Jaundice | NA |
Using the PubMed, MEDLINE, Google Scholar, and Google databases, 72 articles involving 91 patients published between January 1925 and August 2020 were compatible with the above-mentioned criteria. The four countries with the highest numbers of published articles were Turkey (n = 13), the United States (n = 12), India (n = 8), and Japan (n = 7). Sixty-two articles were written in English, three in Turkish, two in Japanese, one in French, one in German, one in Chinese, one in Russian, and one in Spanish. The full text was obtained for 69 of the 72 articles, whereas only abstracts were available for three articles. Of the 91 patients, 62 were female and 25 male; no gender data were available for the remaining four patients. The age of these 87 patients ranged from five days to 91 years; this information was unavailable for the remaining four patients.
Eleven patients had a history of various liver diseases, while 12 patients had no liver disease. No data could be obtained on whether the remaining 68 patients had any liver disease. Forty-nine patients underwent surgery for chronic cholecystitis and/or cholelithiasis, while 14 patients underwent surgery for a presumed diagnosis of acute cholecystitis. The remaining 28 patients underwent laparotomy for unrelated reasons. Sixty-one patients underwent laparoscopic cholecystectomy and 11 underwent open cholecystectomy. The remaining 19 patients underwent cholecystectomy and various surgical procedures such as autopsy, liver transplantation, living donor hepatectomy, Whipple procedure, and liver segment V resection. Demographic, clinical, and histopathological characteristics of the 91 patients with ectopic liver tissue are summarized in Tables 1 and 2.
| Ref. | Lesion sizes (mm) | Surgical indication | Surgical procedure | Histopathological findings of ELT | Histopathological findings of GB |
| Kachi et al[1], 2020 | 10 | CC | LC | ELT | NA |
| 5 | CC | LC | ELT | NA | |
| Avdaj et al[2], 2020 | NA | CC | LC | ELT | NA |
| Baral et al[3], 2019 | 30 | CC | LC | ELT | NA |
| Yuksel et al[4], 2019 | 17 | CC | LC | ELT | CC |
| Mannan et al[5], 2019 | 5 | AC | LC | ELT | NA |
| Isa et al[6], 2019 | NA | CC | LC | ELT | NA |
| Pandit et al[7], 2019 | 35 | CC | LC | ELT | NA |
| Granek et al[8], 2019 | 19 | AC | LC | ELT | NA |
| Lodha et al[9], 2018 | 20 | Kidney tumor | Lap nephrectomy | ELT (no excised) | NA |
| Topcu et al[10], 2018 | 15 | CC | OC | ELT | NA |
| 80 | Pancreatic tumor | Whipple procedure | ELT | NA | |
| Burke et al[11], 2018 | NA | CC | LC | ELT | NA |
| Greenberg et al[12], 2018 | 30 | CC | LC | ELT | NA |
| Termos et al[13], 2017 | 30 | Diag lap | LC | ELT | NA |
| Weber-Alvarez et al[14], 2017 | 10 | AC | LC | ELT | AC + CC |
| Galimov et al[15], 2017 | 6 | AC | LC | ELT | Phlegmonous cholecystitis |
| Handra-Luca et al[16], 2016 | 5 | CC | LC | ELT | CC |
| 11 | CC | LC | ELT | CC | |
| Mani et al[17], 2016 | NA | CC | LC | ELT | NA |
| Ito et al[18], 2016 | 15 | CC | LC | ELT | NA |
| Leena et al[19], 2016 | 15 | Autopsy | Autopsy | ELT | NA |
| Karaca et al[20], 2016 | 15 | CC | LC | ELT | NA |
| Jaboury et al[21], 2016 | NA | CC | LC | ELT | NA |
| Yahya et al[22 ], 2016 | 60 | CC | LC | ELT | NA |
| NA | CC | LC | ELT | NA | |
| NA | CC | LC | ELT | NA | |
| NA | Penetrating injury | Diag lap | ELT | NA | |
| Aslan et al[23], 2016 | 8 | CC | LC | ELT | NA |
| Longjam et al[24], 2016 | 15 | CC | LC | ELT | CC |
| Kostov et al[25], 2016 | 35 | RCLM | OC | ELT | Hydatid cyst on gallbladder wall |
| Bal et al[26], 2015 | 20 | CC | LC | ELT | NA |
| Smyth et al[27], 2015 | 20 | CC | LC | ELT | CC |
| Abhilash et al[28], 2015 | 10 | AC | LC | ELT | CC |
| Hussein et al[29], 2015 | NA | AC | LC | ELT | NA |
| Yankol et al[30], 2015 | 15 | Donor hepatectomy | LDH | ELT | Accessory gallbladder tissue |
| Arslan et al[31], 2014 | 20 | CC | LC | ELT | NA |
| Pulle et al[32], 2014 | 20 | CC | LC | ELT | CC |
| Terakawa et al[33], 2014 | 12 | CC | LC | ELT | NA |
| Sirasanagandla et al[34], 2013 | 20 | Autopsy | Autopsy | ELT | NA |
| Hassan et al[35], 2013 | 10 | CC | LC | ELT | CC |
| Martinez et al[36], 2013 | 30 | CC | LC | ELT | Chronic inflammation |
| Ozturk et al[37], 2013 | 20 | CC | LC | ELT | NA |
| Yajima et al[38], 2013 | 6 | CC | LC | ELT | NA |
| Khan et al[39], 2013 | NA | CC | LC | ELT (Fatty change) | CC |
| Karaman et al[40], 2012 | 11 | CC | LC | ELT | NA |
| Patel et al[41], 2012 | 26 | CC | LC | ELT | NA |
| Sozen et al[42], 2012 | 7 | CC | LC | ELT | NA |
| Catani et al[43], 2011 | 15 | AC | LC | ELT | NA |
| 14 | CC | LC | ELT | NA | |
| Dettmer et al[44], 2011 | 15 | AC | LC | ELT | Acute cholecystitis |
| Nagar et al[45], 2011 | 45 | AP + Cystic mass | LC | ELT | CC |
| Ates et al[46], 2010 | 5 | AC | LC | ELT | NA |
| 6 | CC | LC | ELT | NA | |
| Triantafyllidis et al[47], 2009 | 15 | CC | LC | ELT | CC |
| Guzman et al[48], 2009 | 30 | CC | LC | ELT | NA |
| Kyeong et al[49], 2008 | 10 | CC | LC | ELT | CC |
| Koh et al[50], 2007 | 15 | AC | LC | ELT | NA |
| Malhas et al[51], 2007 | NA | CC | LC | ELT | NA |
| NA | CC | LC | ELT | NA | |
| Soto et al[52], 2007 | 8 | CC | LC | ELT | NA |
| Beltran et al[53], 2007 | 12 | CC | LC | ELT | CC |
| 17 | CC | LC | ELT | NA | |
| 7 | Gastric cancer | OC + Gastrectomy | ELT | NA | |
| 18 | Pancreatic pseudocyst | OC + Gastrectomy | ELT | NA | |
| Wang et al[54], 2006 | 11 | Gallbladder polyps | LC | ELT | CC + Polyps |
| Ikeda et al[55], 2006 | NA | HCC | OC + Segment V Resection | NASH | NA |
| Ngowe et al[56], 2006 | 30 | CC | LC | ELT | CC |
| Lundy et al[57], 2005 | 30 | Diag lap | LC | ELT | NA |
| Leone et al[58], 2004 | 90 | GBC | OC | ELT + HCC | NA |
| Griniatsos et al[59], 2002 | 10 | CC | LC | ELT | NA |
| 15 | CC | LC | ELT | NA | |
| Acar et al[60], 2002 | 14 | CC | OC | ELT | Papillary epithelial hyperplasia |
| Sakarya et al[61], 2002 | NA | NA | LC | NA | NA |
| Arakawa et al[62], 1999 | 15 | Autopsy | Autopsy | ELT | NA |
| Hamdani et al[63], 1994 | 30 | PSC | LT | ELT | NA |
| Boyle et al[64], 1992 | 20 | AC | OC | ELT | CC |
| Tejada et al[65], 1989 | 11 | CC | OC + Splenectomy | ELT | CC |
| Watanabe et al[66], 1989 | 5 | Cystic lesion of the liver | Diag lap | Biliary hamartoma | NA |
| 8 | Cirr | Diag lap | NA | NA | |
| 10 | Cirr | Diag lap | NA | NA | |
| 6 | Cirr | Diag lap | NA | NA | |
| Fellbaum et al[67], 1987 | NA | NA | NA | NA | NA |
| Natori et al[68], 1986 | 12 | CC | OC + Excision | ELT | Chronic inflammation |
| Ashby et al[69], 1969 | 10 | Duodenal ulcer | OC + Excision | ELT | NA |
| BASSIS et al[70], 1956 | 15 | CC | OC | ELT | CC |
| 10 | CC | OC | ELT | CC | |
| 6 | CC | OC | ELT | CC | |
| 8 | Autopsy | Autopsy | ELT | NA | |
| Thorsness et al[71], 1941 | 5 | Autopsy | Autopsy | ELT | NA |
| Cullen et al[72], 1925 | 12 | Jaundice | Excision | NA | NA |
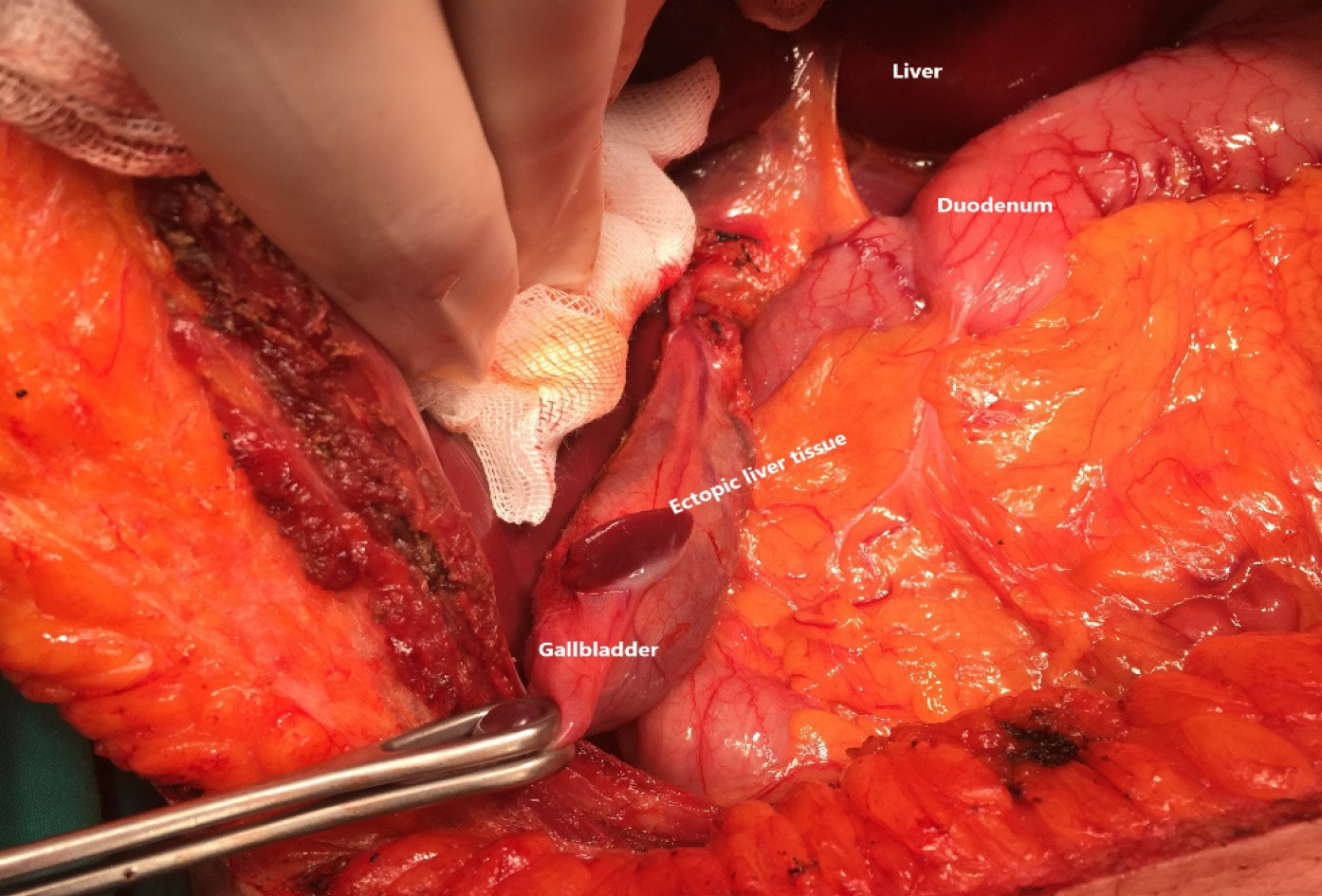
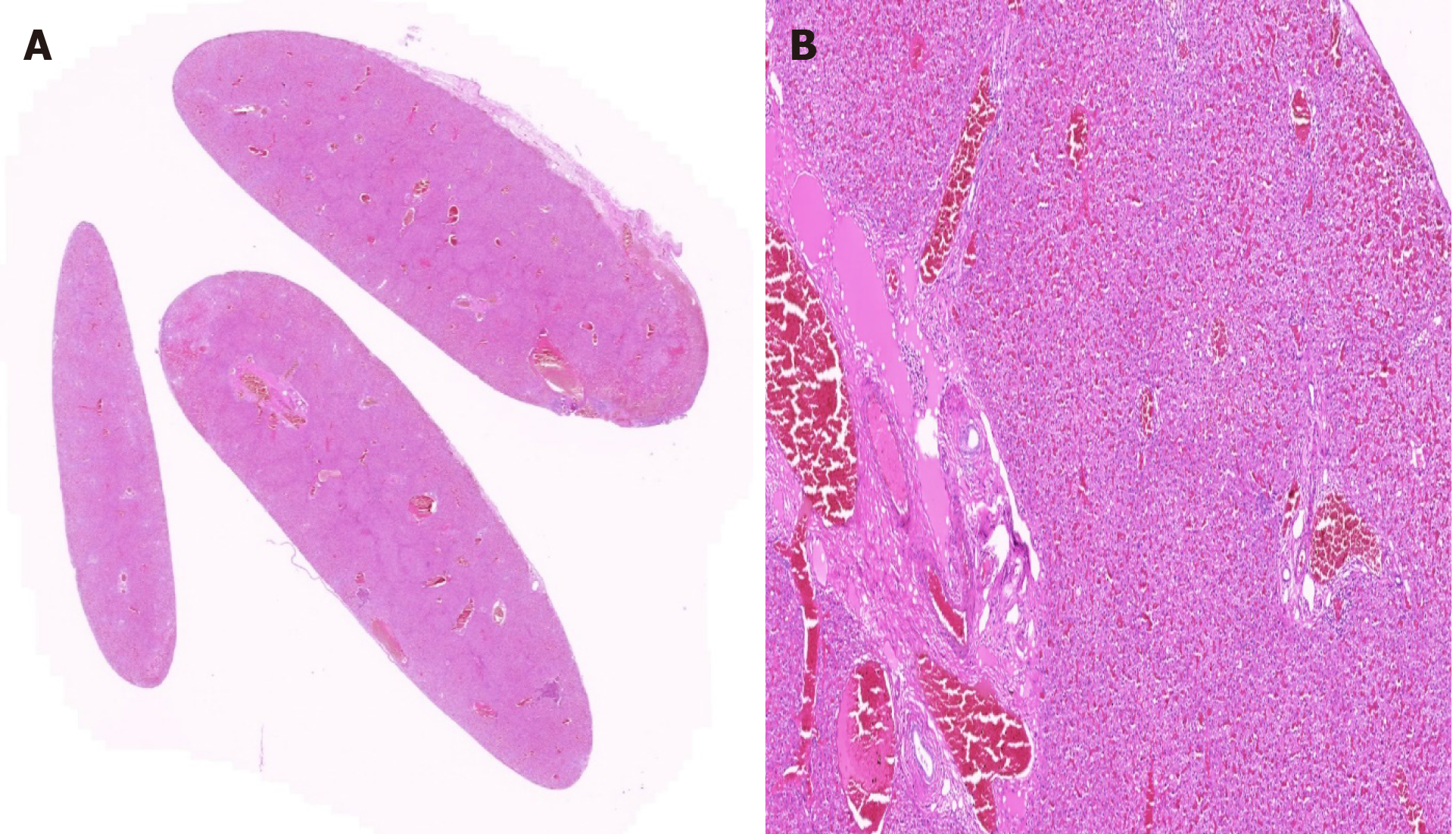
Case 1: A 25-year-old woman [body mass index (BMI): 27 kg/m2, A Rh (+), graft volume: 600 cc, remnant liver: 29%] was admitted to our liver transplant institute to donate a part of her liver to her 33-year-old sister with cryptogenic liver cirrhosis. Radiological and biochemical examinations were completed using the preoperative donor evaluation algorithm available in our liver transplant institute. The donor candidate underwent laparotomy using a modified Makuuchi incision (reversed L-shaped incision). The exploration showed ectopic liver tissue approximately 15 mm × 5 mm in size, located in the gallbladder corpus, and had no association with the liver (Figure 1). Cholecystectomy was performed to include the ectopic liver tissue, and cholangiography was carried out via the cystic duct, and the biliary tract anatomy was found to be normal (Choi Type I). Right lobe donor hepatectomy was performed as previously described in our transplant institute. The donor was discharged without any postoperative complications. Macroscopically, the gallbladder specimen was 70 mm in length, 50 mm in diameter, and 3 mm in wall thickness. Histopathologically, the tissue (15 mm × 3 mm × 2 mm) located in the gallbladder corpus was ectopic liver tissue (Figure 2A and B).
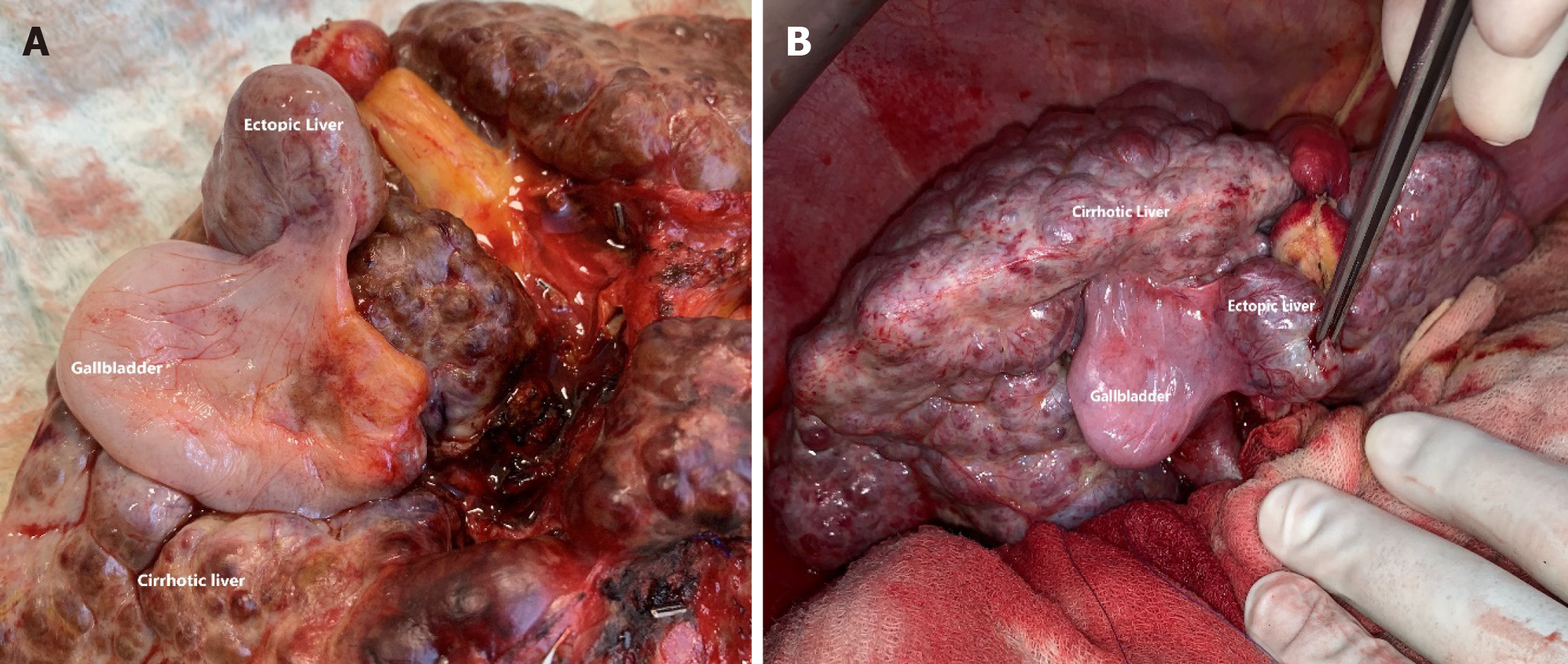
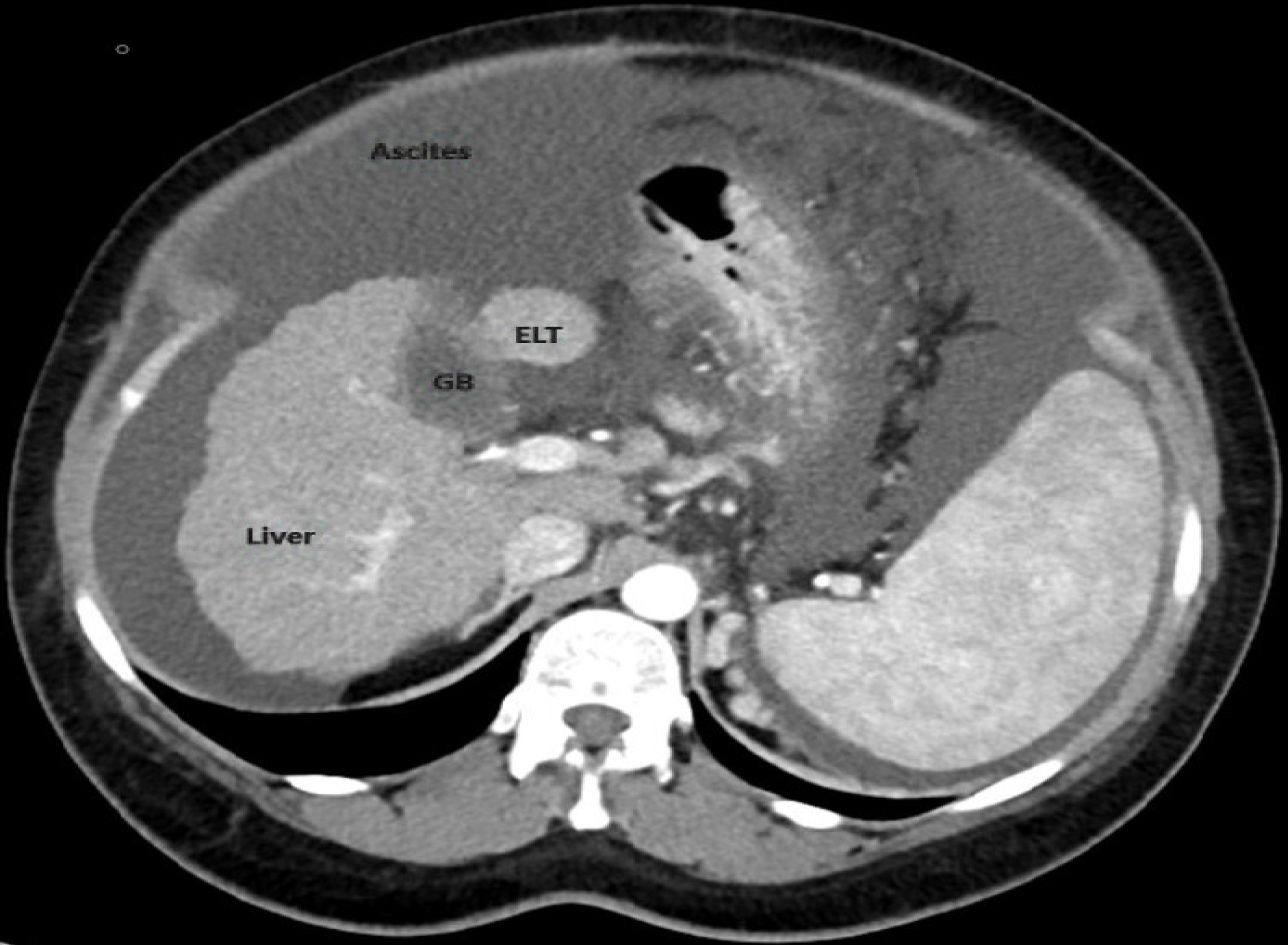
Case 2: A 45-year-old female patient with cryptogenic liver cirrhosis [BMI: 37.2 kg/m2, A Rh (-), MELD-Na: 16, Child: 10/C] presented to our liver transplant institute for live-donor liver transplantation. Both the liver recipient and the 40-year-old male [BMI: 25.5 kg/m2, A Rh (+), graft volume: 940 cc, remnant liver: 31%] living liver donor candidate were evaluated according to an algorithm consisting of radiological and biochemical analyses. Laparotomy was performed using a reversed L-shaped incision. During exploration, it was revealed that the liver had a macronodular appearance and a relatively small size. Ectopic liver tissue associated with the gallbladder mesentery was seen on the corpus of the gallbladder without an association with the liver. The ectopic liver tissue showed a cirrhotic appearance similar to the main liver tissue (Figure 3A and B). The gallbladder was removed en-bloc with the liver without recipient cholecystectomy as described previously (recipient hepatectomy). The recipient was discharged on postoperative day 15 without complications. The ectopic liver tissue, located in the gallbladder was also seen in the retrospective examinations of computed tomography sections (Figure 4).
Ectopic liver tissue is a rare developmental anomaly in which the liver tissue is situated outside the liver[9,19,28,60]. Four main types are described in the literature: Ectopic liver, which is not connected to the mother liver, and is usually attached to the gallbladder or intra-abdominal ligaments; microscopic ectopic liver found in the gallbladder wall; a large accessory liver lobe attached to the mother liver by a stalk; and a small accessory liver lobe, 10-30 g, attached to the mother liver[73]. However, this classification may not apply to all cases[60].
The real incidence of ectopic liver tissue attached to the gallbladder wall is difficult to assess; most cases are asymptomatic and are diagnosed at laparotomy, laparoscopy, or during an autopsy[1,2,14]. However, the incidence of ectopic liver tissue has been reported to range from 0.24% to 0.47%[2,31]. A review of 5500 autopsies showed that only 0.05% had ectopic liver tissue in which only three cases were attached to the gallbladder wall[74]. A review of 1060 laparoscopic procedures found ectopic liver tissue attached to the gallbladder wall in three patients (0.28%)[10]. To date, we detected only two (0.04%) patients with ectopic liver tissue among 4500 patients who underwent living donor hepatectomy or recipient hepatectomy
Different theories have been proposed to explain the development of an ectopic liver at various sites: Development of an accessory lobe of the liver with atrophy or regression of the original connection to the main liver; migration or displacement of a portion of the pars hepatica to other sites, entrapment of a nest of cells in the region of the foregut following closure of the diaphragm or umbilical ring and trapping of hepatocyte-destined mesenchyma in several areas thus budding hepatic tissue before the closure of the pleuroperitoneal canal[23,28]. Ectopic and accessory liver may occur at different sites, including sites close to the liver, such as the gallbladder and hepatic ligaments or sites far from the liver, for example, omentum, retroperitoneum, and thorax, with the most common location on the gallbladder[66,75,76].
Ectopic liver tissue varies considerably in size[60,62]. Based on 72 reports reviewed in this study, the average size of the ectopic liver tissue was found to be 17.8 mm. In the literature, the reported size of ectopic livers (without hepatocellular carcinoma) ranges from a few millimeters to several centimeters[24,44,58].
No detailed reports on the vascular supply of ectopic liver tissue were given in most of the papers reviewed. In general, three different vascular supply patterns have been described for gallbladder-associated ectopic liver tissue: An artery arising from the cystic artery[50], a vascular pedicle arising from the liver parenchyma substance[26], and vascular structures embedded in a mesentery lying from the hepatic site to ectopic liver tissue[43]. The identification of vascular supply requires surgery to avoid bleeding during the main surgery[3,4,26]. Extensive traction of the gallbladder should be avoided in cases with direct vascular supply from the liver substance. Biliary drainage was not described in detail or was not evident intraoperatively in most reports. In general, accessory liver lobes are classified into three types based on biliary drainage: In type I, the duct of the accessory liver lobe drains into an intrahepatic bile duct of the native liver; in Type II, it drains into an extrahepatic bile duct of the native liver, and if both the accessory lobe and the main liver have a common capsule and the bile duct of the accessory lobe drains into an extrahepatic duct, it is considered Type III[34,77].
Ectopic liver might be associated with other anomalies such as biliary atresia, agenesis of the caudate lobe, omphalocele, bile duct cyst, cardiac, and conotruncal anomalies; however, these abnormalities were not reported when the heterotopic tissue was attached to the surface of the gallbladder[28,59].
Ectopic liver tissue and accessory liver lobes are often asymptomatic, and detection of ectopic liver tissue before surgical intervention or autopsy imaging studies is rare[8,11,20,34]. However, ectopic livers on rare occasions have been reported to cause recurrent abdominal pain due to torsion[78-80], intraperitoneal bleeding[81,82], hemorrhagic necrosis[83], compression of adjacent organs[84], as well as obstruction of the esophagus[85], portal vein[86], and neonatal gastric outlet[87].
The histological architecture of the ectopic tissue resembles normal liver, with regular lobules, central veins, and normal portal areas in most cases[28,47,59]. Unusual architecture of hepatic tissue with absence of the classical hexagonal lobule pattern has been equally described[34]. Ectopic liver like the main liver tissue can undergo fatty changes, hemosiderosis, cholestasis, cirrhosis, hepatitis, or malignant degeneration to hepatocellular carcinoma[36]. Although ectopic liver tissue usually has normal histology of the liver, that is, normal portal structure, regular lobules, and central veins, ectopic liver tissue has an increased risk of hepatocellular carcinoma[27,43,53]. The reason for this increased risk of hepatocellular carcinoma in patients with ectopic liver tissue is unclear, it has been proposed that biliary drainage is insufficient and/or blood supply is reduced in the ectopic liver tissue[58]. Furthermore, many hepatocellular carcinoma cases are related to ectopic liver tissue, and are not associated with cirrhosis in the main liver. Arakawa and colleagues[62] reported that in 22 hepatocellular carcinoma cases related to ectopic liver tissue, only six cases (27%) had cirrhosis in the main liver.
It has been revealed that many authors have misinterpreted the results of the article by Yamashita and colleagues[78]. One of the most important reasons for this misinterpretation is that the article is written in Japanese. Another reason is that the authors copy each other directly without carefully reading the authors’ results[2,3,5,12,17,23,26,28,29,35,36,59,62]. In the review by Yamashita and colleagues[78], 70 cases of ectopic liver were reported in the literature up to 1985. One (4.5%) of 22 cases with ectopic hepatic tissue attached to the gallbladder developed hepatocellular carcinoma while eight (16.7%) of 48 cases with ectopic hepatic tissue located outside the gallbladder developed hepatocellular carcinoma. As a result of the statistical analysis carried out using the Yamashita and colleagues data, no statistically significant difference was found between ectopic liver tissue located on the gallbladder surface and its location outside the gallbladder in terms of hepatocellular carcinoma risk (P = 0.25). Many studies have suggested that ectopic liver tissue on the gallbladder is less susceptible to hepatocellular carcinoma development than ectopic liver tissue outside the gallbladder. A possible explanation proposed for this difference is that ectopic hepatic tissue attached to the gallbladder is an anomaly occurring later during the development of the biliary bud and is; therefore, well-differentiated[12,26,59,62]. However, the results of our analysis using the Yamashita and colleagues data[78] revealed that there was no difference. In the 72 articles reviewed in this study, including 91 patients with ectopic liver tissue attached to the gallbladder, only one patient reported having hepatocellular carcinoma in the ectopic liver tissue (1.09%).
Ectopic liver tissue is a rare developmental anomaly usually detected incidentally during surgery or autopsy. While it is often asymptomatic, it has a risk of malignant transformation and carries the potential for other complications such as bleeding and torsion. Although most studies have suggested that ectopic liver located outside the gallbladder has a higher risk of hepatocellular carcinoma, this is not reflected in the statistical analysis results.
Liver tissue situated outside the liver with a hepatic connection is usually called an accessory liver, and that without a connection to the mother liver, is called ectopic liver tissue. Ectopic liver tissue is a rare developmental anomaly usually detected incidentally.
Although a limited number of case reports on ectopic liver tissue on the gallbladder surface or gallbladder mesentery have been published to date, no systematic literature research has been conducted.
While the main objective of this study was to review the articles published in the medical literature on ectopic liver tissue on the gallbladder surface or gallbladder mesentery, the secondary objective of this study was to present the medical history of two patients diagnosed with ectopic liver tissue.
A systematic literature search was conducted on PubMed, Medline, Google Scholar, and Google databases using the following keywords: Accessory liver lobe, aberrant liver tissue, ectopic liver tissue, ectopic liver nodule, heterotopic liver tissue, hepatic choristoma, heterotopic liver tissue on the gallbladder, and ectopic liver tissue on the gallbladder. The search included articles published before June 2020 with no language restriction.
A total of 72 articles were identified involving 91 patients, 62 females and 25 males; no gender data were available for the remaining four patients. The age of these 87 patients ranged from five days to 91 years; this information was unavailable for the remaining four patients. Eleven patients had a history of various liver diseases, while 12 patients had no liver disease. Forty-nine patients had surgery for chronic cholecystitis and/or cholelithiasis, while 14 patients had surgery for a presumed diagnosis of acute cholecystitis. The remaining 28 patients underwent laparotomy for unrelated reasons. Sixty-one patients underwent laparoscopic cholecystectomy and 11 underwent open cholecystectomy. The remaining 19 patients underwent cholecystectomy and various surgical procedures such as autopsy, liver transplantation, living donor hepatectomy, Whipple procedure, and liver segment V resection.
Ectopic liver tissue is a rare developmental anomaly usually detected incidentally during surgery or autopsy. While it is often asymptomatic, it has a risk of malignant transformation and carries the potential of other complications such as bleeding and torsion.
First, a review of the literature and our clinical experience suggest that ectopic liver tissue-like lesions around the liver should be considered in the differential diagnosis of ectopic hepatocellular carcinoma, especially in patients with chronic liver disease. Therefore, even when the macroscopic appearance is normal, all ectopic liver tissue specimens should be sent for routine histopathological examination. Second, although most studies have suggested that ectopic liver located outside the gallbladder has a higher risk of hepatocellular carcinoma, this is not reflected in the statistical analysis results.
| 1. | Kachi A, Bou Rached C, El-Helou E, Kanj M, Kansoun AH. Incidental Finding of Ectopic Liver during Laparoscopic Cholecystectomy. Am J Case Rep. 2020;21:e921410. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (2)] |
| 2. | Avdaj A, Namani S, Cake A, Bytyqi A. Case report of ectopic hepatic tissue, a rare finding during a laparoscopic cholecystectomy. Int J Surg Case Rep. 2020;68:100-103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Baral S, Babel S, Thapa N, Chhetri RK. Ectopic Liver Tissue in the Gall Bladder: A Rare Entity. Cureus. 2019;11:e6323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Yuksel C, Donder Y, Yuksel Bulut ND, Izol U. Ectopic Liver Tissue On The Gallbladder. Bezmialem Sci. 2019;7:68-70. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Mannan AA, Alshumari OAE, Salama M, Anjok N. Rare Anomaly with Accessory Hepatic Lobe in Symptomatic Gall Bladder Surgery in Saudi Population: A Case Report. Int J Med Rev Case Rep. 2019;3:447-449. [DOI] [Full Text] |
| 6. | Isa M, Al-Mulla H, Al-Rayes A, Al-Marzooq R, Arora R. Case Report on a Rare Intraoperative Finding of Ectopic Liver Tissue Attached to Gallbladder Wall during Laparoscopic Cholecystectomy. Case Rep Surg. 2019;2019:1046909. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Pandit N, Sah R, Lacoul R. Ectopic Liver Tissue on the Gallbladder: a Rare Incidental Finding. Indian J Surg. 2019;81:94-95. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Granek RJ, Battye S, Wijeratne S. Ectopic liver attached to a chronically inflamed gallbladder: a rare and surgically challenging combination. ANZ J Surg. 2019;89:E388-E389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Lodha M, Pande H, Kumar S, Puranik A. Ectopic liver on gall bladder serosa a case report and brief review of literature. Indian J Clin Anat Physiolog. 2018;5:288-289. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Topcu R, Erkent M, Kendirci M, Sahiner IT. Ectopic Liver Tissue on the Gallbladder Wall: A Case Report and Literature Review. Indian J Research. 2018;7:582-583. |
| 11. | Burke EP, Harkins P, Arih I, O'Donoghue G. A case of ectopic liver tissue adherent to the gallbladder. J Surg Case Rep. 2018;2018:rjy128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Greenberg Y, Ahmed MF, Amog F. Ectopic Liver Found on Gall Bladder Wall during Laparoscopic Cholecystectomy. J Surg Oper Care. 2018;3:209. |
| 13. | Termos S, AlDuwaisan A, Alali M, Faour H, AlHomoud H, Alsaleh A. Gallbladder-associated symptomatic hepatic choristoma: Should you resect? Int J Surg Case Rep. 2017;41:243-246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Weber-Alvarez P, Weber-Sánchez LA, Carbó-Romano R, Garteiz-Martínez D. Laparoscopic treatment of hepatic choristoma in the gallbladder wall: A clinical case presentation and literature review. Rev Gastroenterol Mex. 2017;82:189-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Galimov OV, Khanov VO, Rudakov DM, Sagitdinov RR. [Ectopic liver tissue in gallbladder's wall]. Khirurgiia (Mosk). 2017: 95-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Handra-Luca A. Accessory liver lobe of the gallbladder in adults. Anat Sci Int. 2016;91:427-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Mani VR, Farooq MS, Soni U, Kalabin A, Rajabalan AS, Ahmed L. Case Report of Ectopic Liver on Gallbladder Serosa with a Brief Review of the Literature. Case Rep Surg. 2016;2016:7273801. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Ito S, Takeda R, Kokubo R, Kojima Y, Goto M, Tomiki Y, Sakamoto K. Accessory liver lobe attached to the gallbladder wall preoperatively detected by ultrasonography: A case report. Int J Surg Case Rep. 2016;26:205-208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Leena AB. A Case of Ectopic Liver Attached to the Gallbladder Wall. Ann Int Med Den Res. 2016;2:23-25. |
| 20. | Karaca G, Özden H, Pehlivanlı F, Pekcici MR, Yıldırım Y. Ectopic Liver Tissue on the Gallbladder: An Incidental Mass in Laparoscopy. Arch Iran Med. 2016;19:78-79. [PubMed] |
| 21. | Jaboury IA. Ectopic liver, choristoma and hepar succenturiatum. ANZ J Surg. 2016;86:524-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Yahya AI, Ehteweish M and Endash S. Choriostoma (Heterotopic Liver is it of Concern). Ann Surg Perioper Care. 2016;1:1005. |
| 23. | Aslan F, Akkas G. Ectopic Liver Attached to the Gallbladder Wall: A Rare Finding During Laparoscopic Cholecystectomy. Annals of Med Medical Educ. 2016;3:23-27. [DOI] [Full Text] |
| 24. | Longjam D, Devi LR, Sunitarani Kh. Choristoma of liver - A case report. J Evolution Med Dent Sci. 2016;5:6798-6799. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 25. | Kostov DV, Kobakov GL. Hydatid Cyst in Gallbladder-Associated Ectopic Liver. Ann Clin Cytol Pathol. 2016;2:1045. |
| 26. | Bal A, Yilmaz S, Yavas BD, Ozdemir C, Ozsoy M, Akici M, Kalkan M, Ersen O, Saripinar B, Arikan Y. A rare condition: Ectopic liver tissue with its unique blood supply encountered during laparoscopic cholecystectomy. Int J Surg Case Rep. 2015;9:47-50. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 27. | Smyth JK, Ng KS, Snclair EC, Kuo S. Hepatic Choristoma: an Unexpected Finding During Cholecystectomy. J Minim Invasive Surg Sci. 2015;4:e21162. |
| 28. | Abhilash S, Karthik K, Keisham Lokendra Singh, S. Ranita Devi, G. S. Moirangthem. Ectopic Liver in Gall Bladder: A Case Report. J Evolution Med Dent Sci. 2015;4:1574-1577. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 29. | Hussein BA, Abtar H, Al Shaghoury I, Zaaroura A, Zaaroura A, Oweidat M. Choristomas: An incidental ectopic liver: Case Report and Review of Literature. Int J Anat Res. 2015;3:1635-1637. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 30. | Yankol Y, Mecit N, Kanmaz T, Acarli K, Kalayoglu M. A very original case of a mini accessory liver lobe with its own gallbladder. Surg Radiol Anat. 2015;37:535-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Arslan Y, Altintoprak F, Serin KR, Kivilcim T, Yalkin O, Ozkan OV, Celebi F. Rare entity: Ectopic liver tissue in the wall of the gallbladder - A case report. World J Clin Cases. 2014;2:924-926. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 32. | Pulle MV, Mittal T, Dey A, Malik VK. Choristoma (Ectopia) of the liver over gallbladder- A rare congenital anomaly. Current Med Res Practice. 2014;4:174-176. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 33. | Terakawa H, Nakagawara H, Miyashita T, Takamura H, Kitagawa H, Ohta T. [A Case of Ectopic Liver Incidentally Found during Surgery. J Japan Surg Assoc. 2014;75:175-178. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 34. | Sirasanagandla SR, Kumar N, Nayak SB, Shetty SD, Bhat KM. Accessory liver lobe attached to the wall of the gallbladder: a cadaveric case report. Anat Sci Int. 2013;88:246-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (1)] |
| 35. | Hassan MJ, Khan S, Jetley S, Hussain M. Ectopic Liver Tissue Attached to Gallbladder- A Rare Incidental Finding. Int J Basic Applied Med Sci. 2013;3:60-64. |
| 36. | Martinez CA, de Resende HC Jr, Rodrigues MR, Sato DT, Brunialti CV, Palma RT. Gallbladder-associated ectopic liver: A rare finding during a laparoscopic cholecystectomy. Int J Surg Case Rep. 2013;4:312-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 37. | Ozturk A, Ucmakli E, Yananli Z. An ectopic liver tissue on the gallbladder. Gaziantep Med J. 2013;19:46-48. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 38. | Yajima H, Saito R, Yanagisawa A, Yanaga K. Ectopic Liver on the Serosal Surface of Gallbladder Found on Laparoscopic Cholecystectomy: A Case Report. J Japanese College of Surg. 2013;38:1097-1100. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 39. | Khan S, Jetley S, Husain M. Spectrum of histopathological lesions in cholecystectomy specimens: A study of 360 cases at a teaching hospital in South Delhi. Arch Int Surg. 2013;3:102-105. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 40. | Karaman K, Teke Z, Ercan M, Keklik TT, Bostanci EB, Akoglu M. Ectopic liver (choristoma) attached to the gallbladder wall. ANZ J Surg. 2012;82:948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 41. | Patel A, Yousuf SM, Abou Samra SW. Gall bladder associated ectopic liver. 2012. Available from: https://scientificsurgery.bjs.co.uk/image/gall-bladder-associated-ectopic-liver/. |
| 42. | Sozen S, Emir S, Ozdemir CS. Heterotopic liver tissue on the gallbladder wall: A case report Heterotopic liver tissue. Medical Journal of Kocaeli. 2012;1:42-45. |
| 43. | Catani M, De Milito R, Romagnoli F, Mingazzini P, Silvestri V, Usai V, Romeo V, Modini C. Ectopic liver nodules: a rare finding during cholecystectomy. G Chir. 2011;32:255-258. [PubMed] |
| 44. | Dettmer M, Cathomas G, Willi N. Alpha 1-antitrypsin retention in an ectopic liver. Diagn Pathol. 2011;6:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 45. | Nagar S, Koffron A, Raofi V. A Case of Hemorrhagic Necrosis of Ectopic Liver Tissue within the Gallbladder Wall. HPB Surg. 2011;2011:389381. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 46. | Ates M, Dirican A, Ara C, Yilmaz S. Ectopic Liver Tissue on the Gallbladder: Two Case Reports. J Inonu Univ Faculty Med. 2010;17:127-129. |
| 47. | Triantafyllidis I, Papapavlou L, Nikoloudis N, Economou A, Andreadis E, Chrissidou M, Georgakis K, Chrissidis T. Ectopic Liver Tissue Attached to the Gallbladder Wall: a case report. Cases J. 2009;2:6786. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 48. | Guzman RS, Gallegos VLP, Roblero JAV. [Liver coristoma: Case in the Hospital General de Zona No. 2 of the Instituto Mexicano del Seguro Social, laparoscopic surgery report. Tuxtla Gutierrez, Chiapas]. Rev Mex Cir Endoscop. 2009;10:130-132. |
| 49. | Kyeong HE, Park Y, Park S. Ectopic Liver Associated with the Gallbladder - A Brief Case Report. Korean J Pathol. 2008;42:128-130. |
| 50. | Koh CE, Hunt R. Ectopic liver encountered during laparoscopic cholecystectomy. Asian J Surg. 2007;30:227-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 51. | Malhas A, Howlader M, Chishti I, Siddiqui M. An incidental finding of ectopic liver tissue on the gallbladder of two patients during routine elective laparoscopic cholecystectomy. Internet J Surg 2007; 16. . |
| 52. | Soto FC, Szomstein S, Rosenthal RJ. Ectopic liver attached to the gallbladder: An unusual incidentaloma. Surgical Round 2007. Available from: https://www.hcplive. com/view/2007-04_07. |
| 53. | Beltran MA, Barria C, Pujado B, Barrera R, Mendez P, Pozo C. Hepatic heterototopic tissue on the gallbladder wall: an incidental finding with pathological potential. J Gastrointestin Liver Dis. 2007;16:347-349. [PubMed] |
| 54. | Wang Y, Liu FJ. [Ectopic liver tissue in the gallbladder serosa: a case report]. Zhonghua Ganzangbing Zazhi. 2006;14:369. [PubMed] |
| 55. | Ikeda H, Suzuki M, Takahashi H, Kobayashi M, Okuse N, Moriya H, Koike J, Maeyama S, Yotsuyanagi H, Itoh F. Hepatocellular carcinoma with silent and cirrhotic non-alcoholic steatohepatitis, accompanying ectopic liver tissue attached to gallbladder. Pathol Int. 2006;56:40-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 56. | Ngowe MN, Bahebeck J, Pisoh-Tangnym C, Mahop JB, Ndjolo A, Sosso AM. A choristoma of the gallbladder (ectopic liver). Louvain Med. 2006;125:311-313. |
| 57. | Lundy J, Johnson E, Edwards K, Rivera D. Laparoscopic management of gallbladder-associated ectopic liver. JSLS. 2005;9:485-487. [PubMed] |
| 58. | Leone N, De Paolis P, Carrera M, Carucci P, Musso A, David E, Brunello F, Fronda GR, Rizzetto M. Ectopic liver and hepatocarcinogenesis: report of three cases with four years' follow-up. Eur J Gastroenterol Hepatol. 2004;16:731-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 59. | Griniatsos J, Riaz AA, Isla AM. Two cases of ectopic liver attached to the gallbladder wall. HPB (Oxford). 2002;4:191-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 60. | Acar T, Taçyildiz R, Karakayali S. Ectopic liver tissue attached to the gallbladder. Acta Chir Belg. 2002;102:210-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 61. | Sakarya A, Erhan Y, Aydede H, Kara E, Ilkgül O, Ciftdoğan C. Ectopic liver (choristoma) associated with the gallbladder encountered during laparoscopic cholecystectomy: a case report. Surg Endosc. 2002;16:1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 62. | Arakawa M, Kimura Y, Sakata K, Kubo Y, Fukushima T, Okuda K. Propensity of ectopic liver to hepatocarcinogenesis: case reports and a review of the literature. Hepatology. 1999;29:57-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 118] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 63. | Hamdani SD, Baron RL. Ectopic liver simulating a mass in the gallbladder wall: imaging findings. AJR Am J Roentgenol. 1994;162:647-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 64. | Boyle L, Gallivan MV, Chun B, Lack EE. Heterotopia of gastric mucosa and liver involving the gallbladder. Report of two cases with literature review. Arch Pathol Lab Med. 1992;116:138-142. [PubMed] |
| 65. | Tejada E, Danielson C. Ectopic or heterotopic liver (choristoma) associated with the gallbladder. Arch Pathol Lab Med. 1989;113:950-952. [PubMed] |
| 66. | Watanabe M, Matsura T, Takatori Y, Ueki K, Kobatake T, Hidaka M, Hirakawa H, Fukukmoto S, Shimada Y. Five cases of ectopic liver and a case of accessory lobe of the liver. Endoscopy. 1989;21:39-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 72] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 67. | Fellbaum C, Beham A, Schmid C. [Isolated accessory liver (hepar succenturiatum) at the neck of the gallbladder. Case report with review of the literature]. Wien Klin Wochenschr. 1987;99:825-827. [PubMed] |
| 68. | Natori T, Hawkin S, Aizawa M, Asai T, Kameda Y, Ikuyohashi K. Intra-cholecystic ectopic liver. Acta Pathol Jpn. 1986;36:1213-1216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 69. | Ashby EC. Accessory liver lobe attached to the gall-bladder. Br J Surg. 1969;56:311-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 70. | Bassis ML, Izenstark JL. Ectopic liver; its occurrence in the gall bladder. AMA Arch Surg. 1956;73:204-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 71. | Thorsness ET. The relationship of ‘‘True Luschke Ducts,’’ adenoma, and aberrant liver tissue in the wall of the human gall bladder. Am J Clin Pathol. 1941;11:878-881. [RCA] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 72. | Cullen TS. An accessory hepatic lobe springing from the surface of the gallbladder. Arch Surg. 1925;11:718-764. [RCA] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 78] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 73. | Collan Y, Hakkiluoto A, Hastbacka J. Ectopic liver. Ann Chir Gynaecol. 1978;67:27-29. |
| 74. | Eiserth P [Contributions to the knowledge of the secondary liver]. Virchows Arch A Pathol Anat Histol. 1940;307:307-313. [RCA] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 31] [Article Influence: 0.4] [Reference Citation Analysis (1)] |
| 75. | Asada J, Onji S, Yamashita Y, Okada S, Morino M, Kanaoka M. Ectopic liver observed by peritoneoscopy: report of a case. Gastroenterol Endosc. 1982;24:309-315. [DOI] [Full Text] |
| 76. | Clearfield HR. Embryology, malformation and malposition of the liver. In: Berk JE, Haubrick WS, Kaiser MH, Roth JLA, Schaffner F (editors): Bockus Gastroenterology, 4th edn. Philadelphia: Saunders; 1985: 2659-2665. |
| 77. | Elmasalme F, Aljudaibi A, Matbouly S, Hejazi N, Zuberi MS. Torsion of an accessory lobe of the liver in an infant. J Pediatr Surg. 1995;30:1348-1350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 45] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 78. | Yamashita M, Nagamine Y, Ozaki K, Ueshima S, Takahashi H, Inoue H. An autopsy case of a cirrhotic ectopic liver with a review of the literature. Acta Hepatol Jpn. 1985;26:510-514. [RCA] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 79. | Corbitt N, Eric JR, Marta HS, Dai HC. Accessory hepatic lobes in the pediatric population: A report of three cases of torsion and literature review. JPS Case Reports. 2017;16:15-18. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 80. | Pujari BD, Deodhare SG. Symptomatic accessory lobe of liver with a review of the literature. Postgrad Med J. 1976;52:234-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 33] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 81. | Koplewitz BZ, Manson DE, Ein SH. Posttraumatic torsion of accessory lobe of the liver and the gallbladder. Pediatr Radiol. 1999;29:799-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 82. | Garba ES, Ameh EA. Isolated rupture of an accessory liver from blunt abdominal trauma in childhood. Pediatr Surg Int. 2002;18:62-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 83. | Parmeggiani D, Cimmino G, Cerbone D, Avenia N, Ruggero R, Gubitosi A, Docimo G, Mordente S, Misso C, Parmeggiani U. Biliary tract injuries during laparoscopic cholecystectomy: three case reports and literature review. G Chir. 2010;31:16-19. [PubMed] |
| 84. | Collan Y, Hakkiluoto A, Hästbacka J. Ectopic liver. Ann Chir Gynaecol. 1978;67:27-29. [PubMed] |
| 85. | Zhang ZL, Wang JL, Guo CL, Li Q, Li L, Pang Y, Meng XC. Ectopic liver tissue in the esophagus: A case report. Medicine (Baltimore). 2019;98:e15260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 86. | Matley PJ, Rode H, Cywes S. Portal vein obstruction by ectopic liver tissue. J Pediatr Surg. 1989;24:1163-1164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 87. | el Haddad MJ, Currie AB, Honeyman M. Pyloric obstruction by ectopic liver tissue. Br J Surg. 1985;72:917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Mizuguchi T, Ooi L, Wang G S-Editor: Fan JR L-Editor: Webster JR P-Editor: Li JH